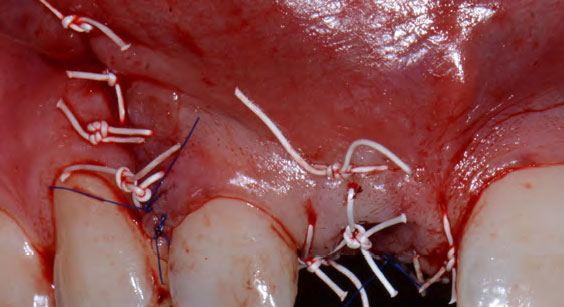
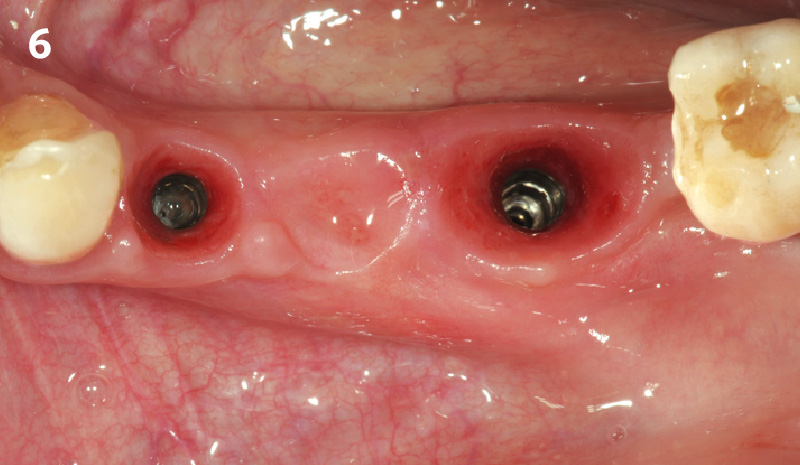
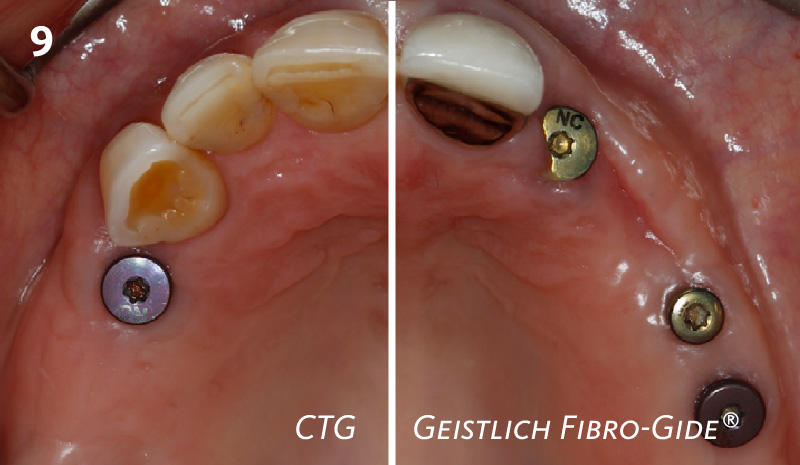
CLINICAL CASE
THE OUTCOME
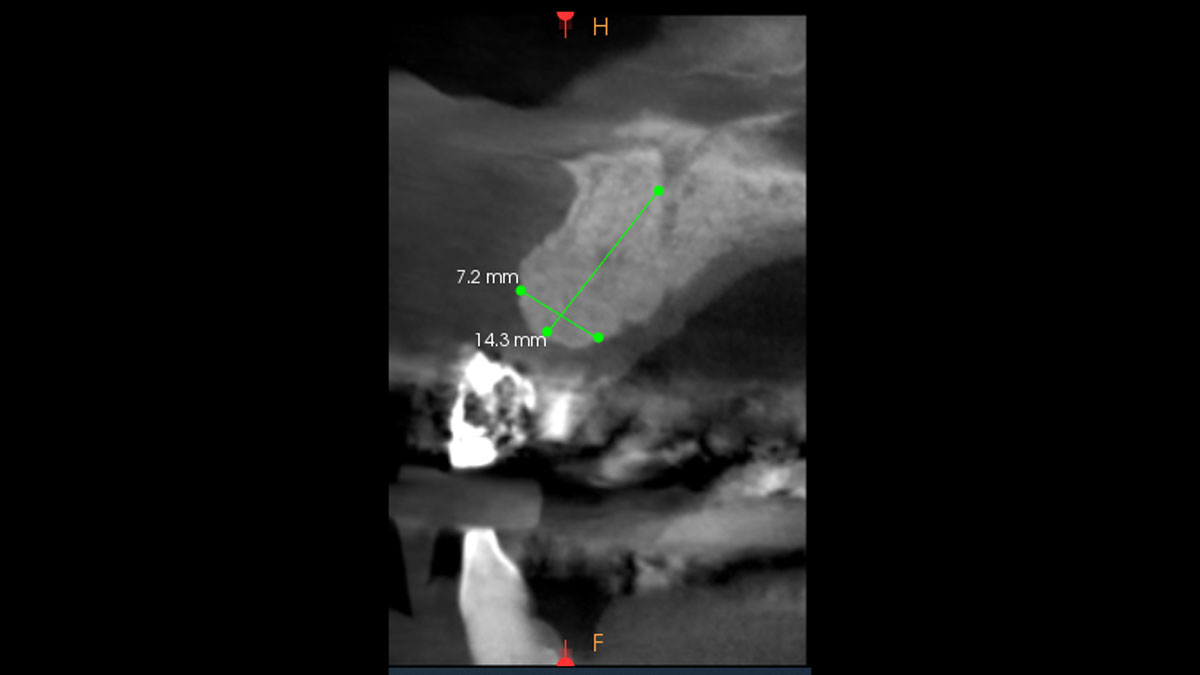
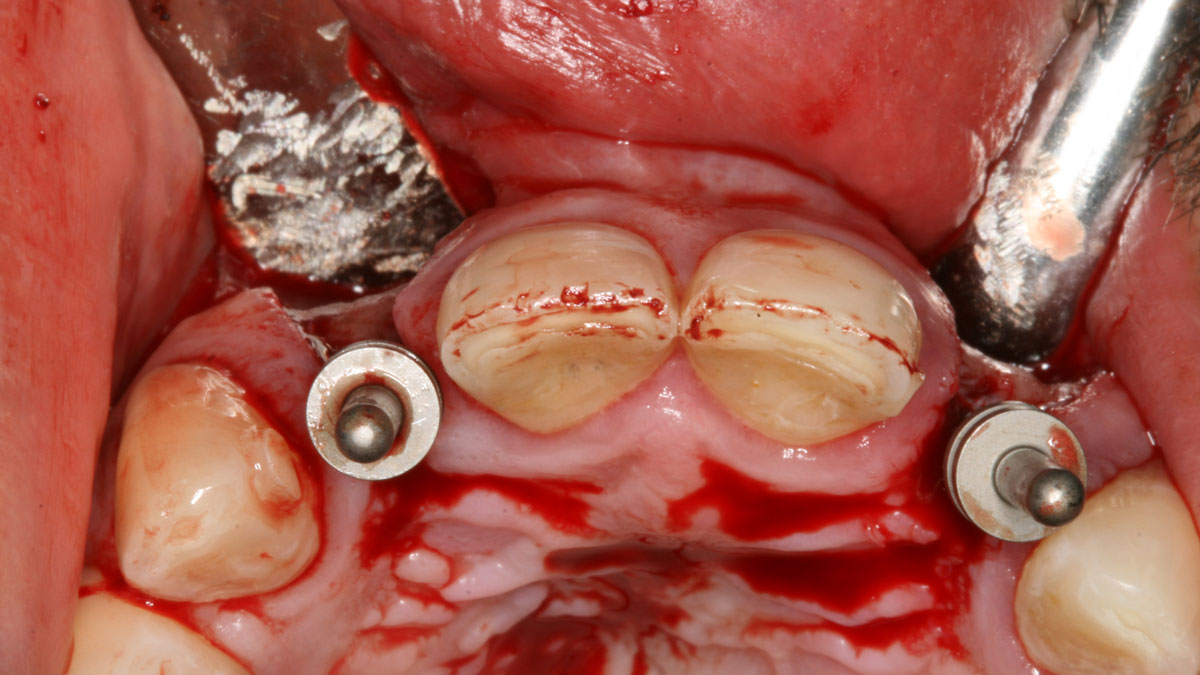
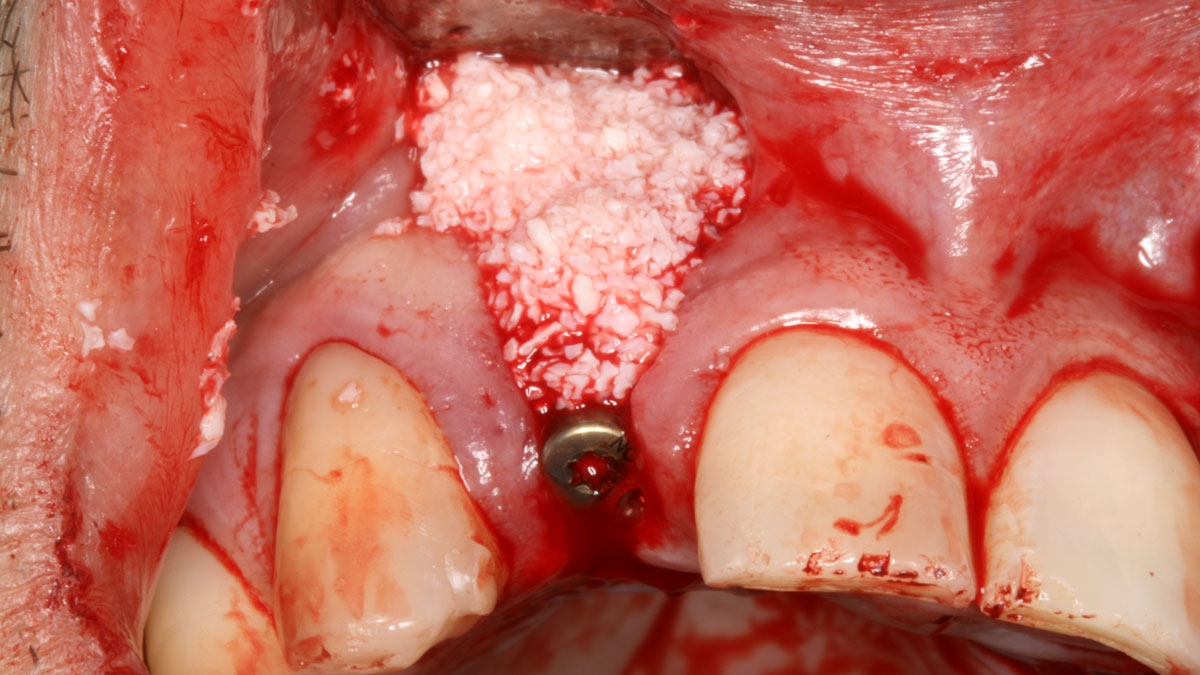
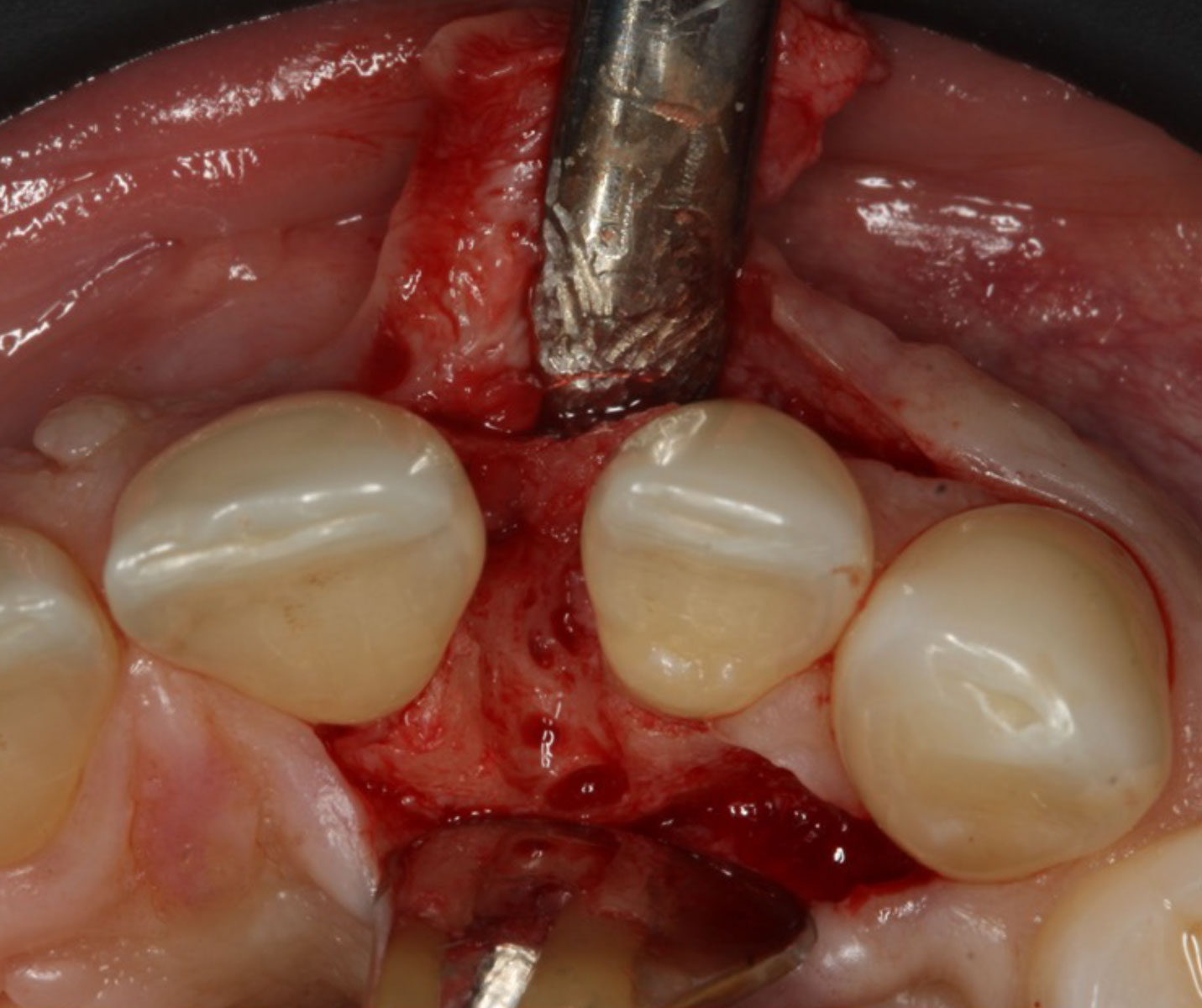
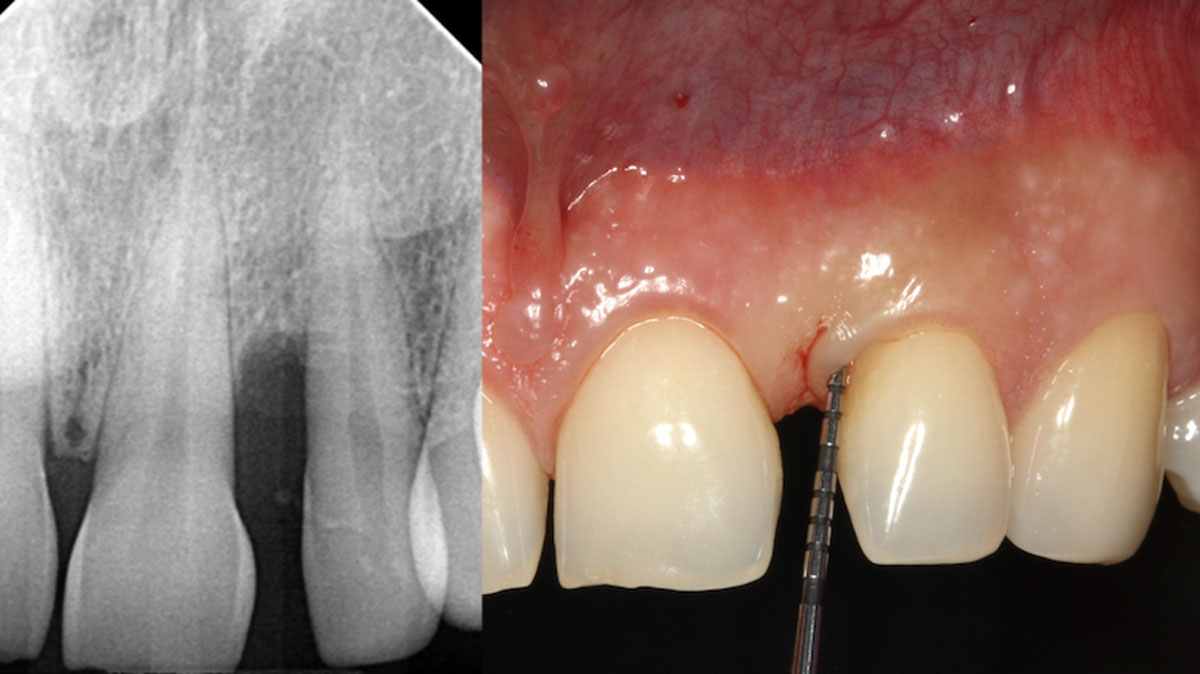
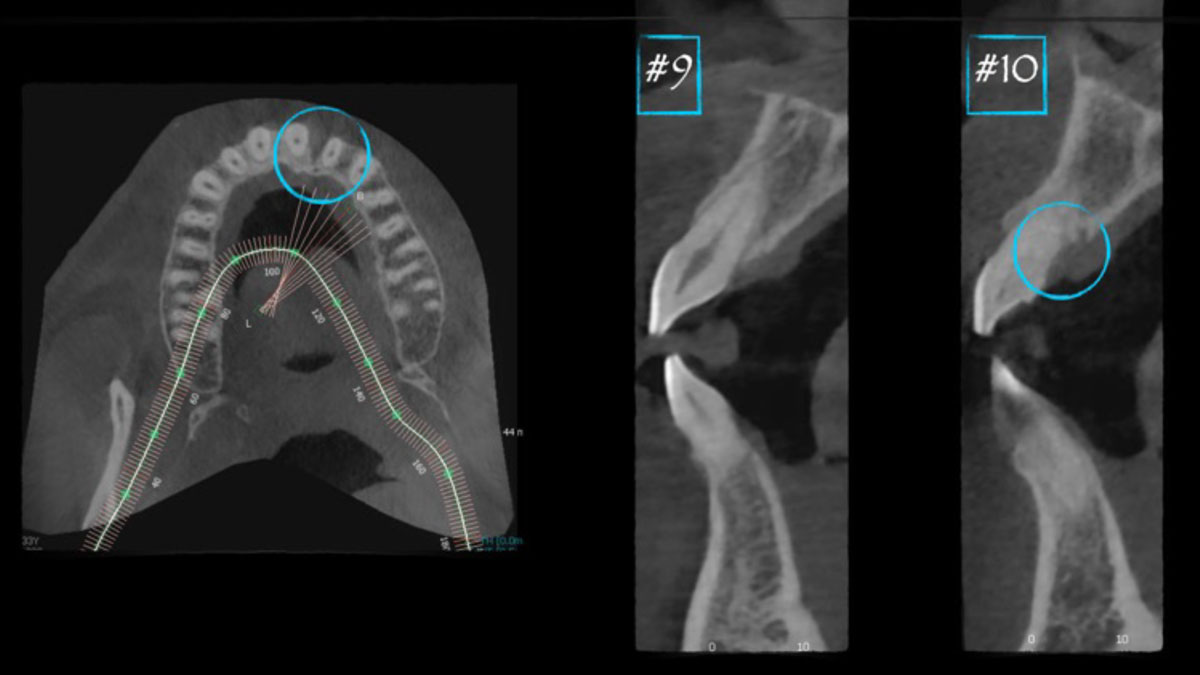
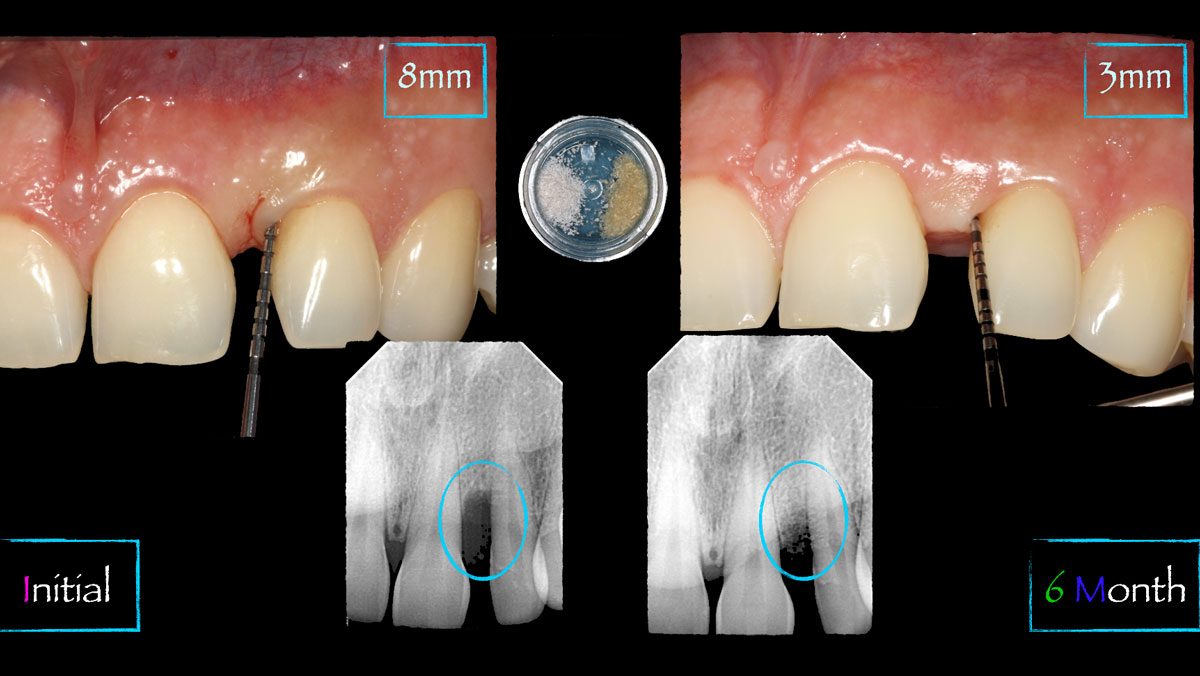
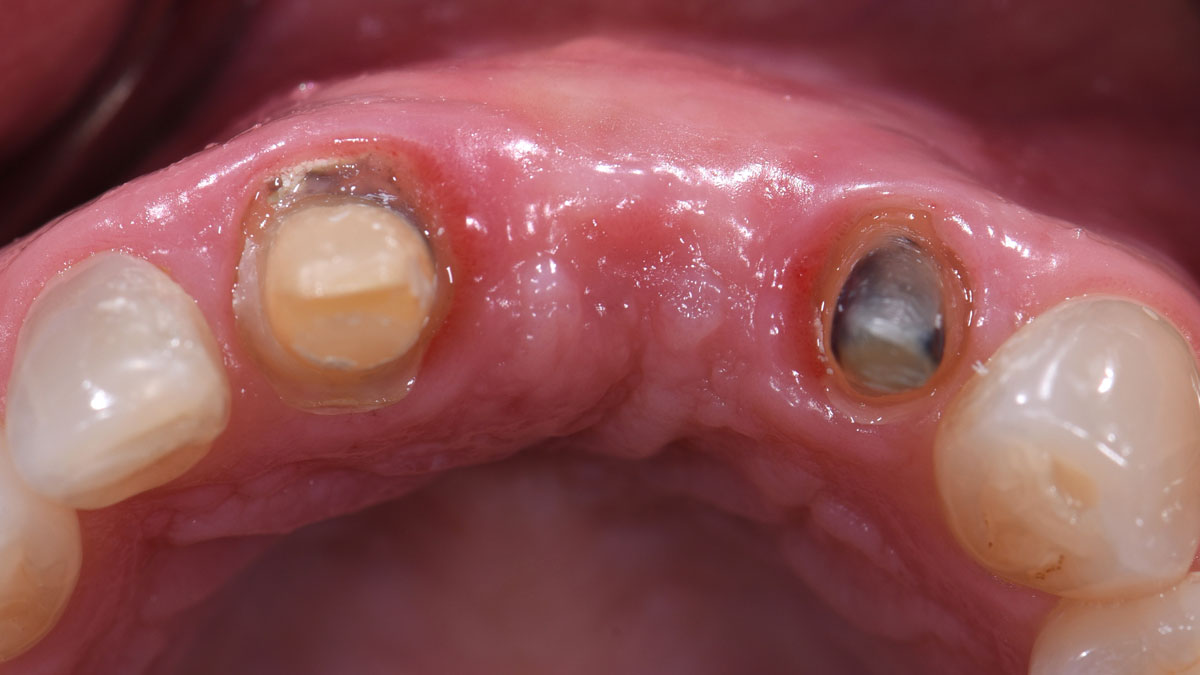
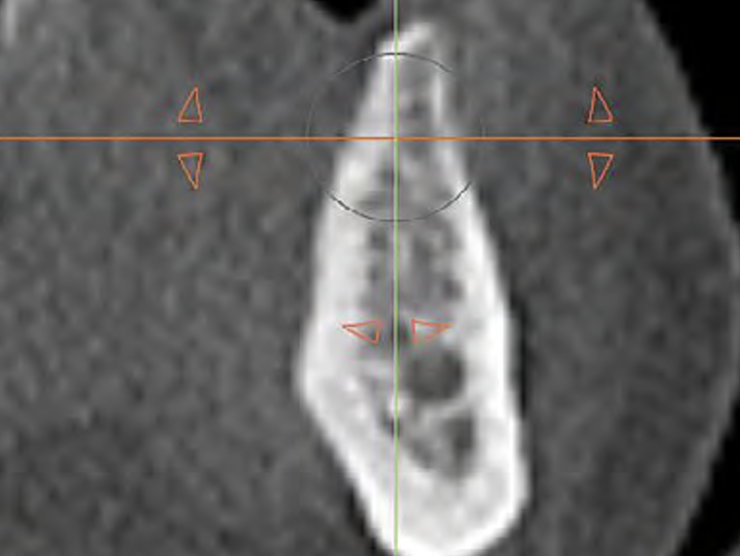
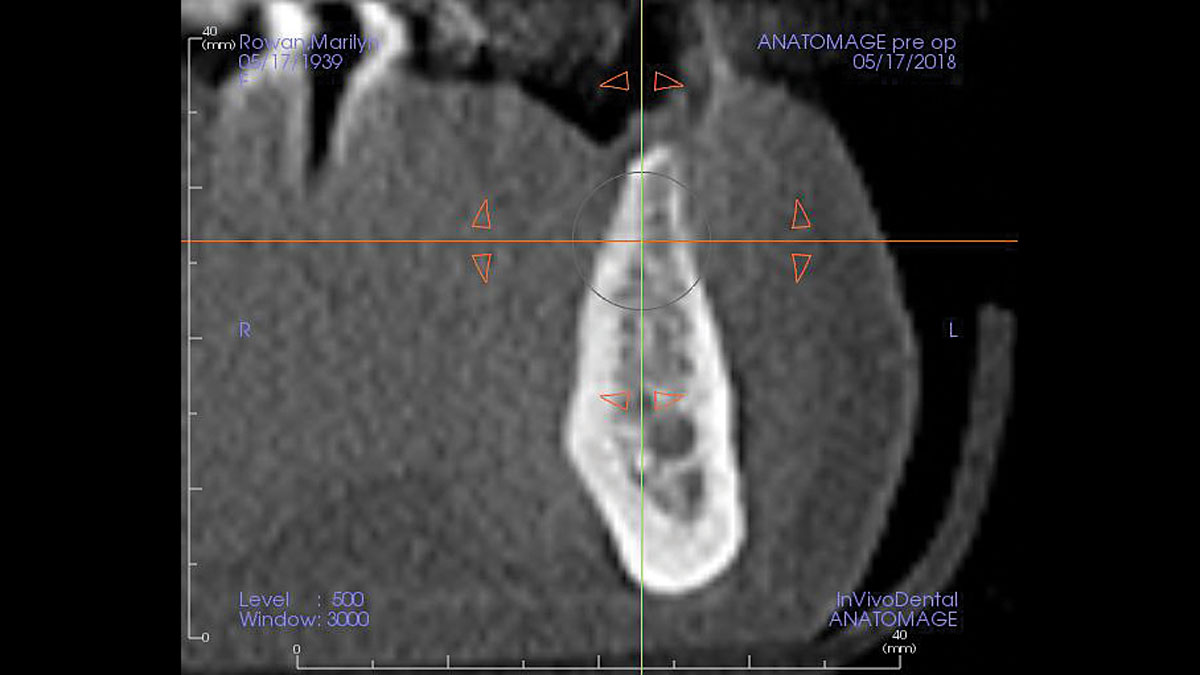
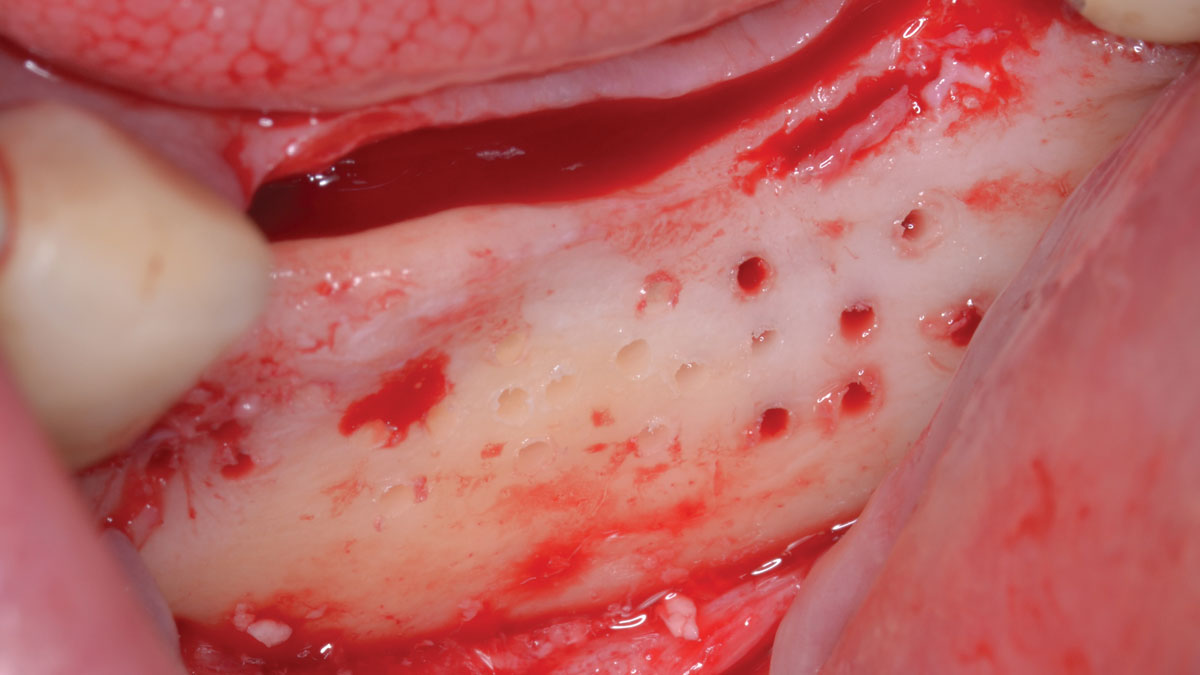
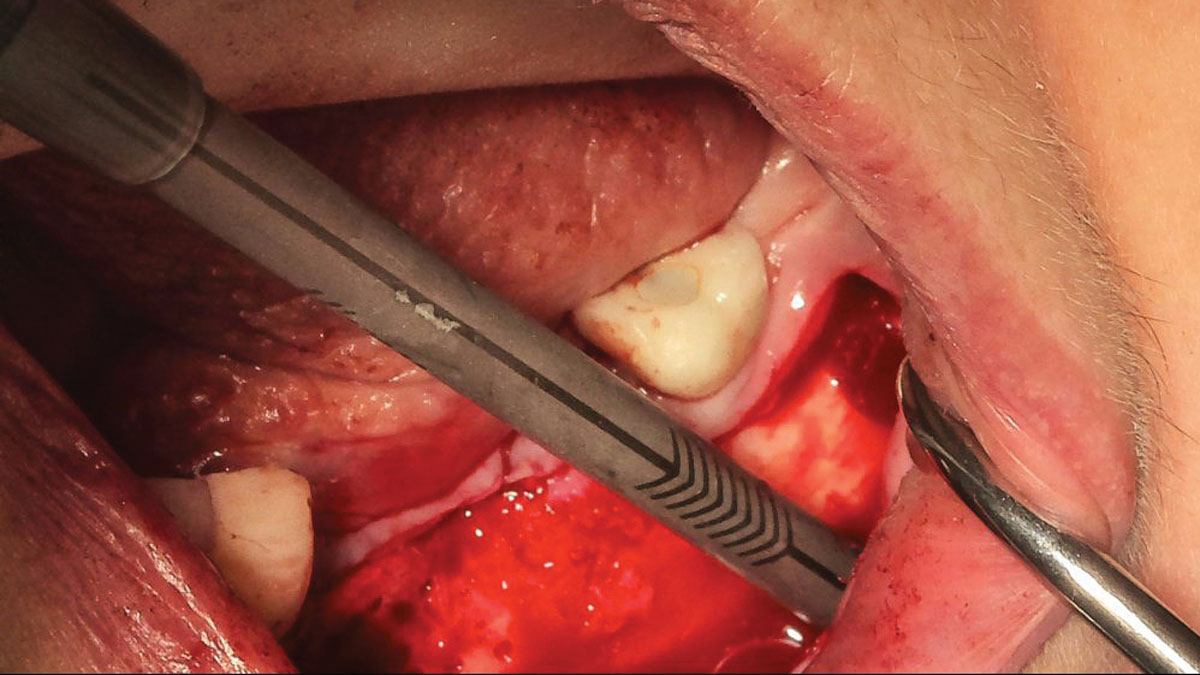
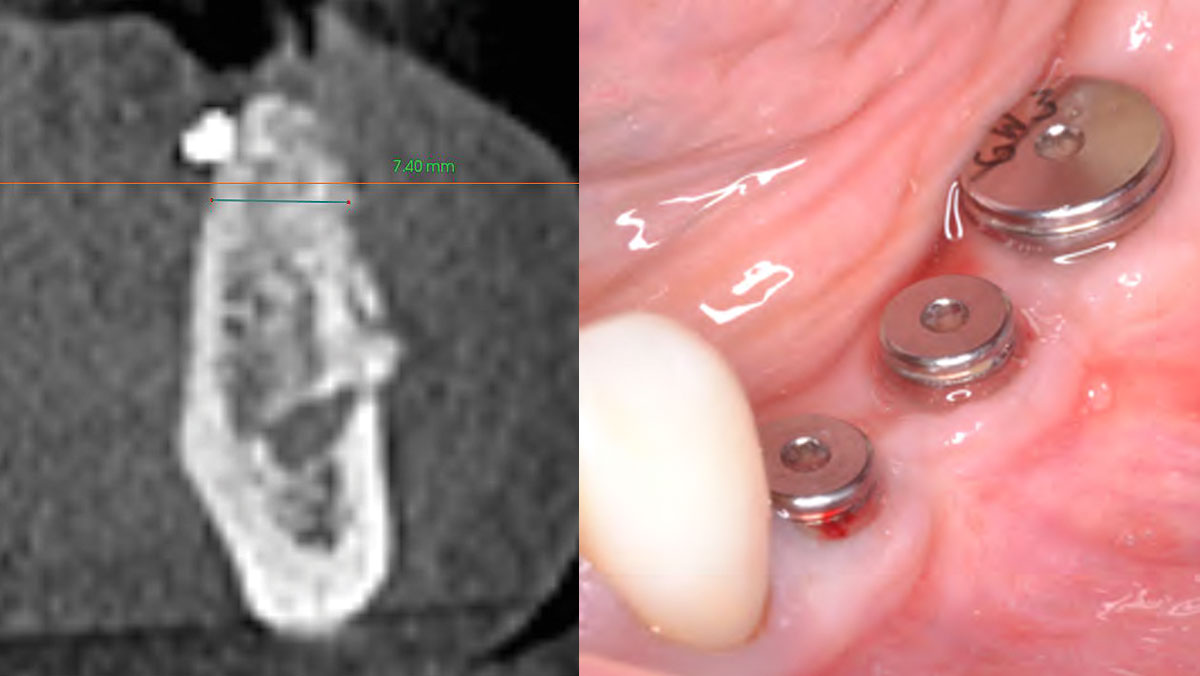
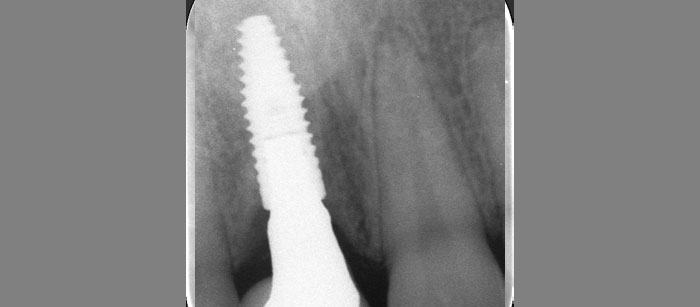
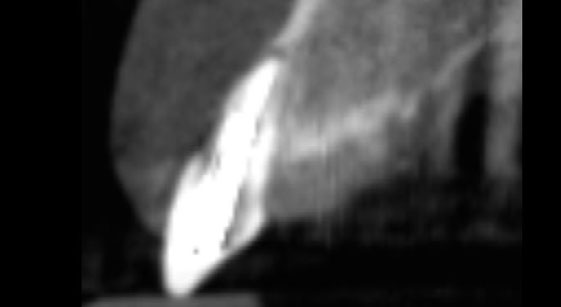
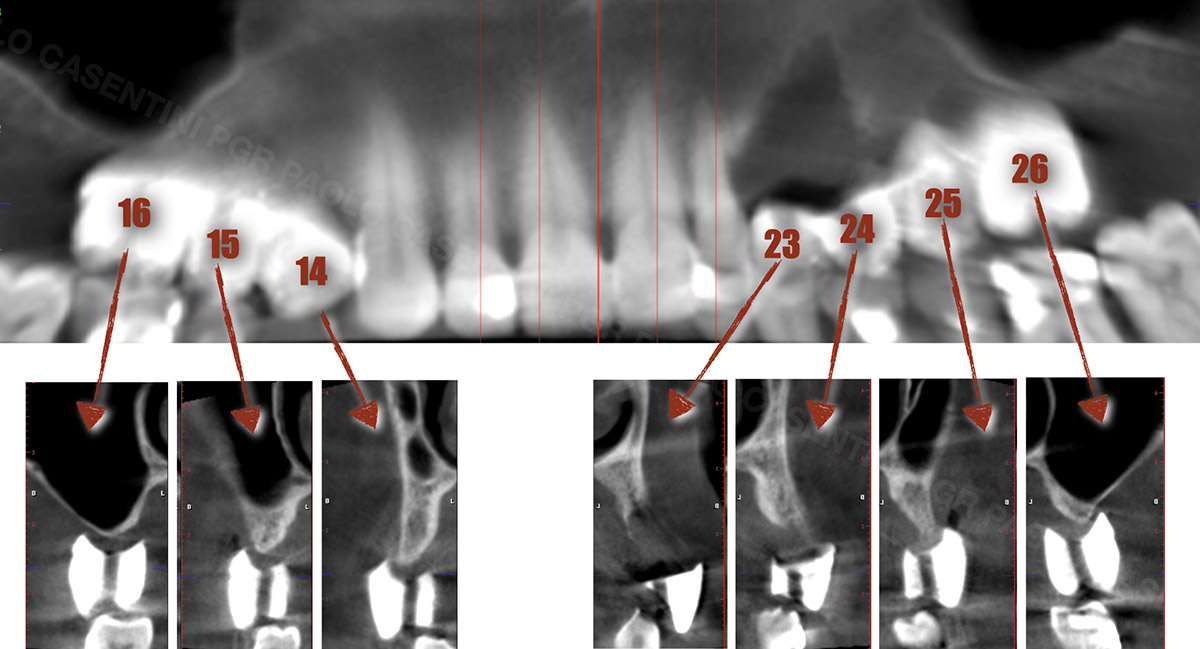
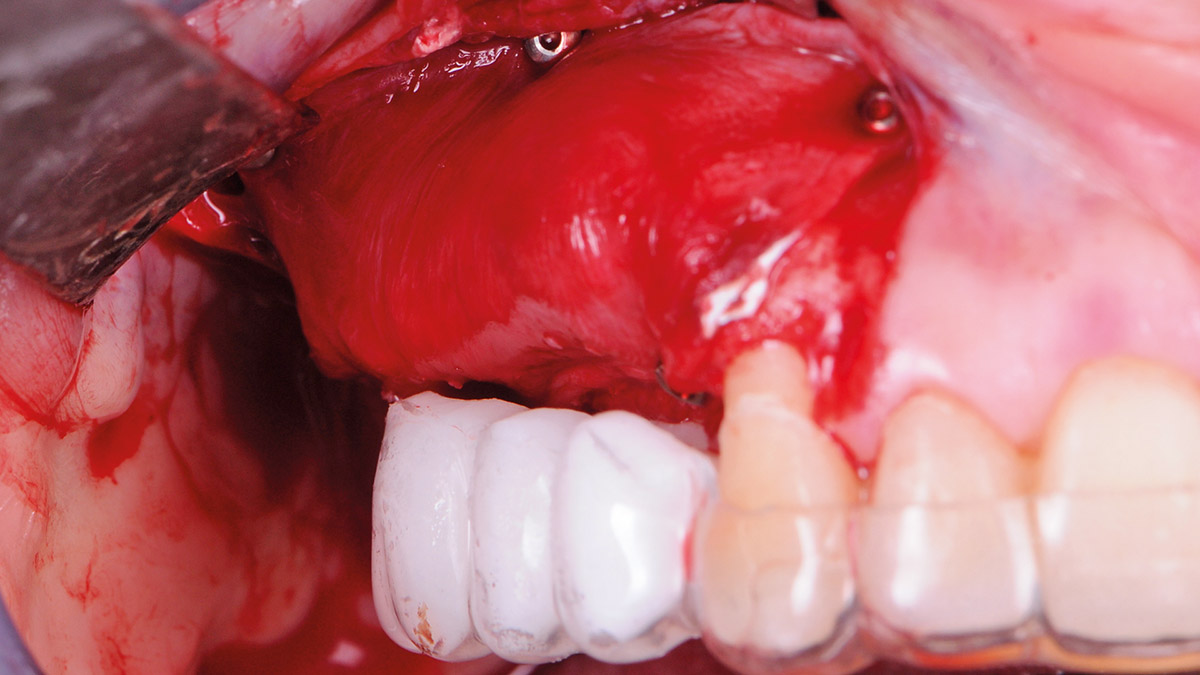
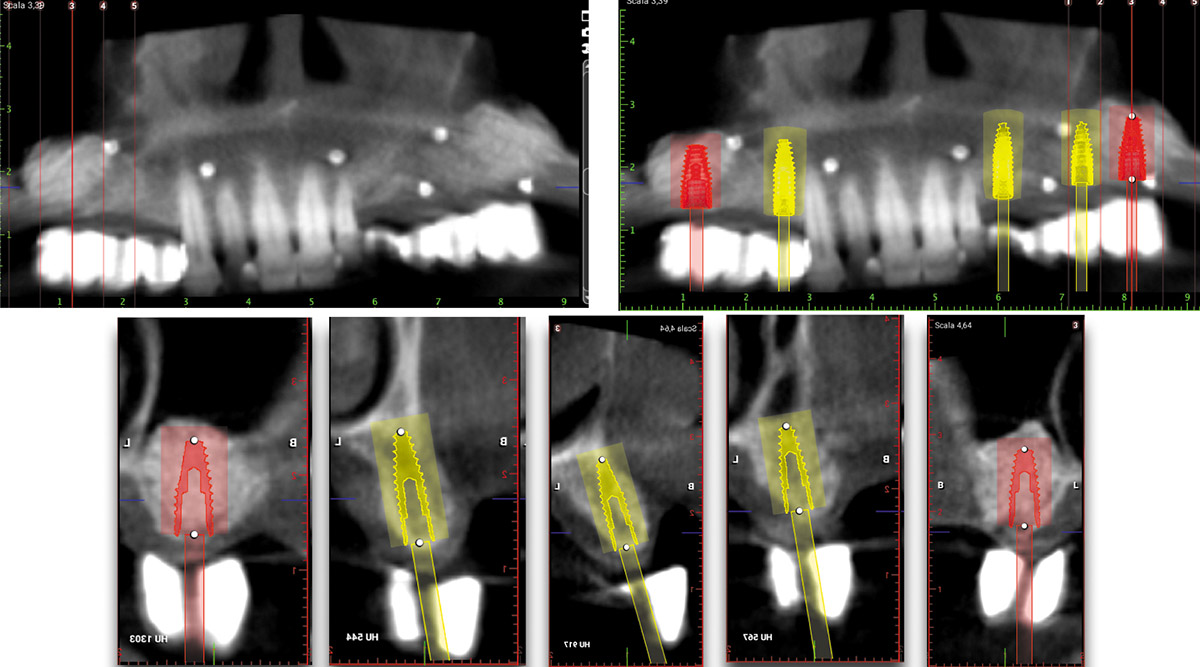
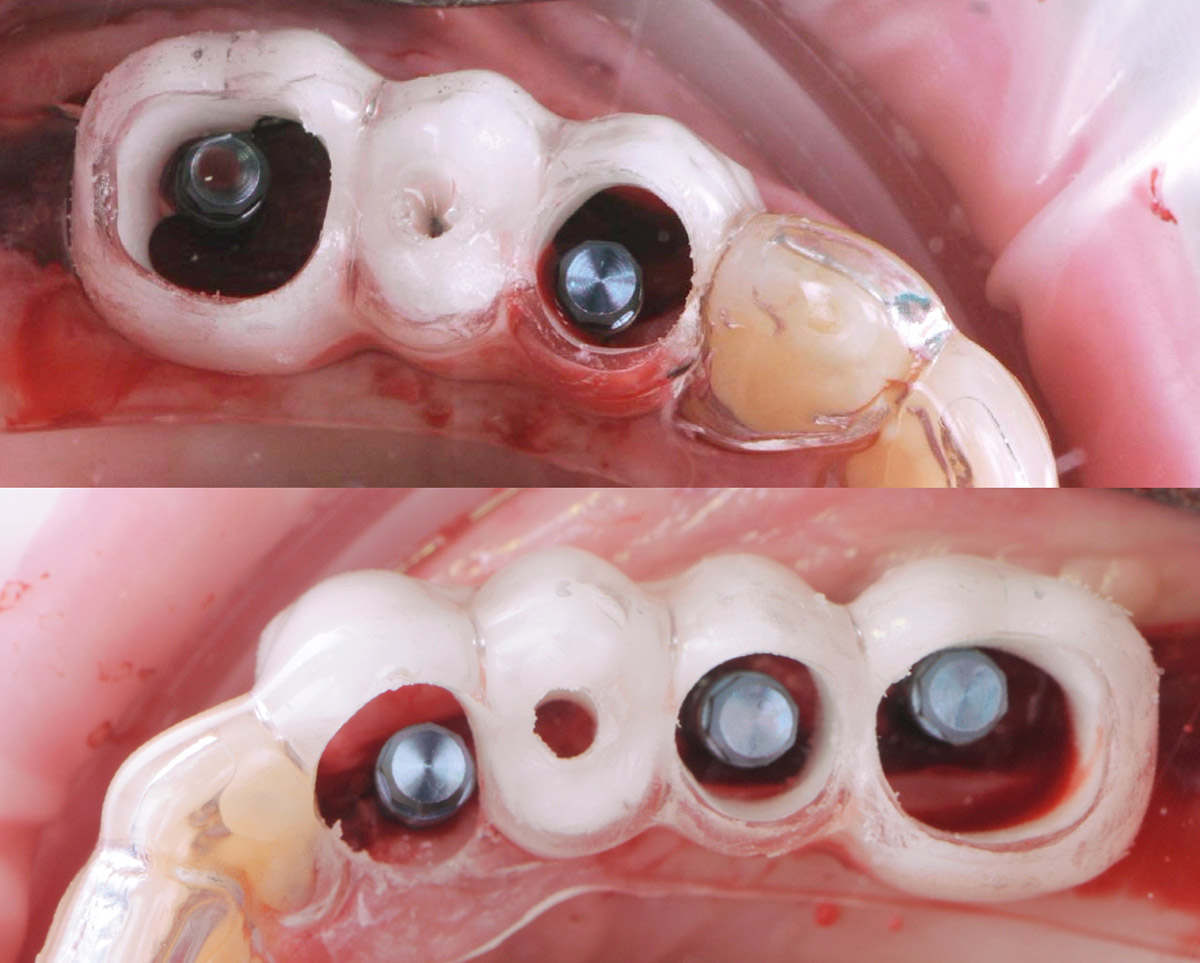
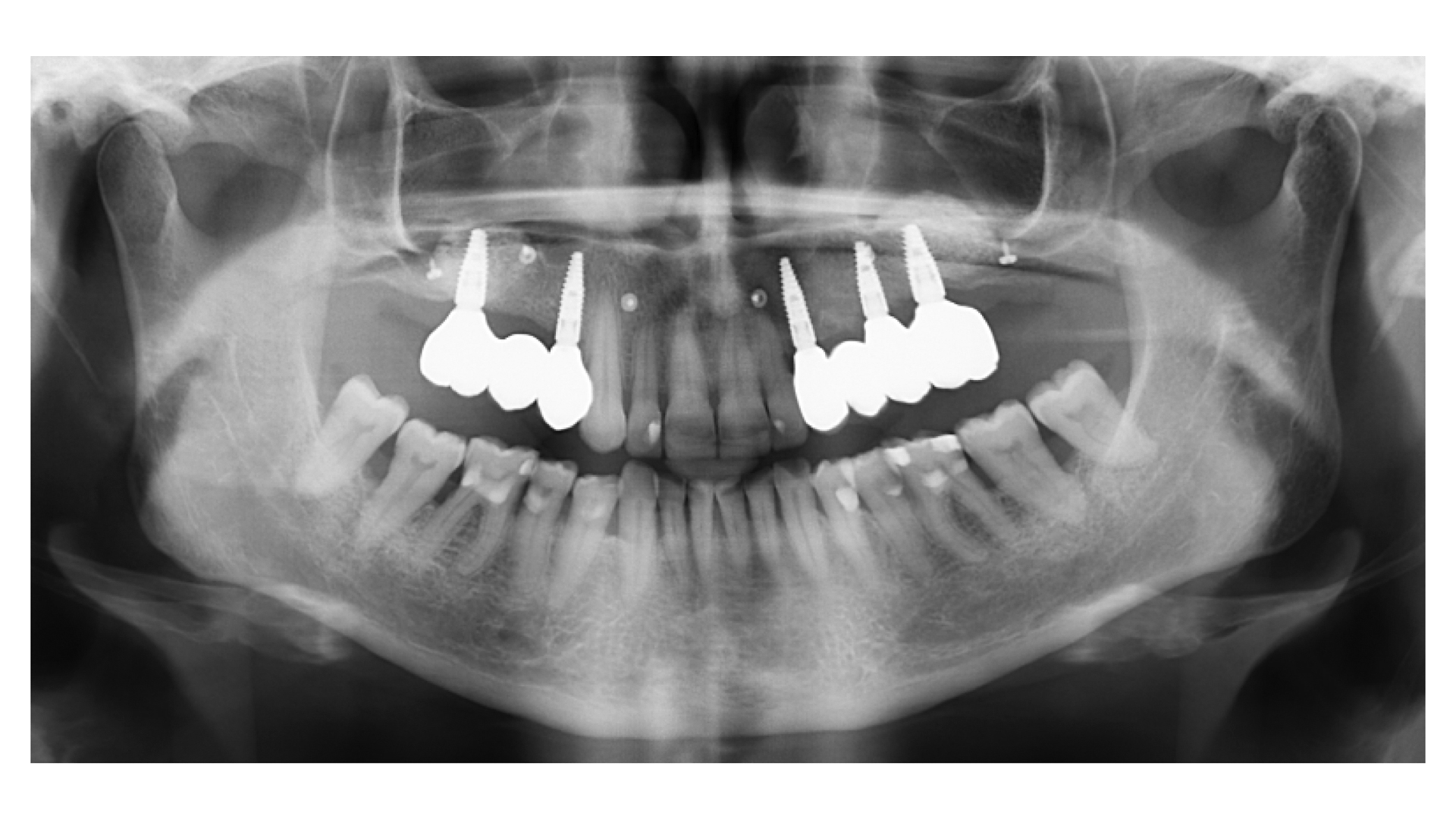
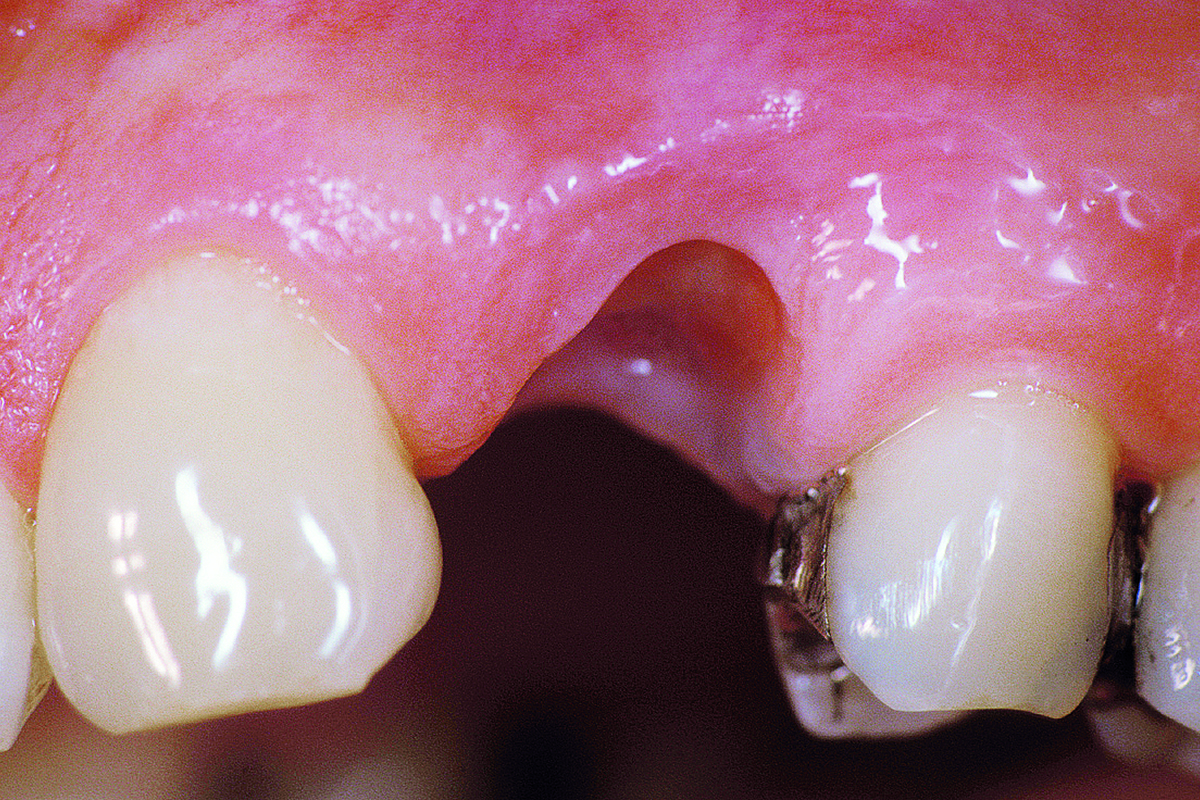
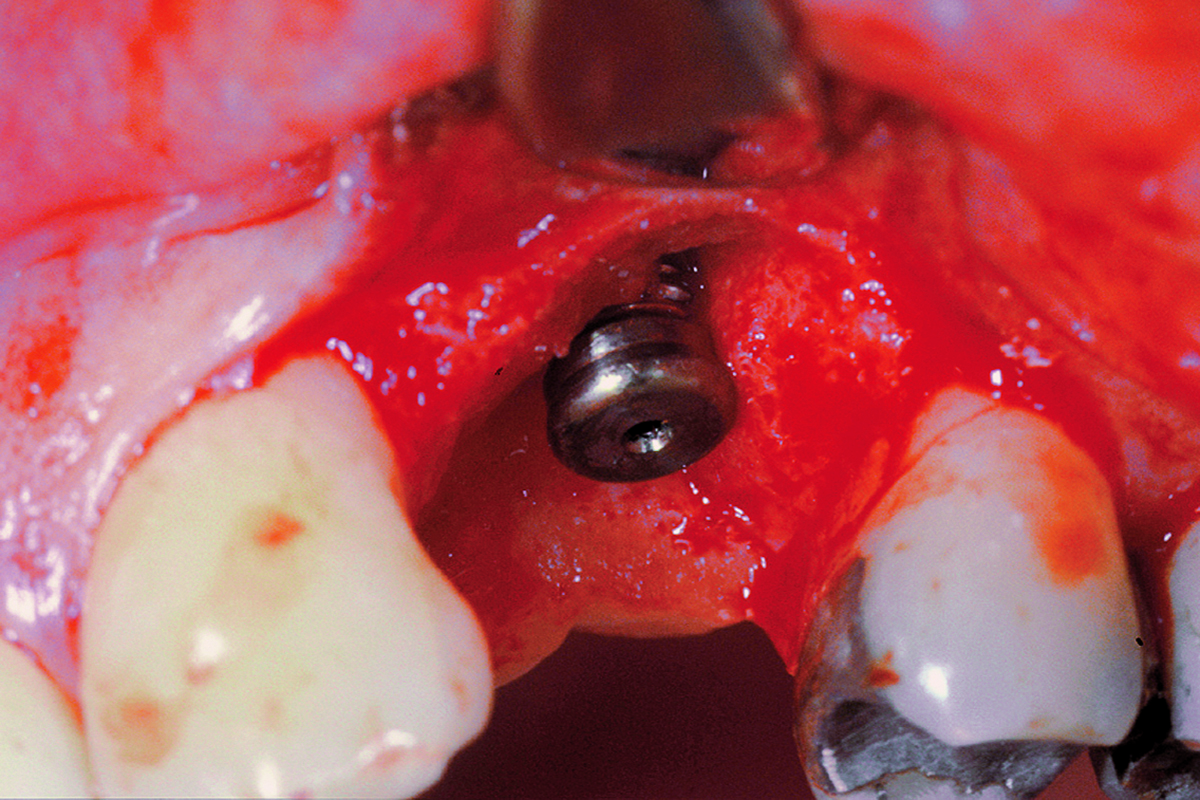
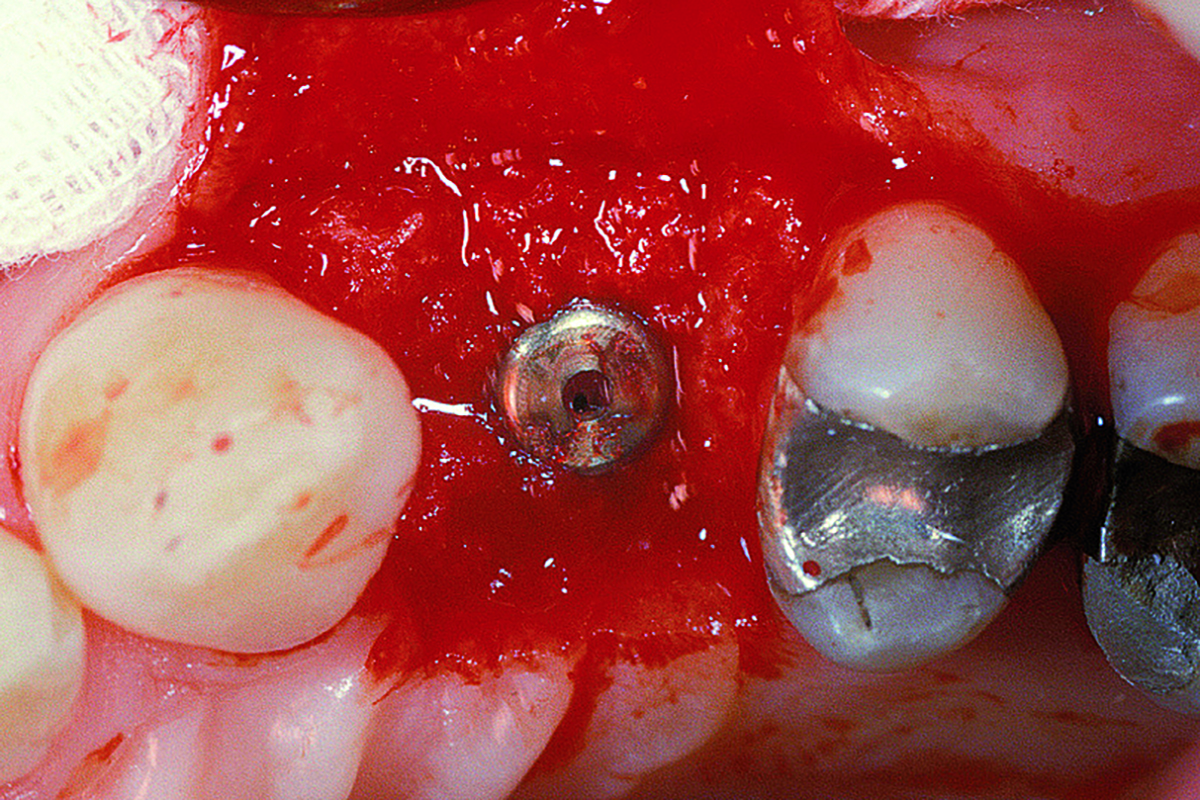
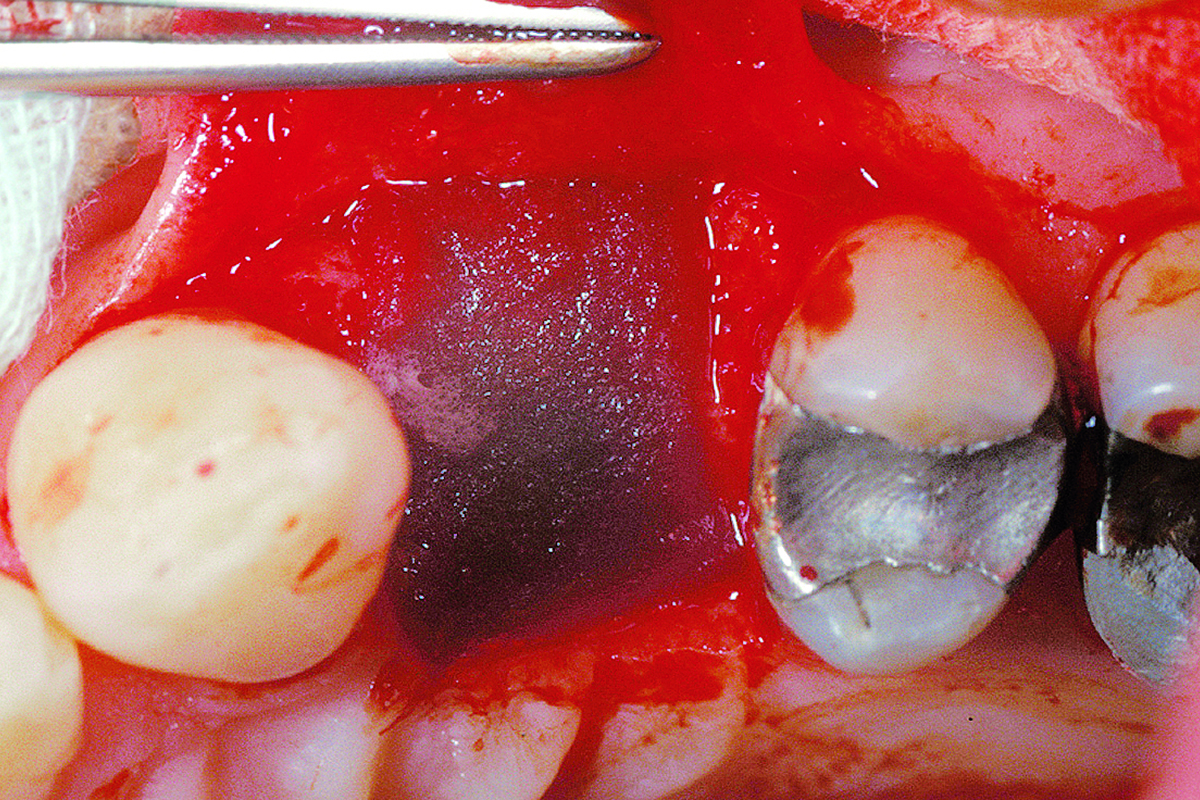
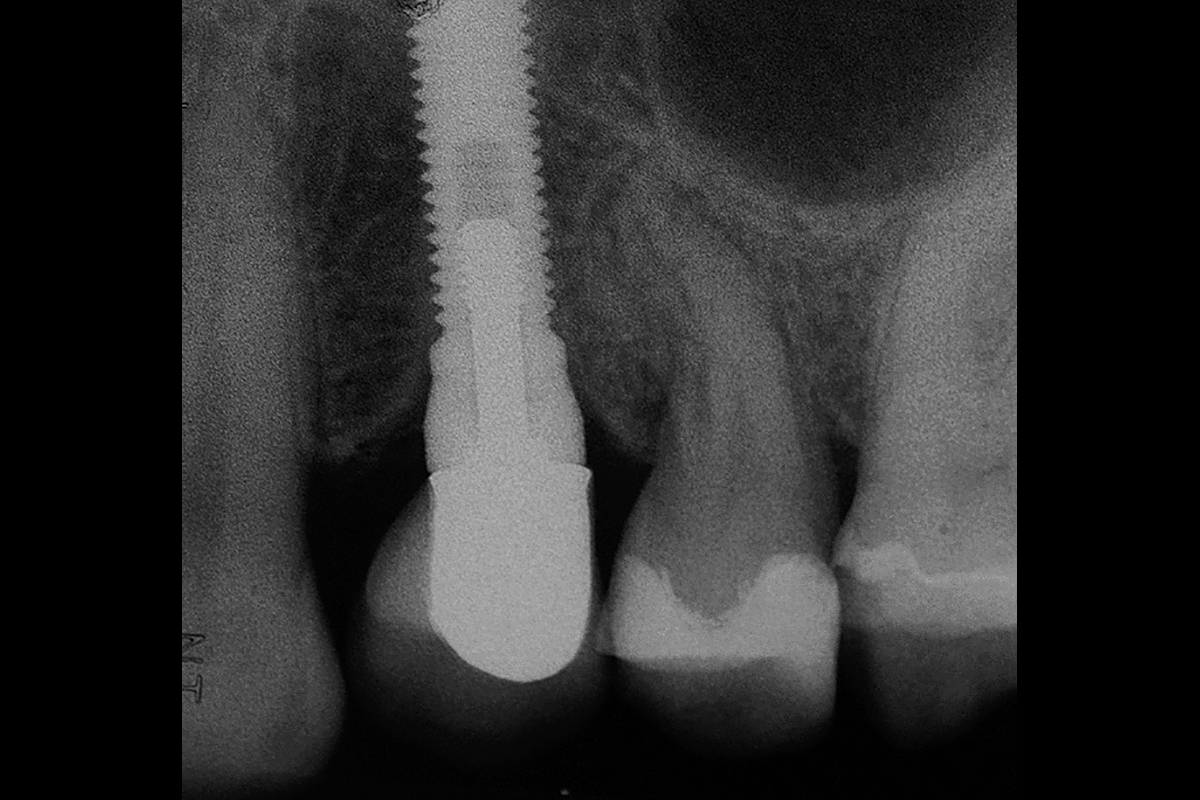
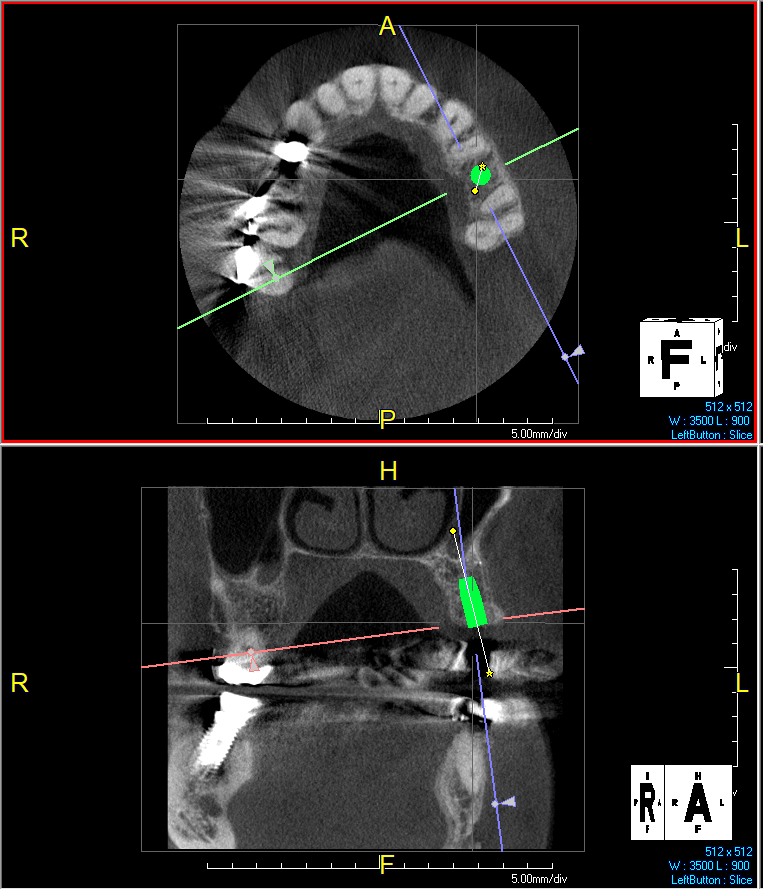
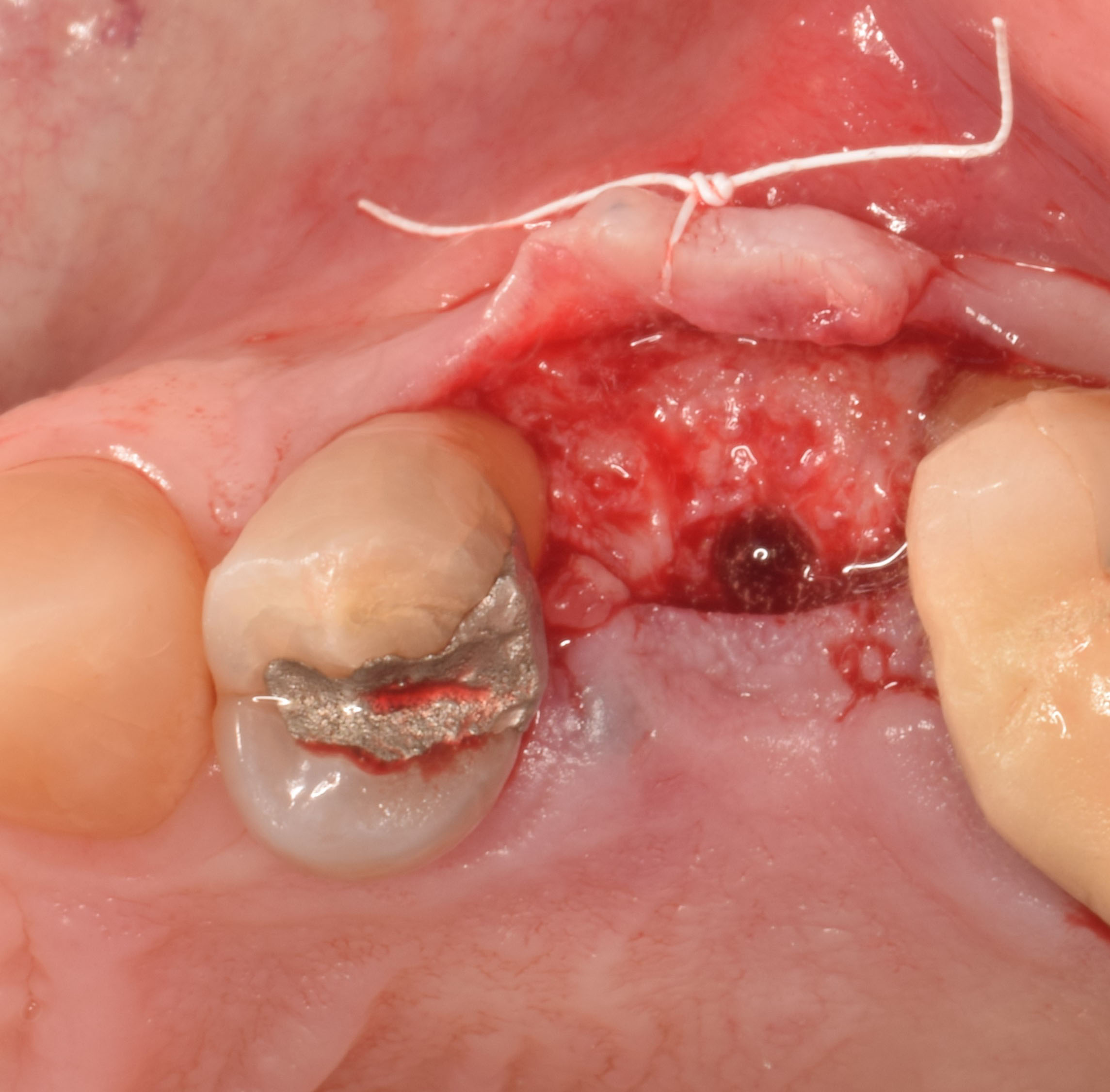
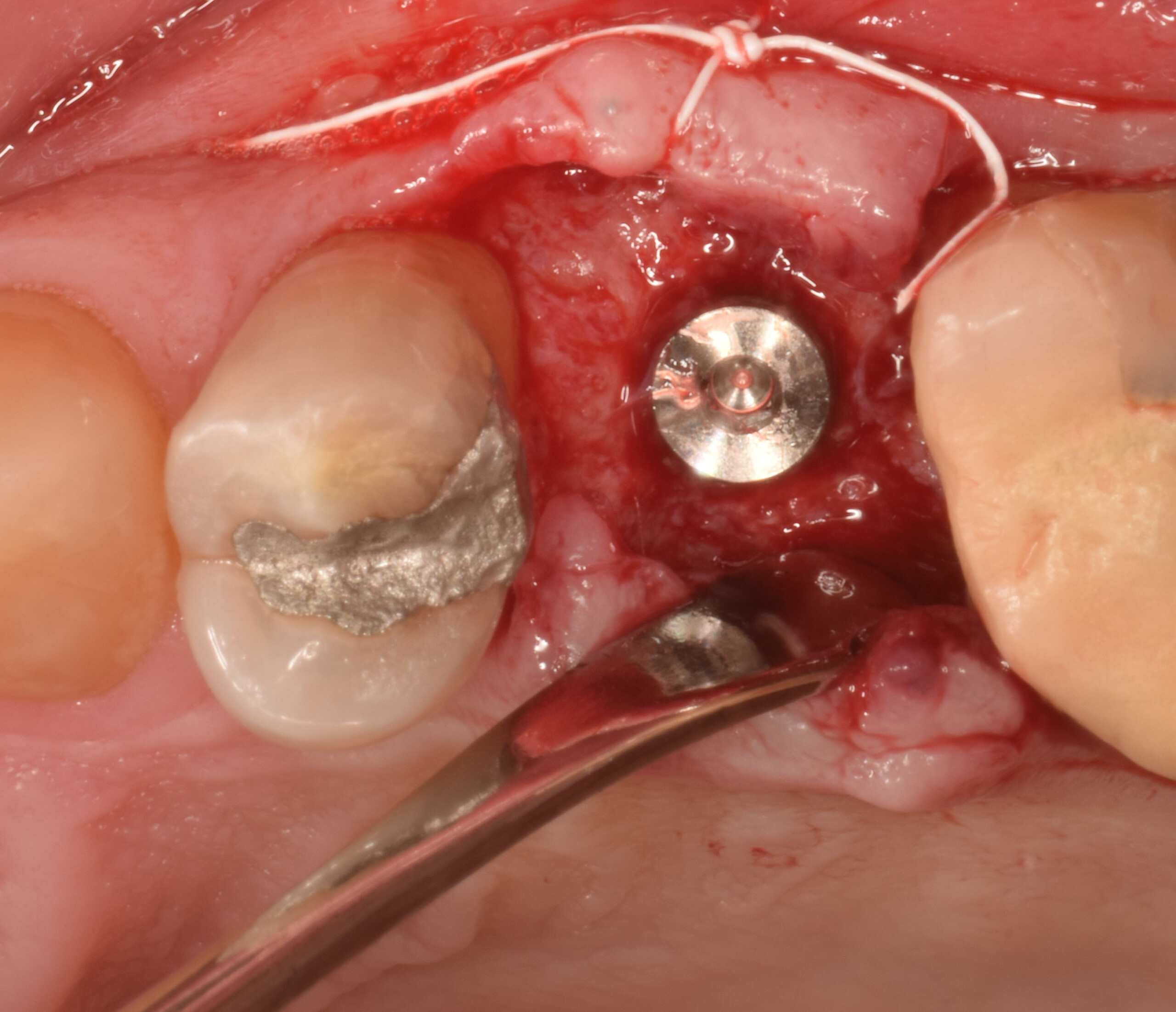
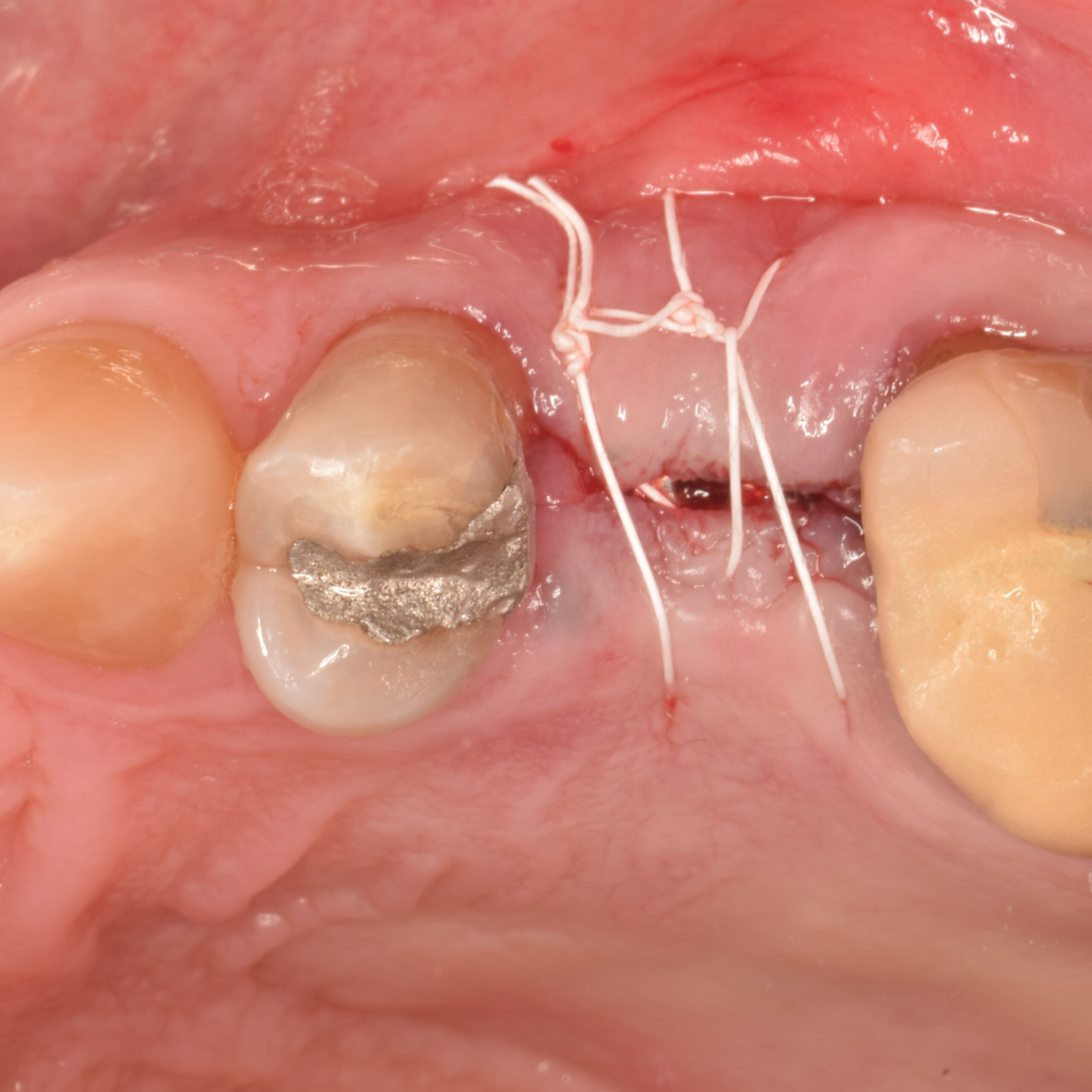
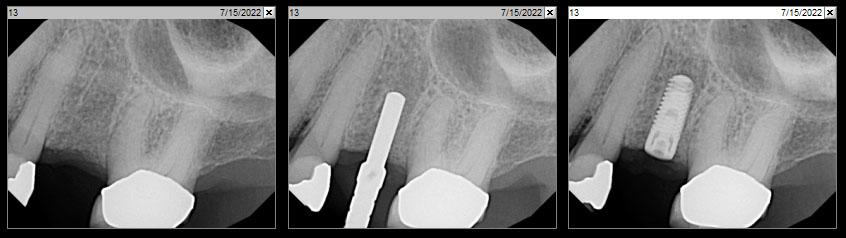
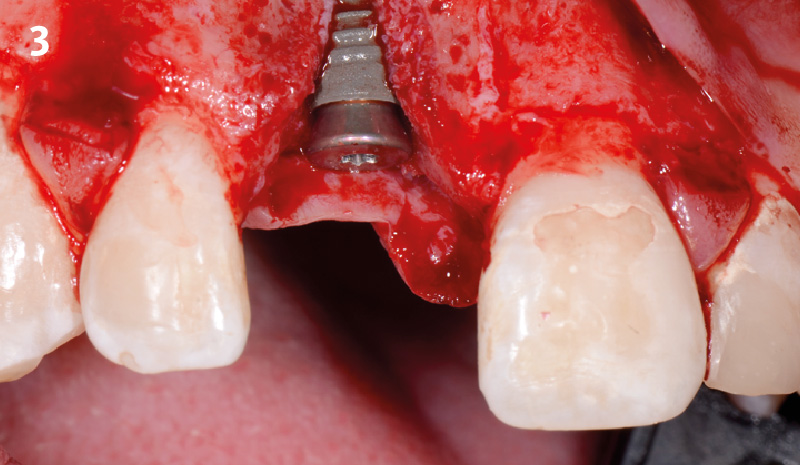
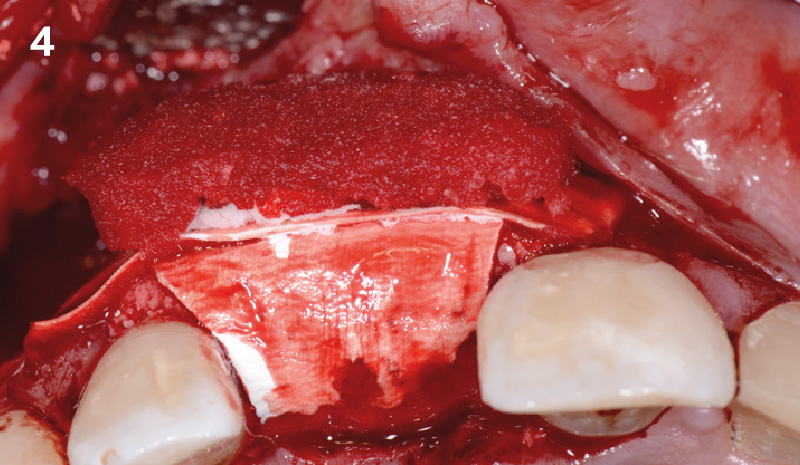
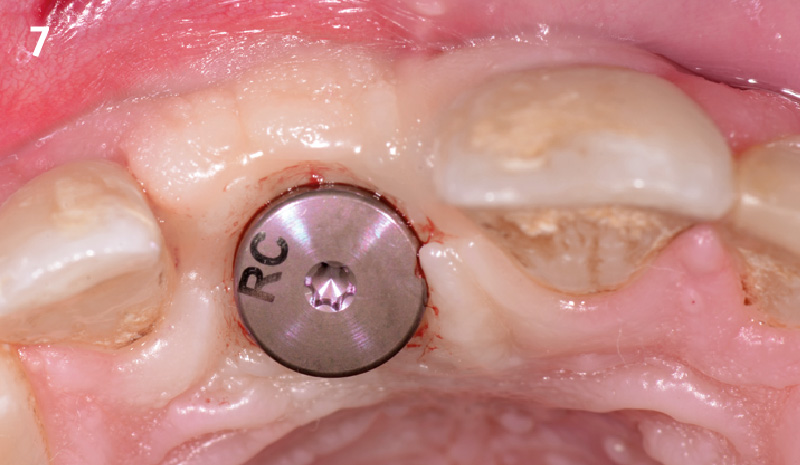
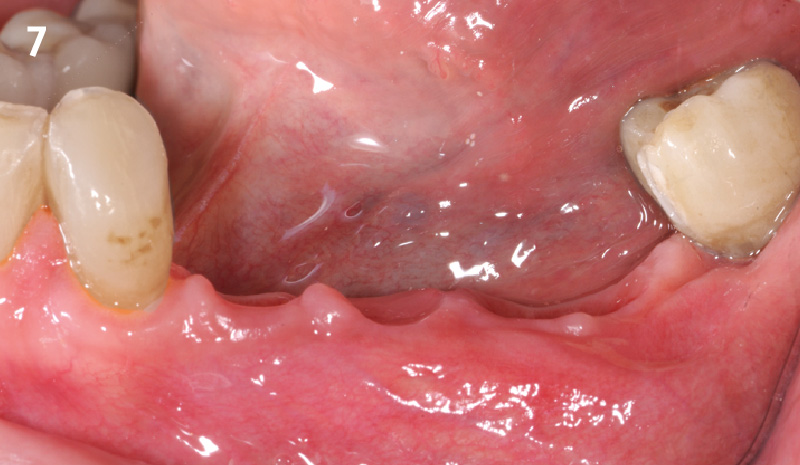
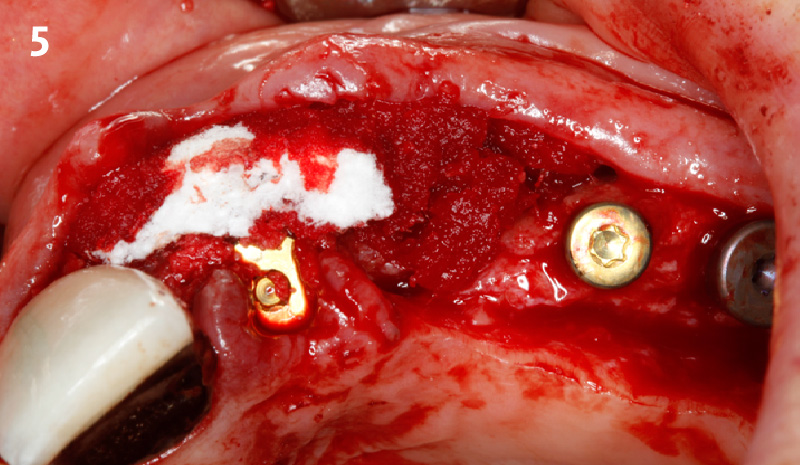
At 6 months, healing was complete with a bone fill of 10x10x6.5 mm. Tooth #7, affected by the combined defect, was fully regenerated. The adjacent ridge defect was also restored, enabling the placement of a regular-sized implant without the need for additional grafting.