BIOBRIEF
Alveolar Ridge Preservation with vallos® Mineralized Cortico-Cancellous Allograft

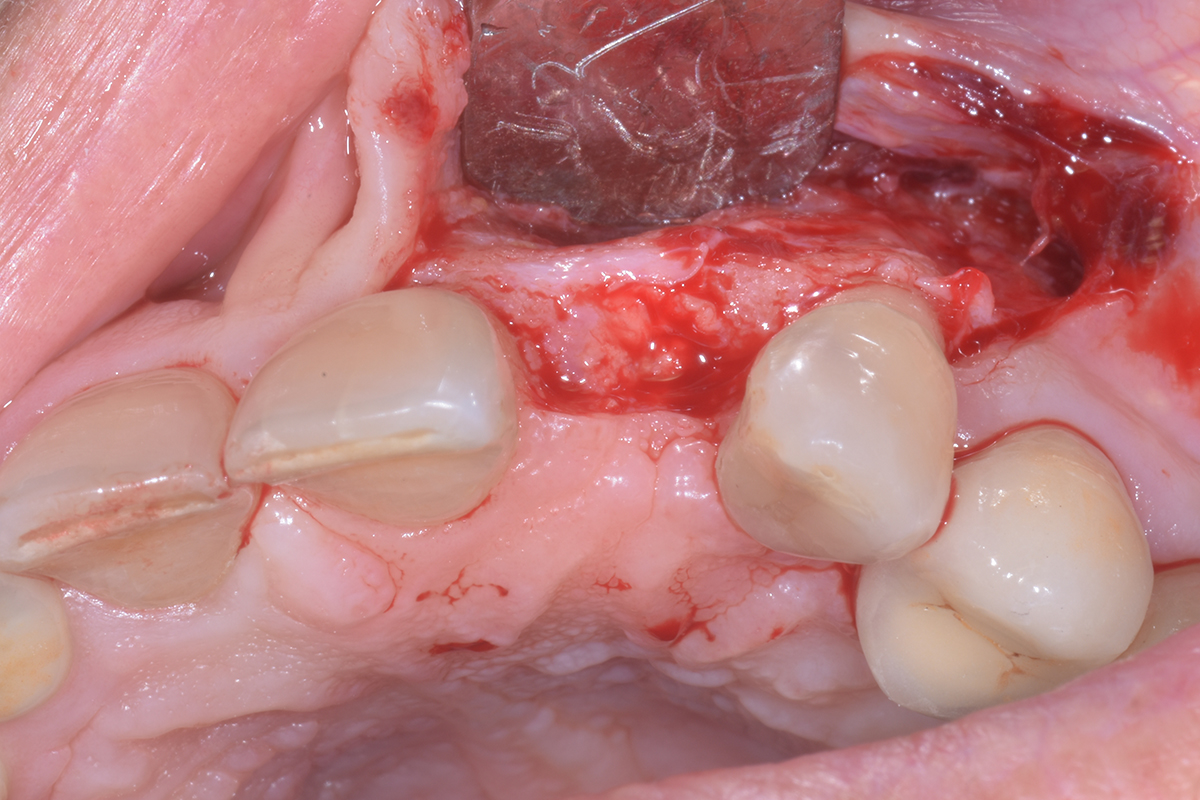
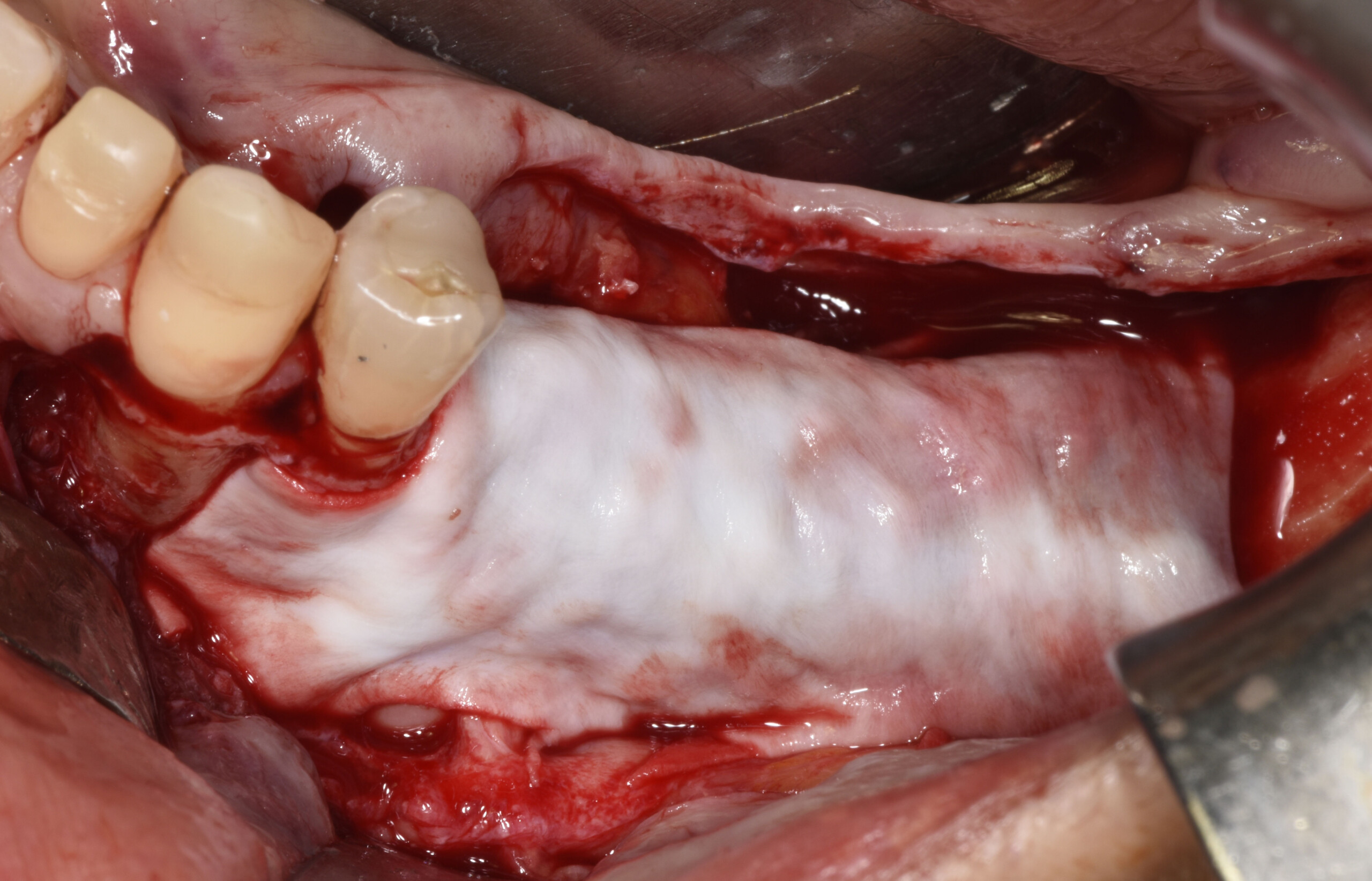
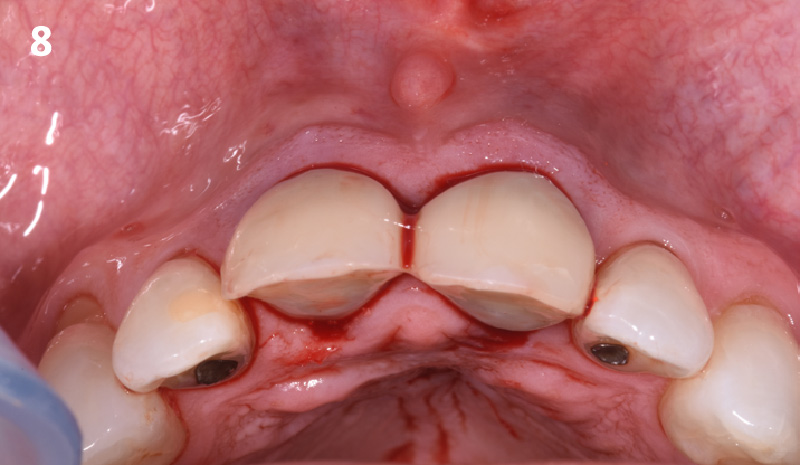
THE SITUATION
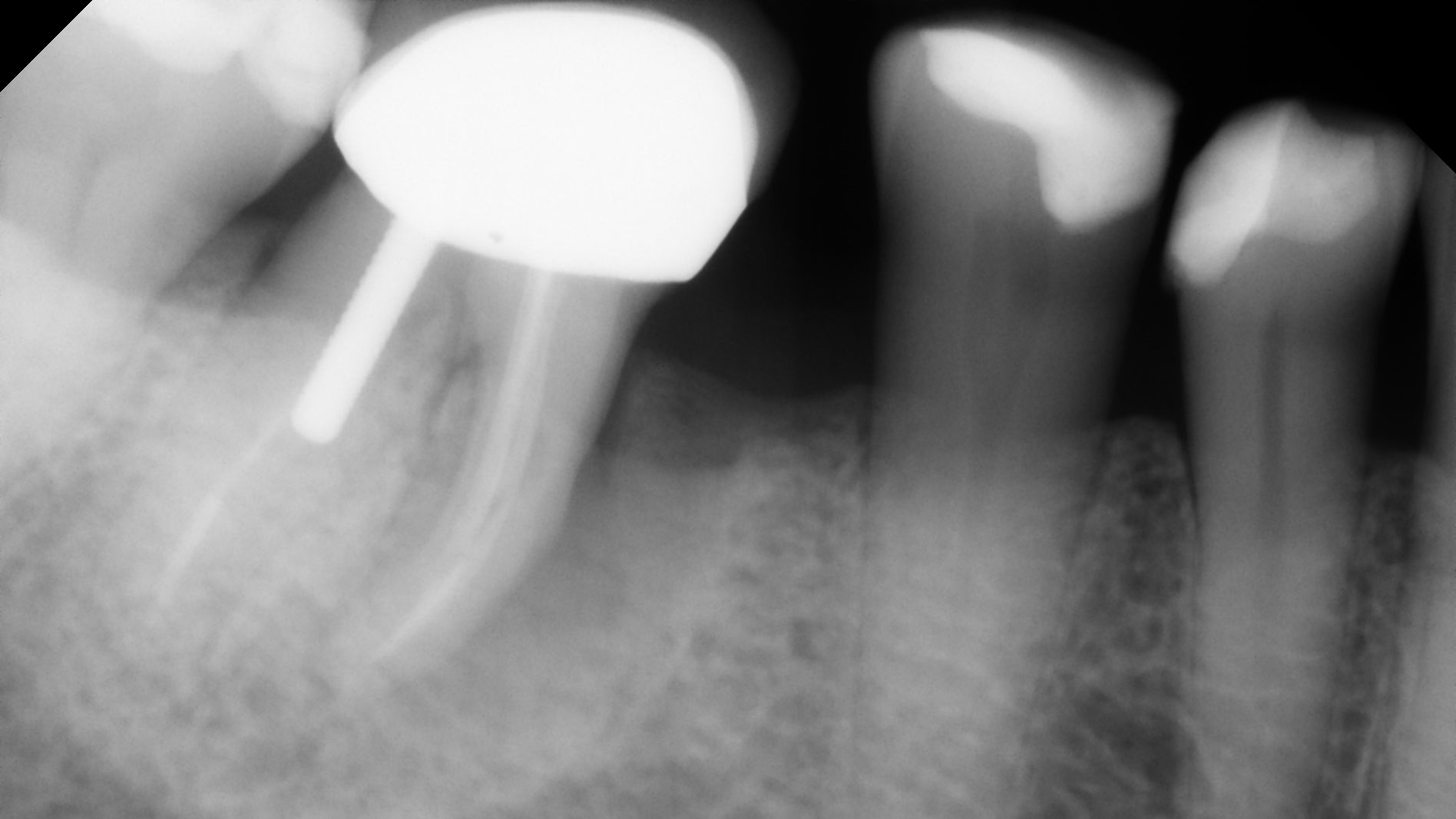
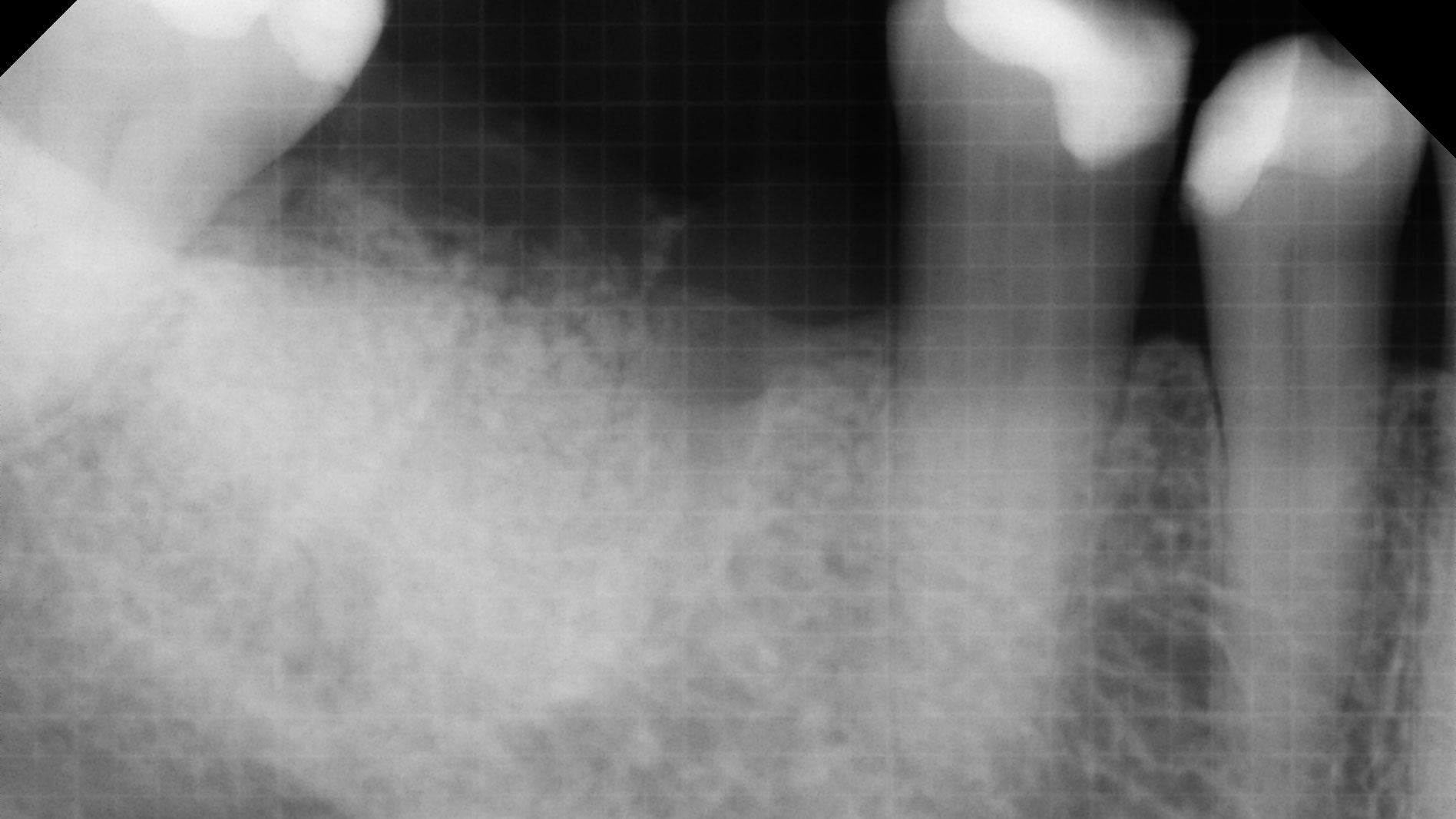
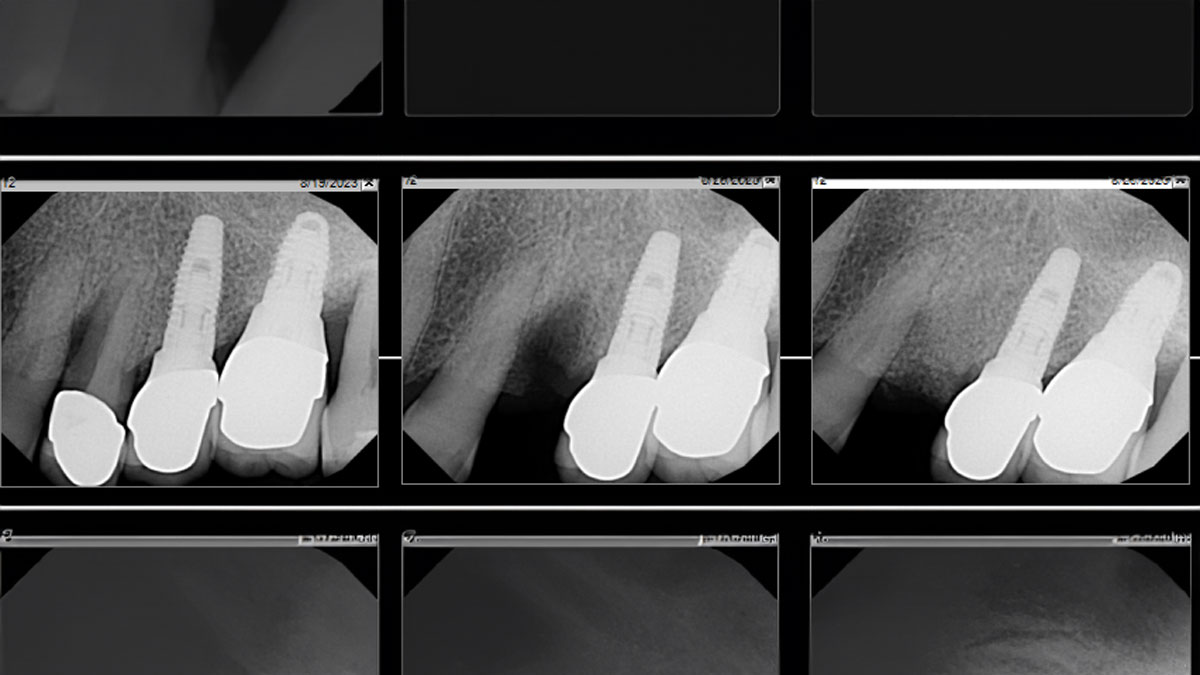
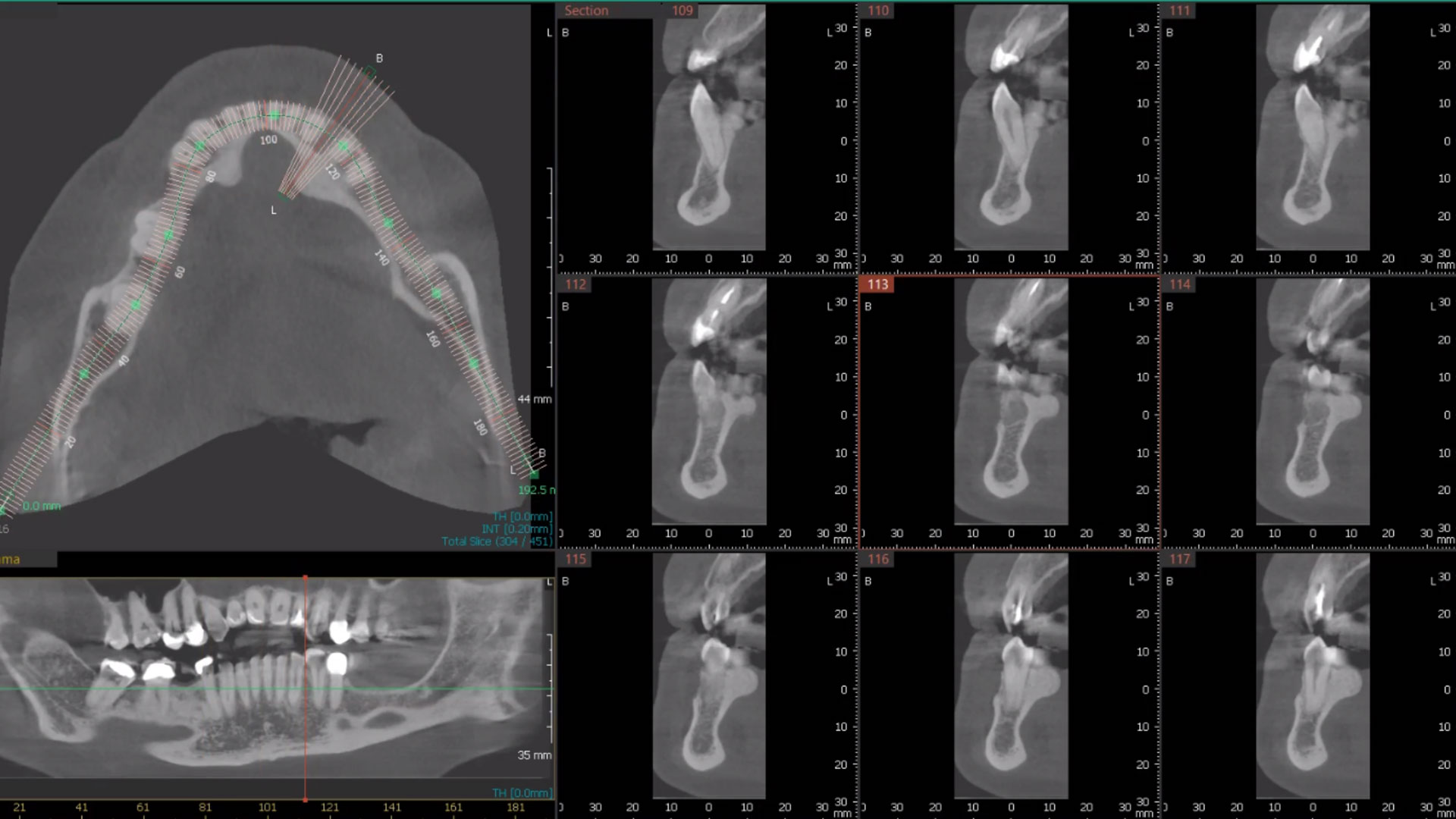
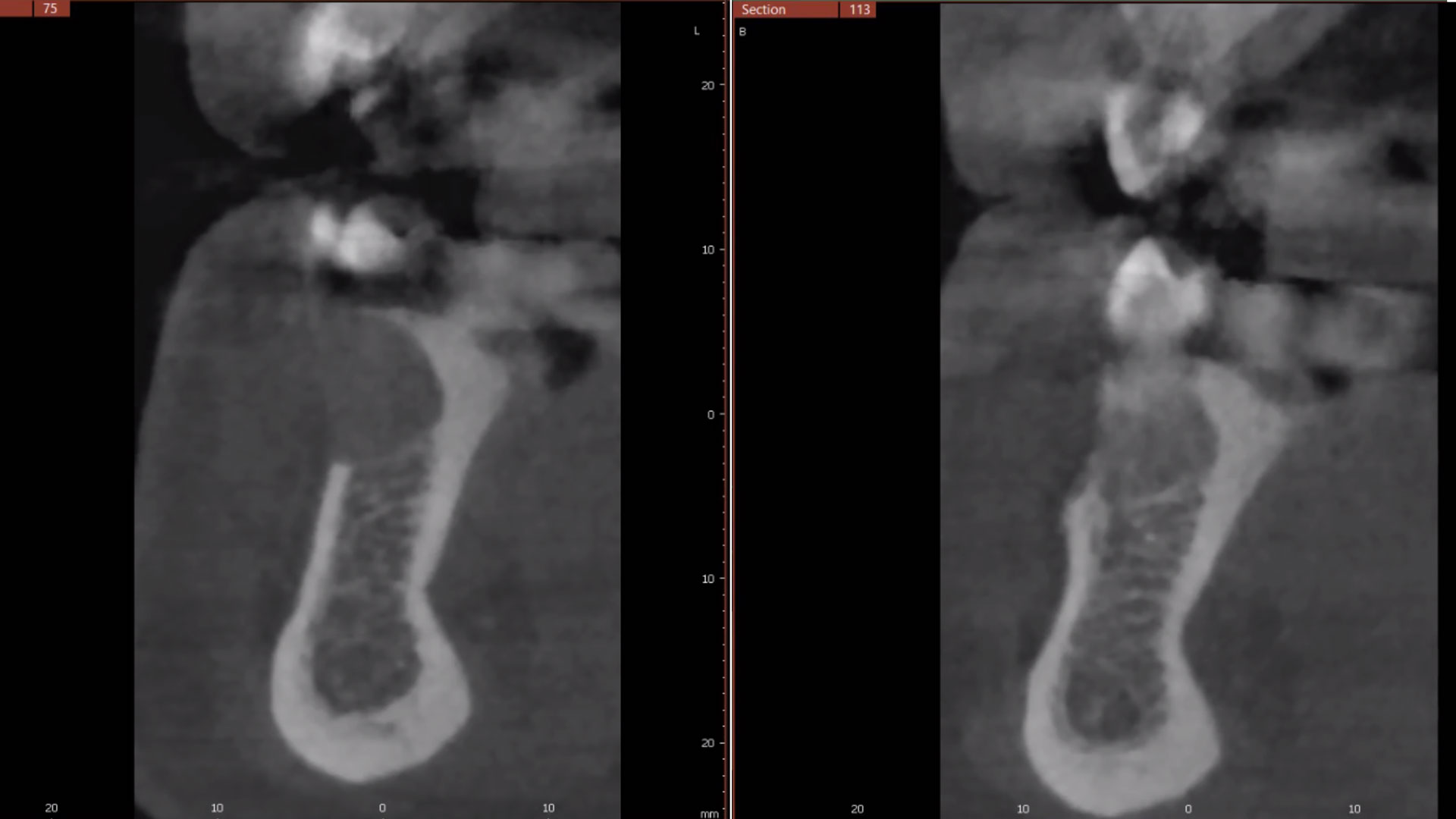
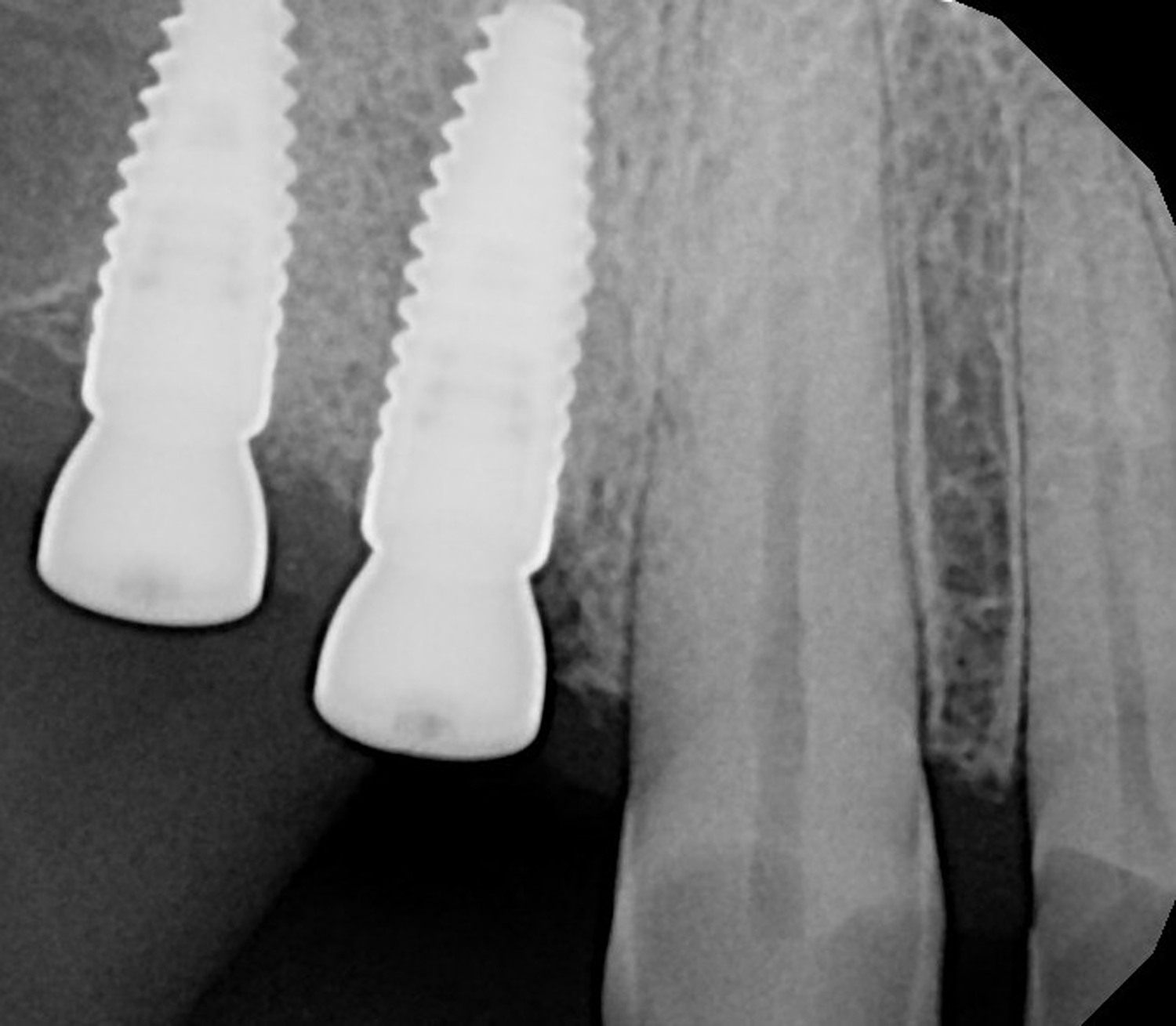
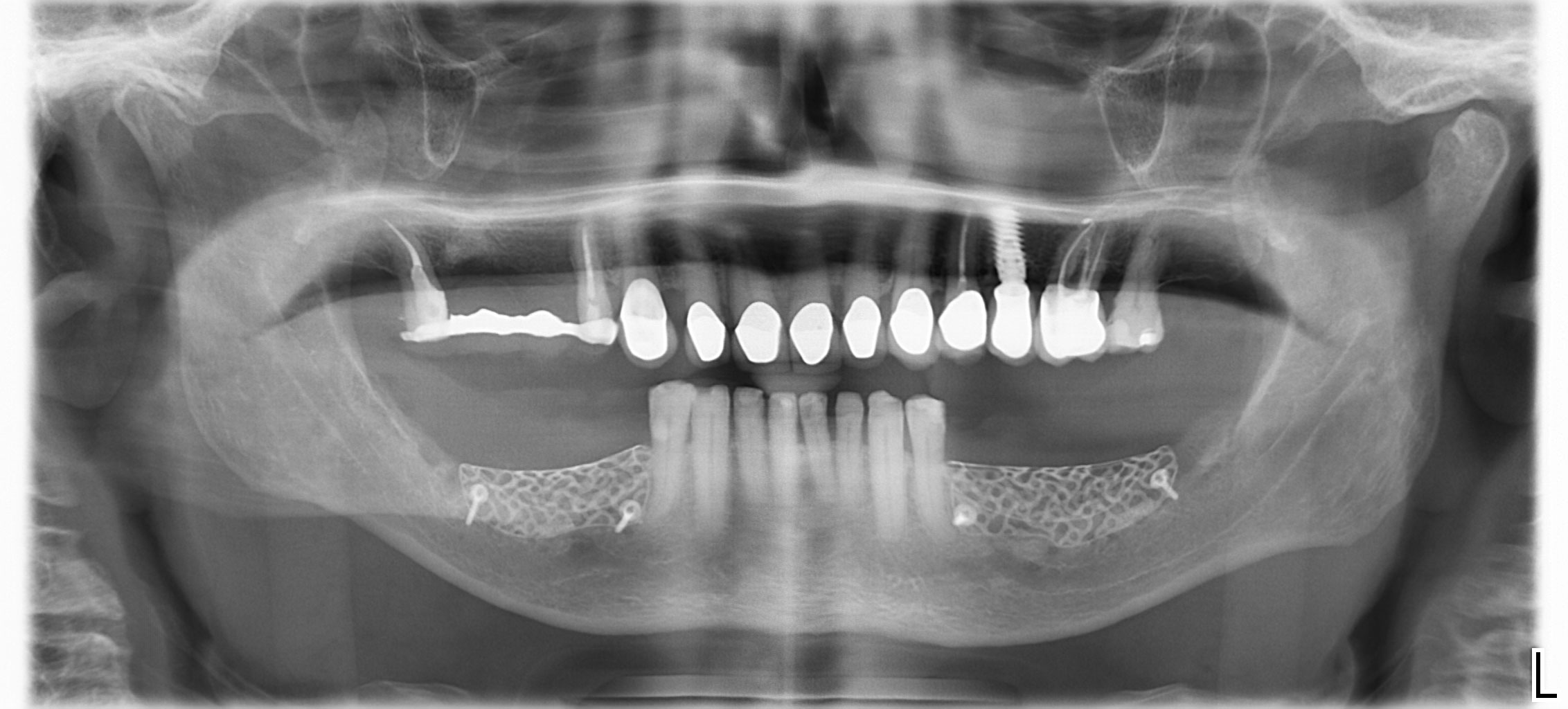
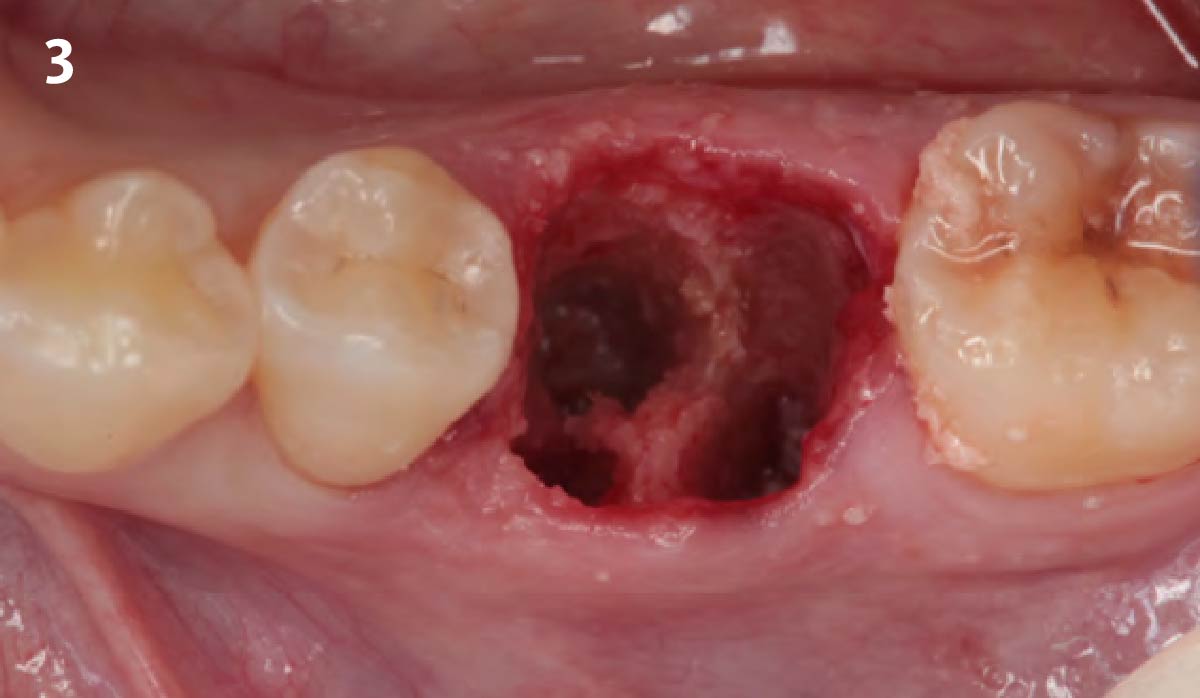
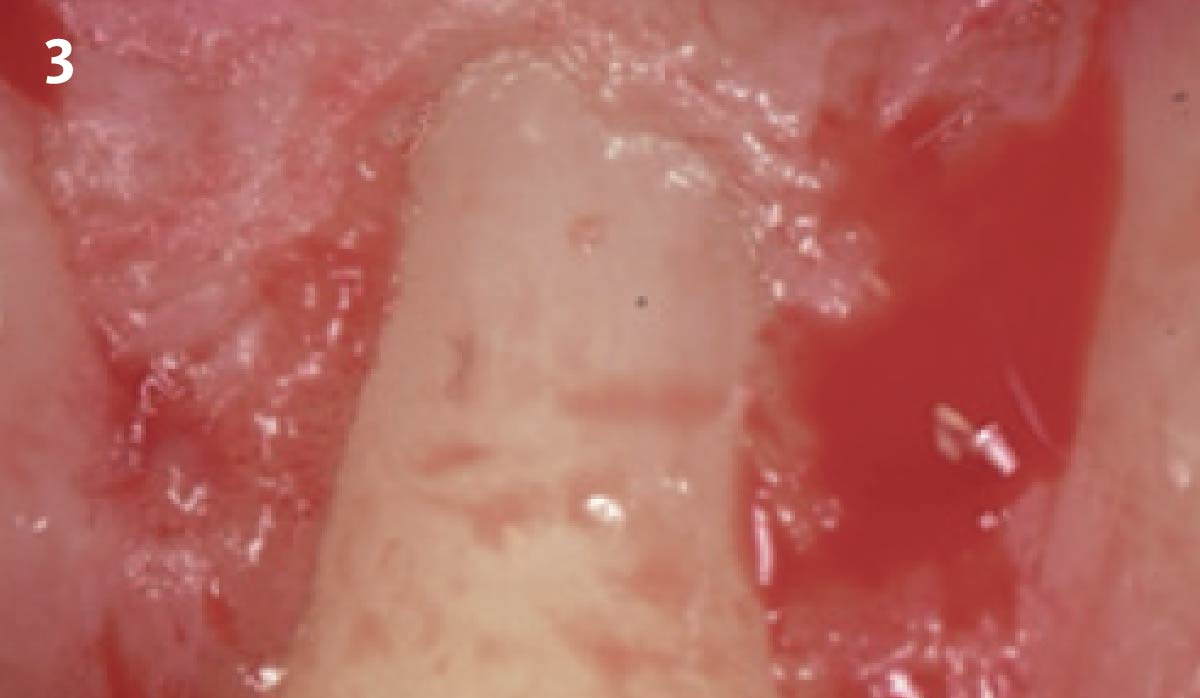
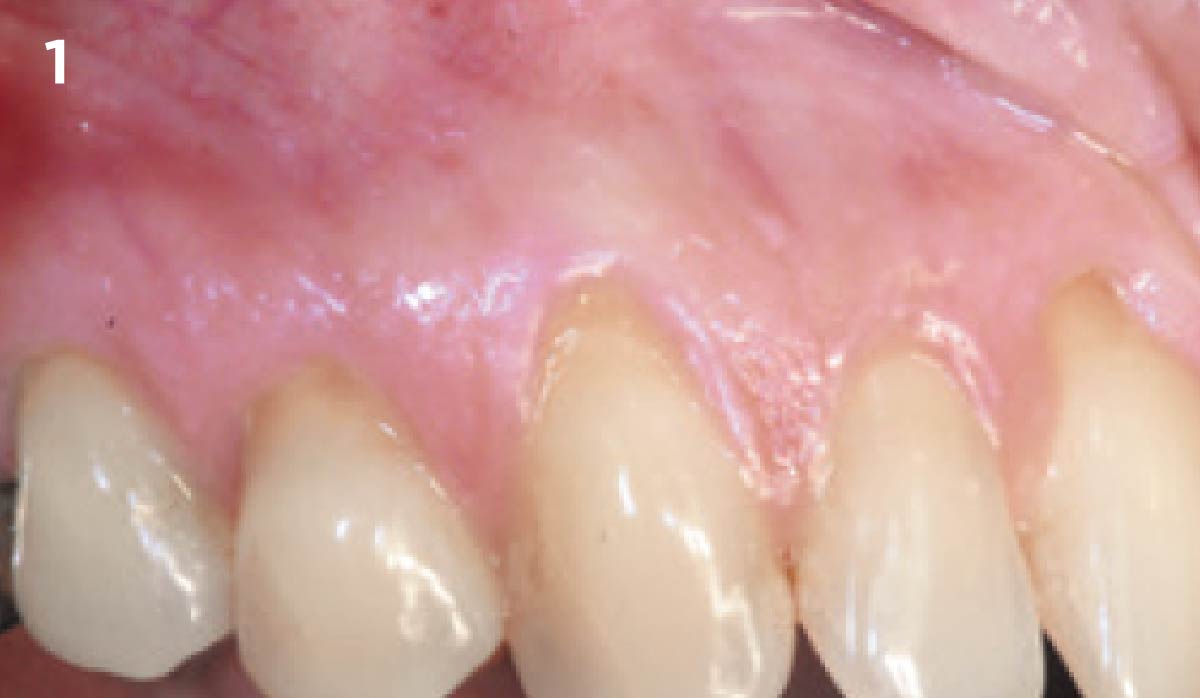
A 68 year old female patient was referred from her general dentist for persistent minor discomfort on #31, suspected endo-perio lesion. Upon the examination, deep probing depth and grade 1 mobility were noted. Radiographic interpretation indicating a large J shaped lesion and possible root fracture. Patient had missing #30 and #32 has been mesially drifted and left a restorative space more than > 13 mm mesio-distally.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system/Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
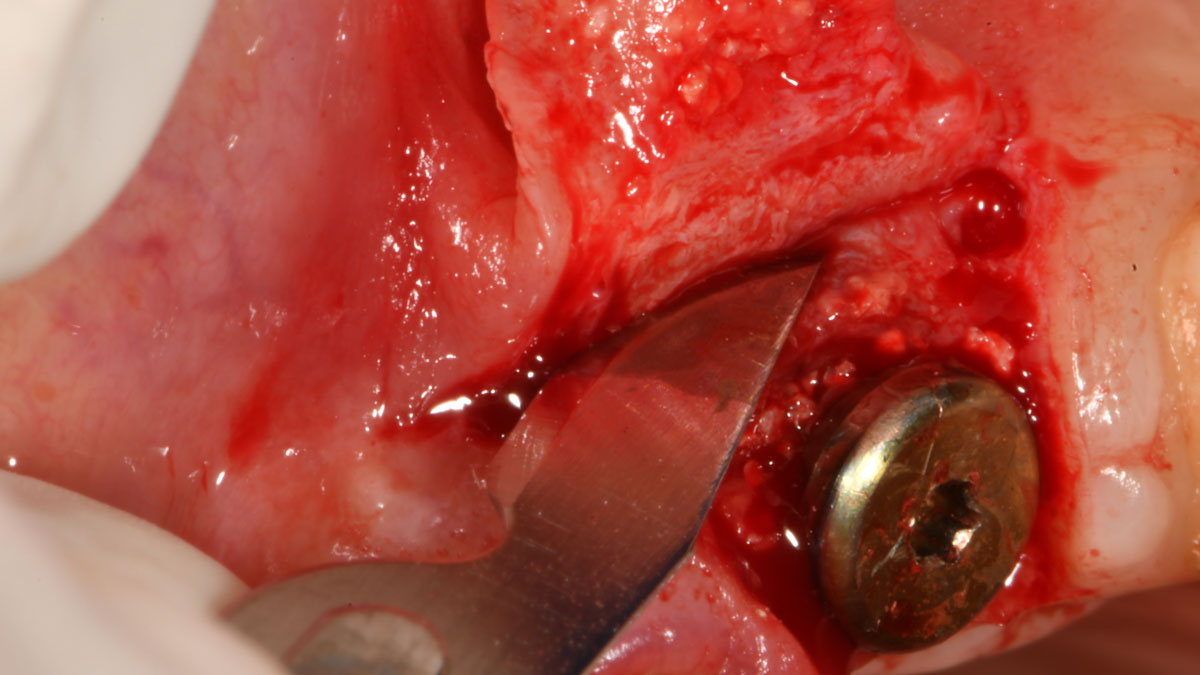
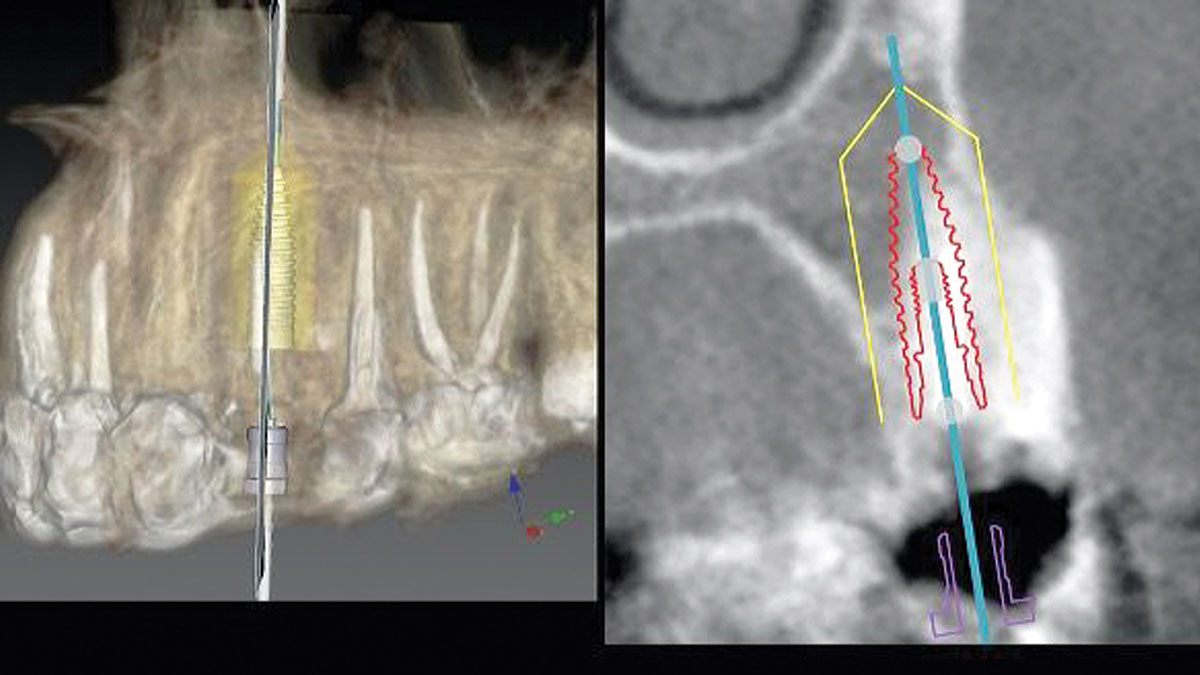
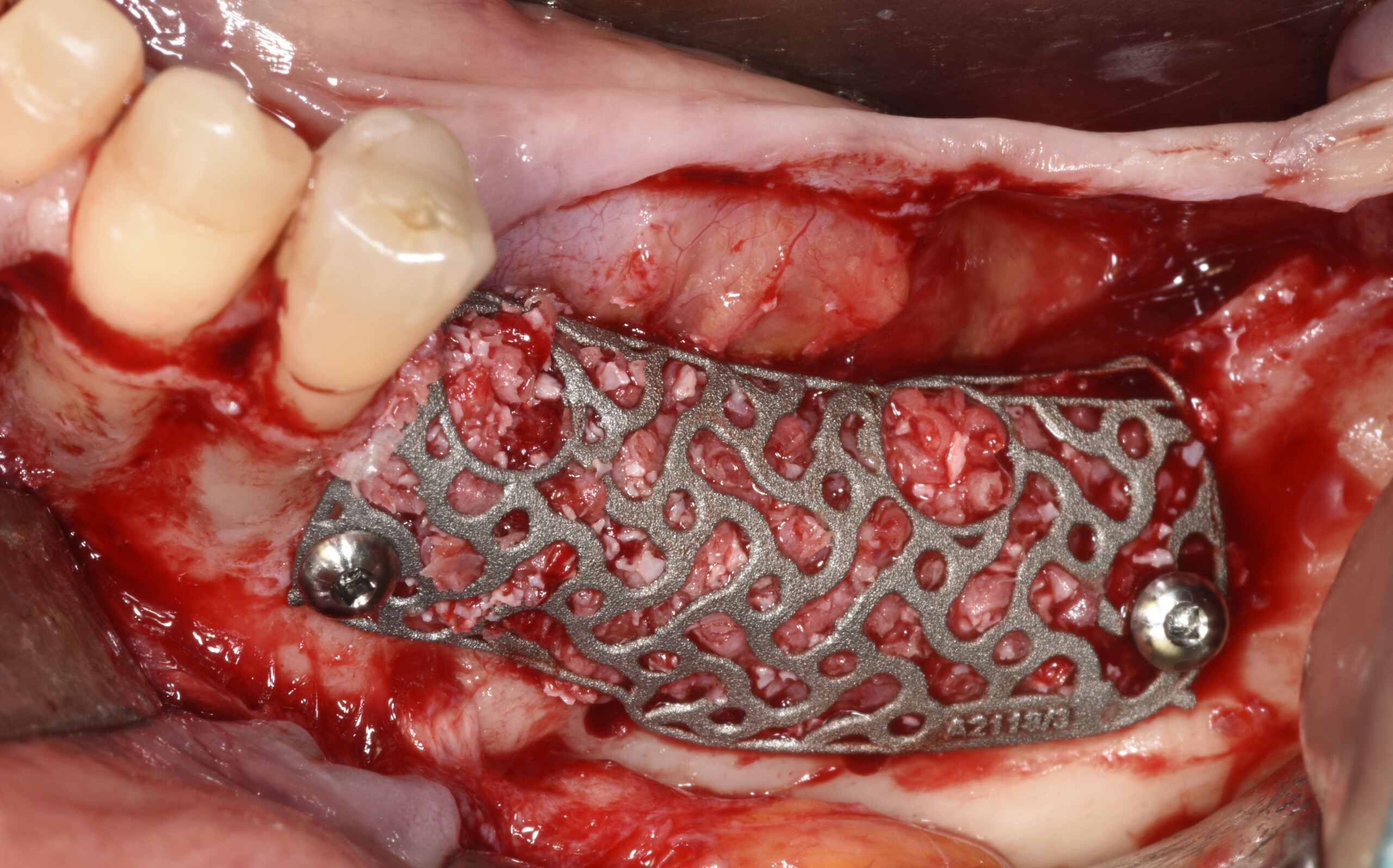
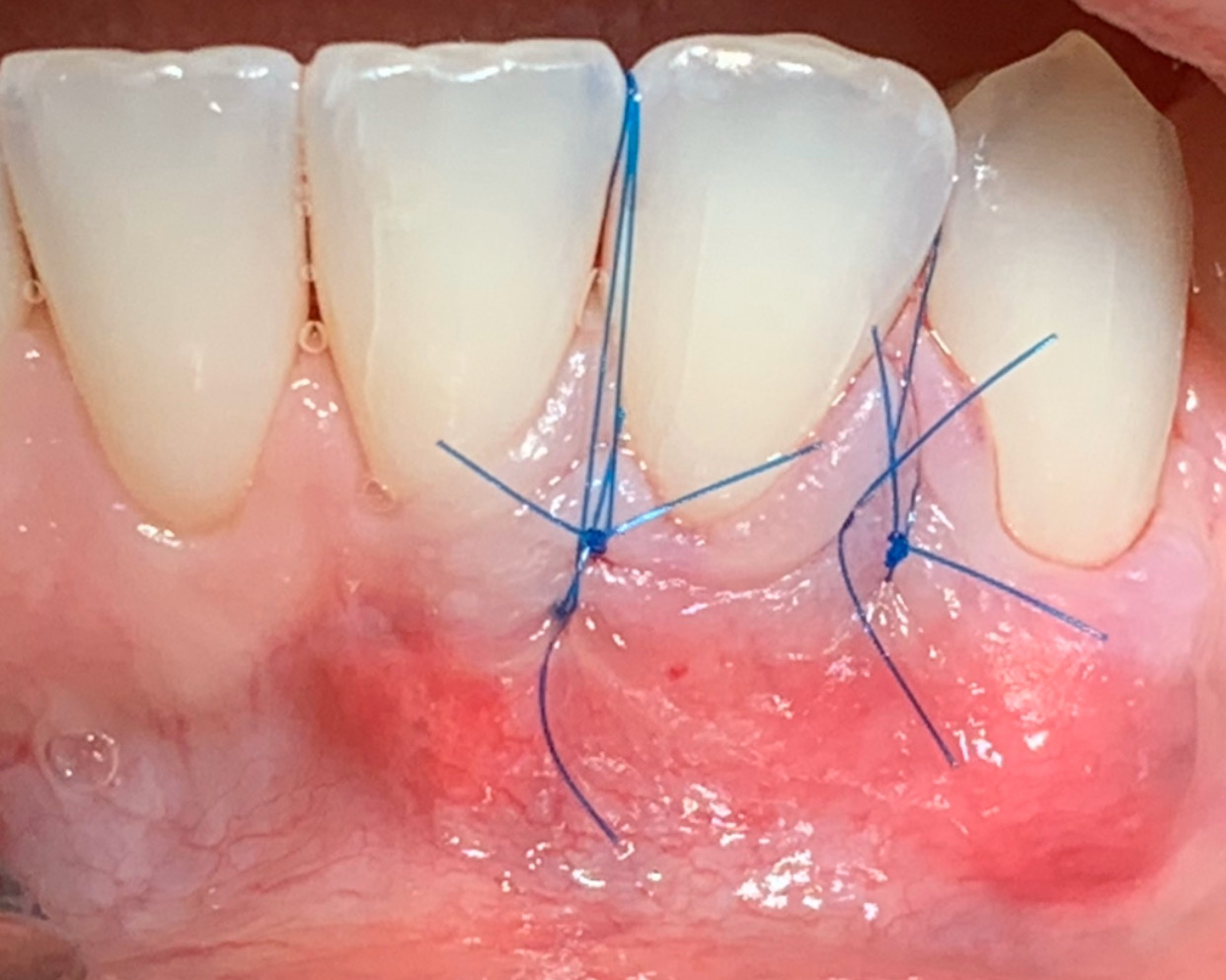
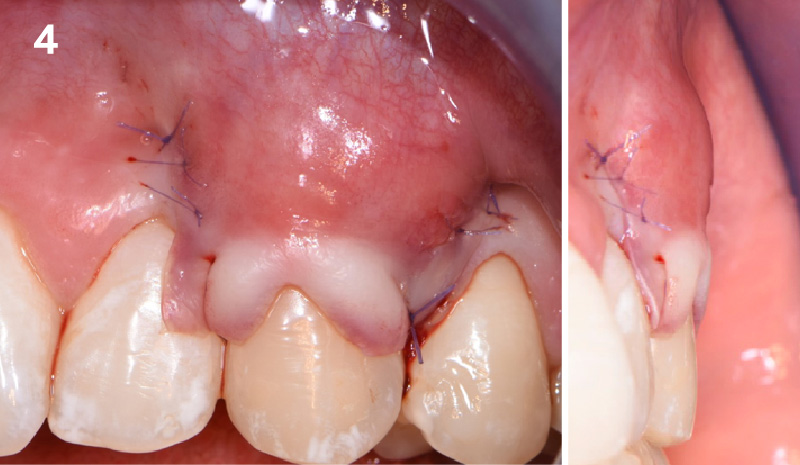
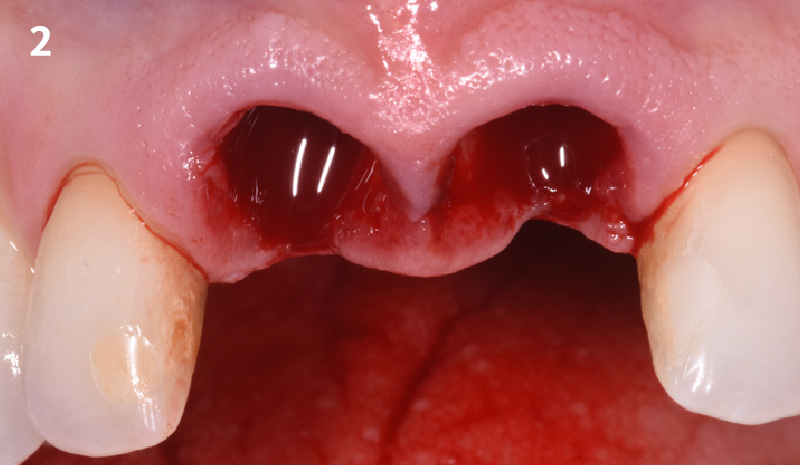
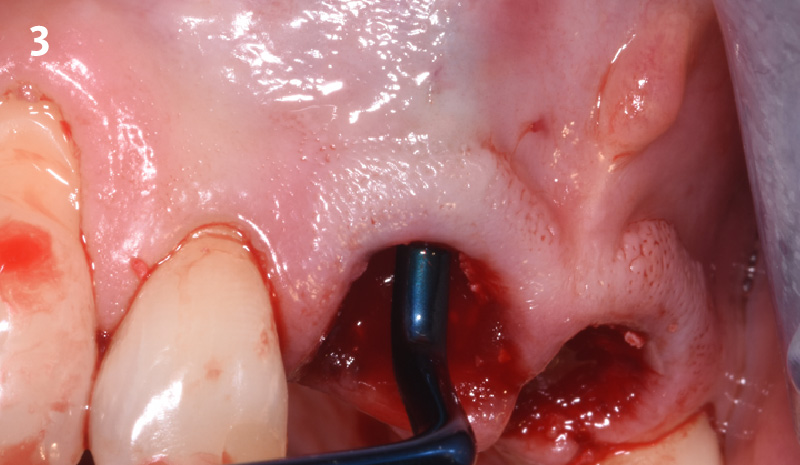
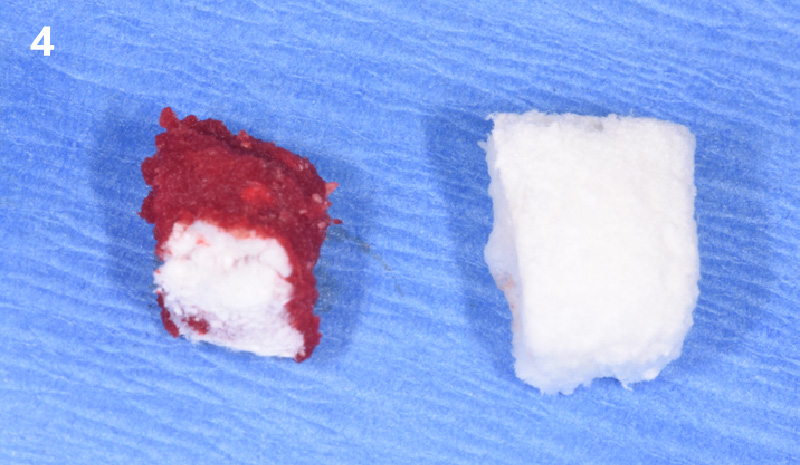
THE APPROACH
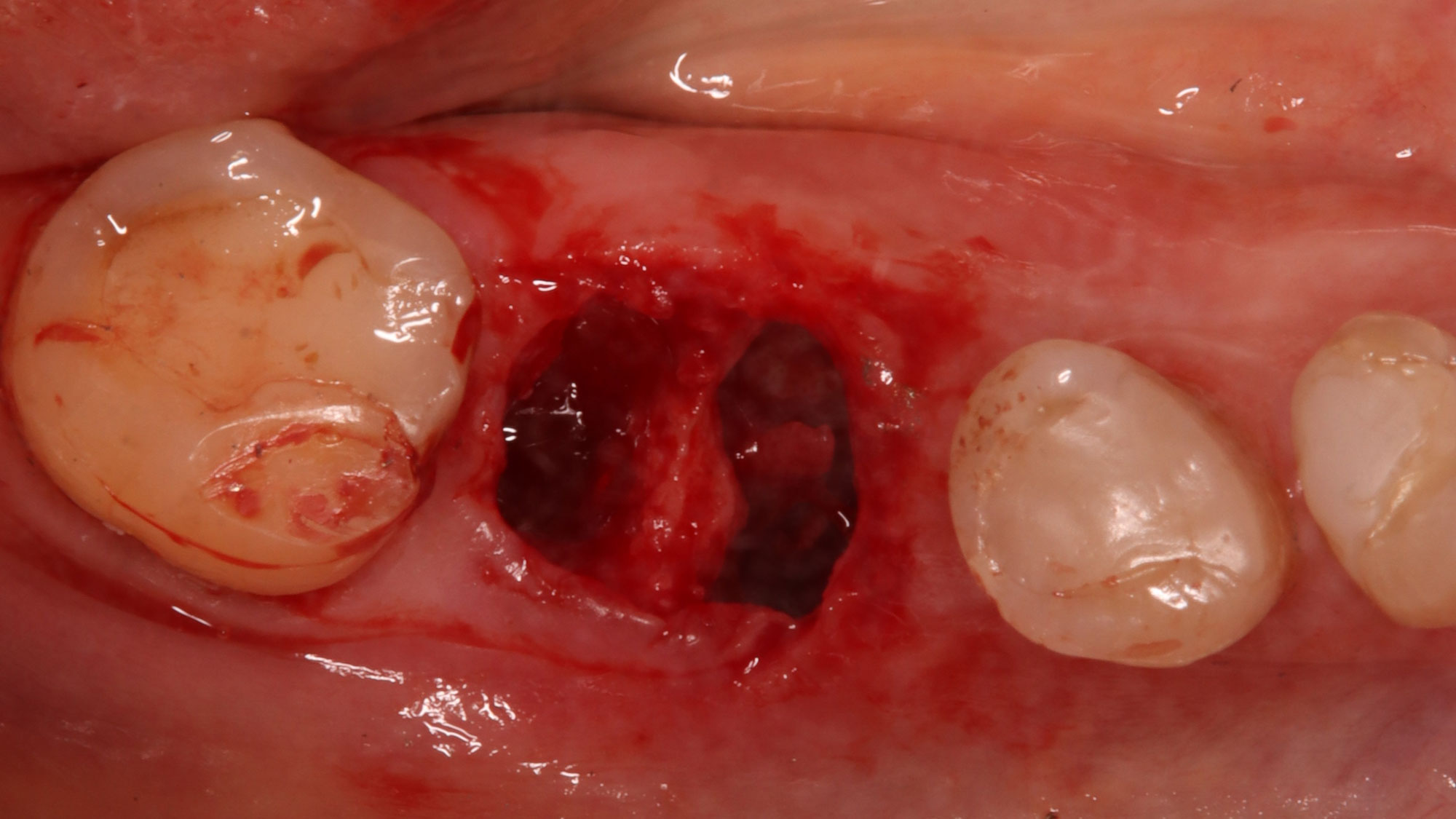
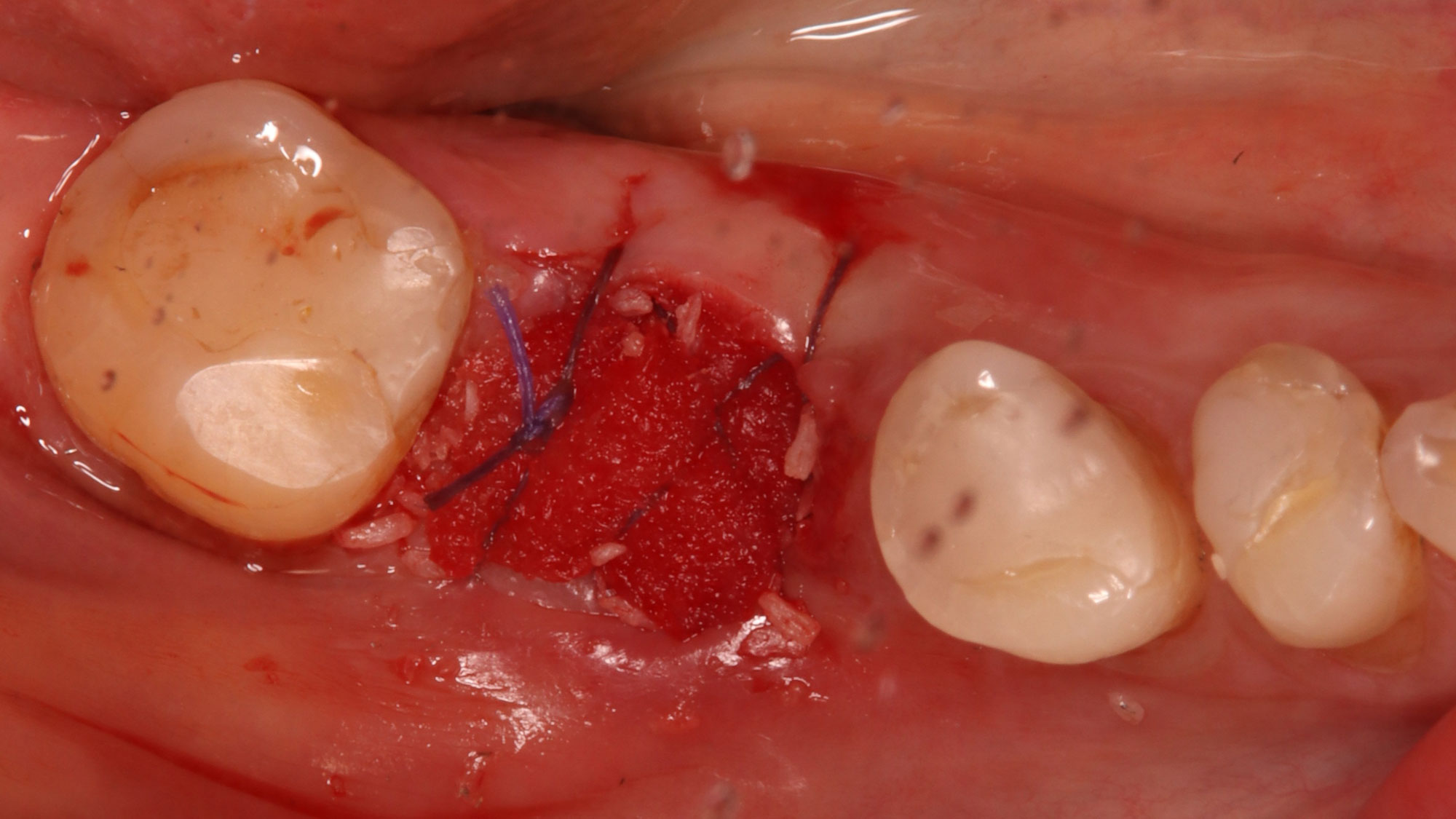
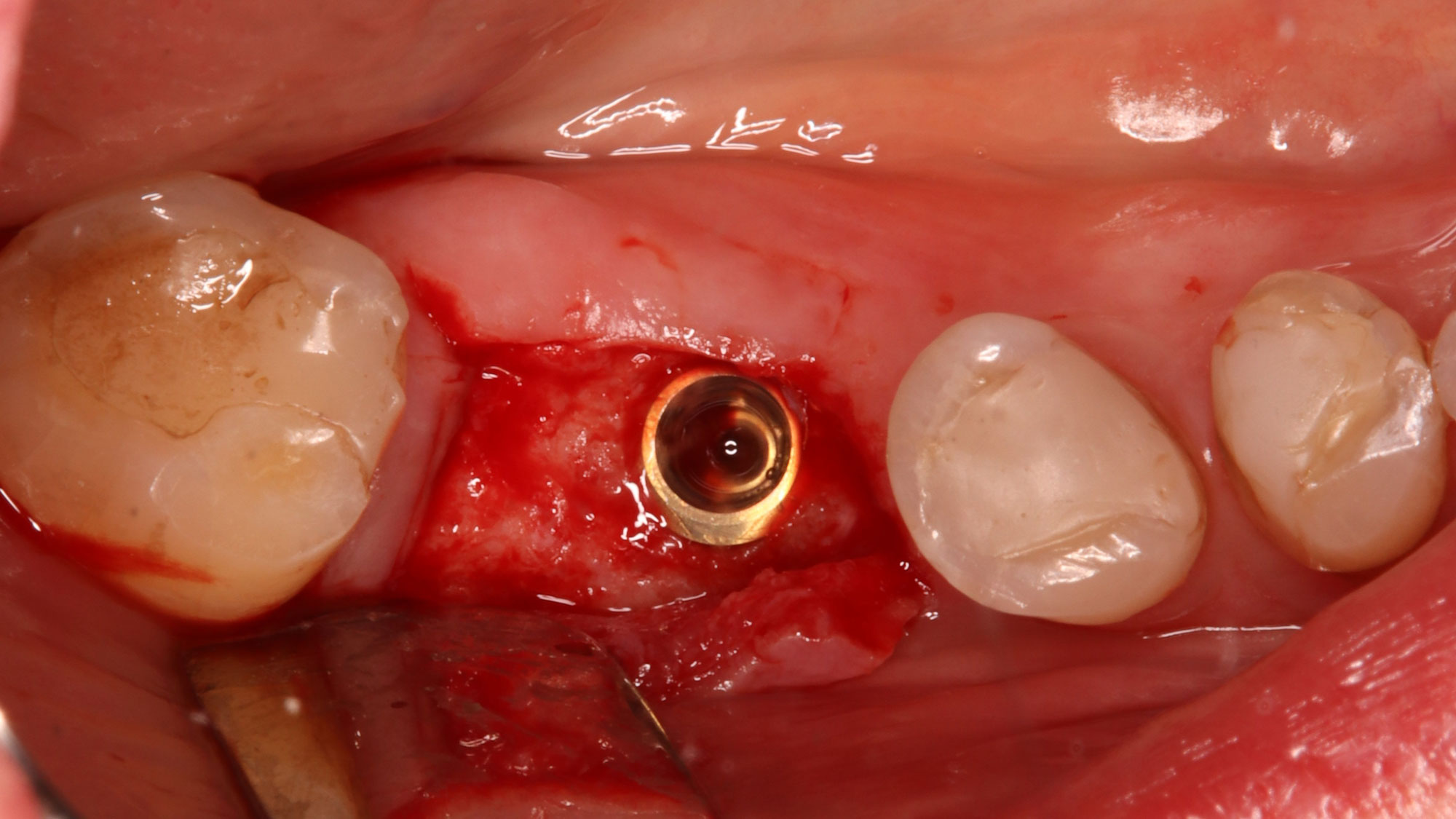
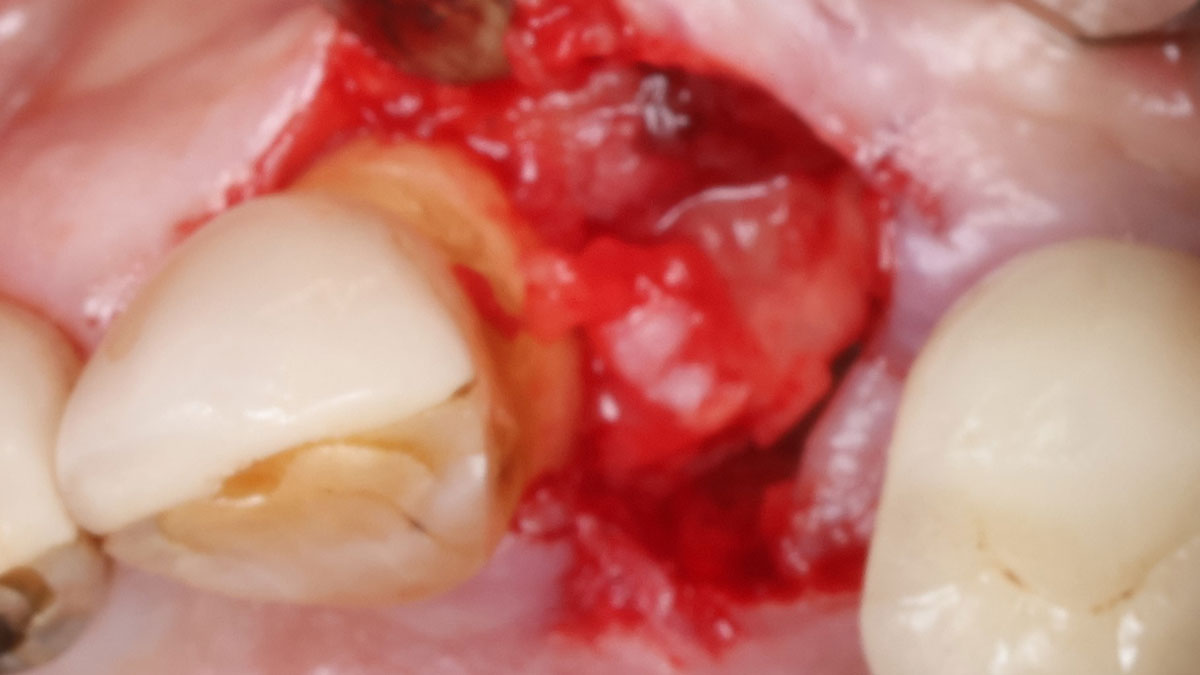
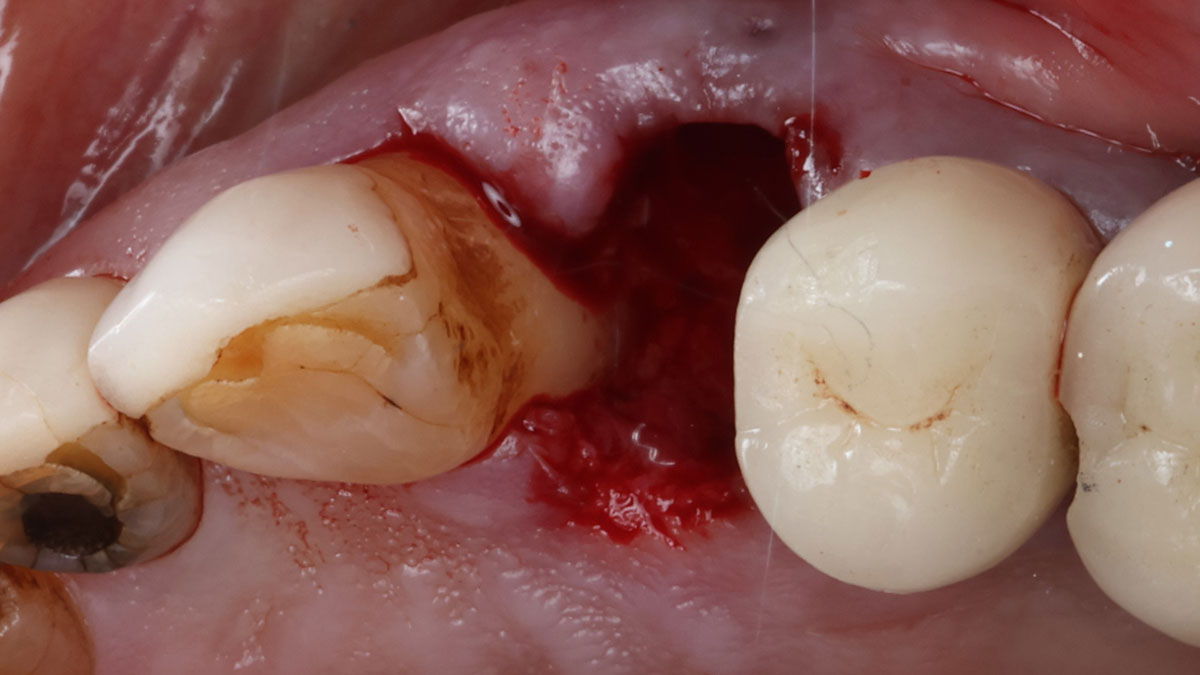
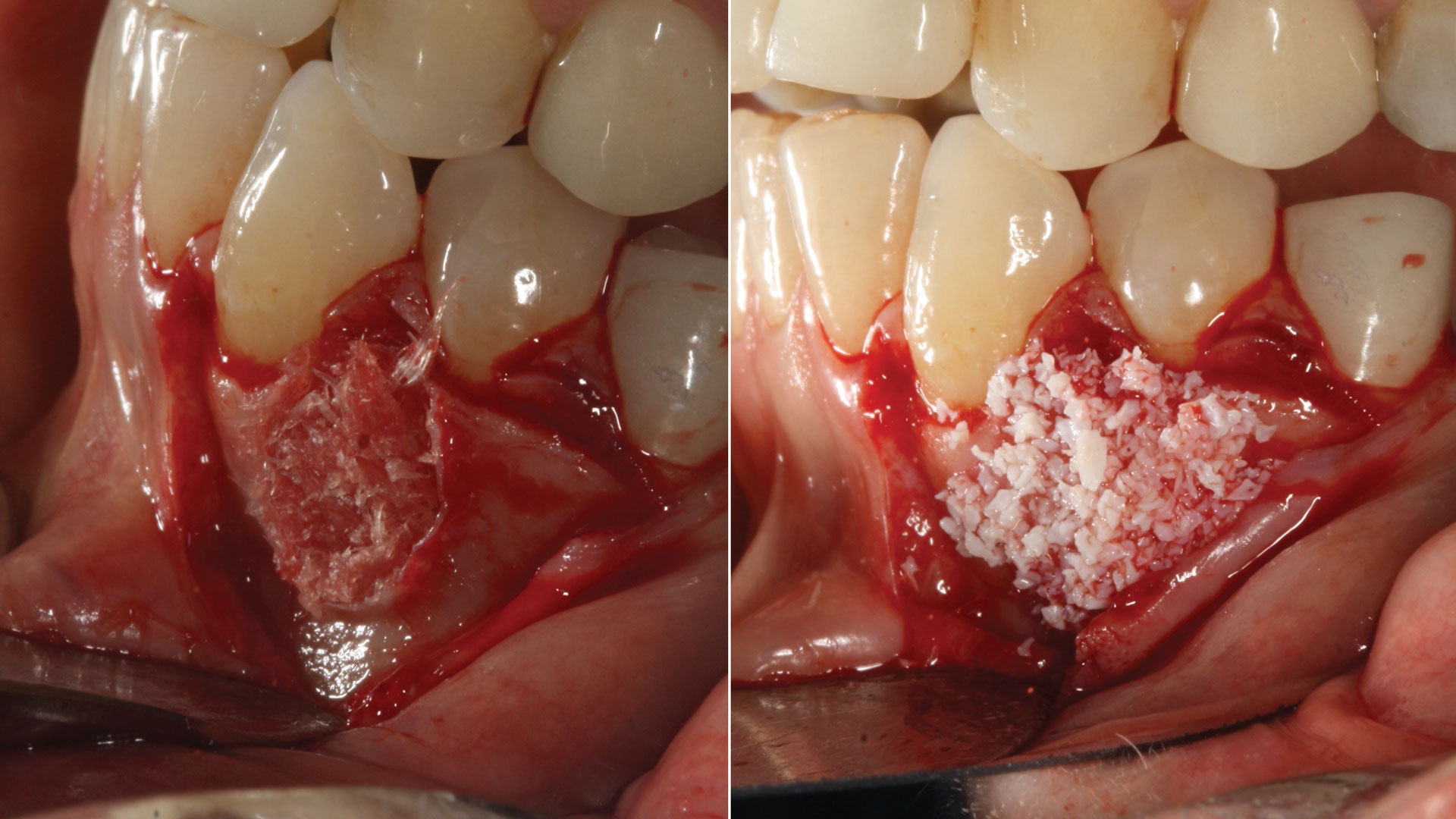
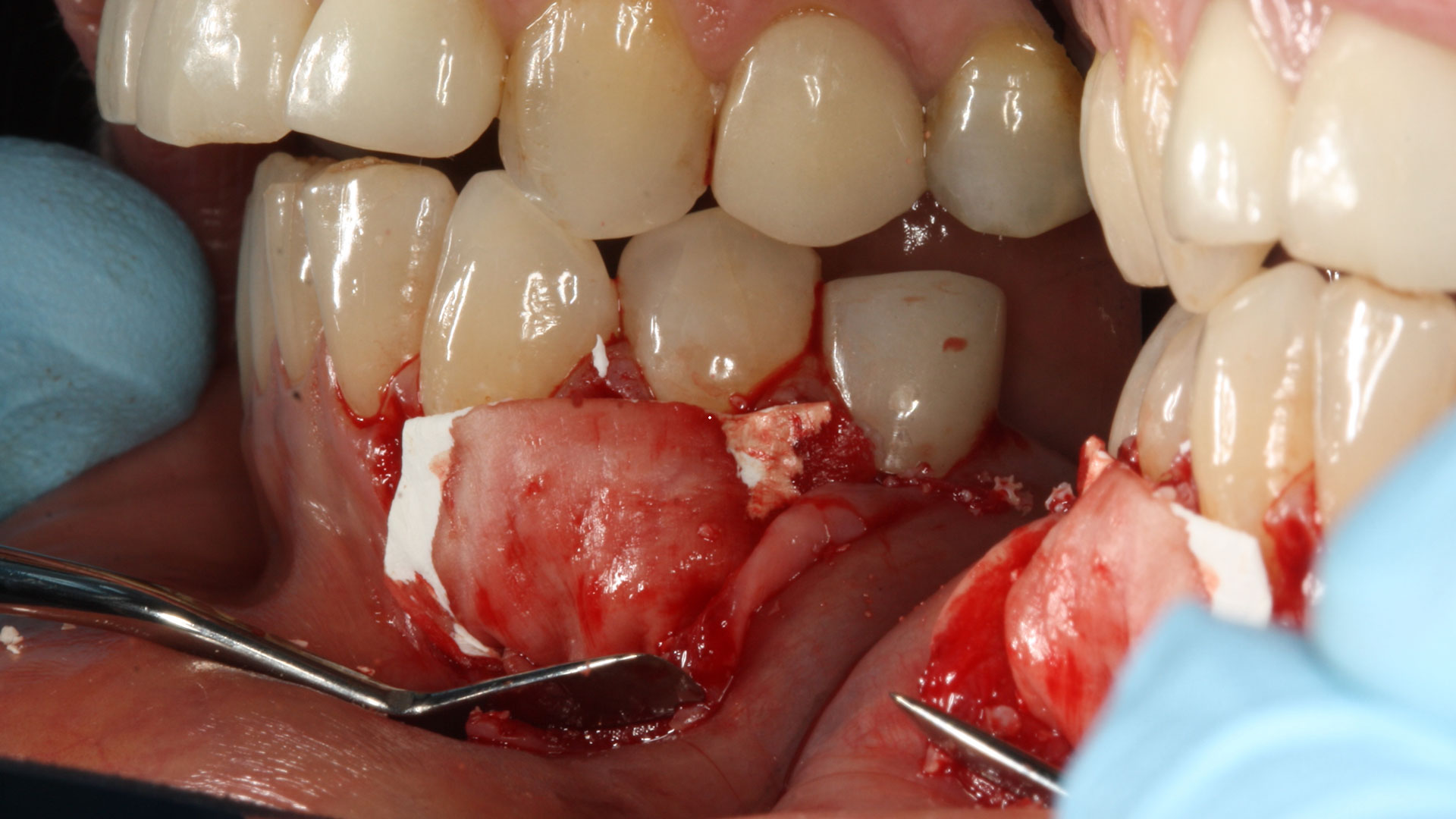
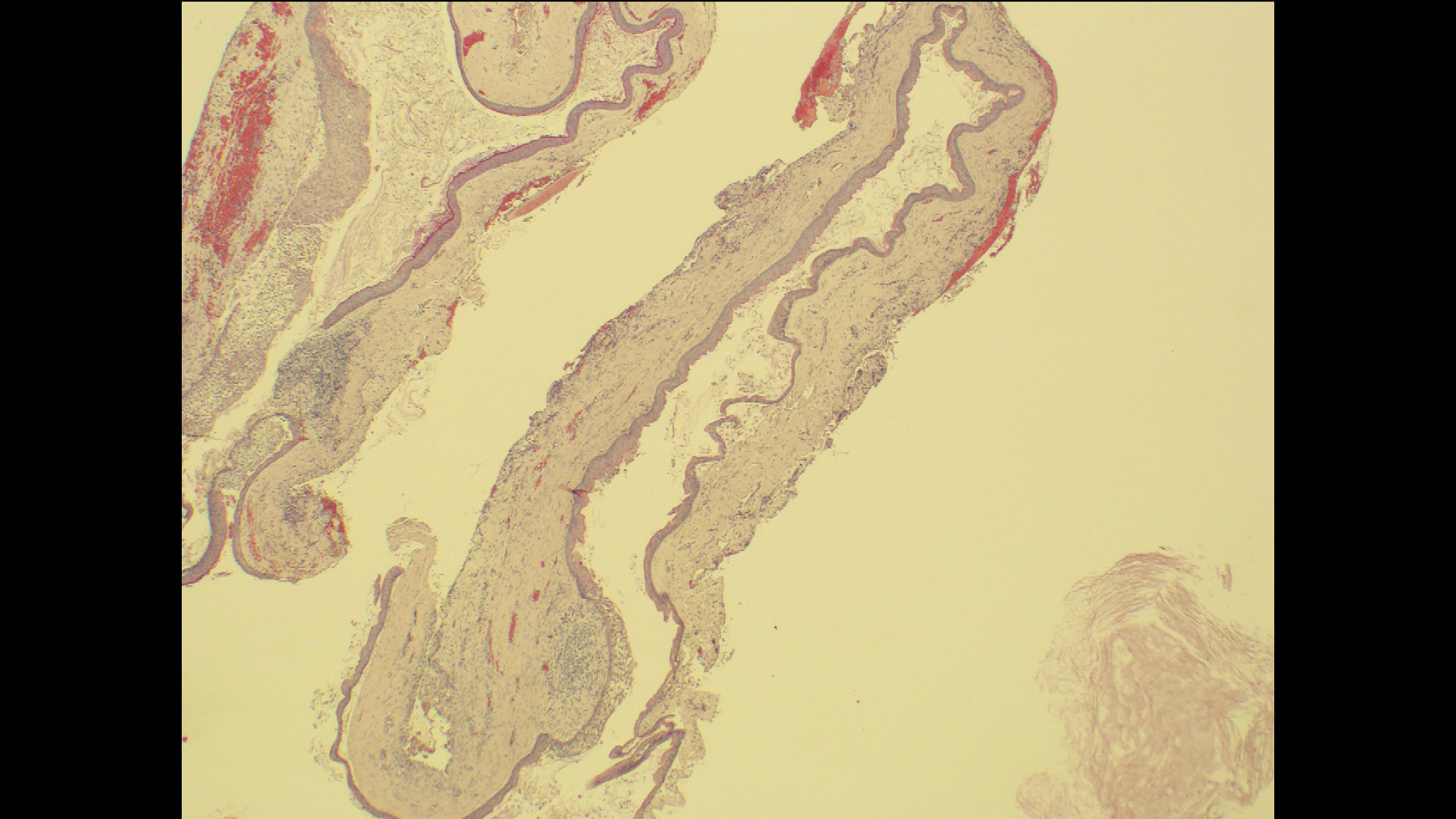
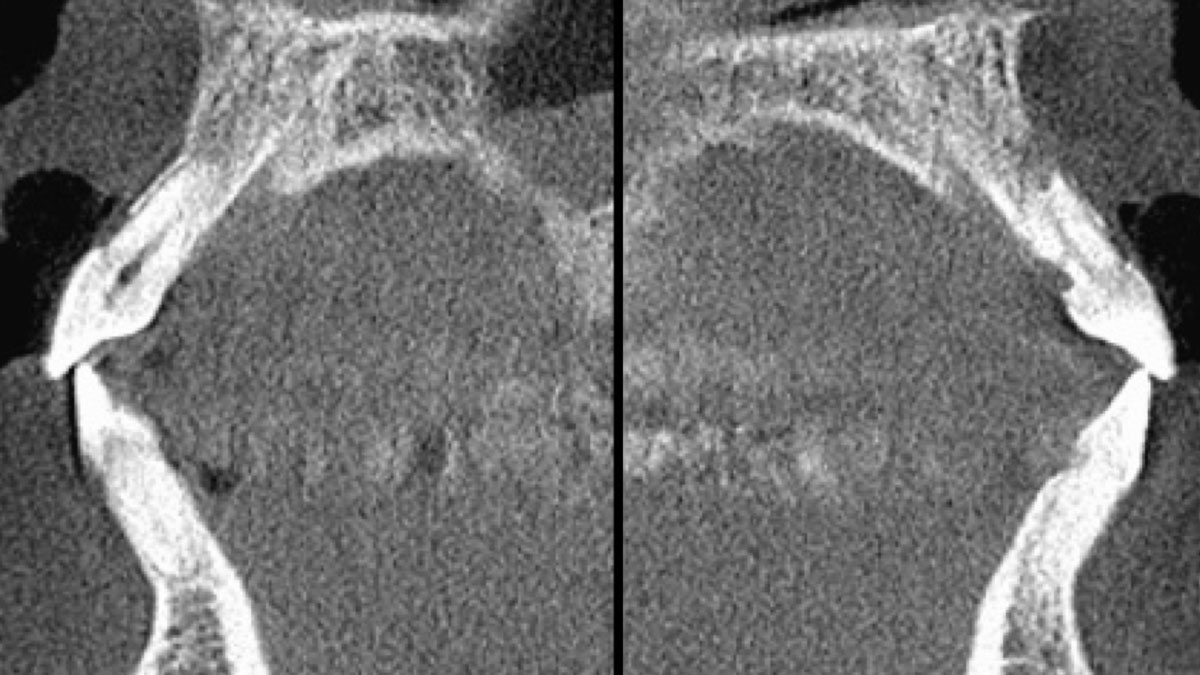
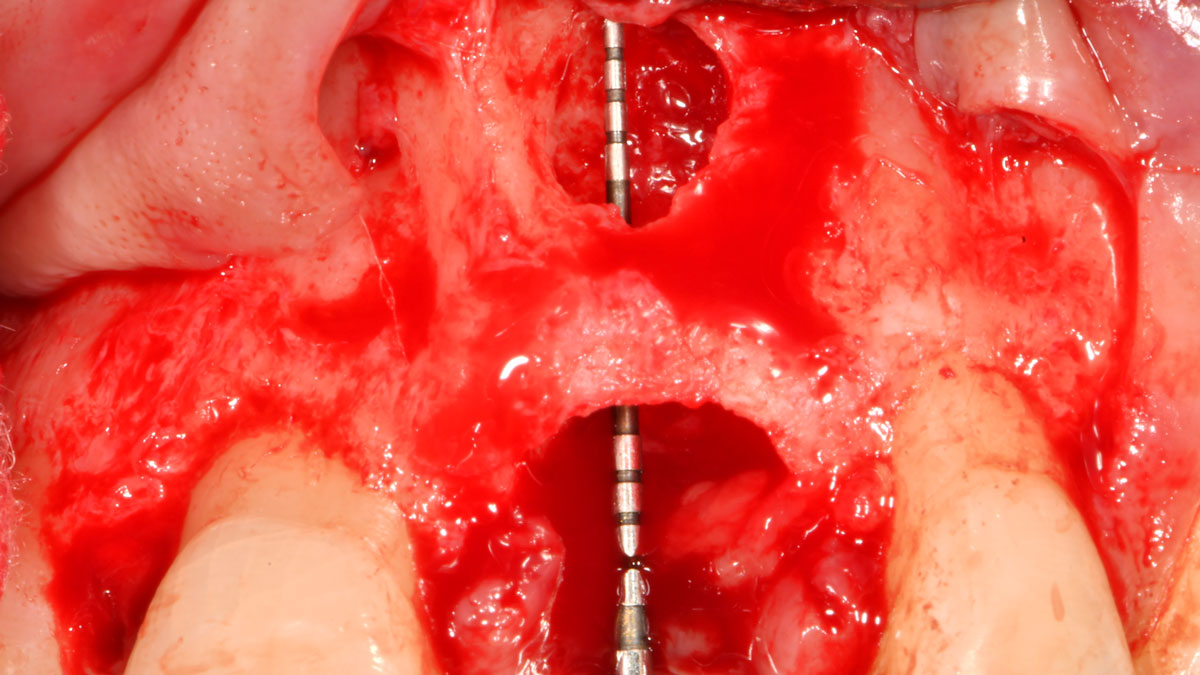
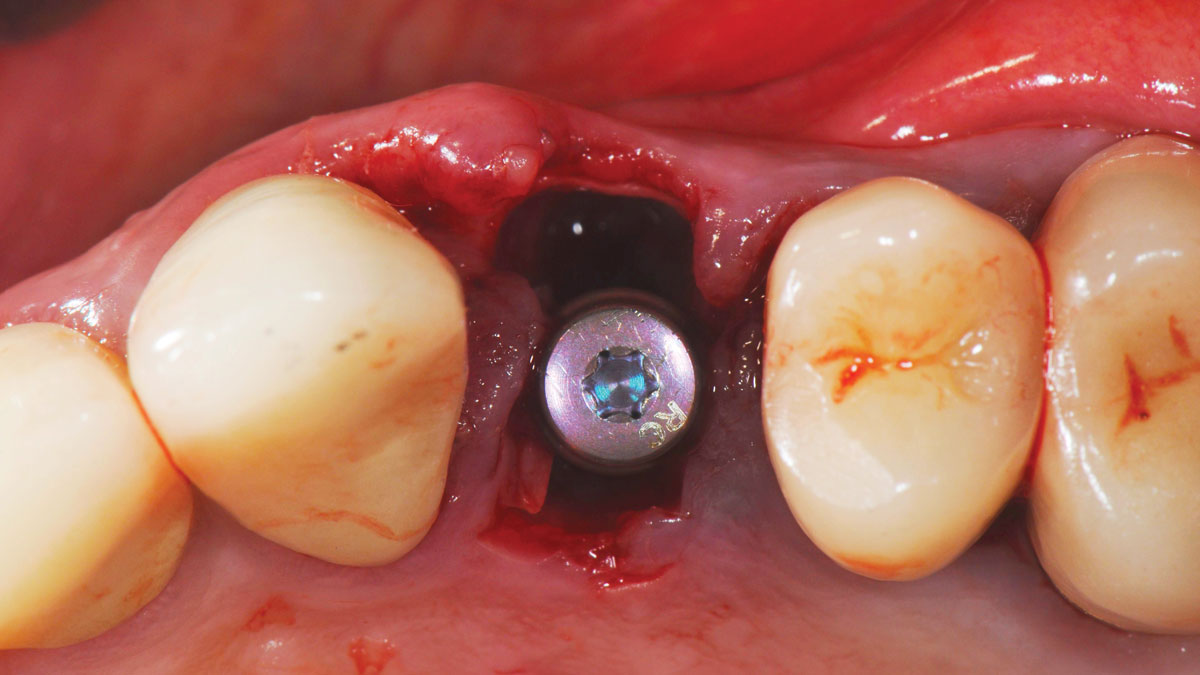
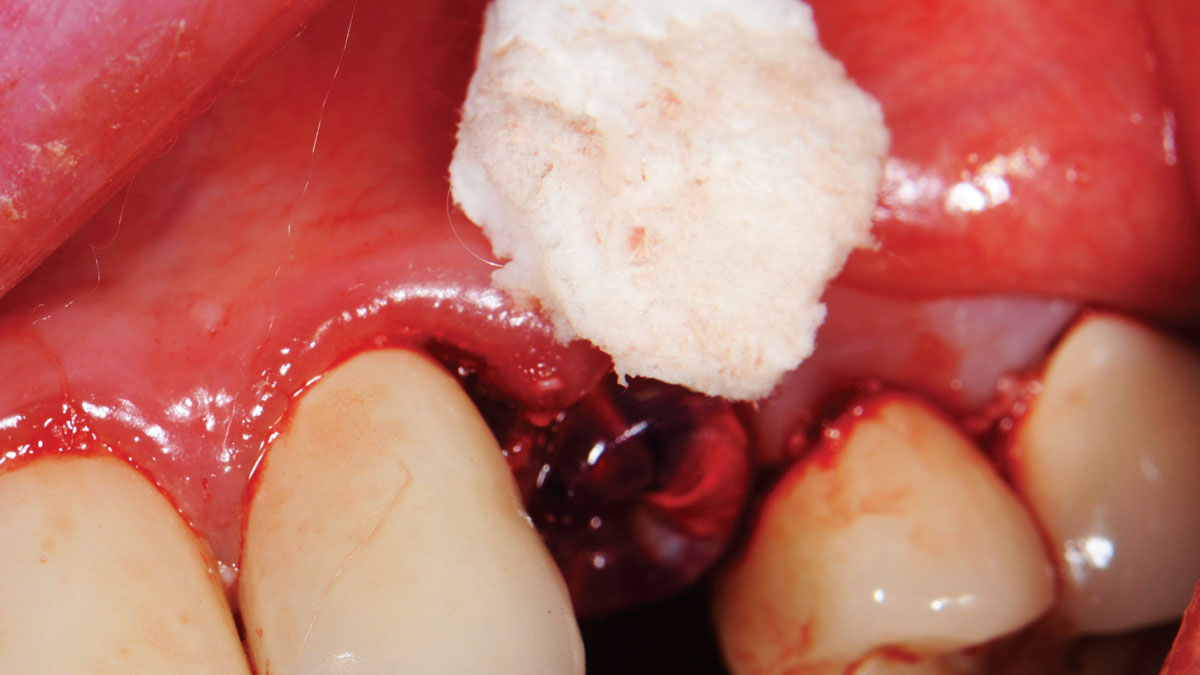
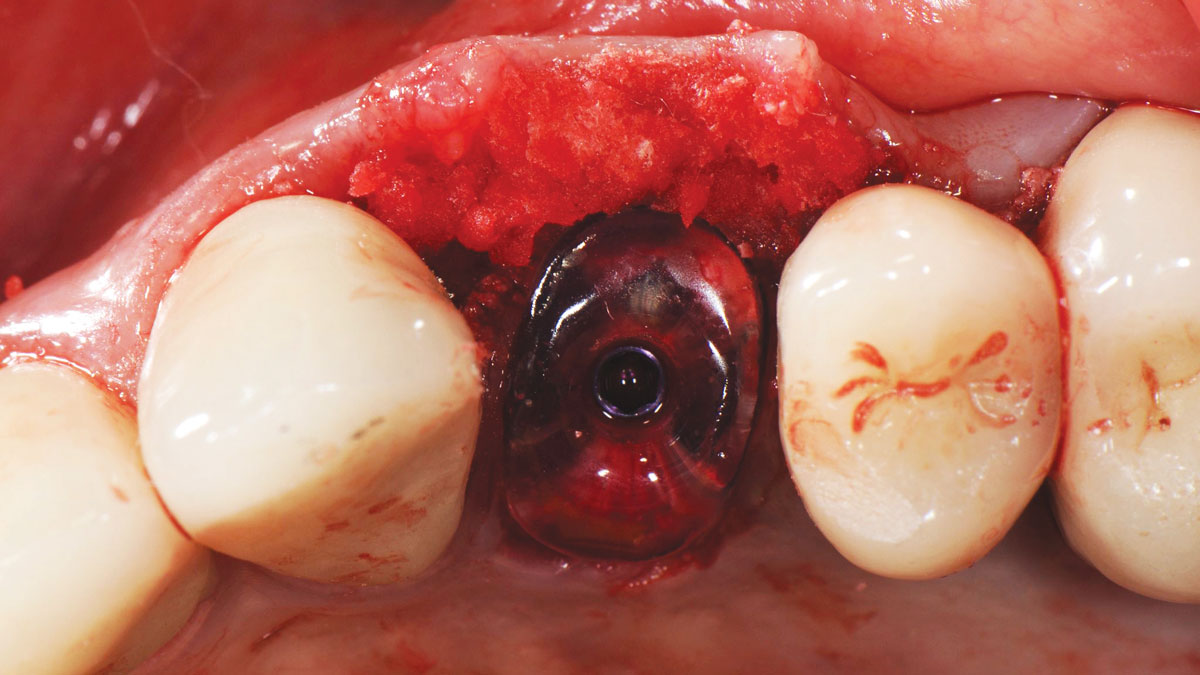
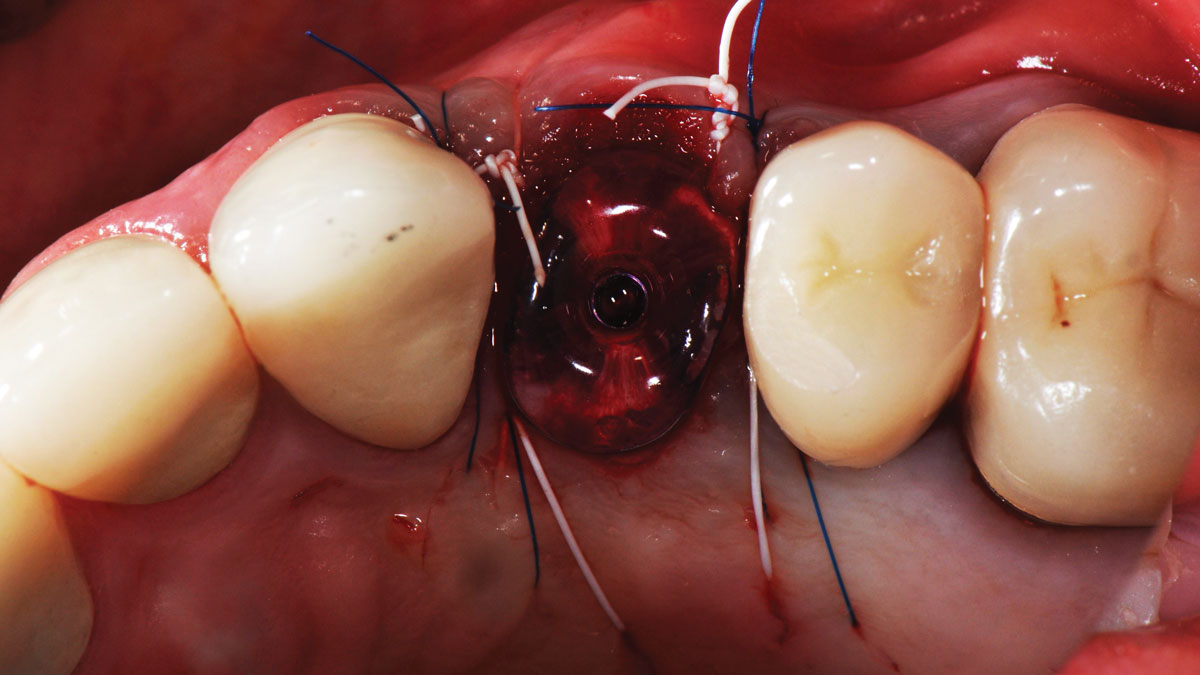
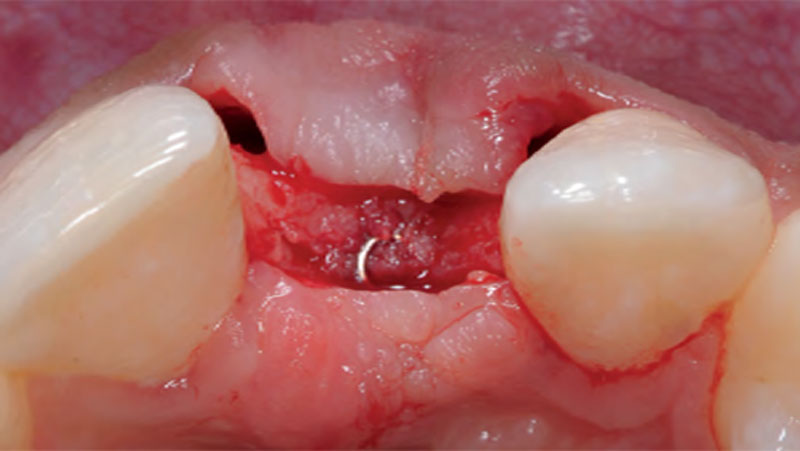
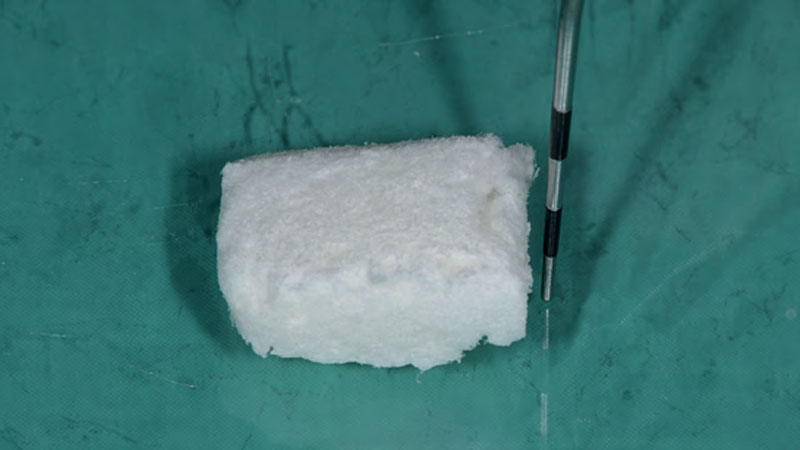
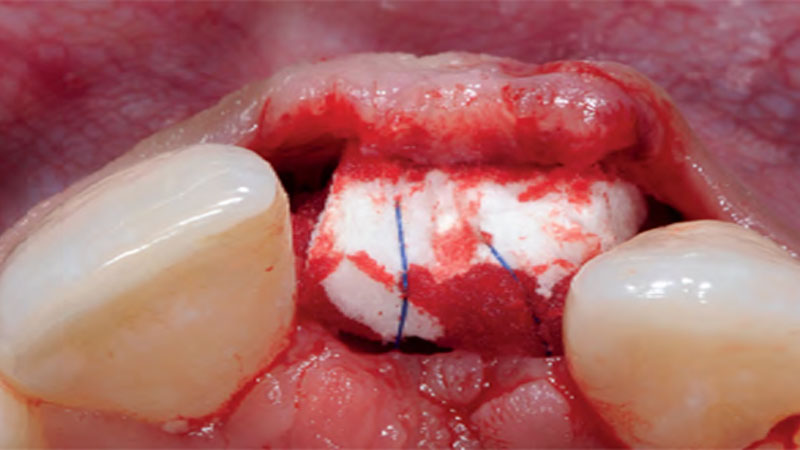
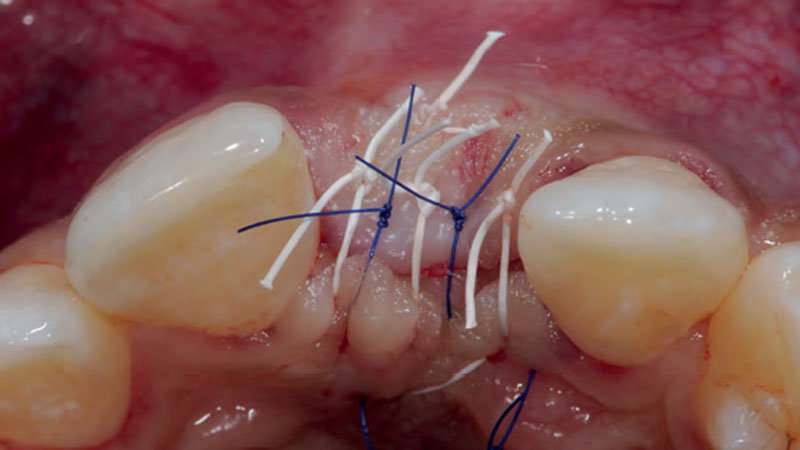
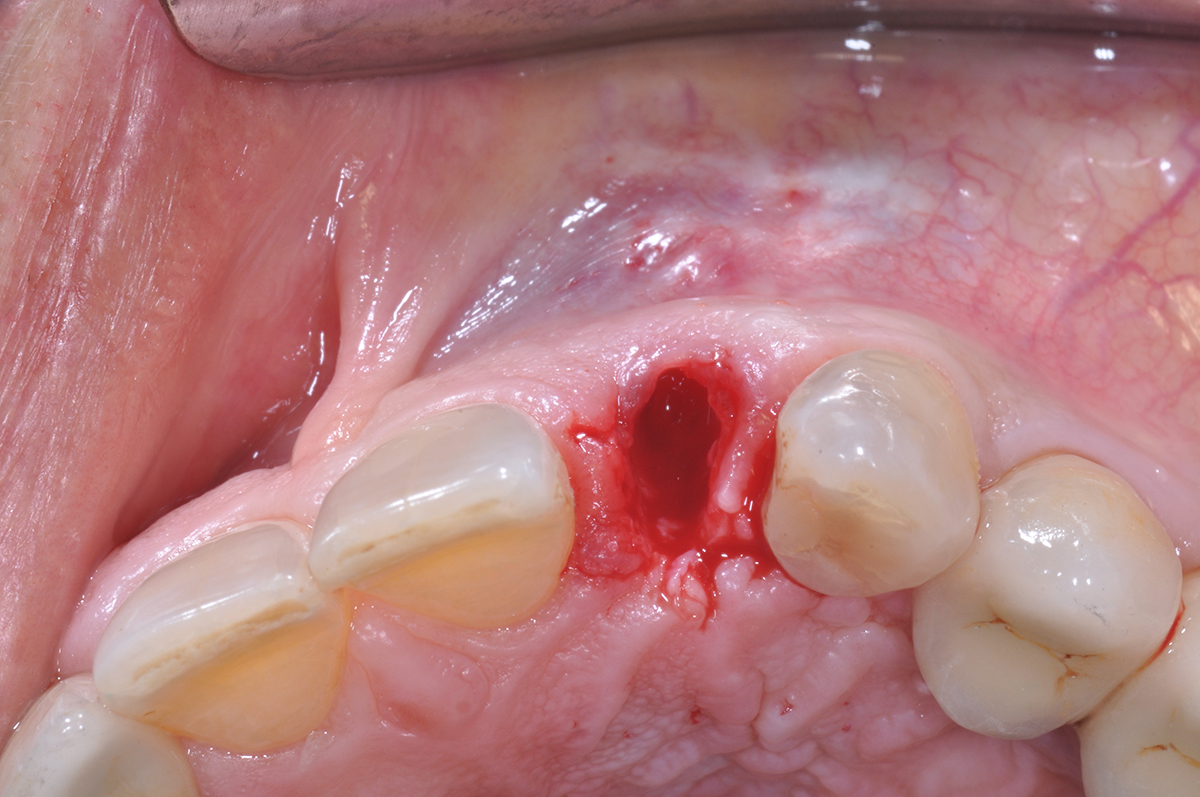
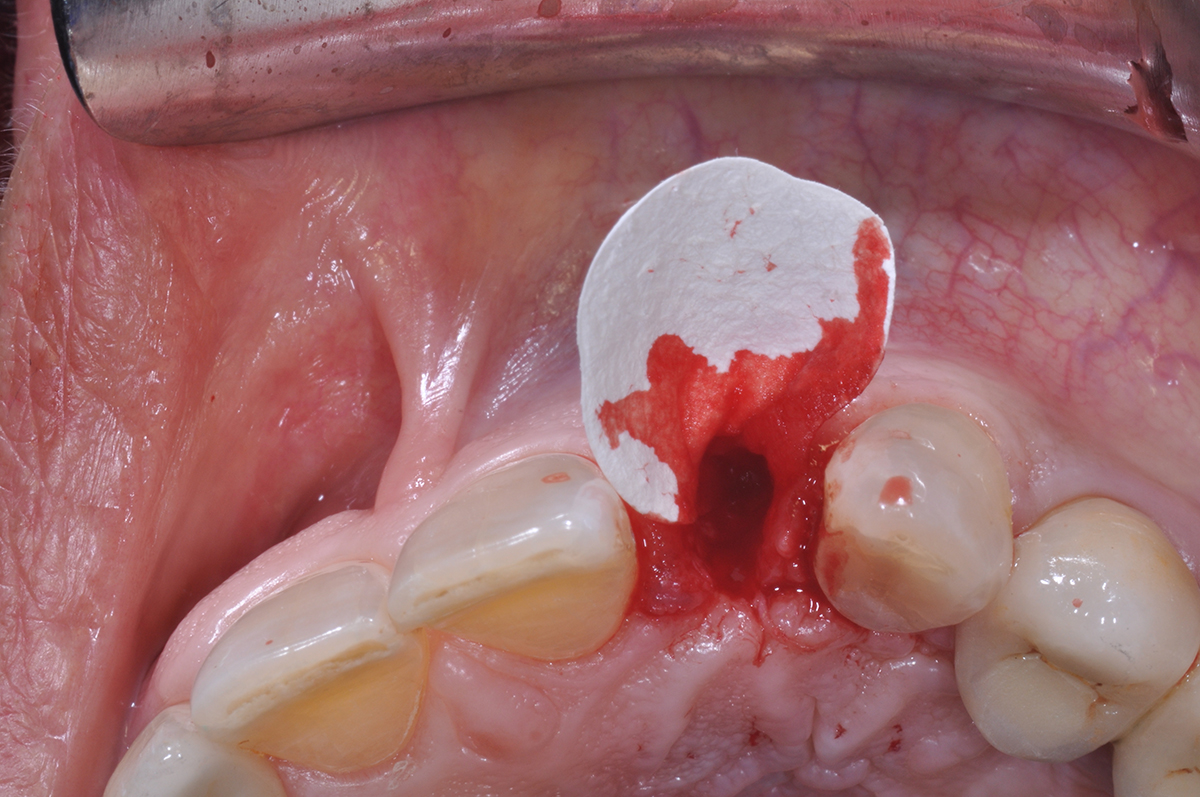
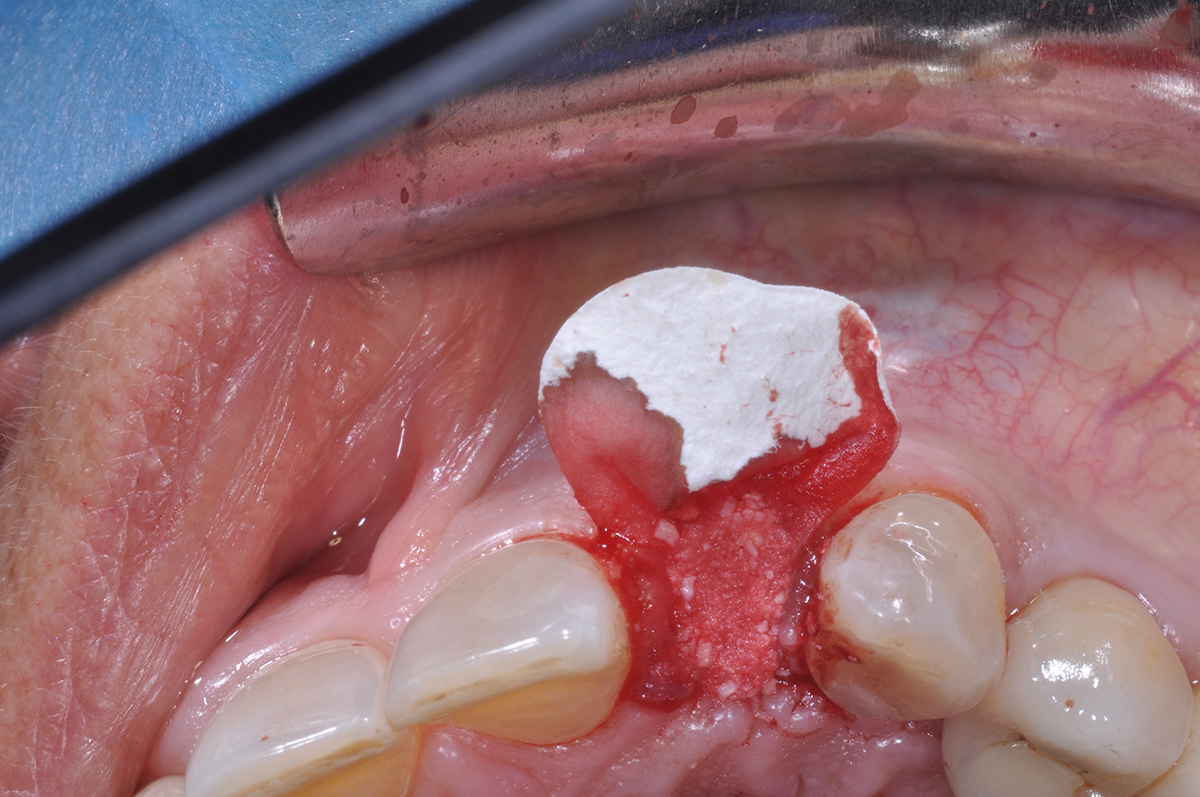
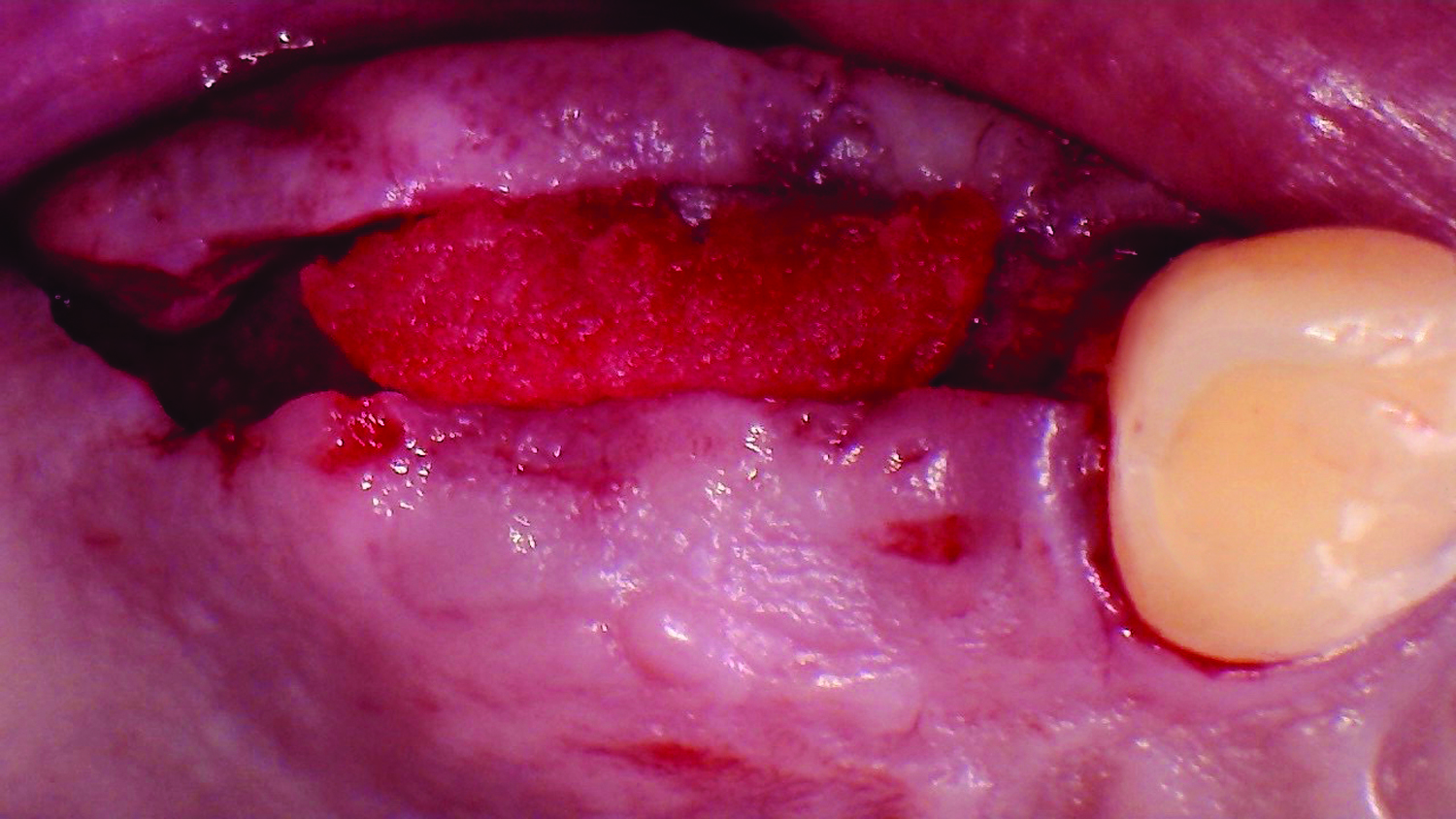
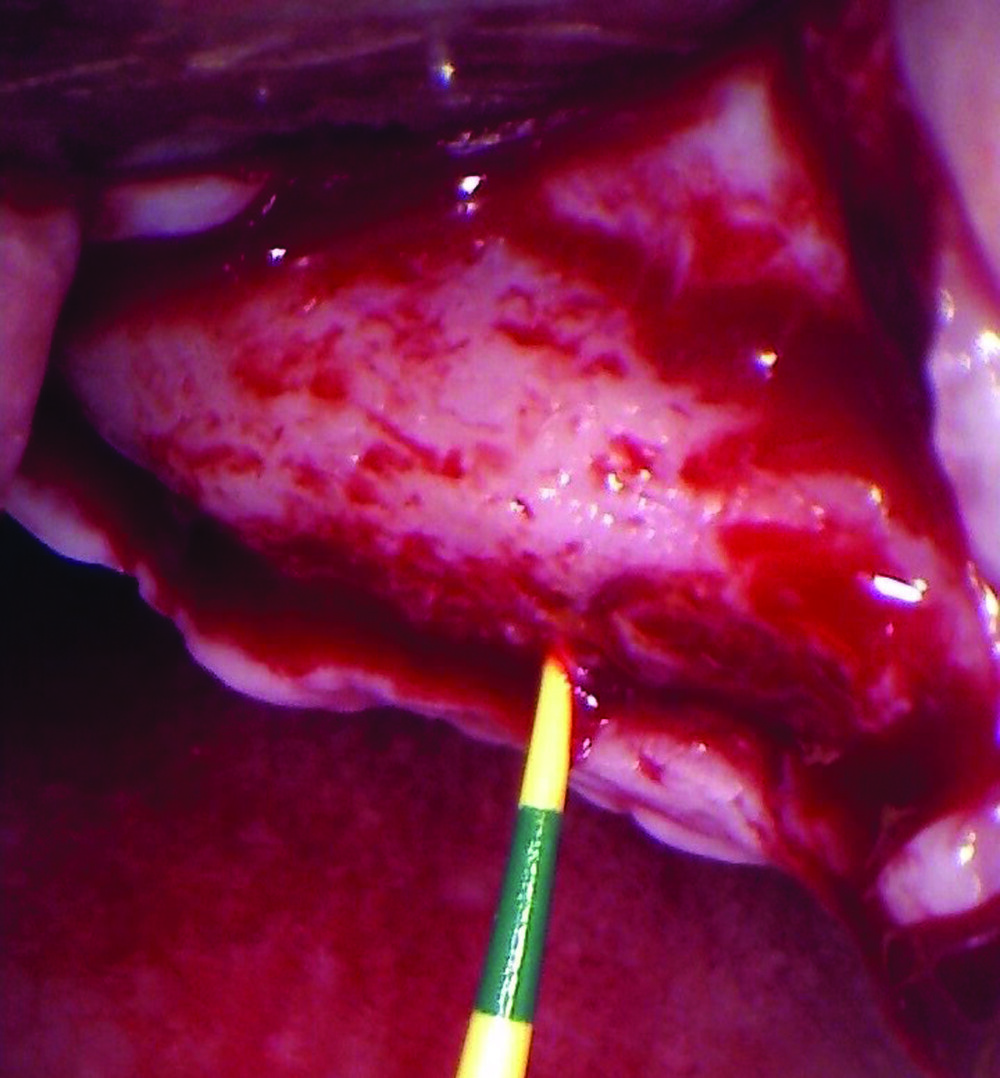
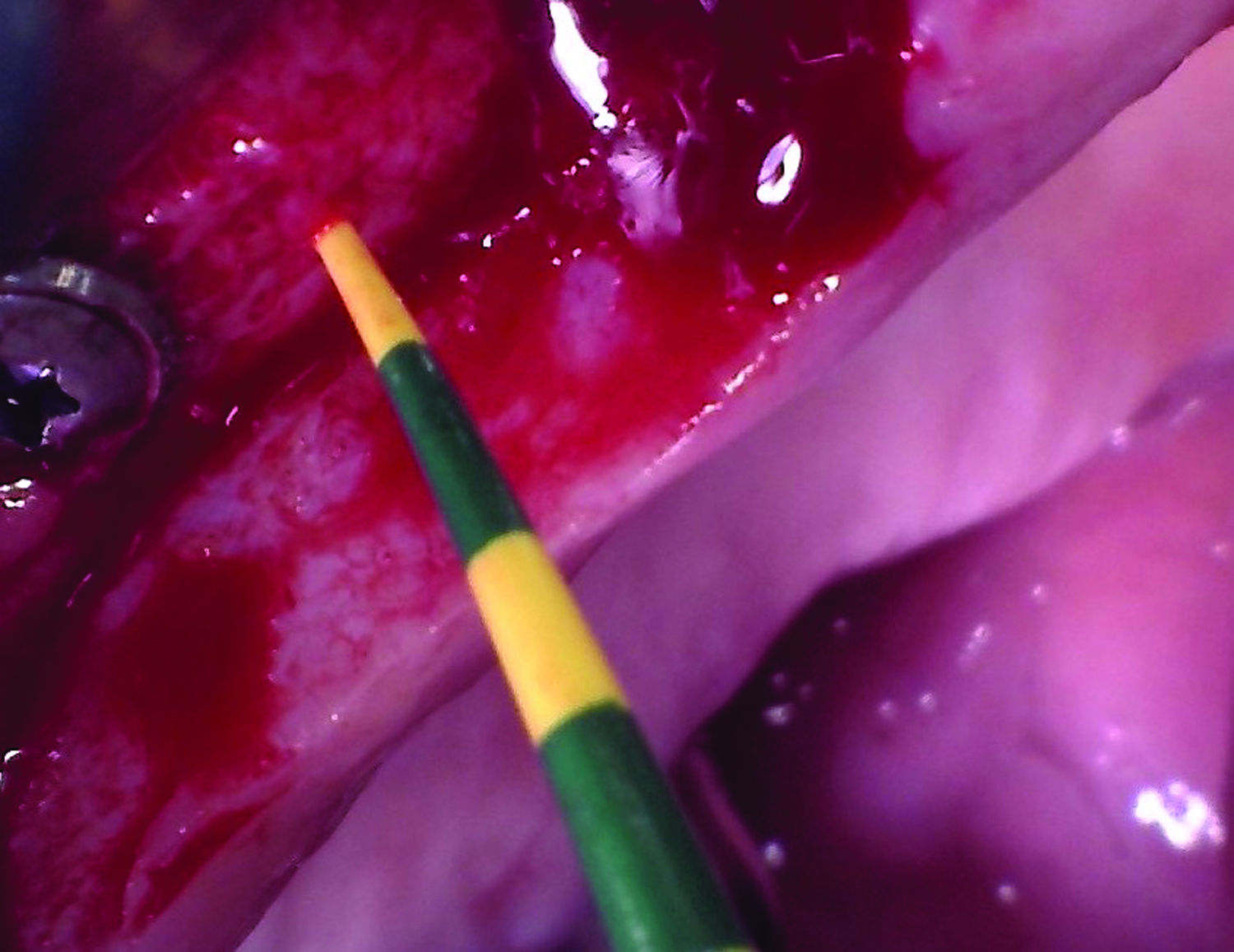
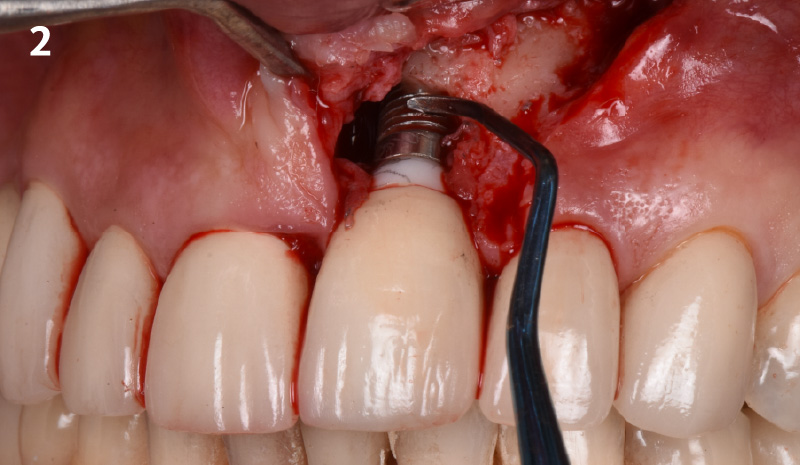
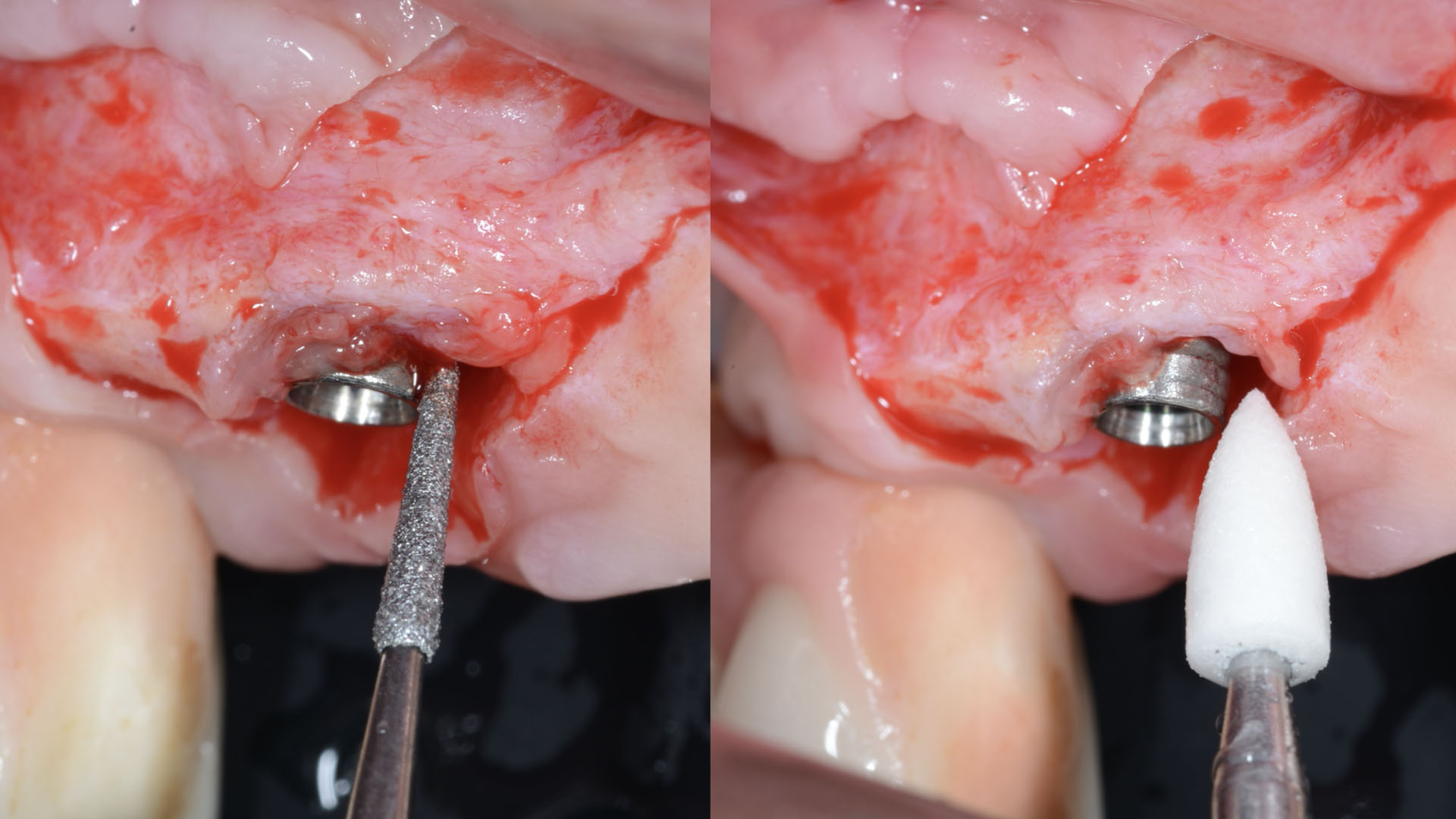
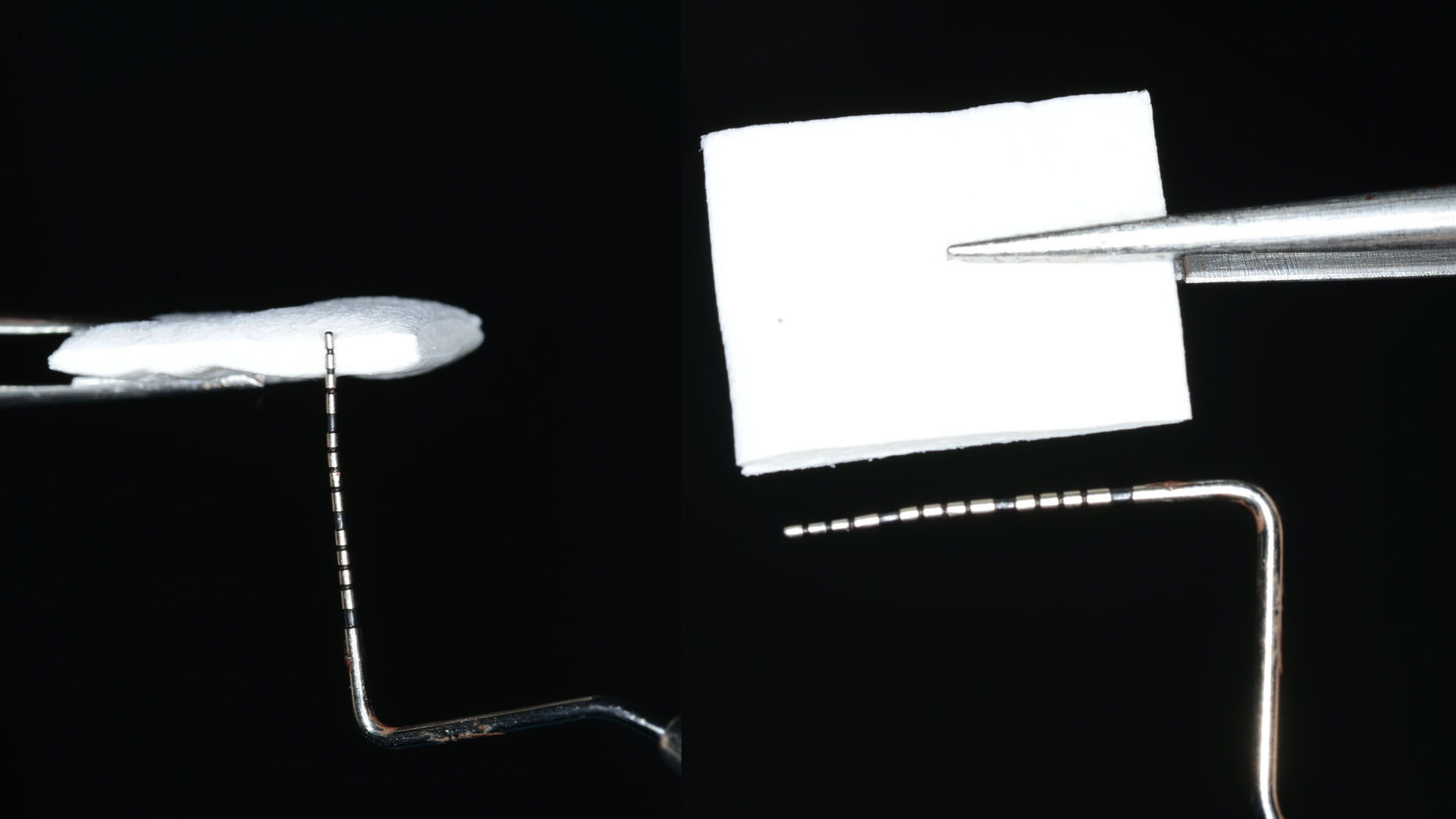
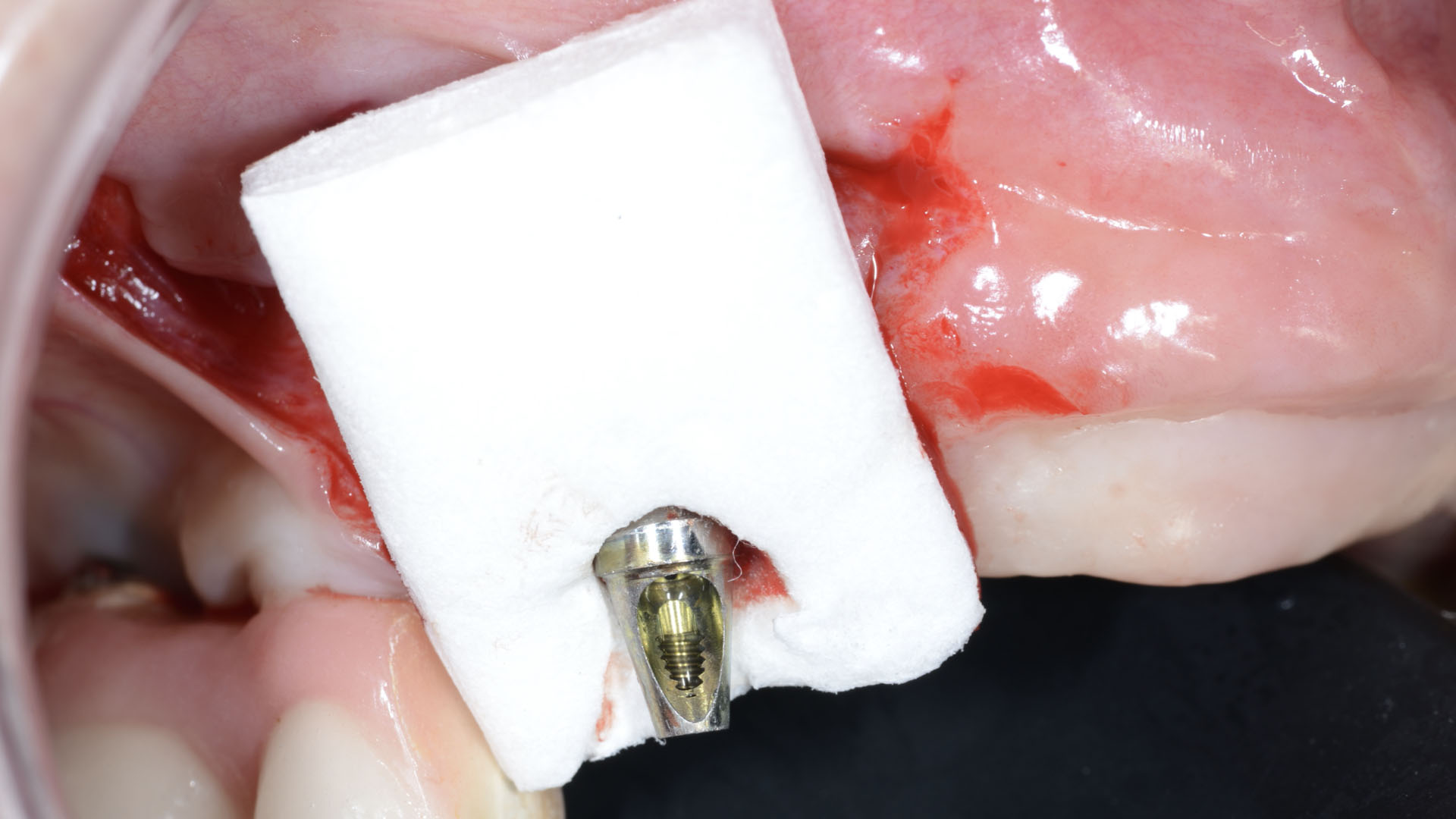
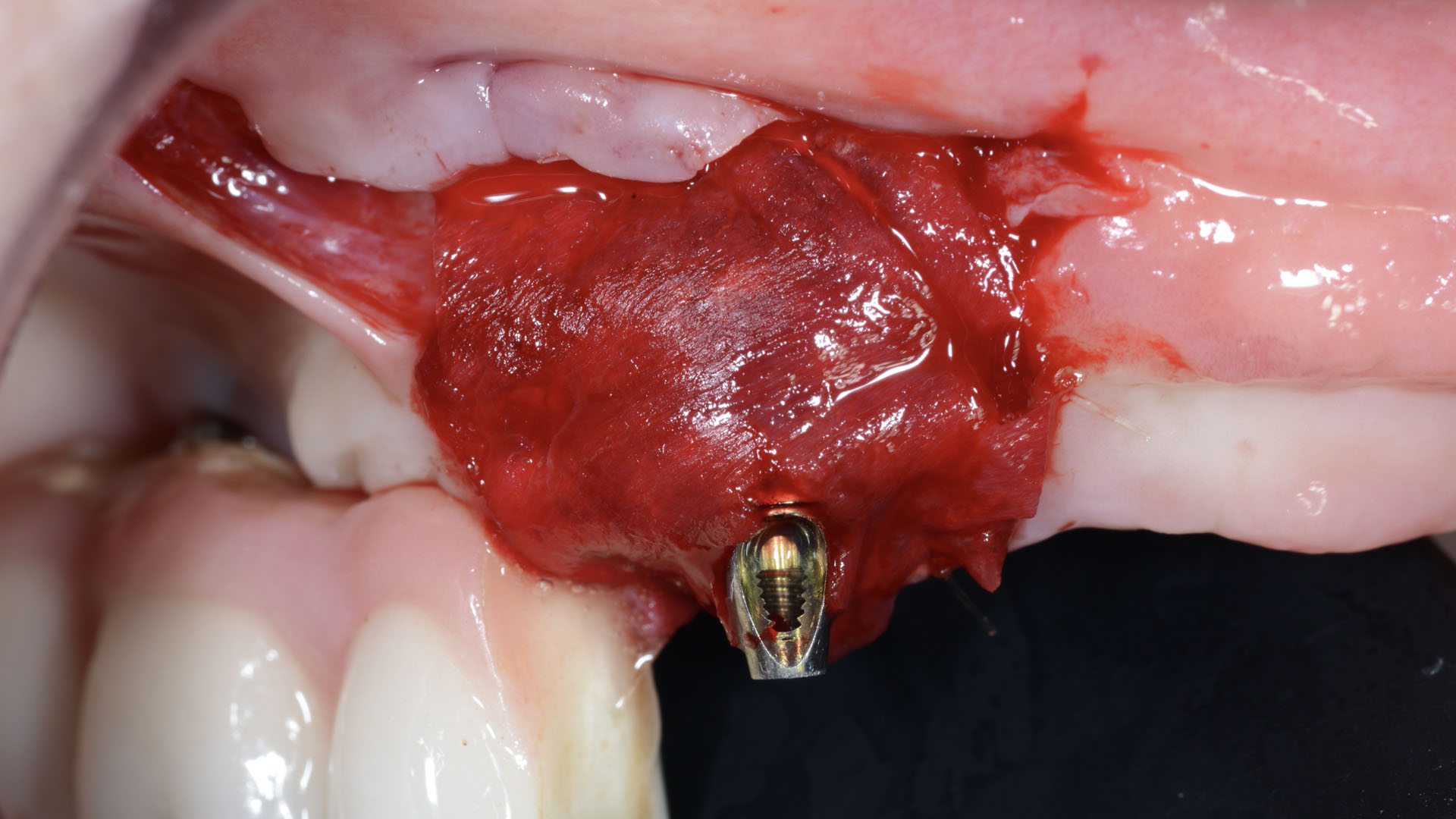
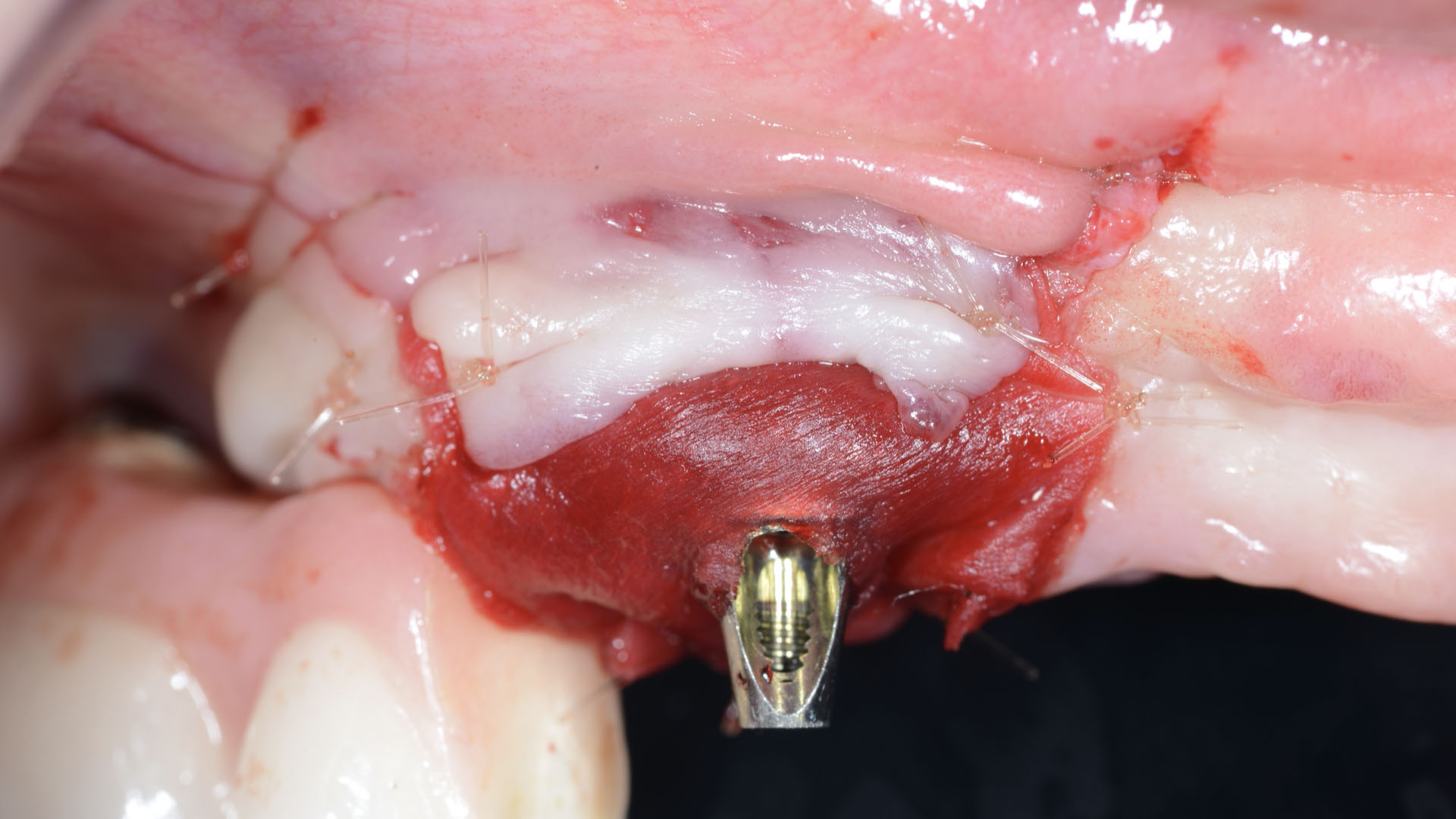
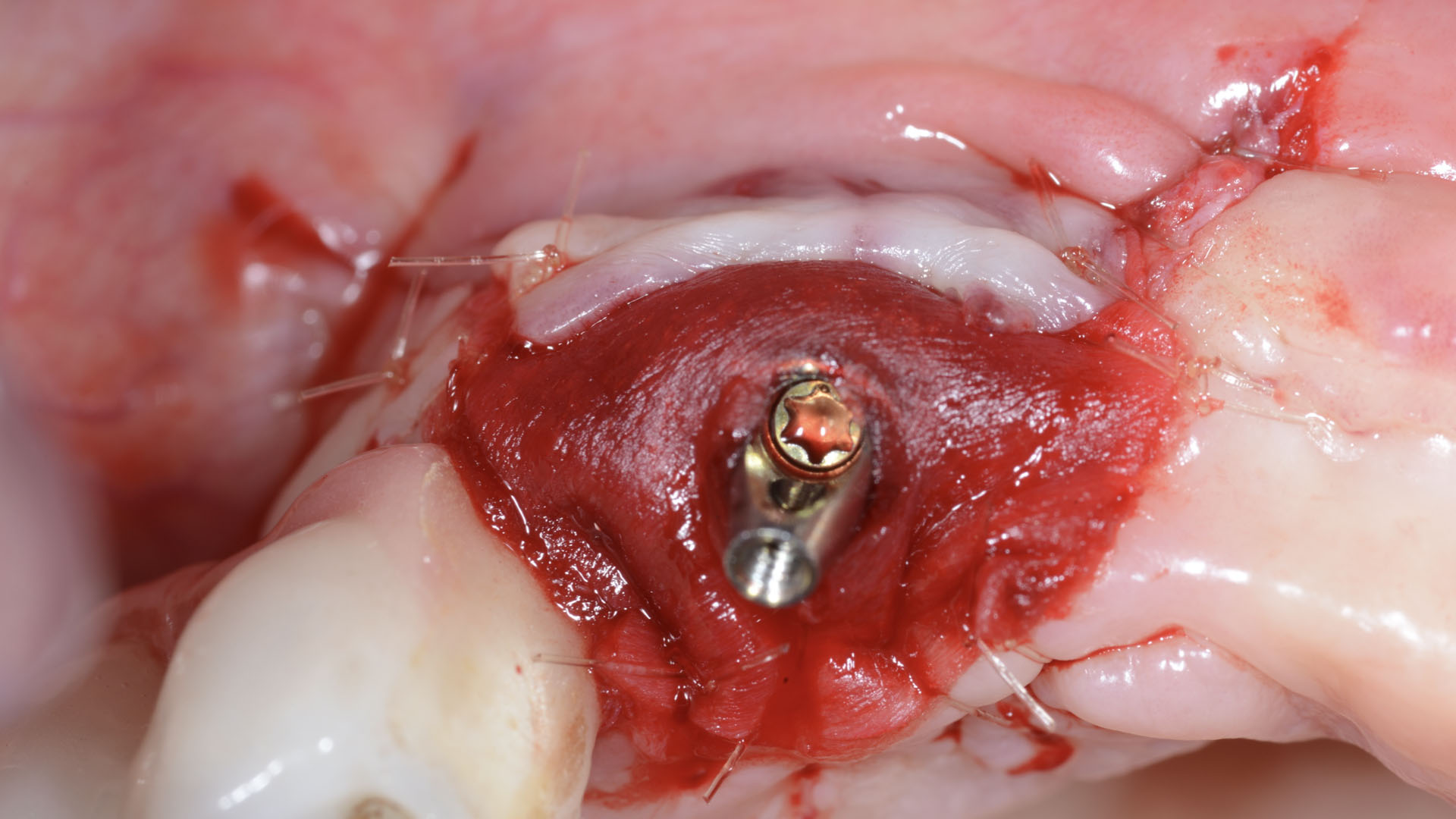
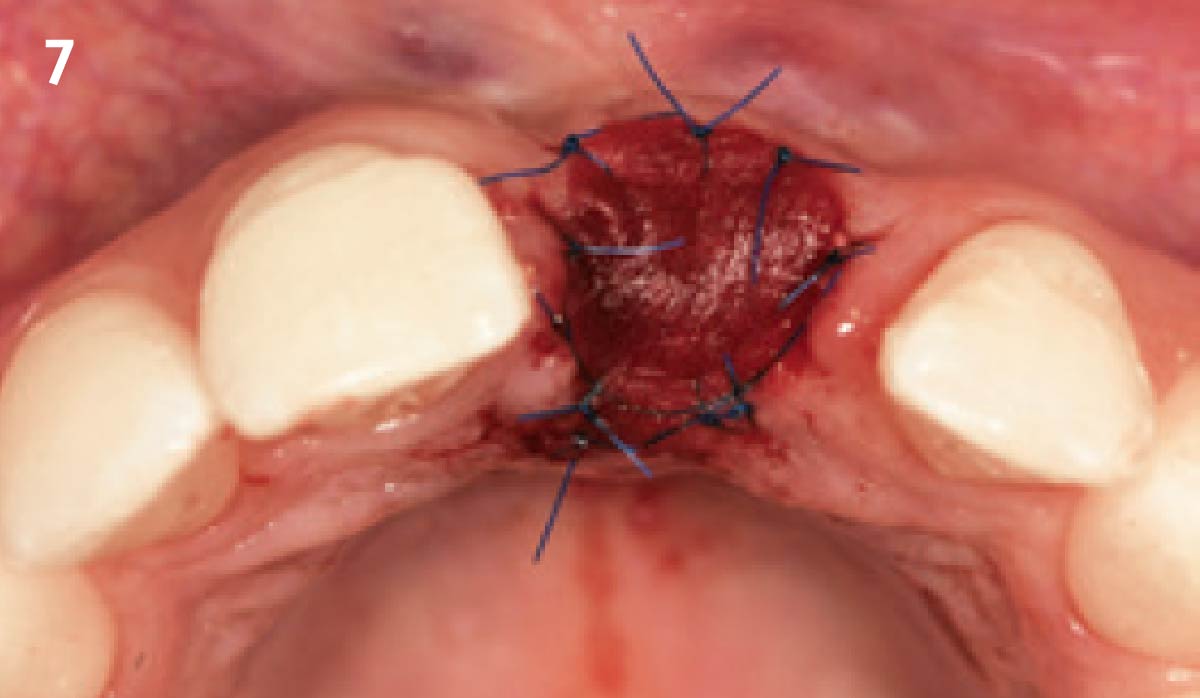
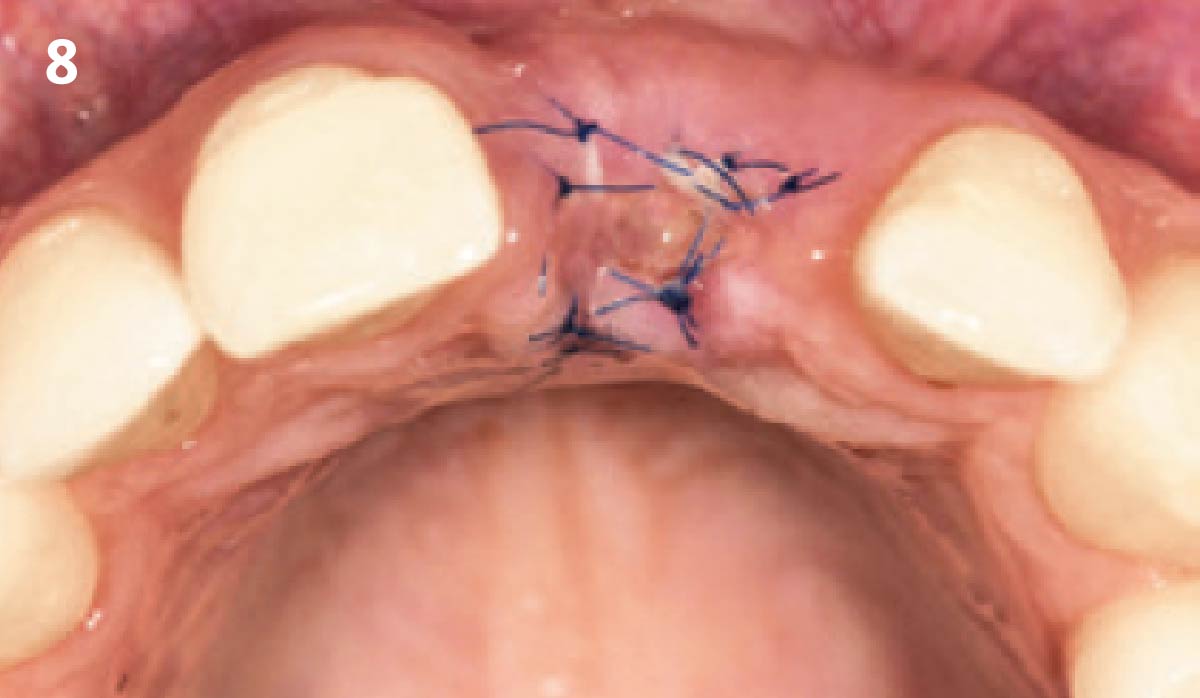
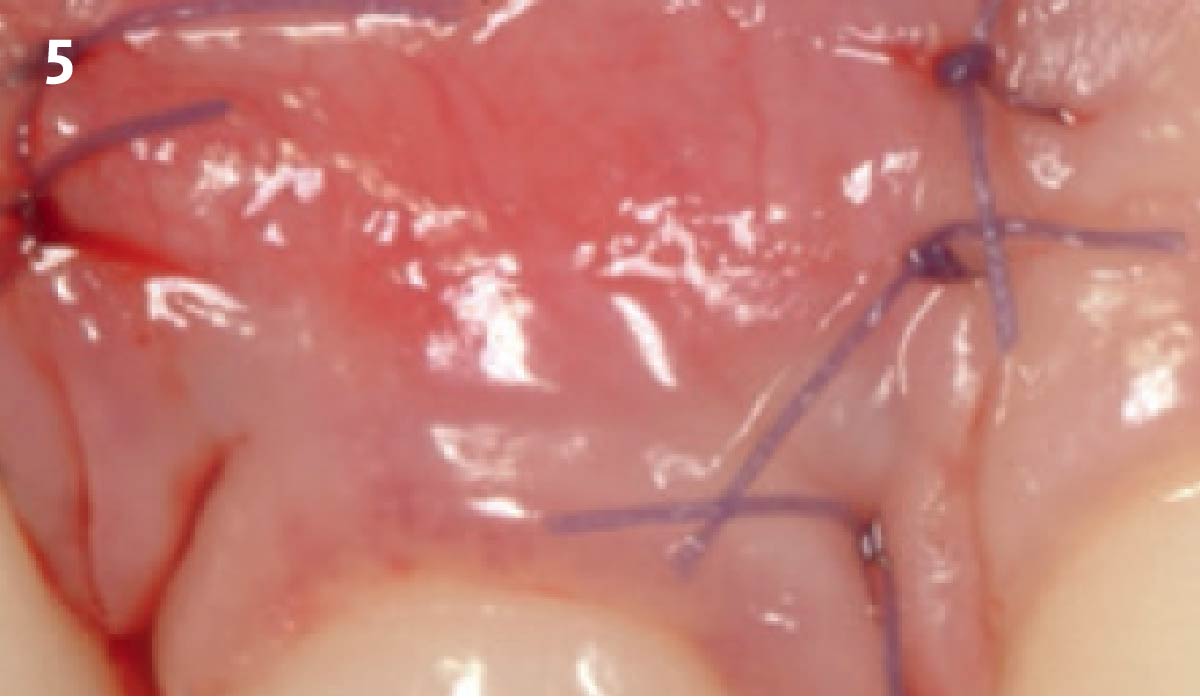
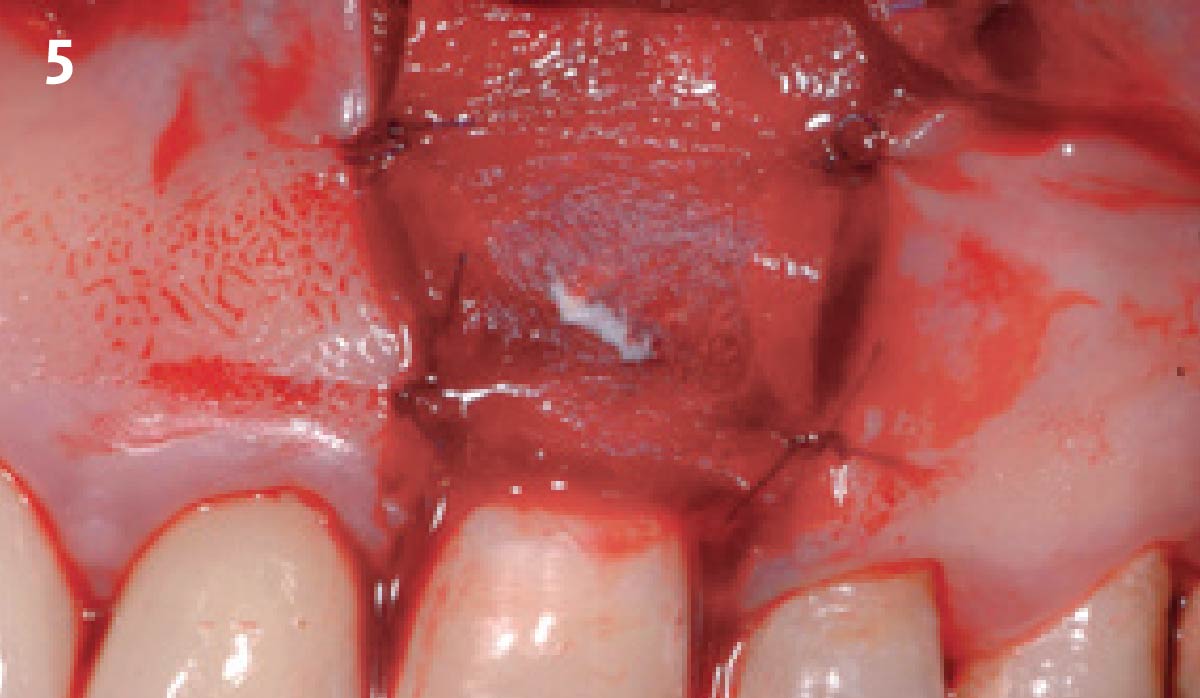
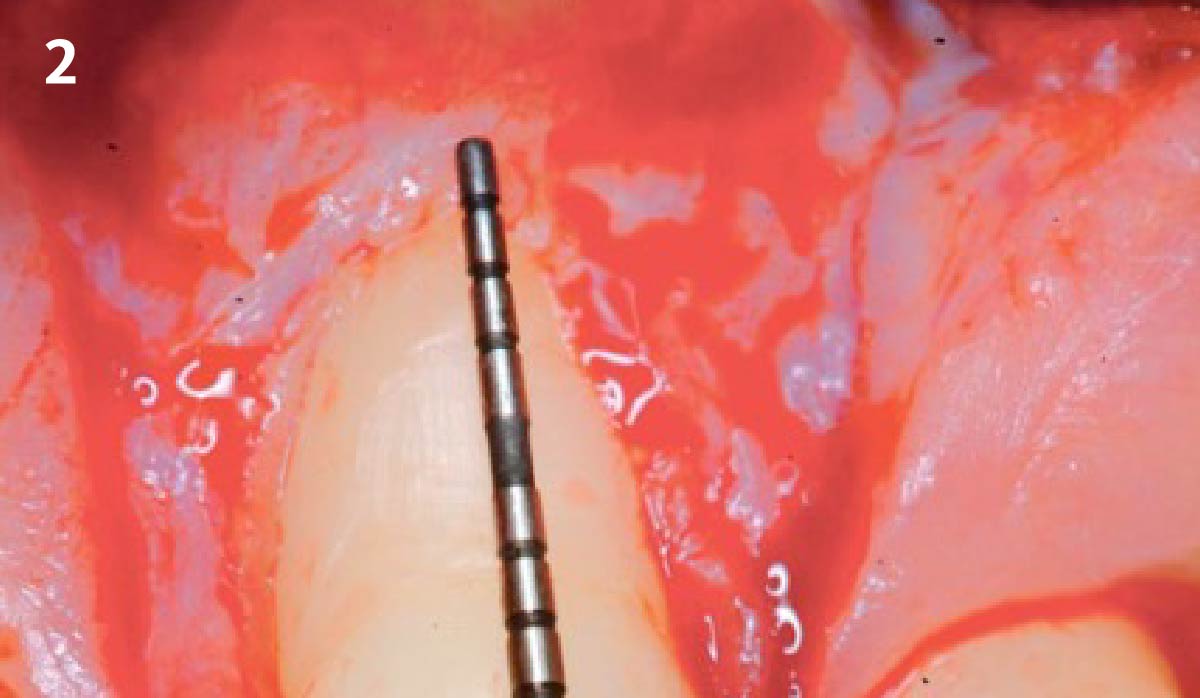
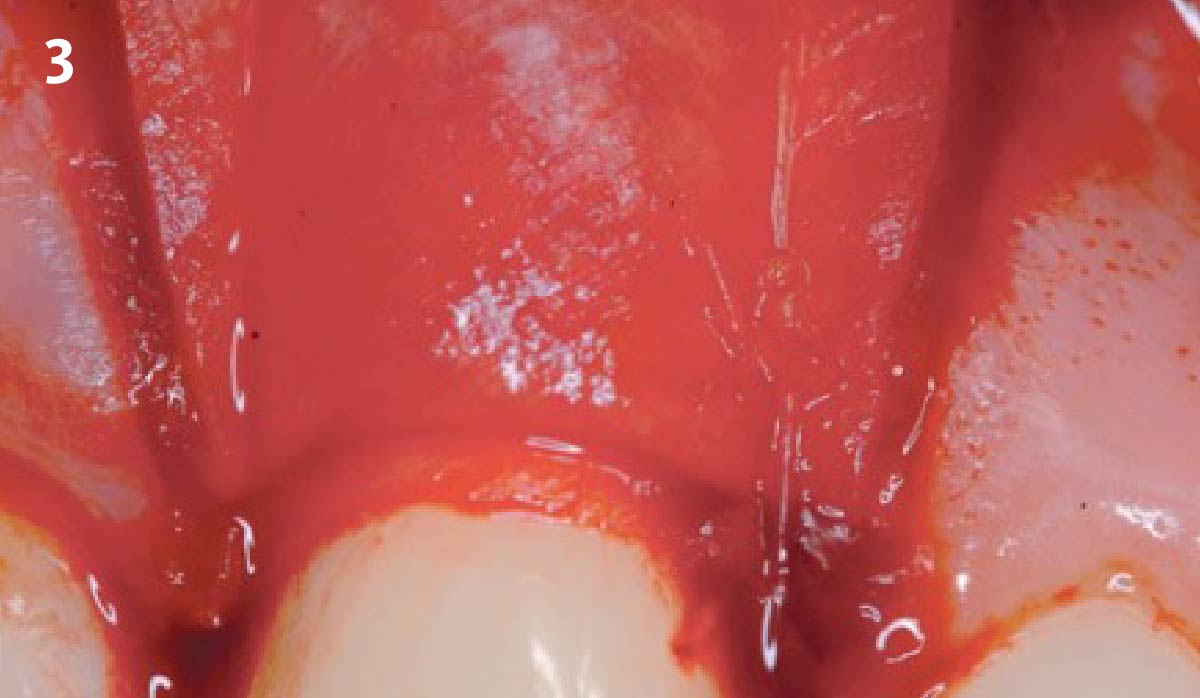
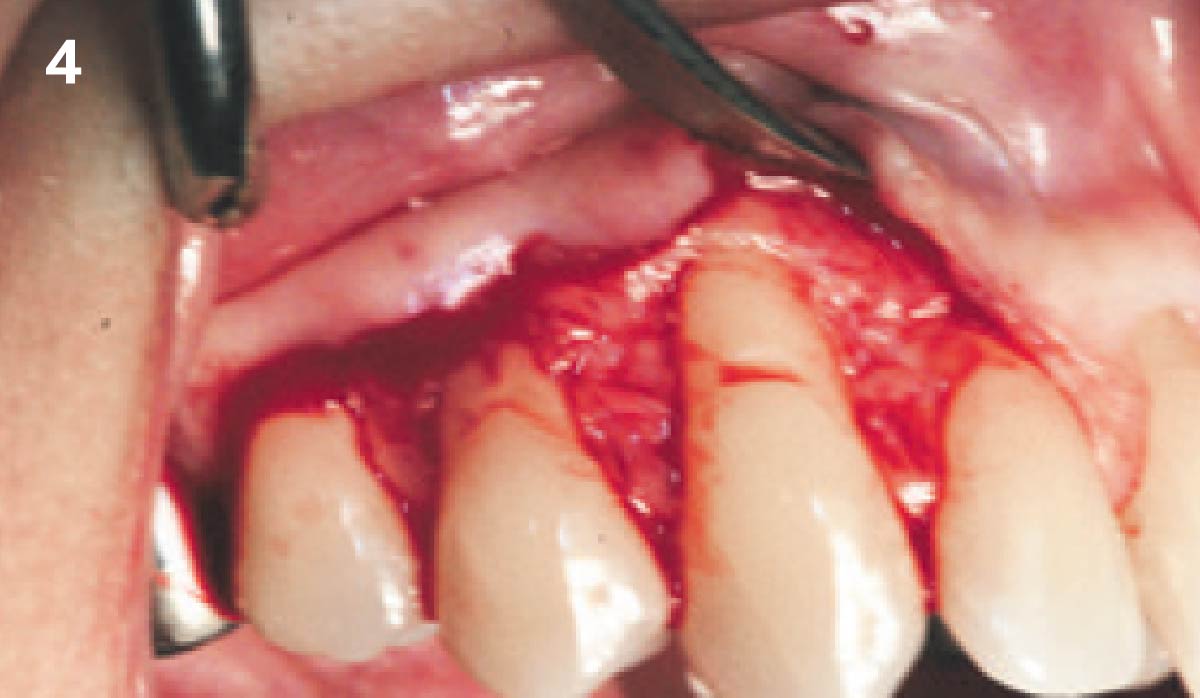
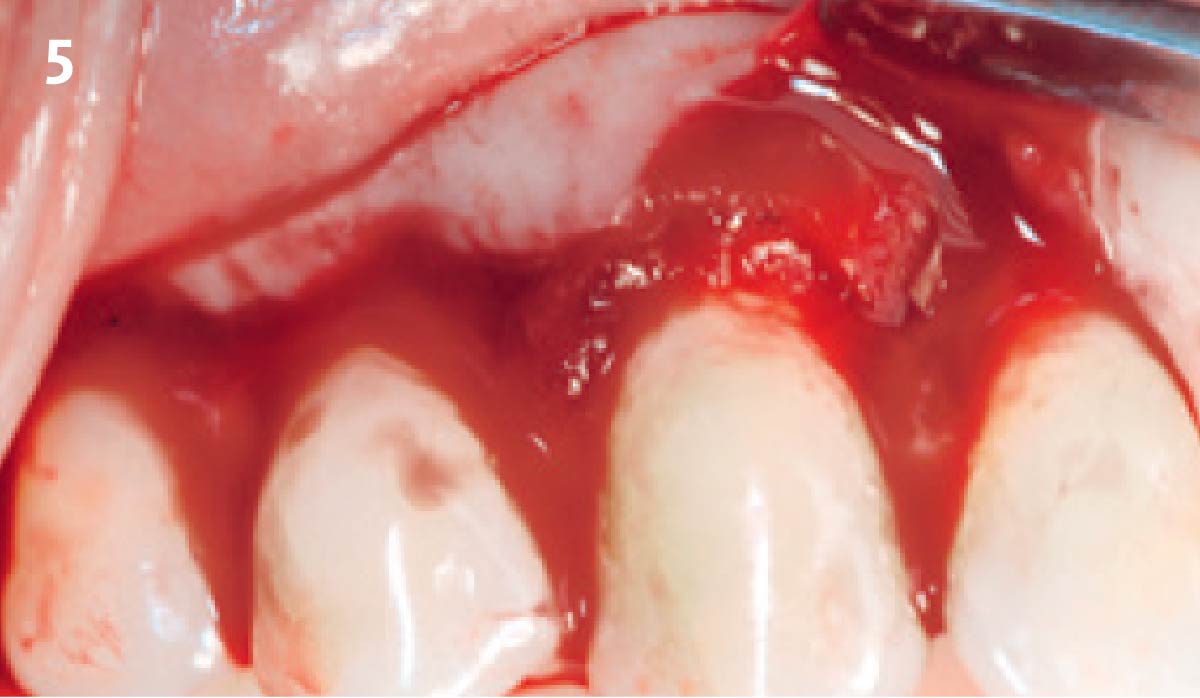
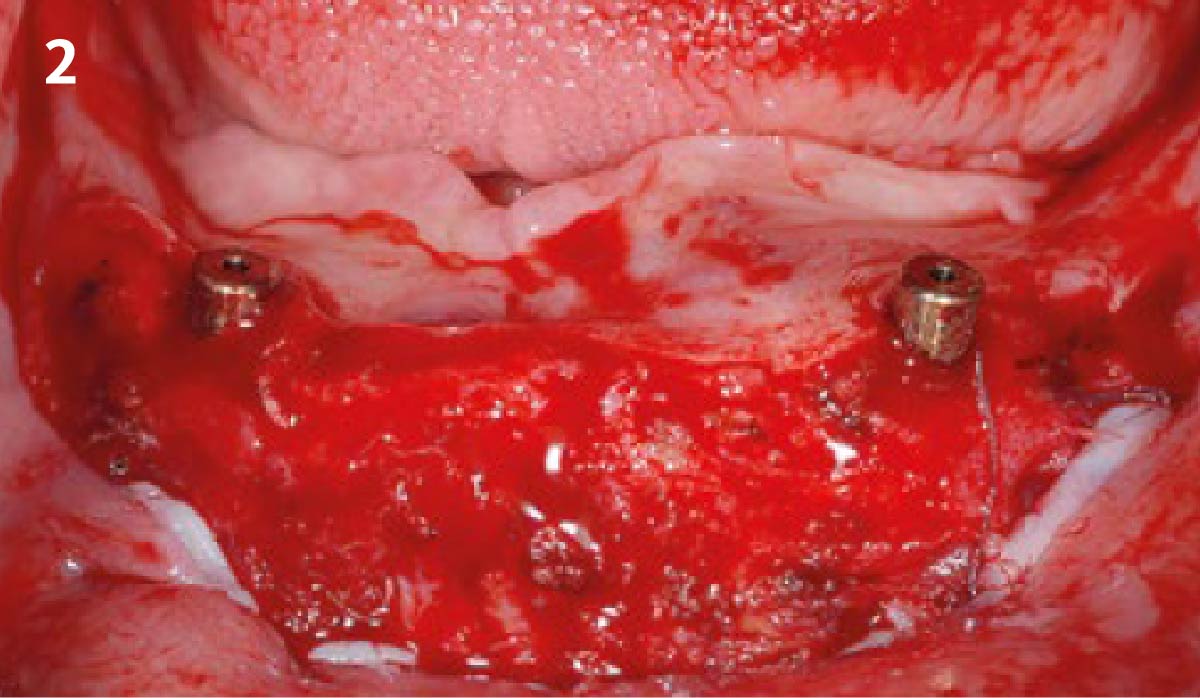
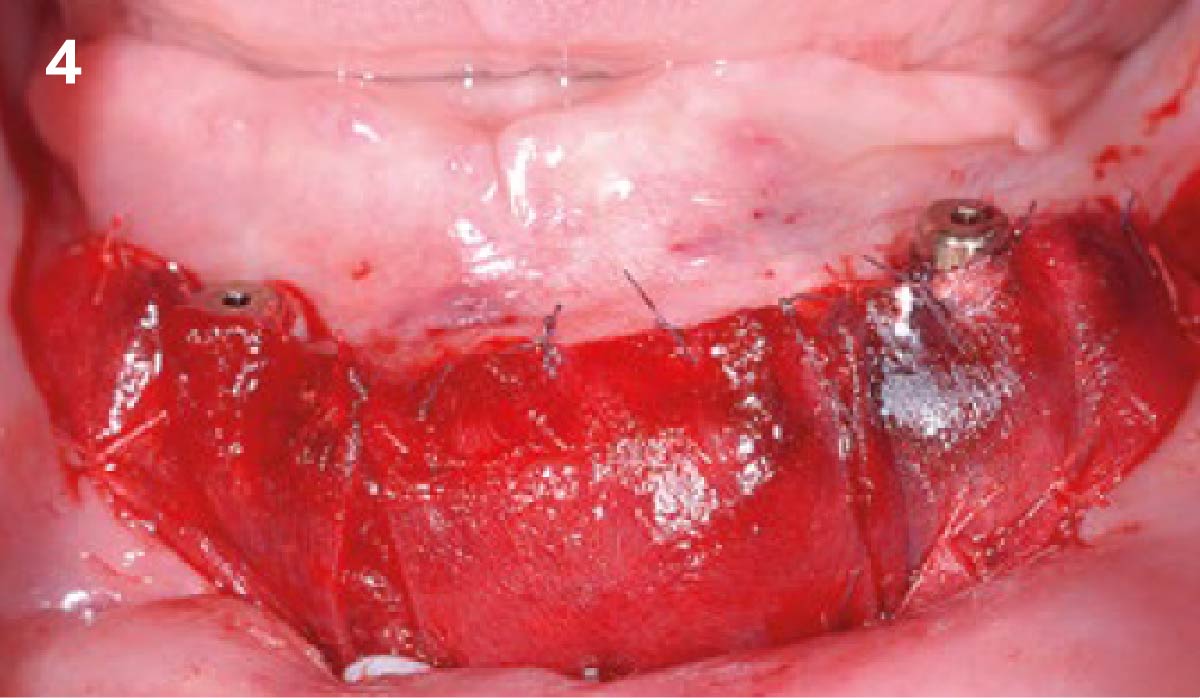
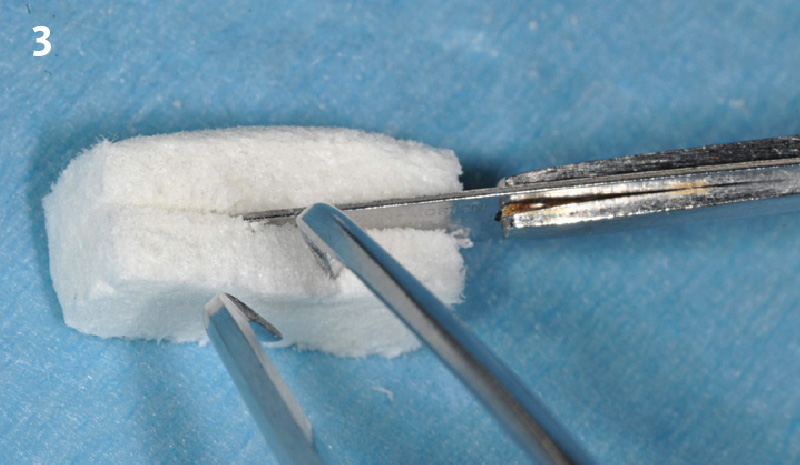
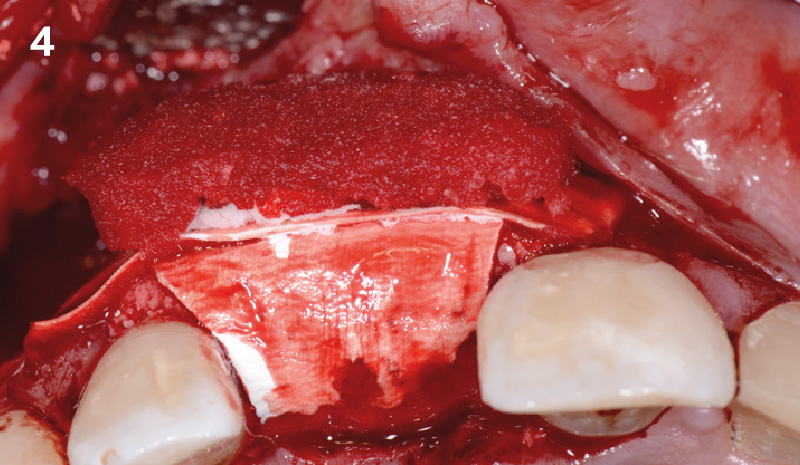
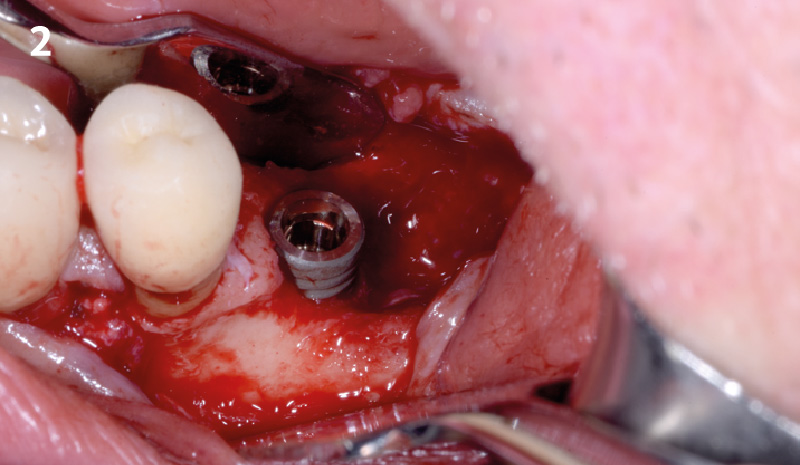
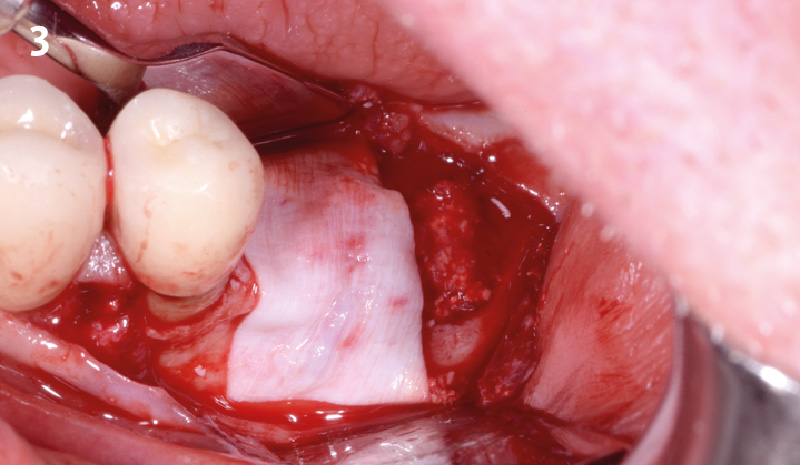
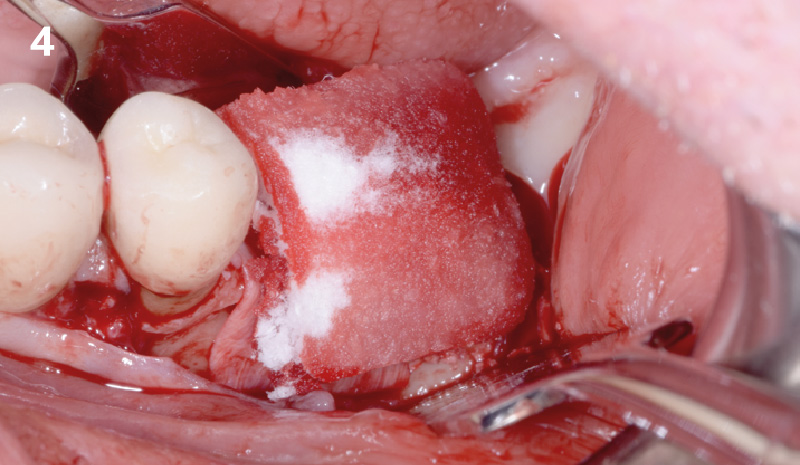
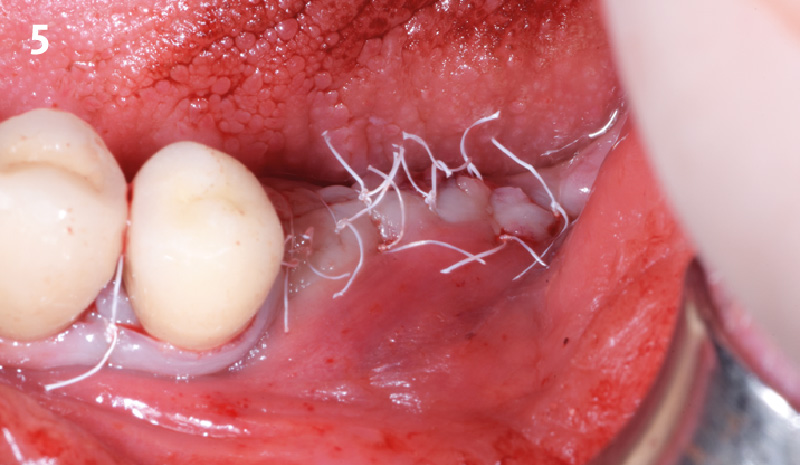
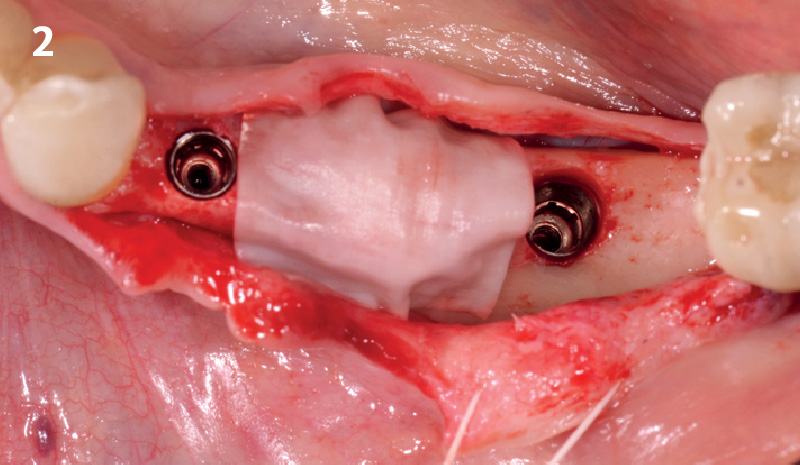
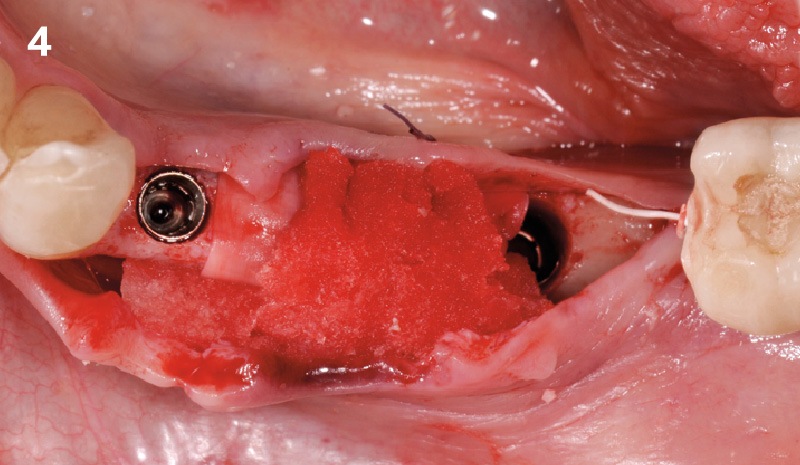
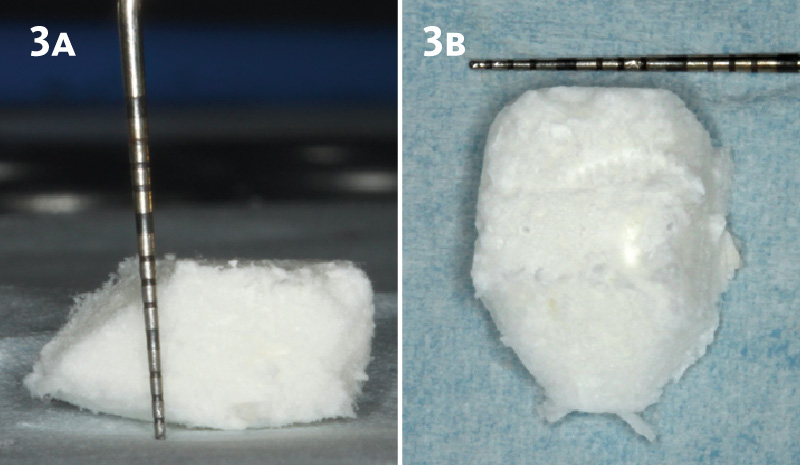
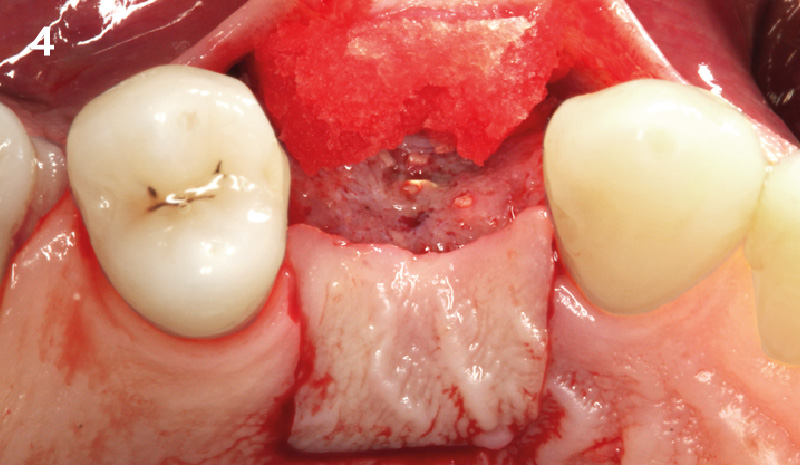
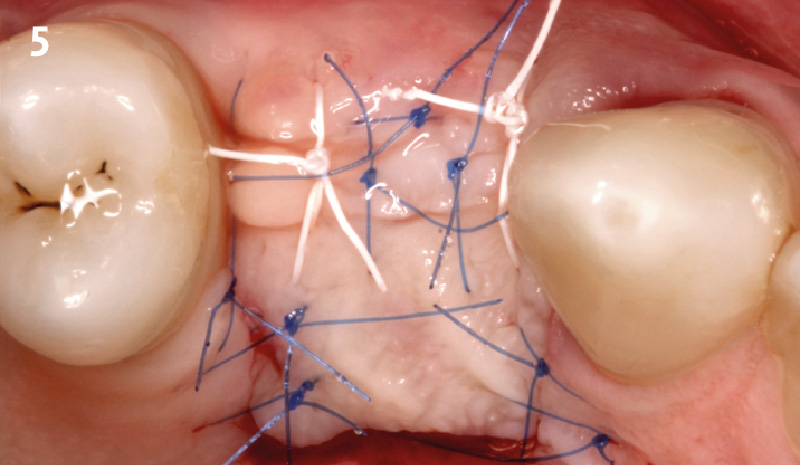
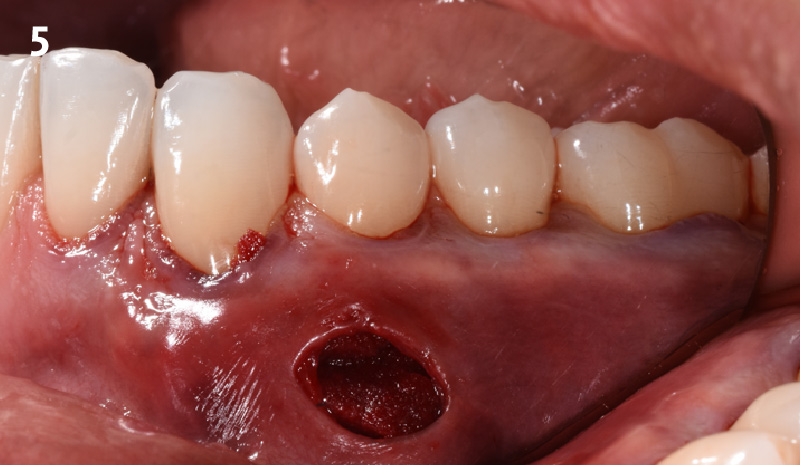
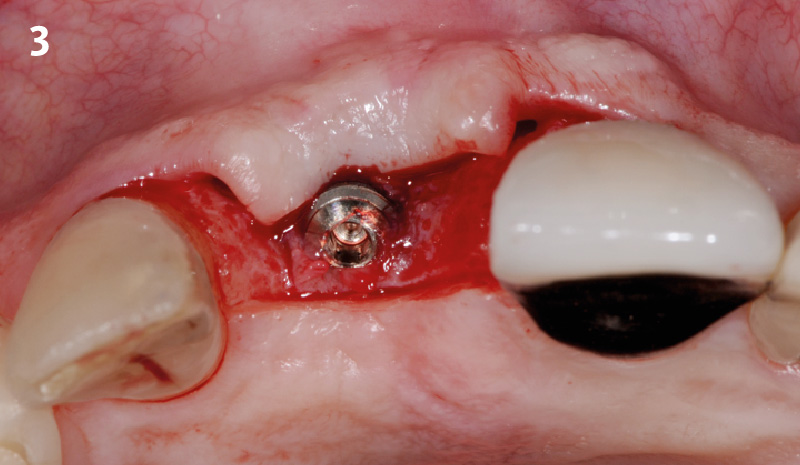
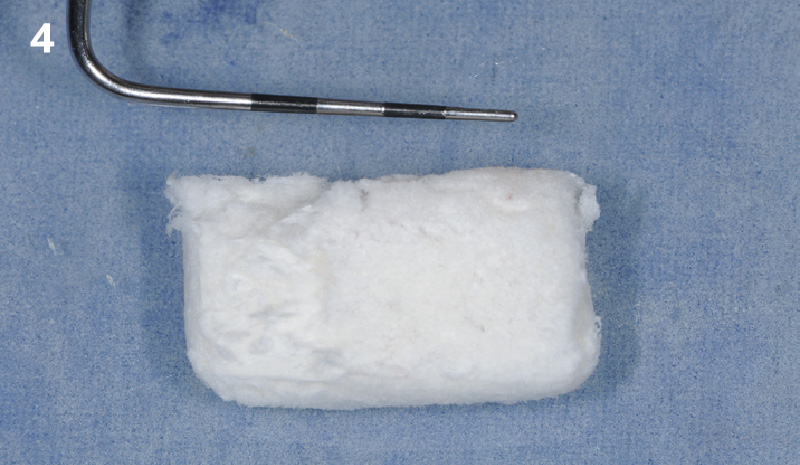
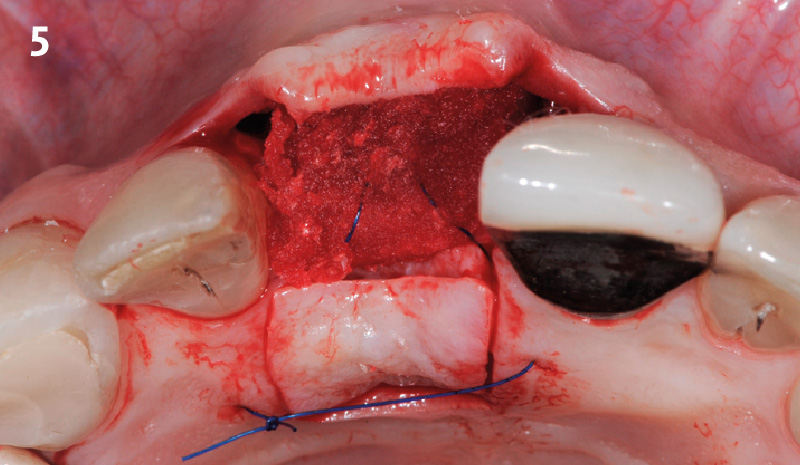
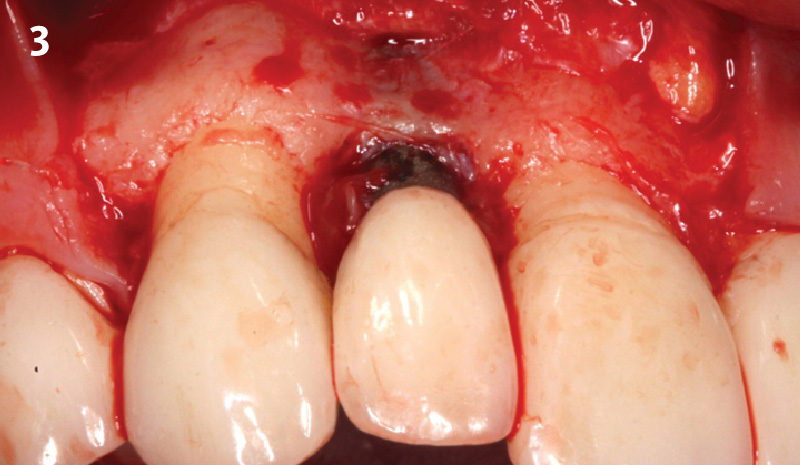
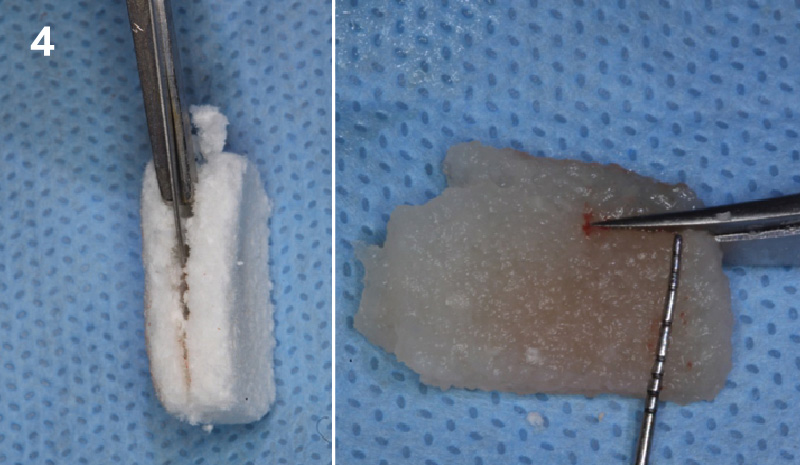
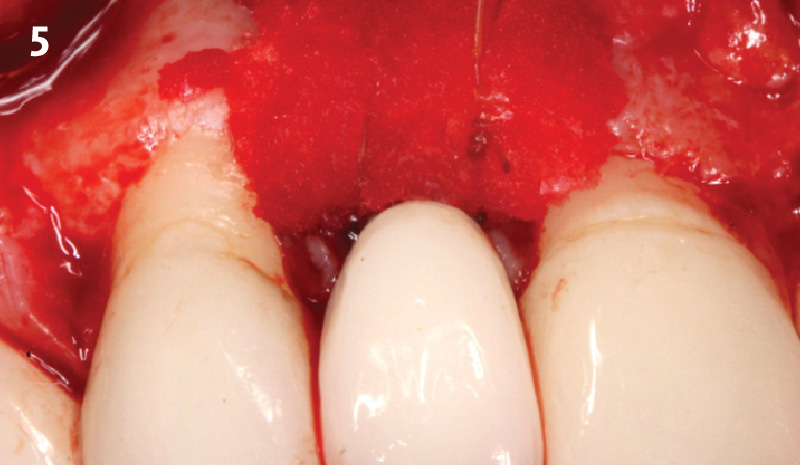
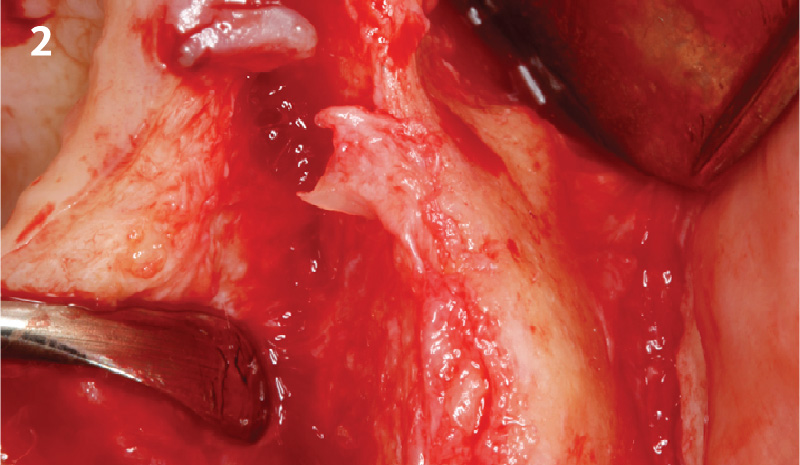
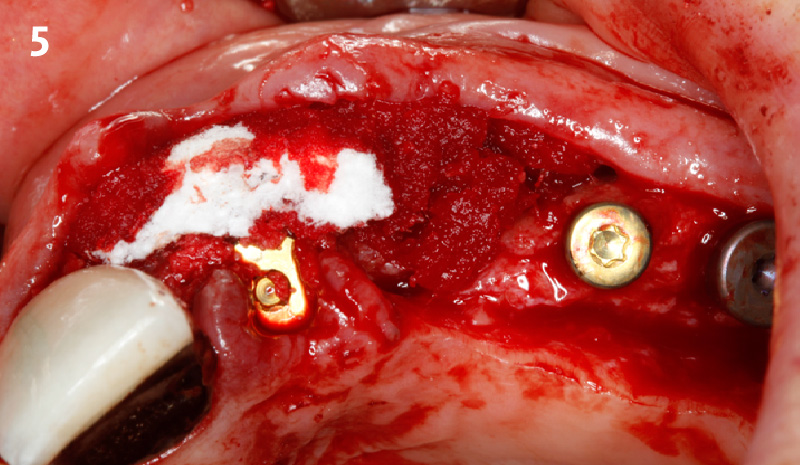
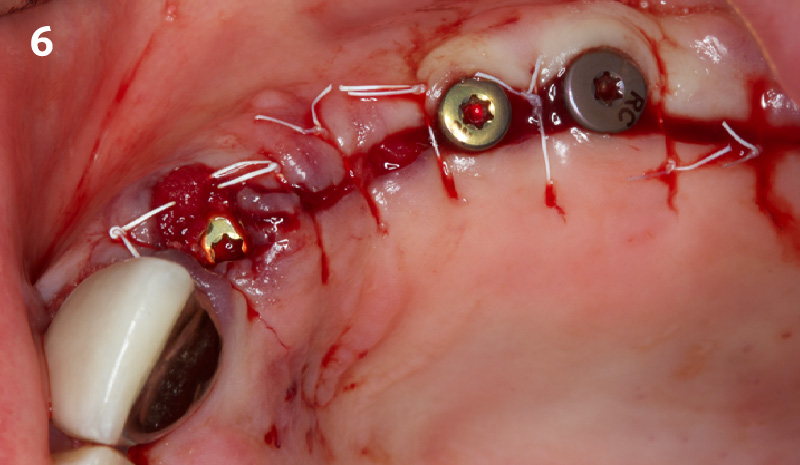
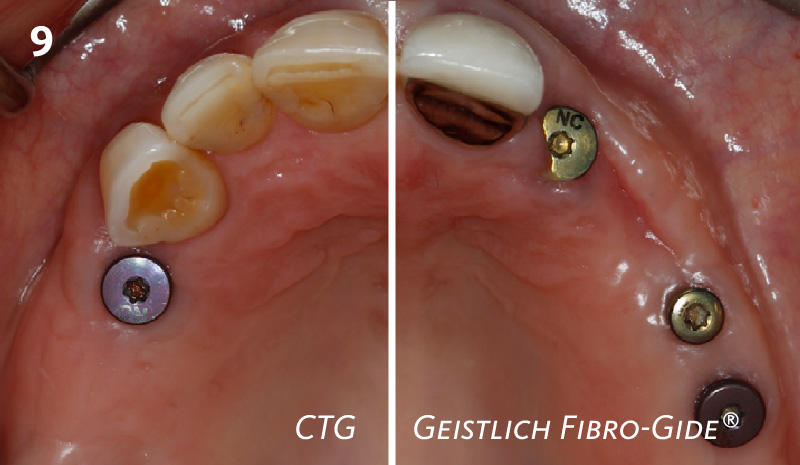
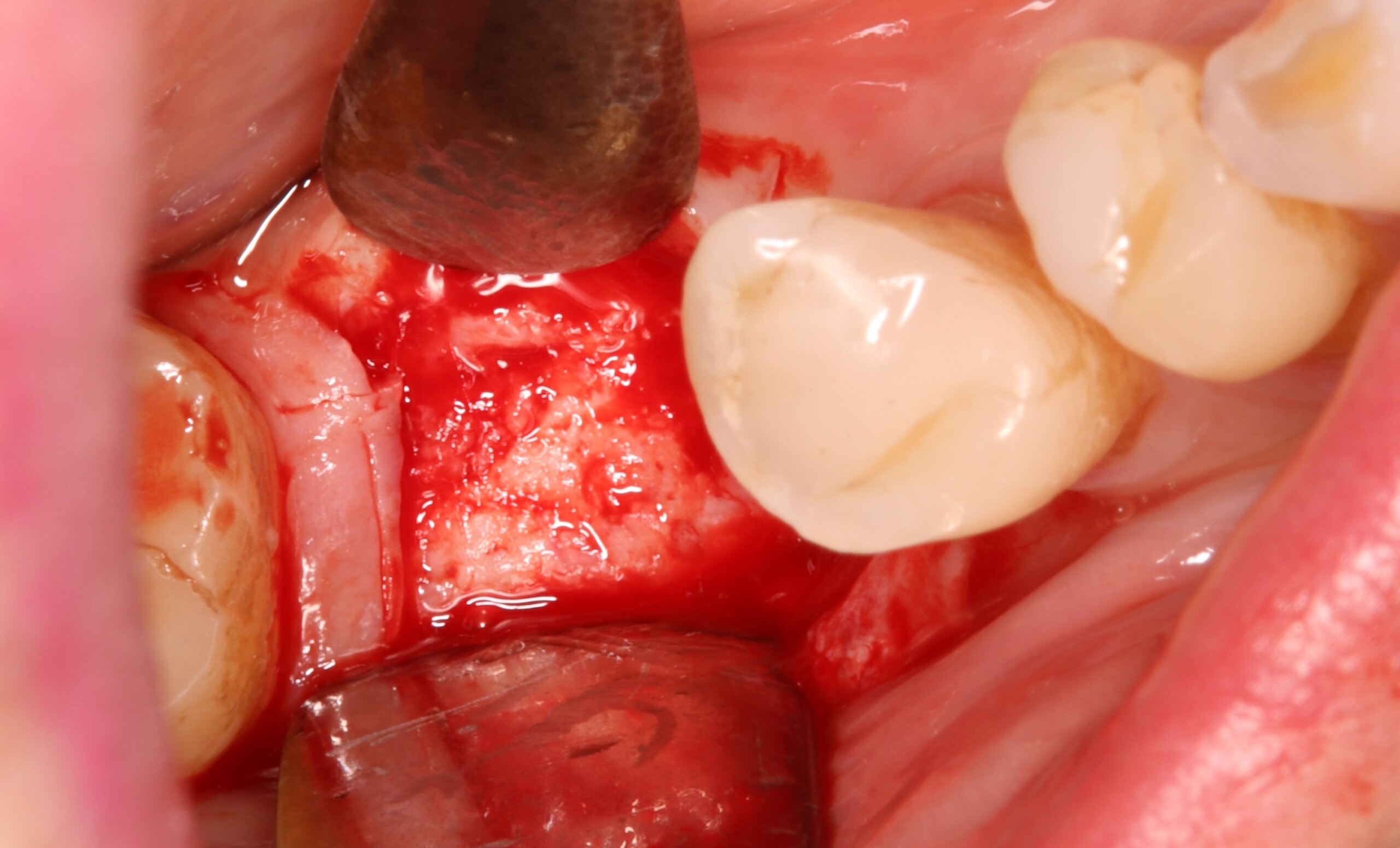
A successful treatment outcome comes with proper selection of the technique and materials. In order to facilitate an implant supported restoration in the site with > 13mm mesio-distal space, a staged approach was selected, with alveolar ridge preservation (ARP) performed using an atraumatic extraction technique and vallos® mineralized cortico-cancellous bone allograft chosen as the material.
“Ensuring atraumatic extraction techniques, regardless of whether it’s in the anterior or posterior regions, is crucial for preserving the integrity of both hard and soft tissues. Equally important is the selection of biomaterials that not only offer structural support but also possess bone regeneration properties.”
— Dr. Hanae Saito
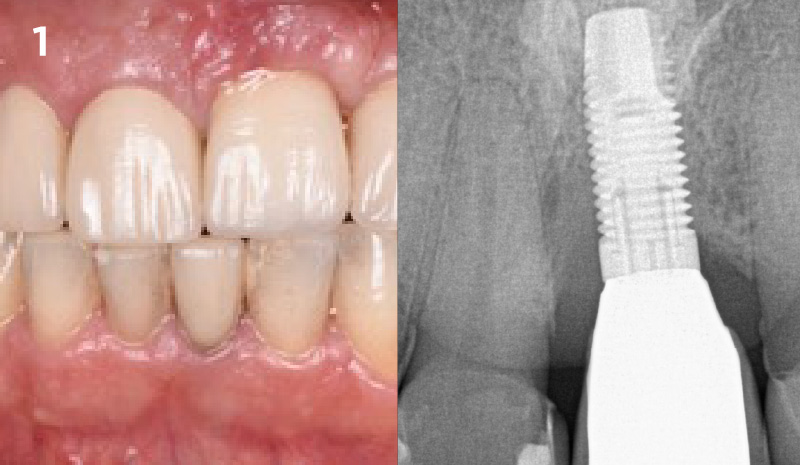
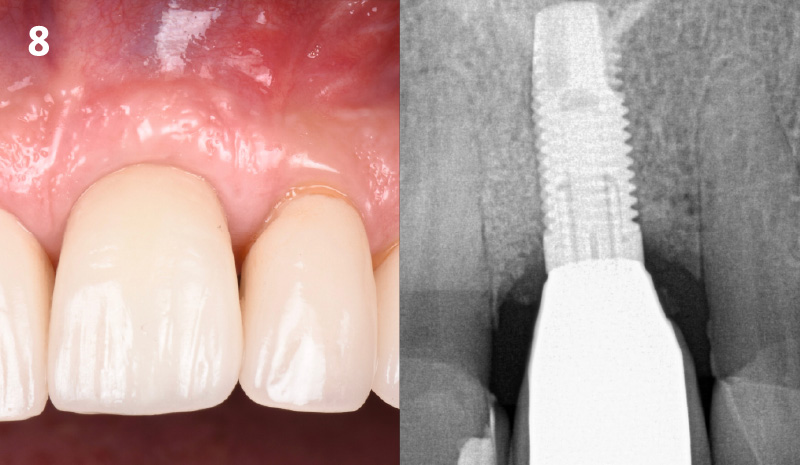
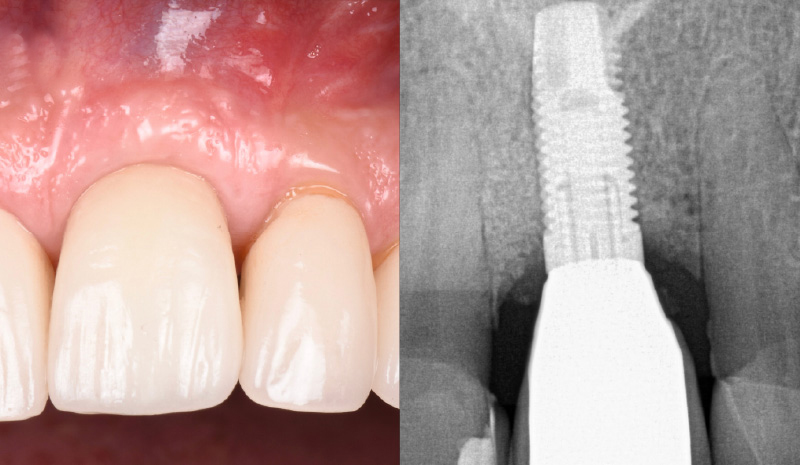
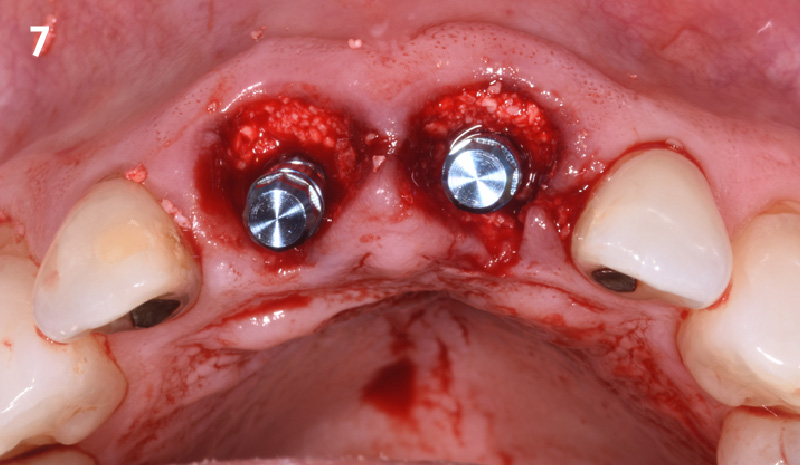
THE OUTCOME
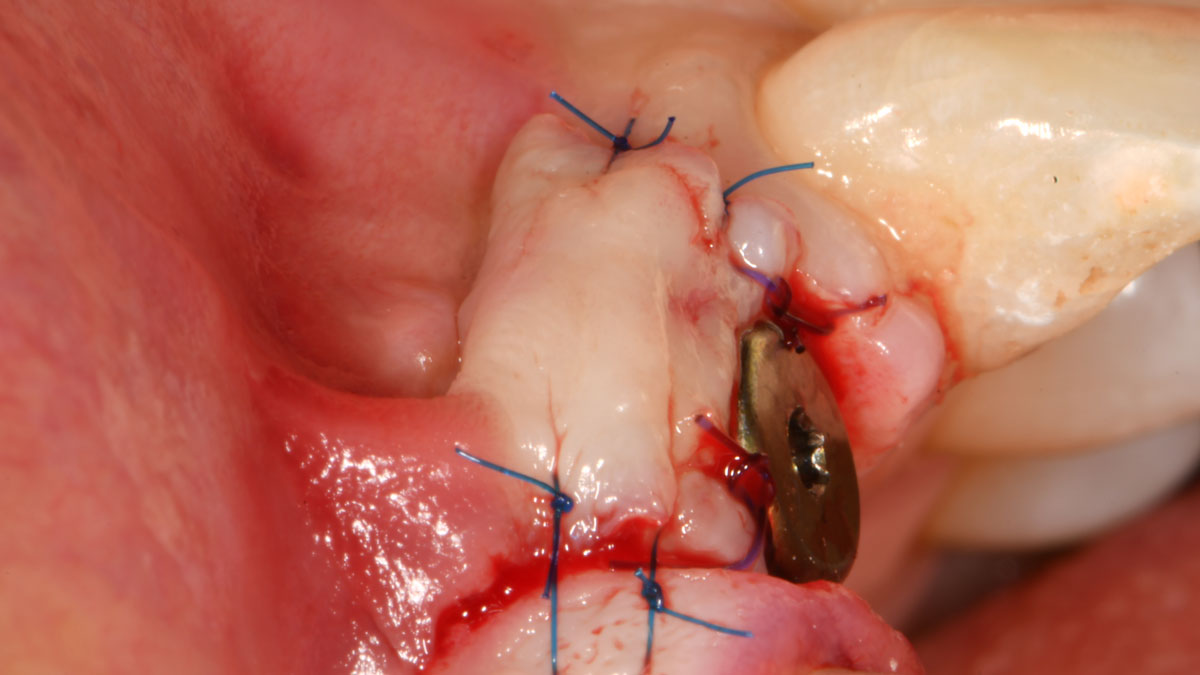
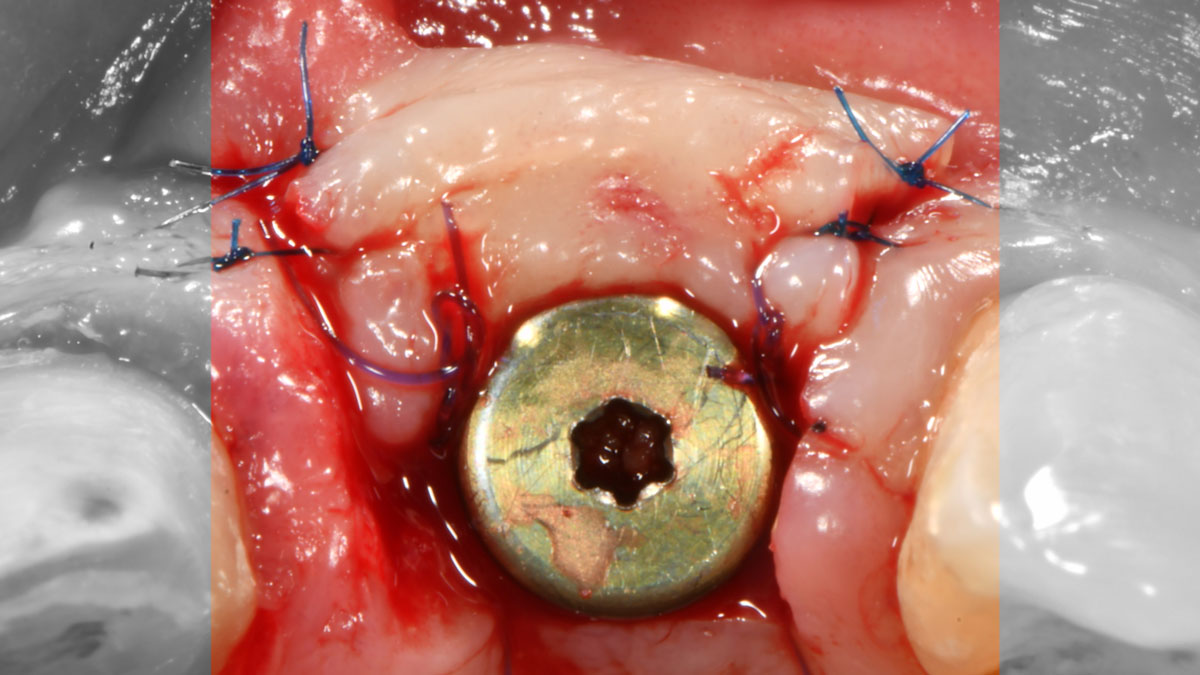
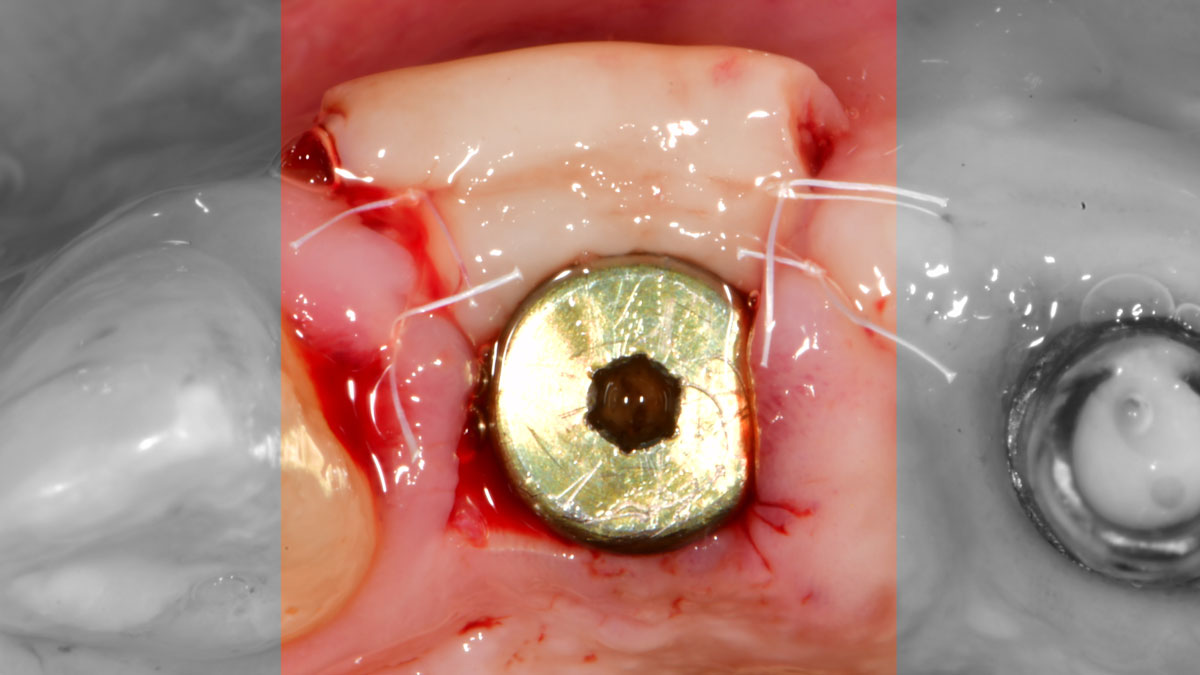
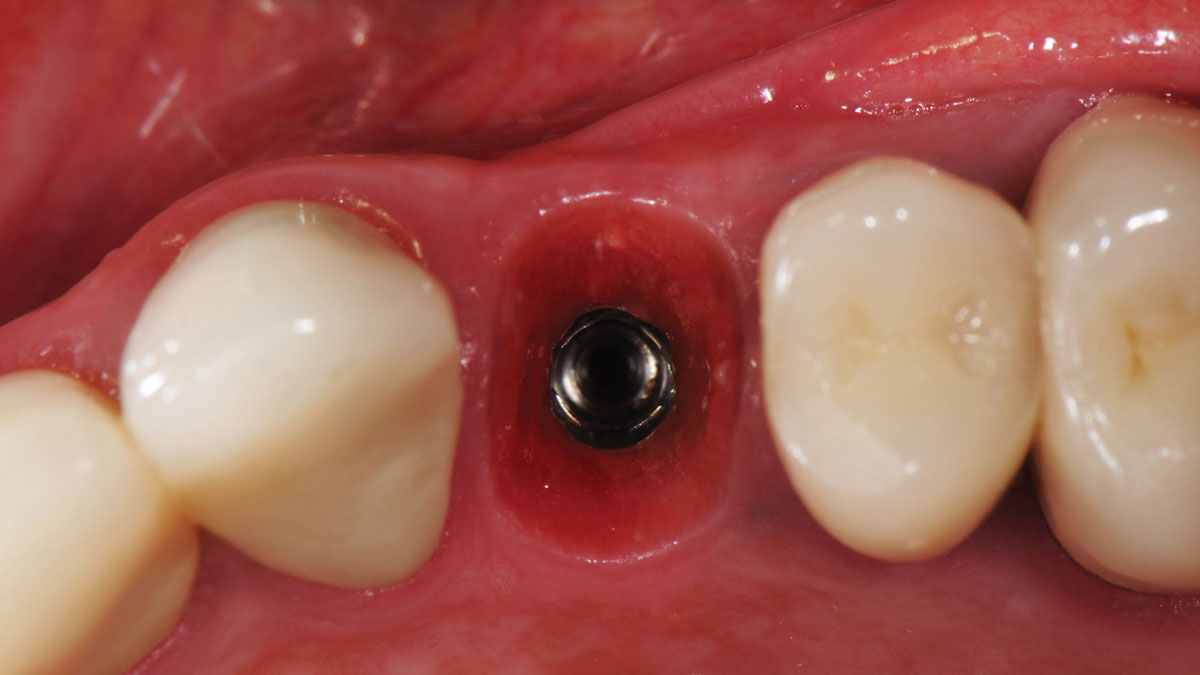
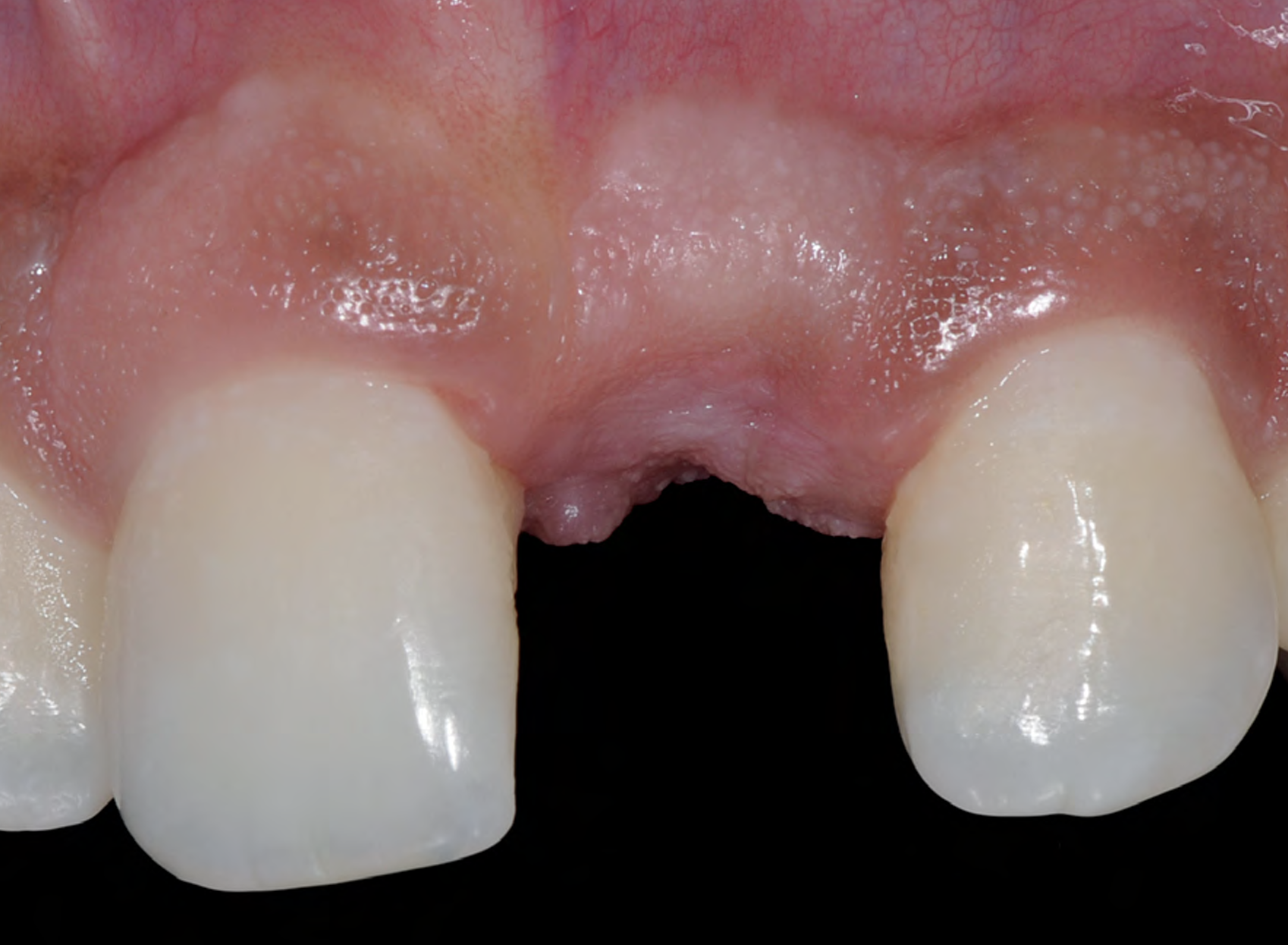
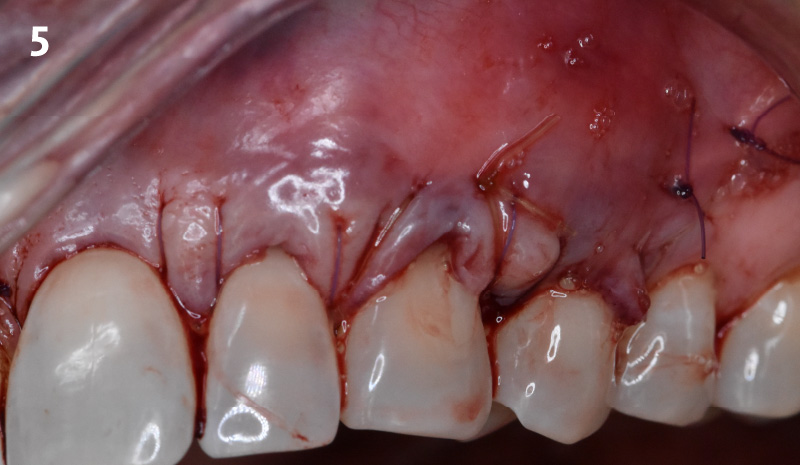
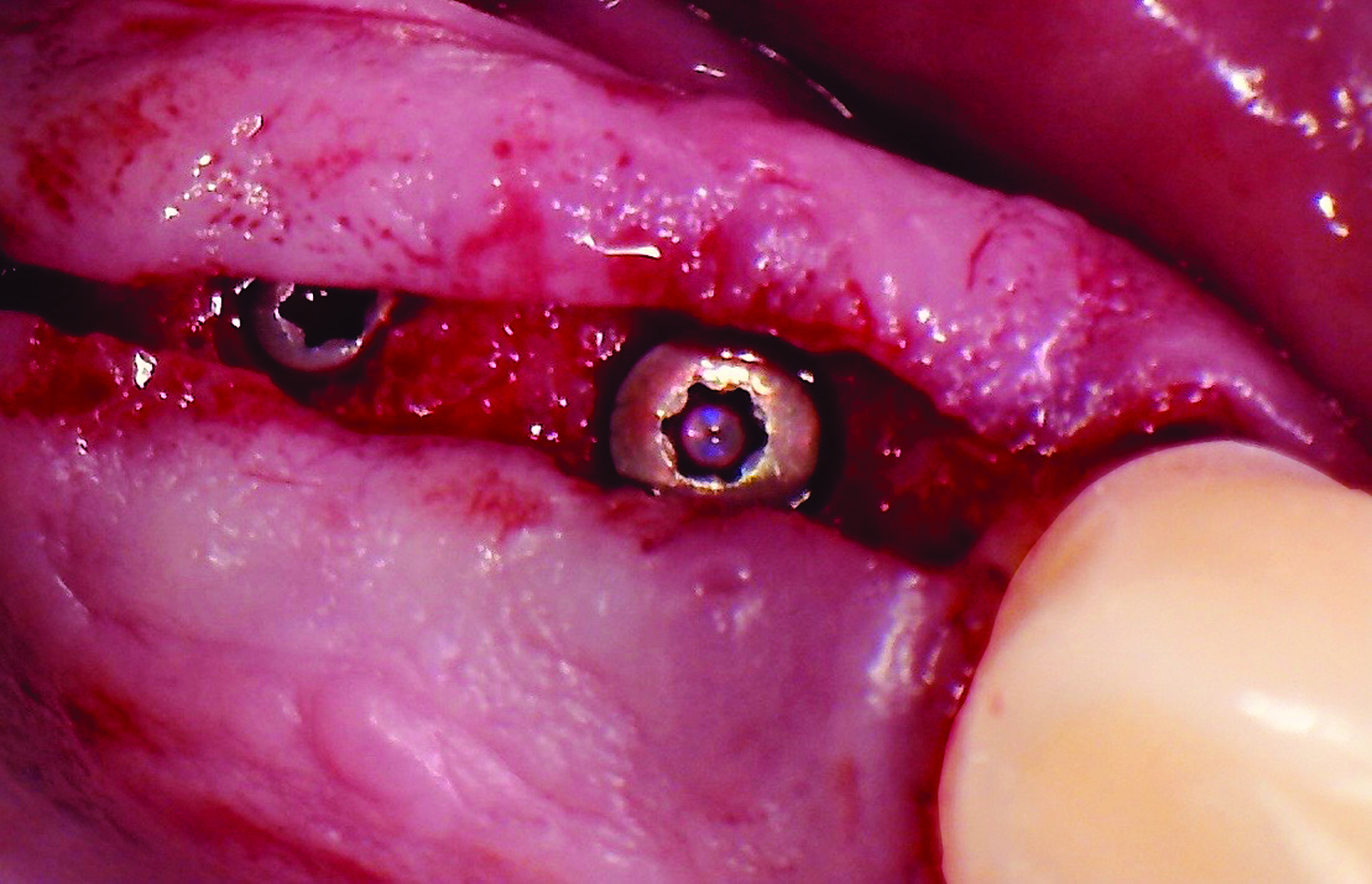
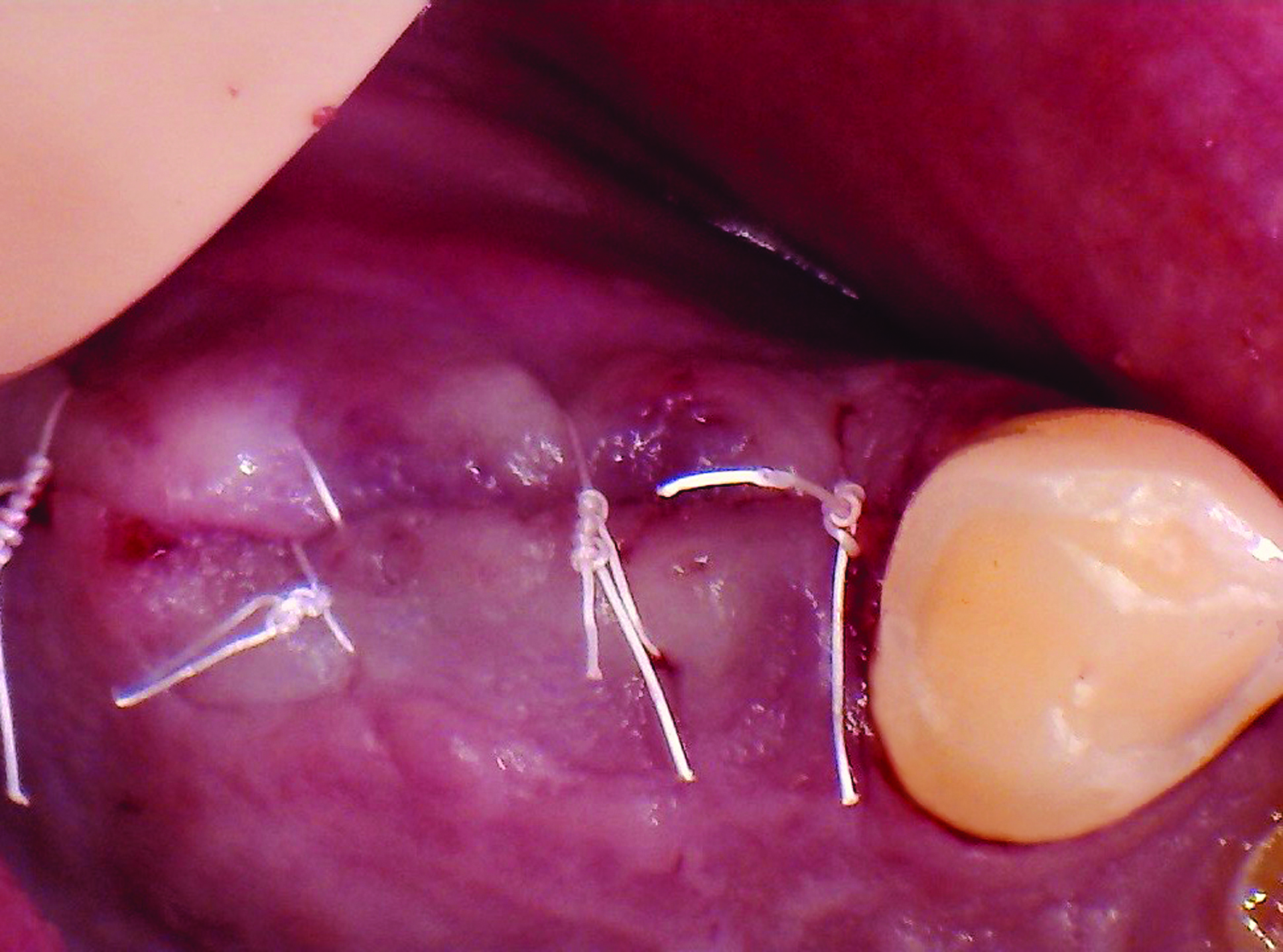
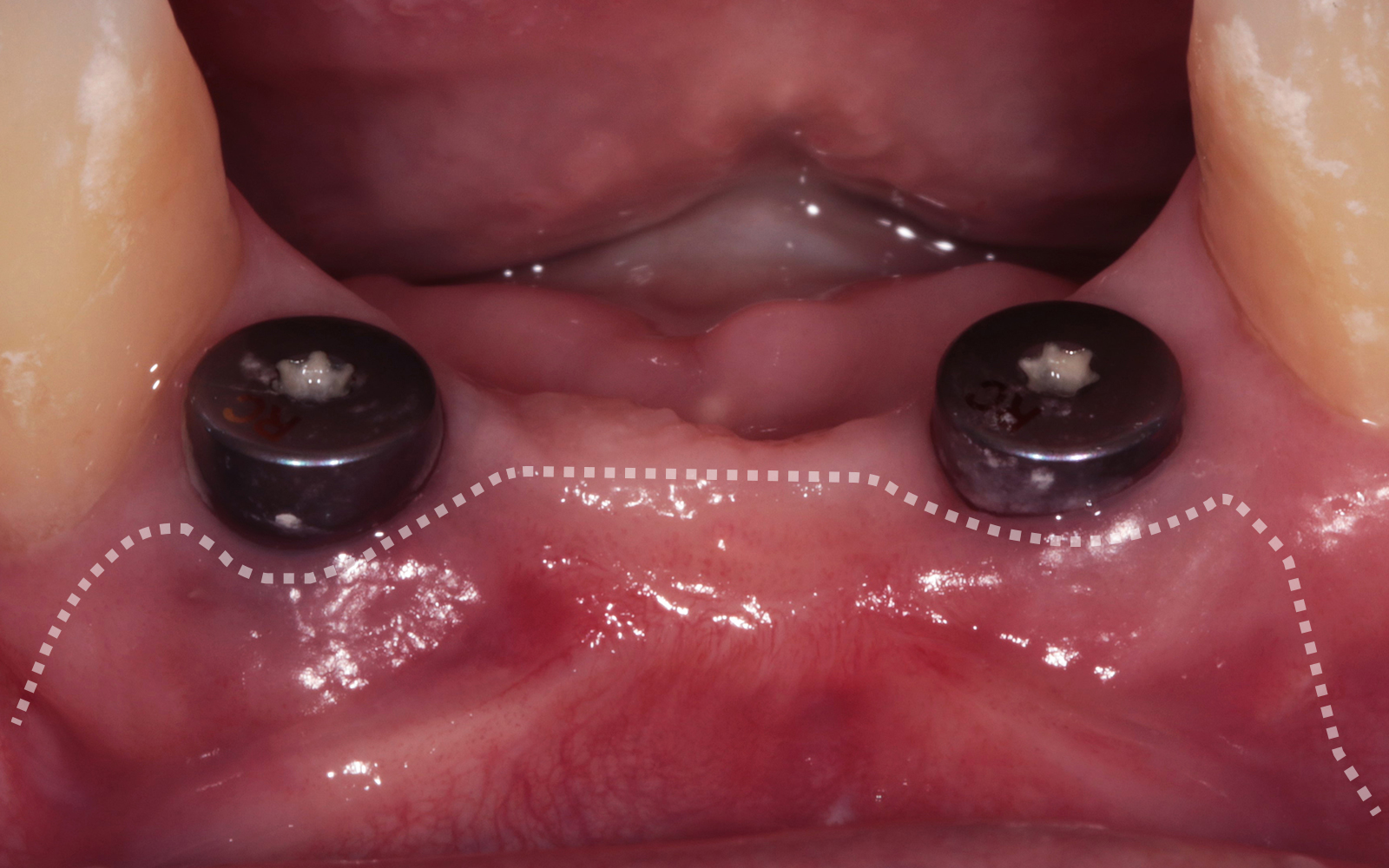
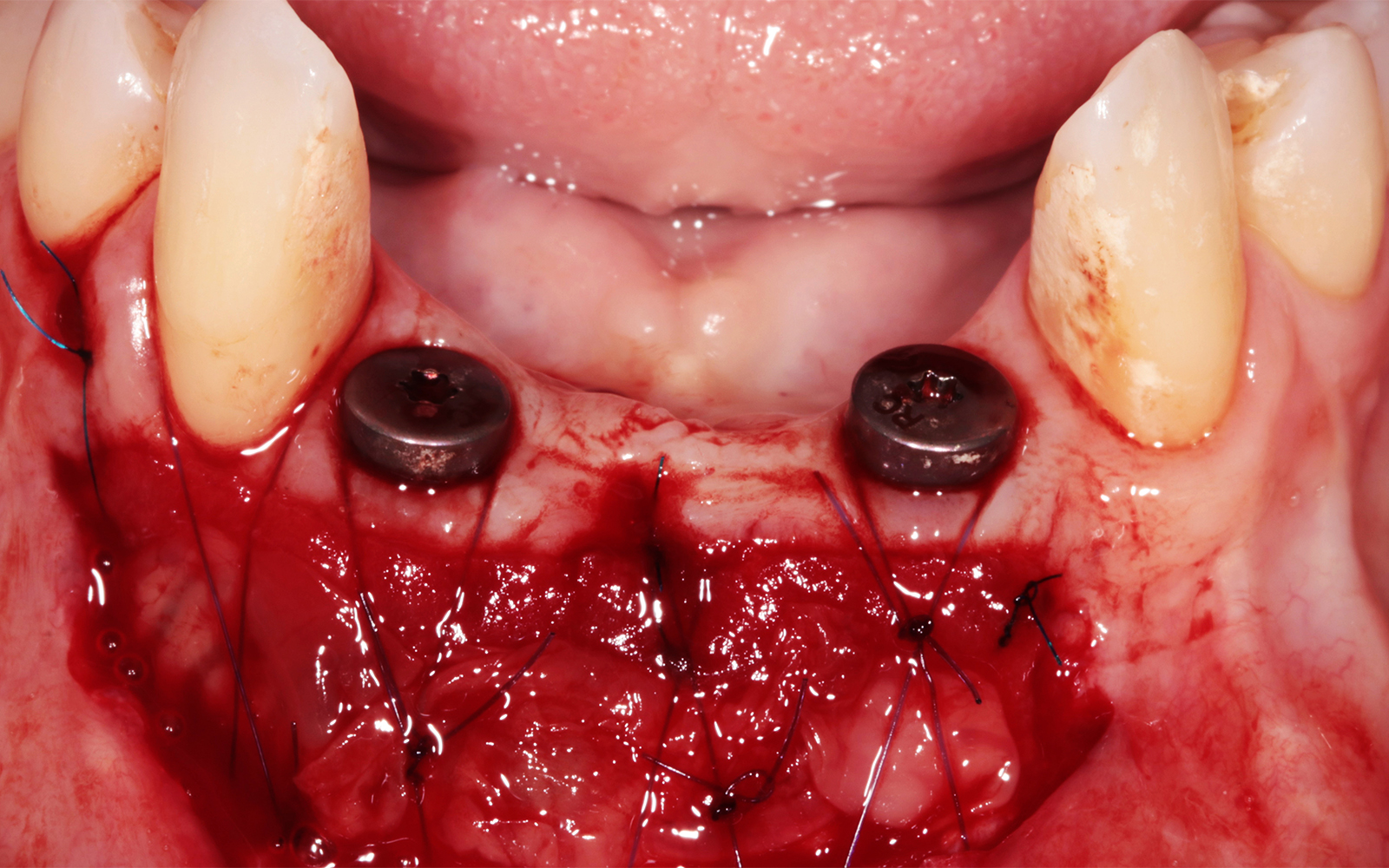
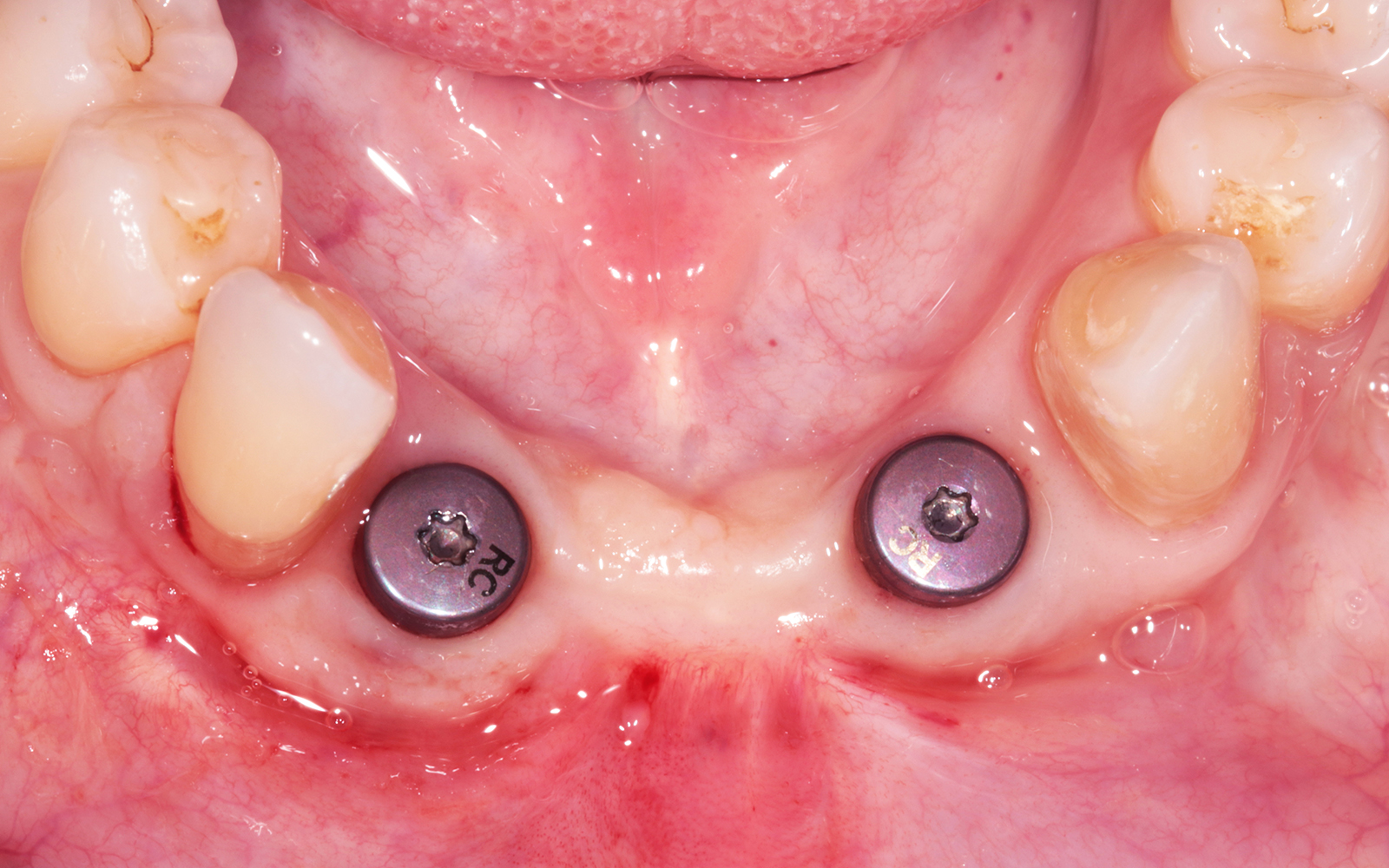
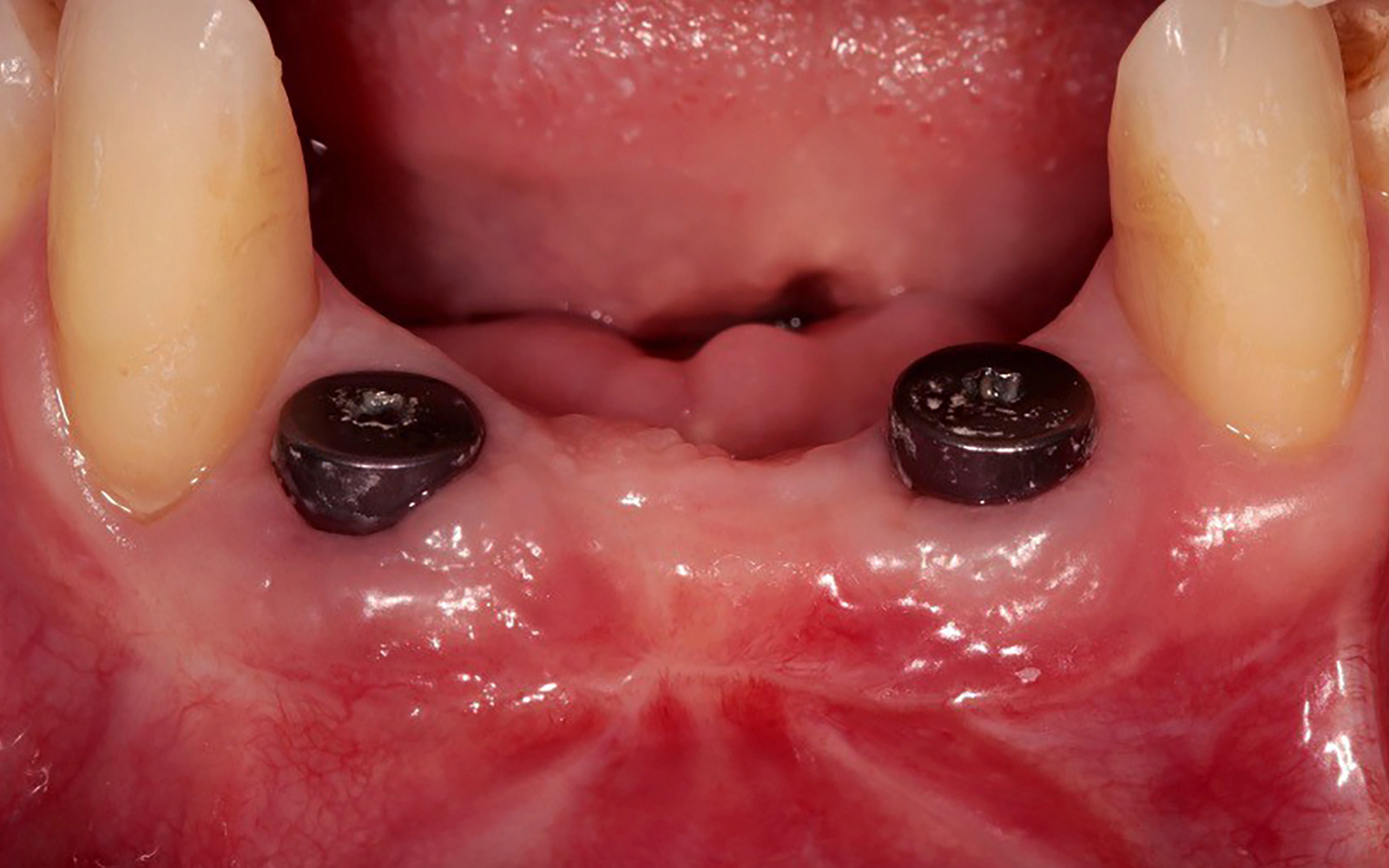
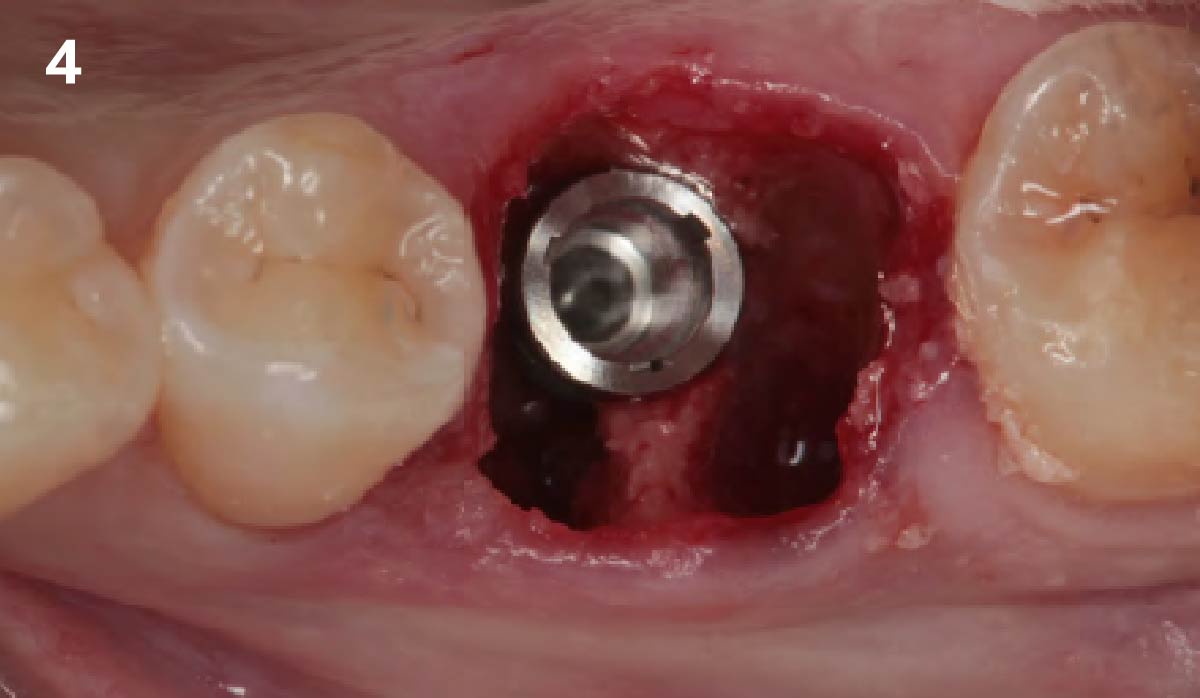
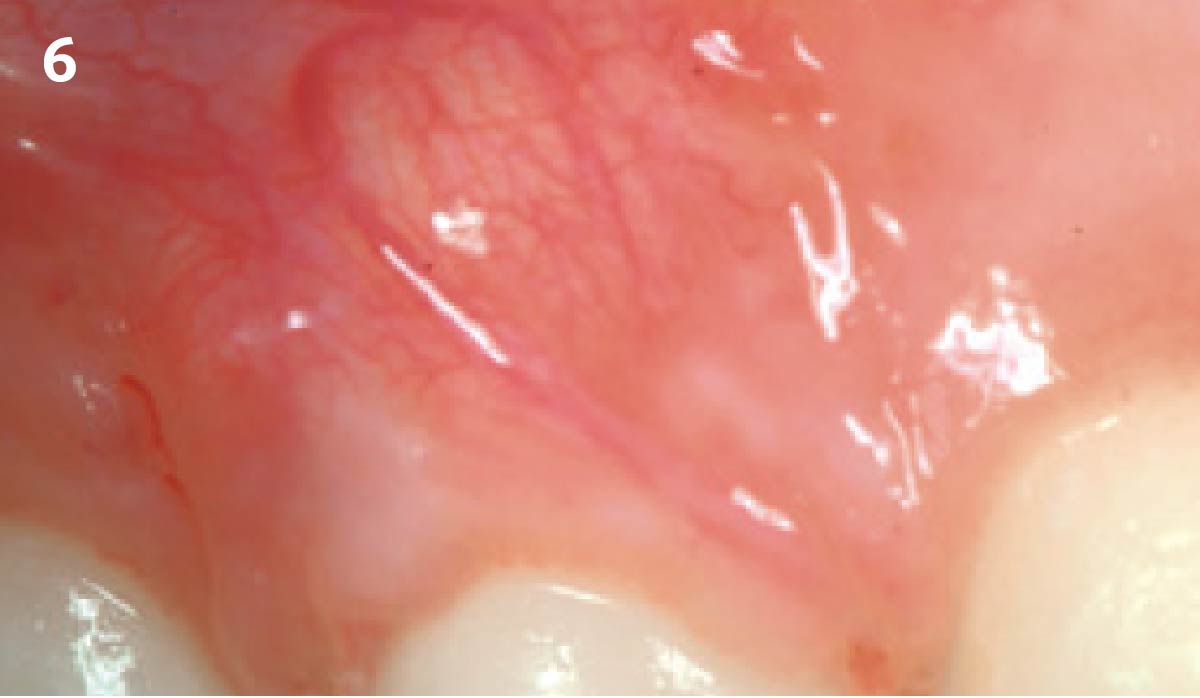
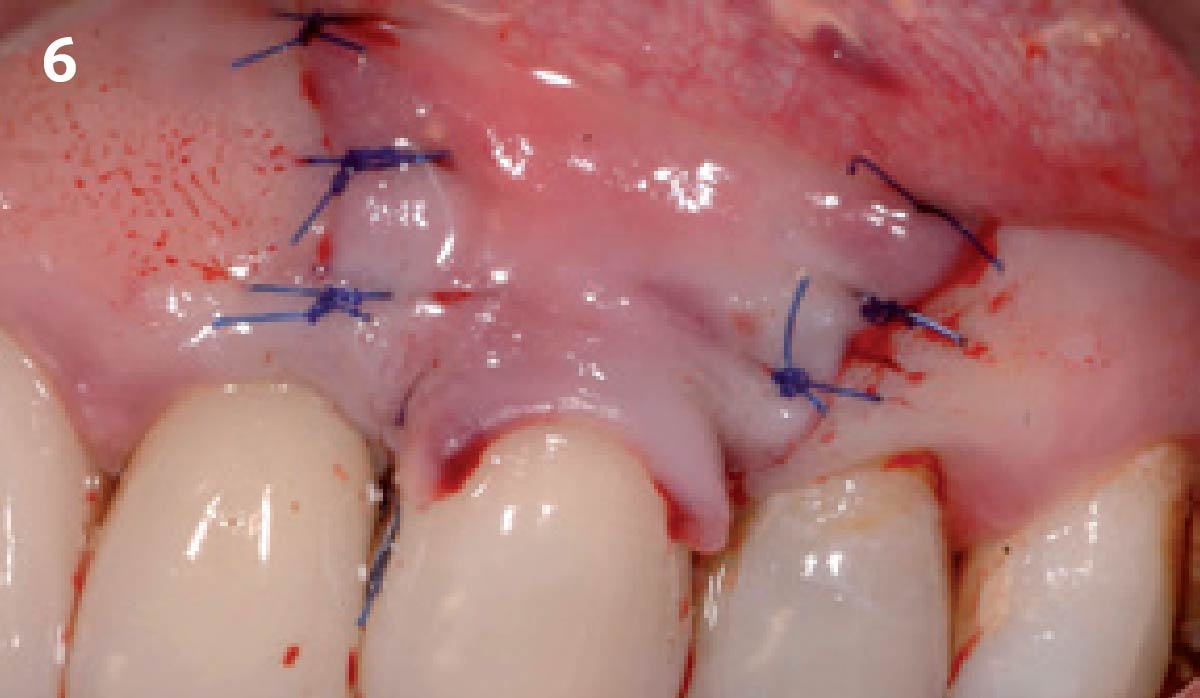
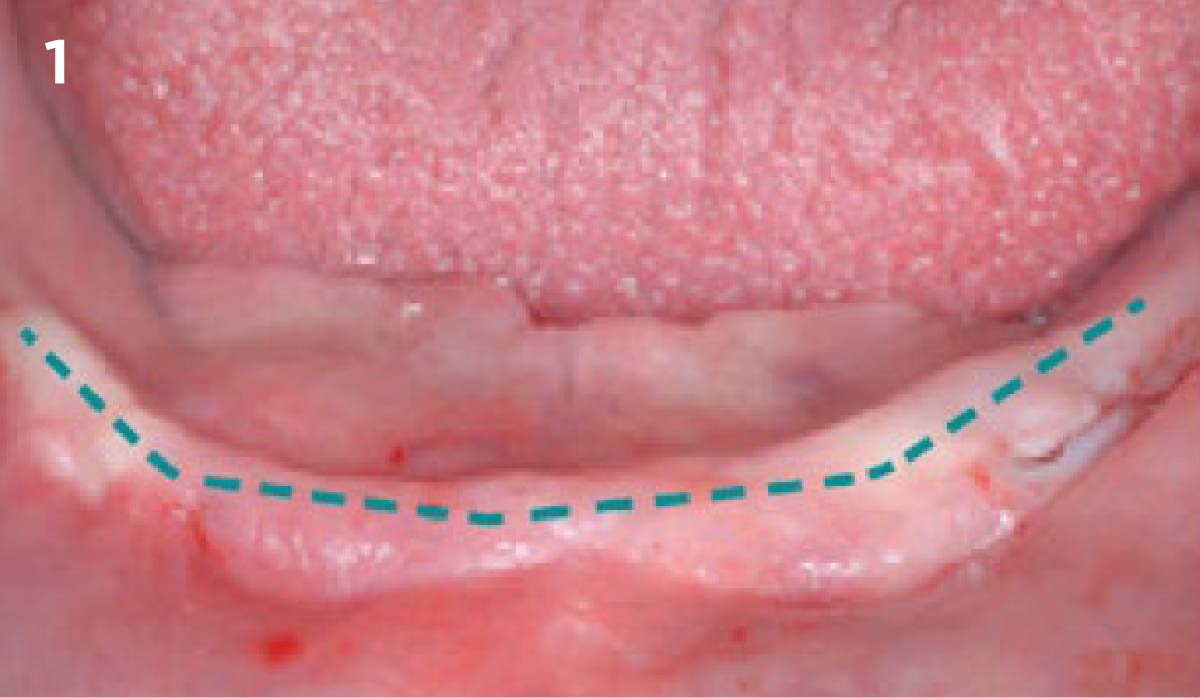
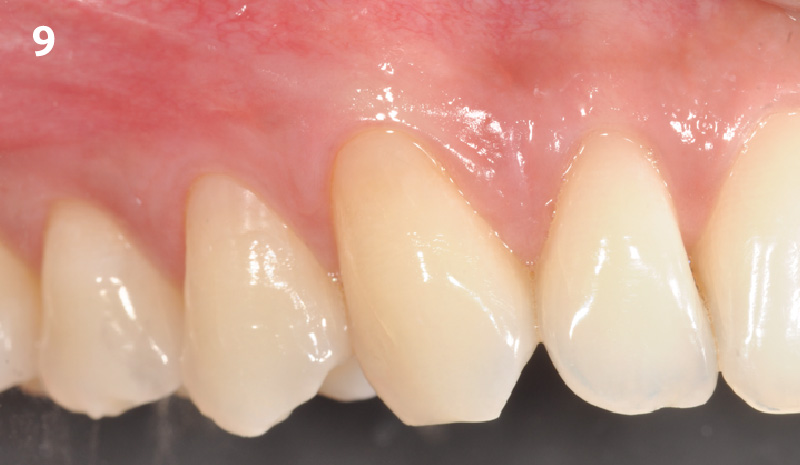
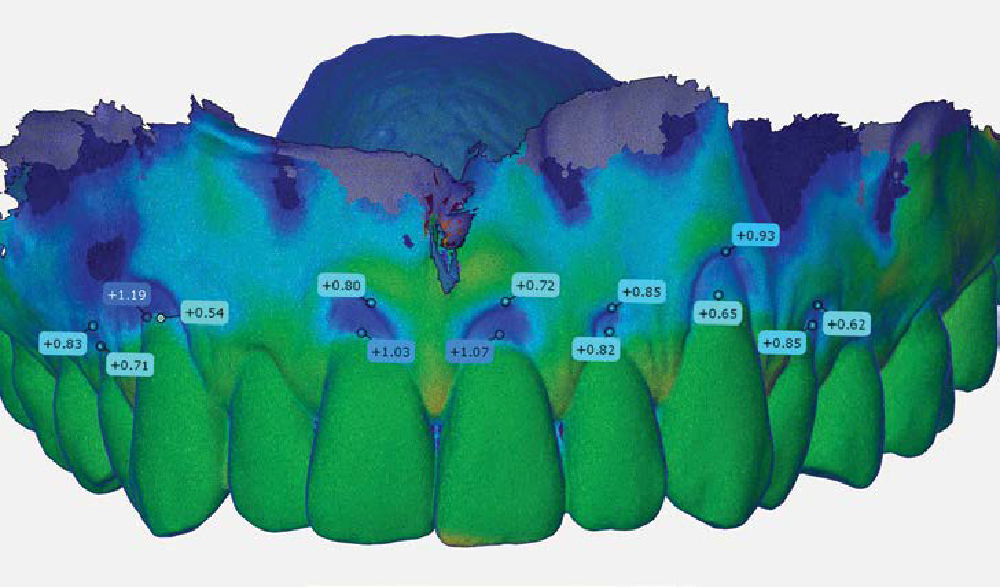
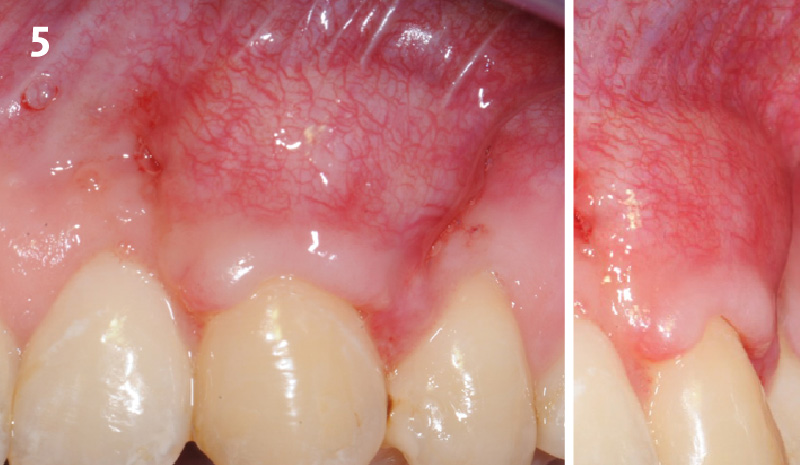
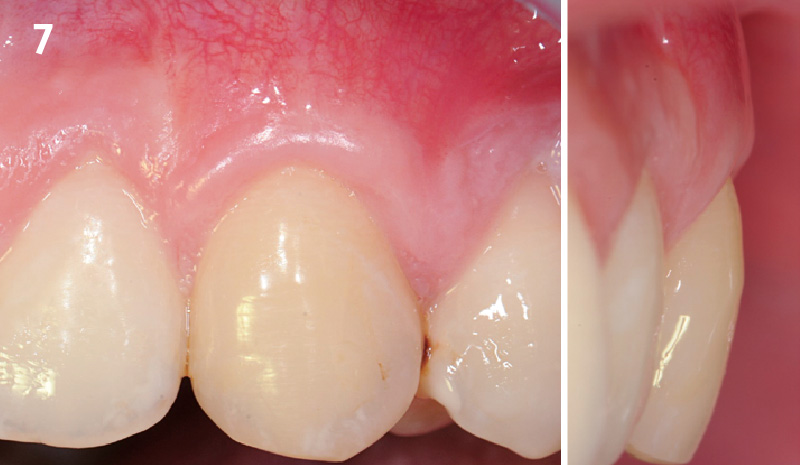
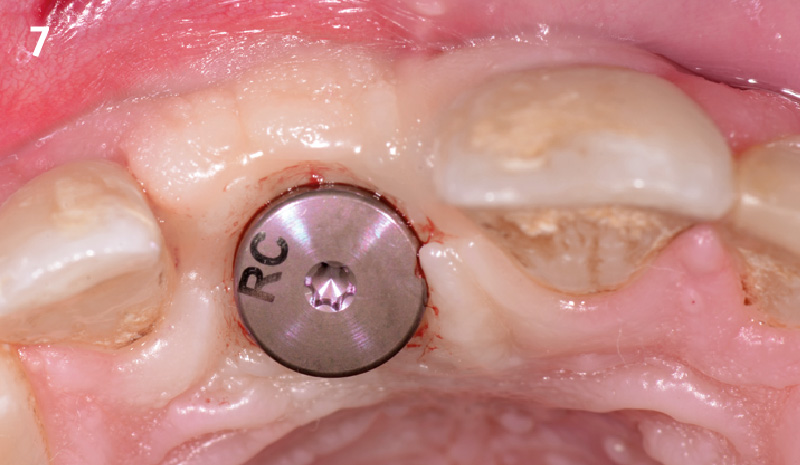
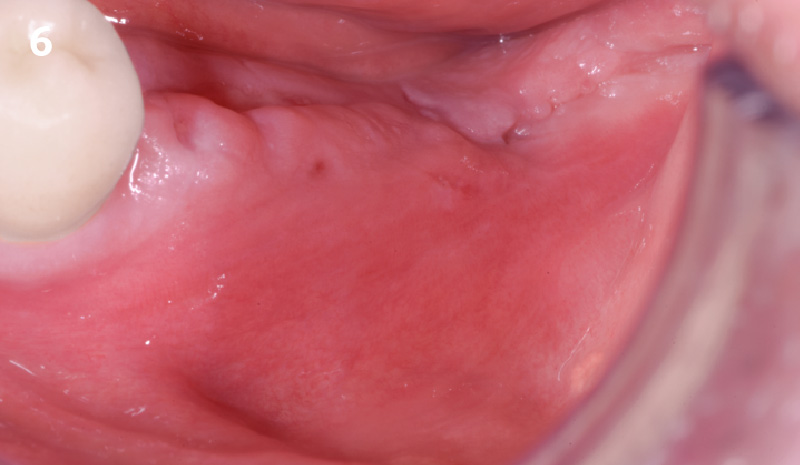
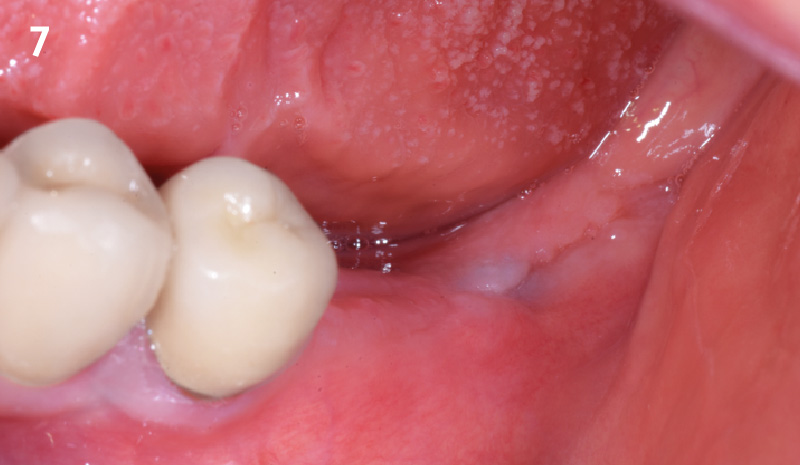
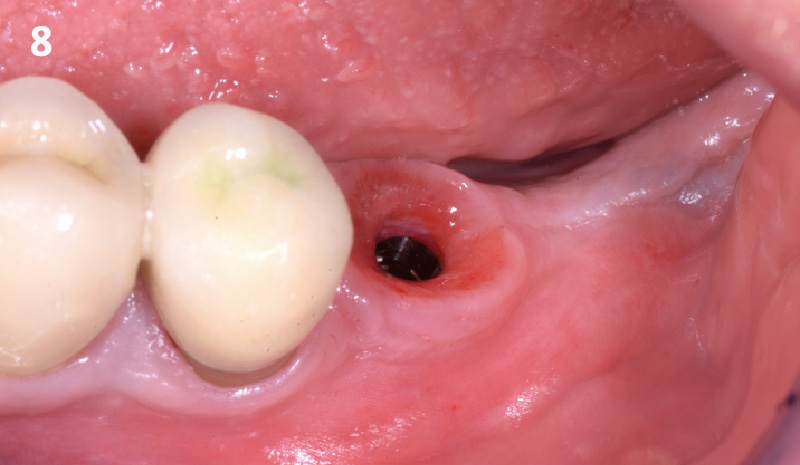
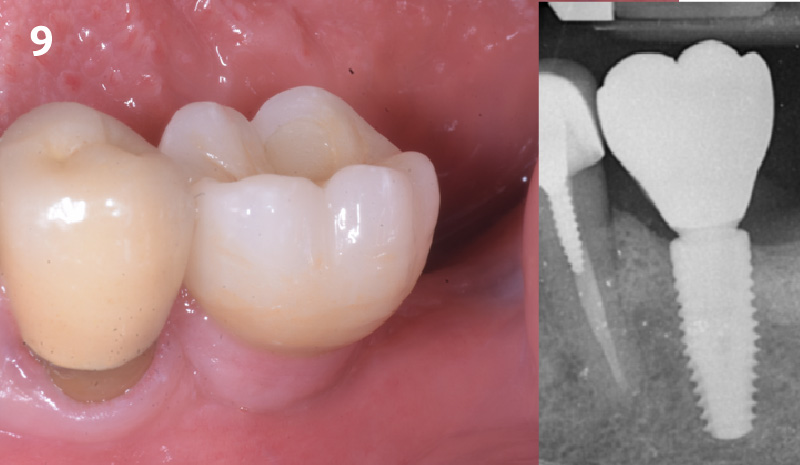
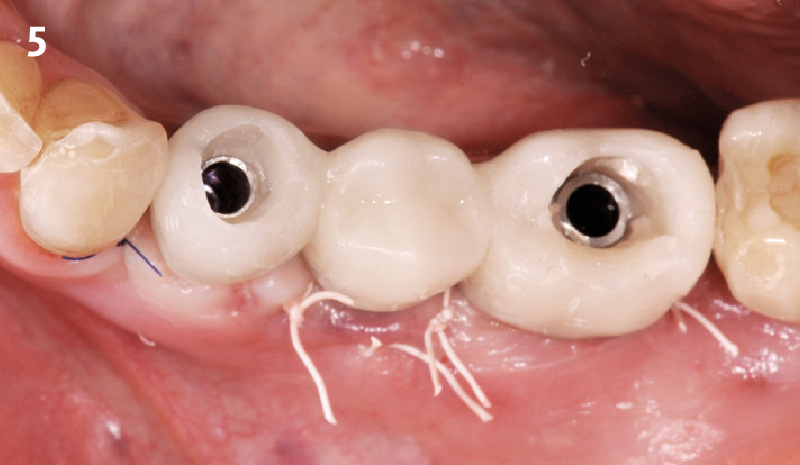
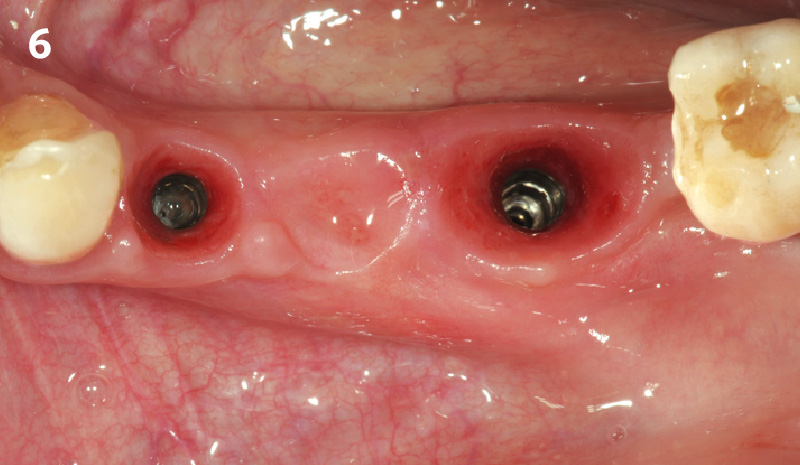
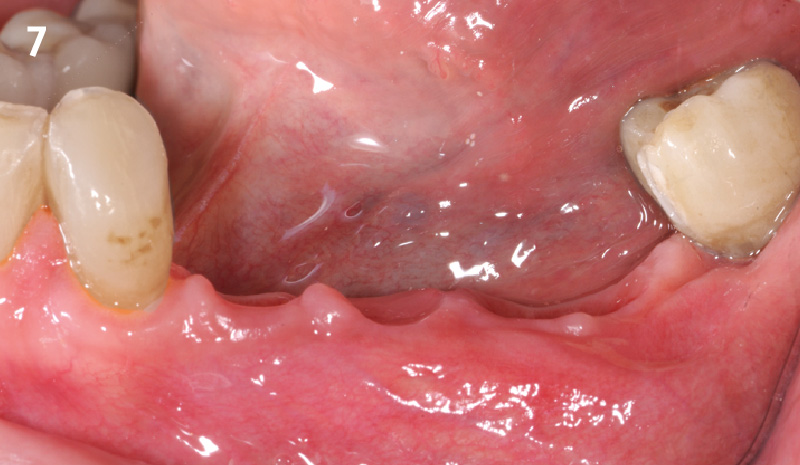
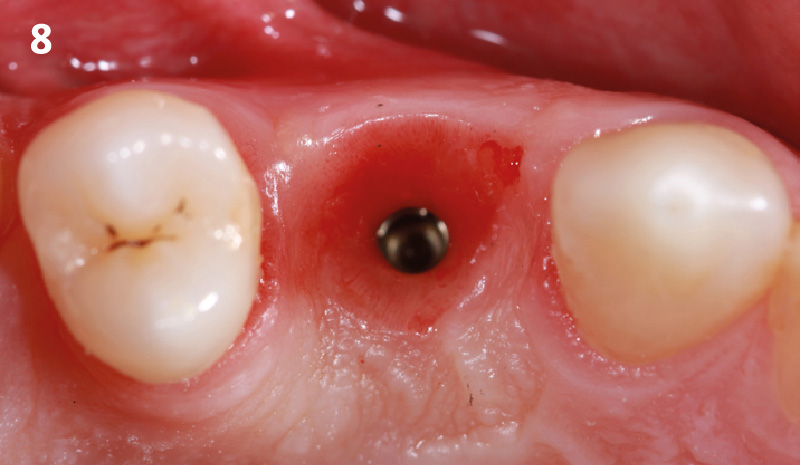
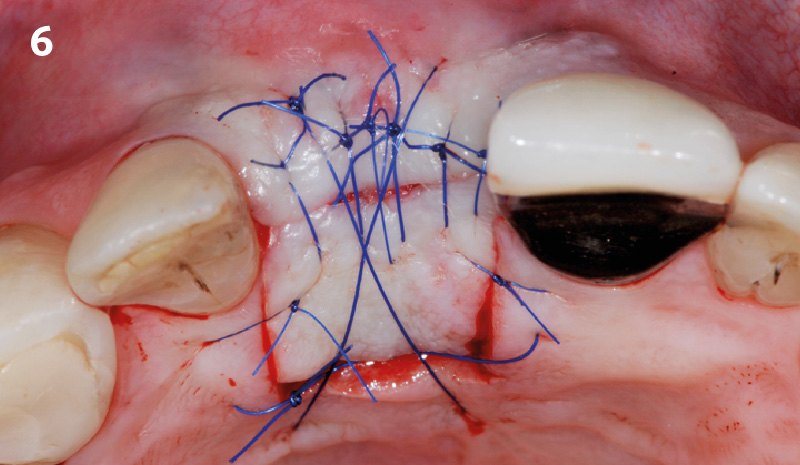
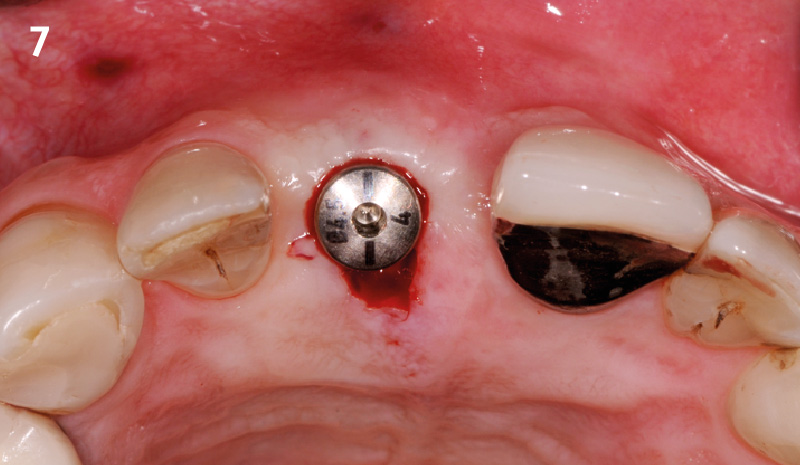
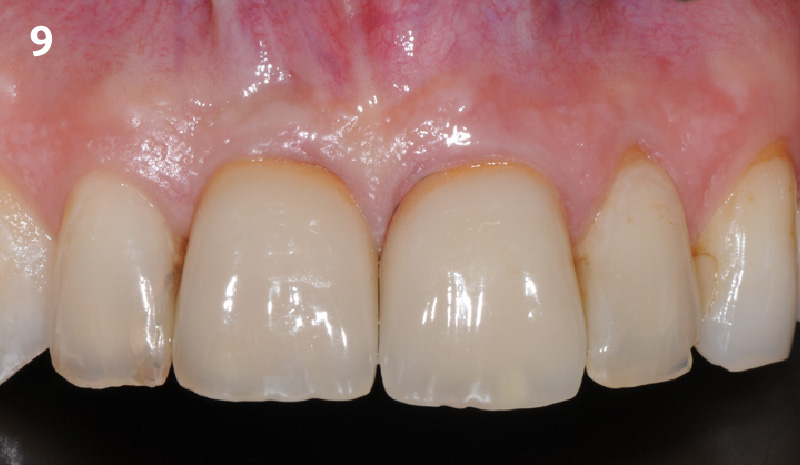
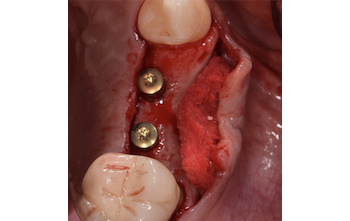
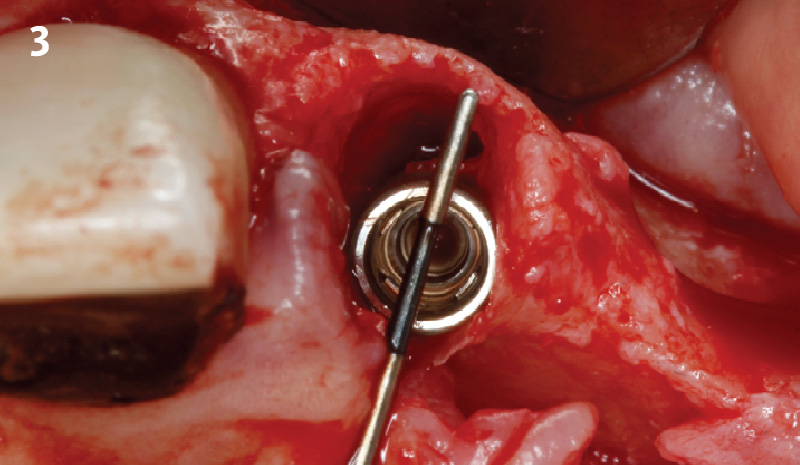
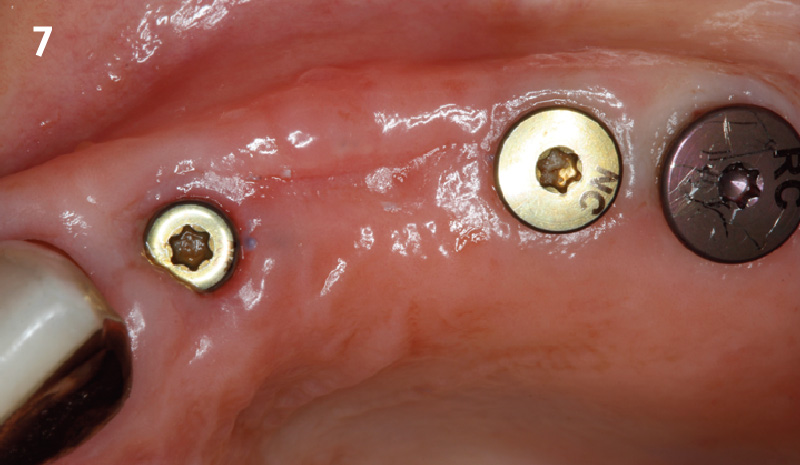
The planned treatment of replacing a tooth with a dental implant in the regenerated alveolar ridge was achieved. By employing secondary intention healing following ARP and utilizing a lingual paracrestal incision, adequate keratinized tissue was preserved on the buccal side of the implant-supported restoration.


Hanae Saito, DDS, MS, CCRC
Hanae Saito, DDS, MS, CCRC serves as a clinical associate professor and oversees the Dual Perio-Pros program and predoctoral periodontal education within the Division of Periodontics, at the University of Maryland School of Dentistry. She is a Diplomate of the American Board of Periodontology. Dr. Saito obtained a Master of Science in Clinical Research and a certificate in Periodontics from New York University College of Dentistry. Additionally, she operates a faculty practice focused on periodontology and implant dentistry.
Andrew Tong, DDS
Andrew Tong, DDS earned his Bachelor of Science degree from the University of Maryland at College Park in 2015 before completing his Doctor of Dental Surgery (D.D.S) degree at the University of Maryland School of Dentistry in 2019. Following this, he undertook a General Practice Residency at the Newark Beth Israel Medical Center in New Jersey from 2019 to 2020. Dr Tong now practices general dentistry at Tong Dental Care in Gaithersburg, MD. Concurrently, he is pursuing a Master’s degree in Periodontics at the University of Maryland School of Dentistry.