NEW EBOOK: How to Master Bone Regeneration with Digital Innovation. Download Today!
Product: Geistlich Mucograft®

WEBINAR

BIOBRIEF
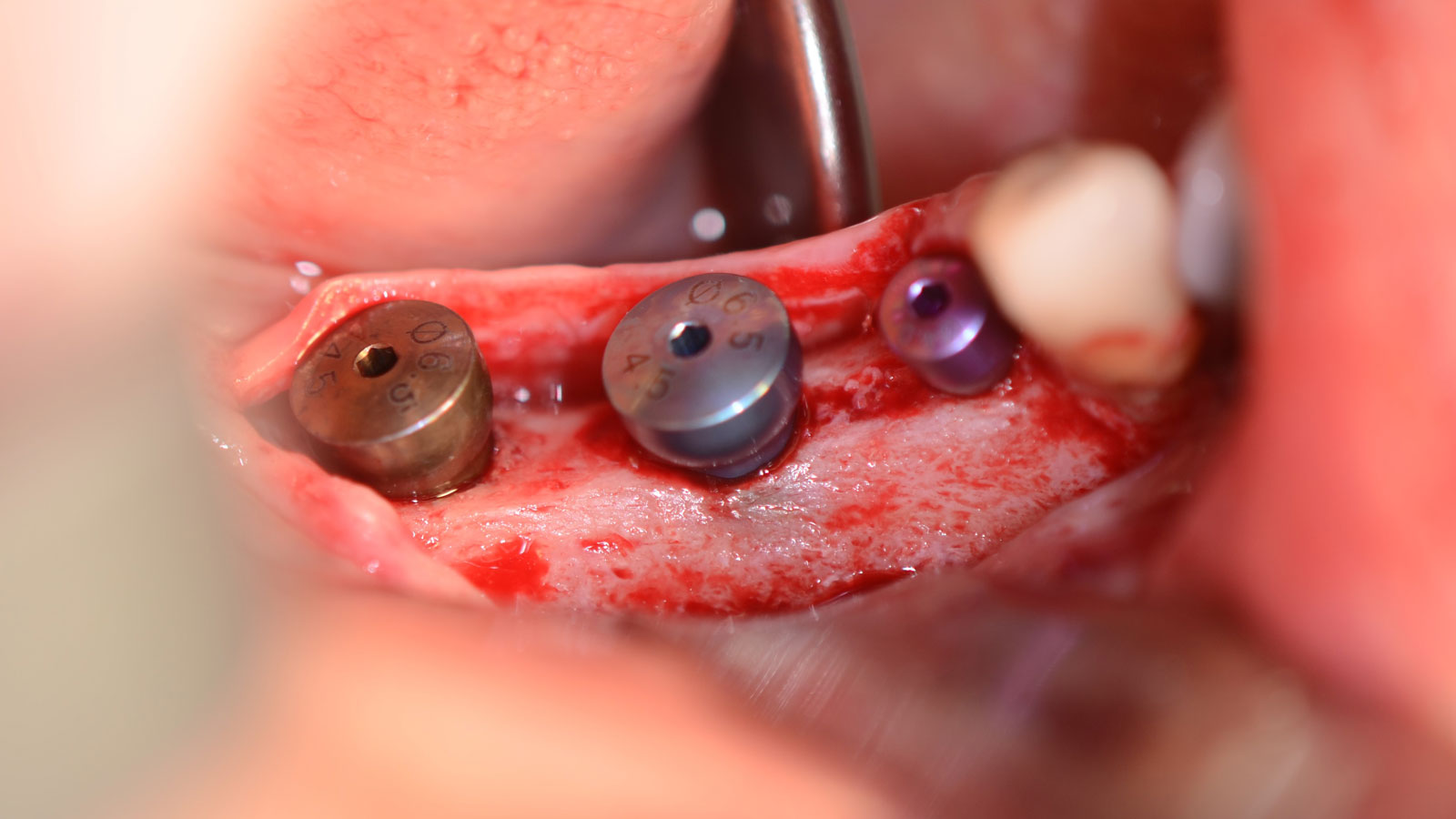
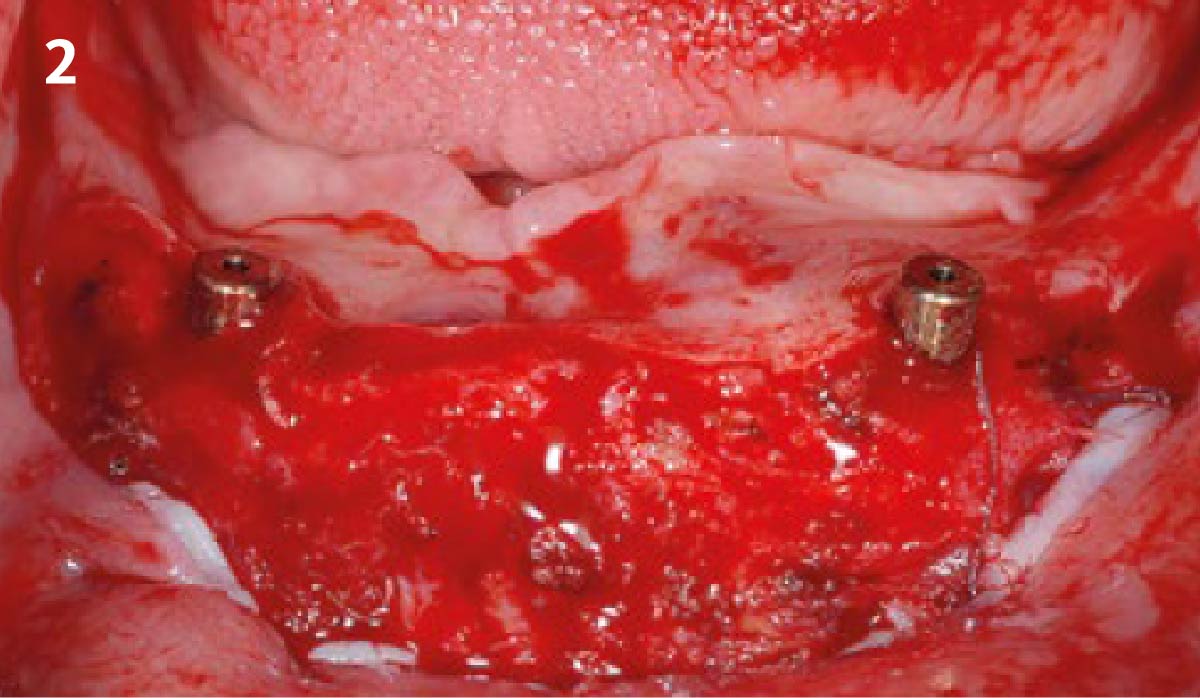
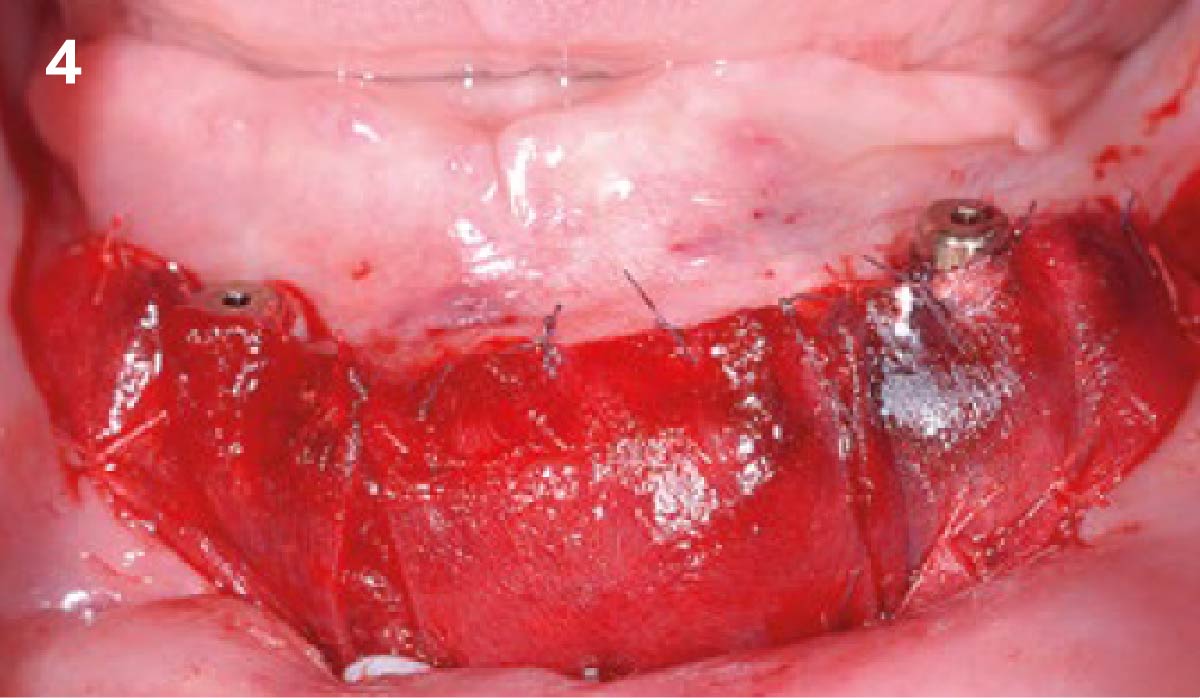
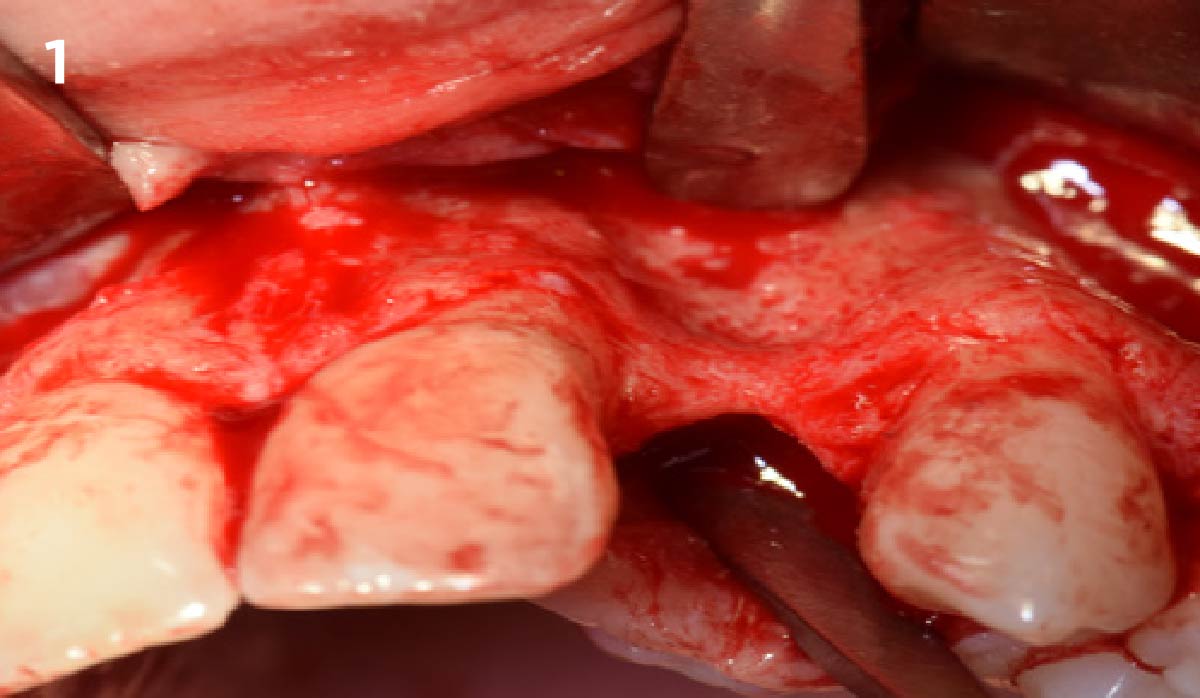
Mandibular Alveolar Ridge Split with Delayed Implant Placement


THE SITUATION
A healthy (ASA 1) non-smoker 63-year-old female presented to my office with Kennedy Class II partial edentulism in the mandibular right posterior quadrant for several years. She denied removable options and wanted dental implants to individually replace her missing teeth. The clinical and radiographic evaluation revealed atrophic mandibular bone height and width at site #’s 29, 30 & 31. The edentulous site required engineering prior to the placement of conventional dental implants and prosthetics.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system/Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The goal is to provide adequate soft and hard tissue at edentulous site #’s 29, 30 & 31 in order to place dental implants and restore a stable balanced occlusion.
“The hard and soft tissue of the edentulous posterior mandible were inadequate to rehabilitate with dental implants.”
— Dr. Gregory Santarelli
THE OUTCOME
The patient summarized this challenging case very well – “I never imagined I would have fixed teeth again.” Geistlich Bio-Oss® and Geistlich Mucograft® allowed for retention of the hard and soft tissue volume to achieve our final result and for maintenance of the final prosthesis.


Gregory A. Santarelli, DDS
Dr. Santarelli earned his DDS degree in 1998 from the University School of Dentistry, Milwaukee, WI, after graduating with his B.S. in Biology from Arizona State University (Tempe, AZ). In 1999, he completed his General Practice Residency at the University of Iowa Hospital and Clinics, and went on to an Oral & Maxillofacial Surgery Internship at the Medical College of Virginia (Richmond, VA) as well as an Oral & Maxillofacial Surgery Residency Program, Christiana Care Health System (Wilmington, DE).
After completing his formal training in 2004, Dr. Santarelli’s work experience includes the Bankor Hospital for Children, Cambodia (2003), Adjunct Clinical Professor, University of Marquette, School of Dentistry, Department of Oral Sugery, Marquette, WI (2005), and Oral Surgery Associates of Milwaukee, Milwaukee, WI (2004-2005). He now maintains a private practice in Kenosha, WI with his partner Dr. Deno Tiboris.
Dr. Santarelli performs numerous hard/soft tissue regeneration surgeries in preparation for dental implants and is actively involved in clinical research with The McGuire Institute (iMc).

BIOBRIEF
Geistlich Mucograft® for the Treatment of Multiple Adjacent Recession Defects: A More “Palatable” Option


THE SITUATION
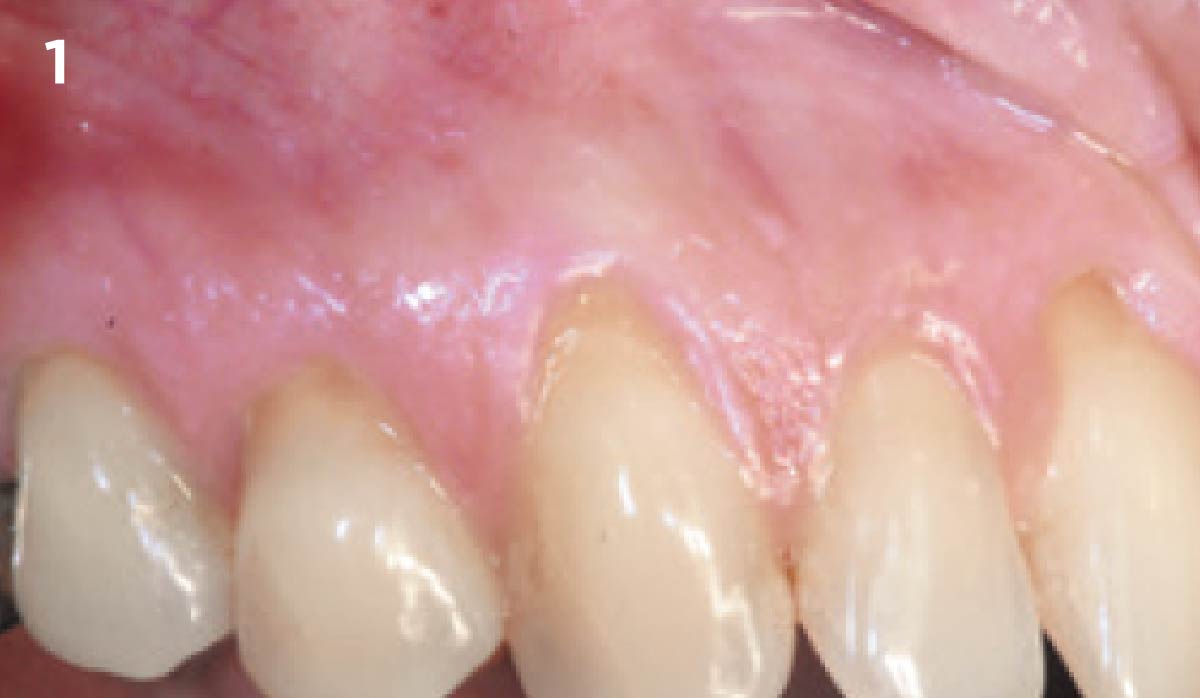
A 35-year-old male presented in my practice with a chief complaint of recession. Multiple buccal recession defects ranging 2-5 mm were noted by teeth #11-14 with a minimal amount of keratinized tissue on the buccal of #14. Bone levels were within normal limits with no loss of interproximal tissue observed. These recession defects are classified as Miller Class I recession defects. Typically, 100% root coverage is expected for recession defects of this type.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Bone defect(s) | Not present | Slight defect <2mm | Significant >3mm |
| Keratinized tissue | Adequate 5mm | Inadequate <5mm | Inadequate <3mm |
| Miller classification | Class I-II | Class III | Class IV |
THE APPROACH
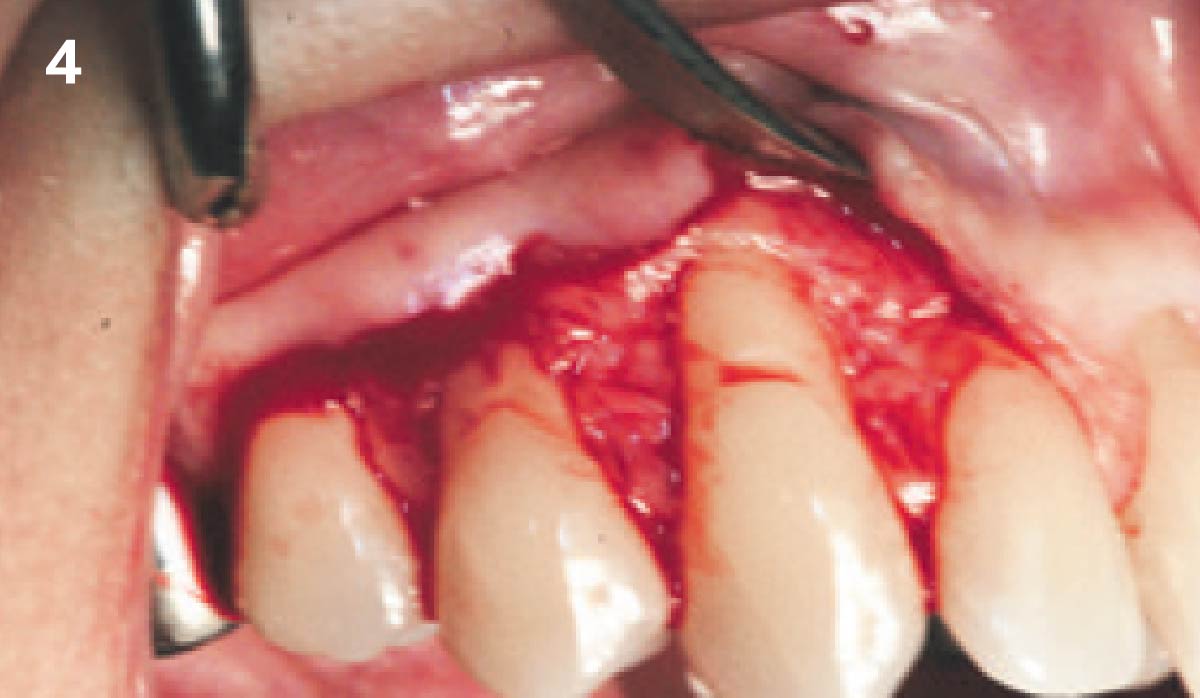
My treatment goals included completing root coverage of the recession defects and augmentation of the width of attached keratinized tissue by tooth #14. My patient had similar recession defects on teeth #3-6 which were previously treated with an autogenous sub-epithelial connective tissue graft. Instead of autogenous tissue grafting, Geistlich Mucograft®, a xenogenic collagen matrix, was used in conjunction with a coronally advanced flap.
“The patient was unhappy with the post-operative morbidity he
experienced as a result of the previous connective tissue graft.”
THE OUTCOME
This case illustrates the successful use of Geistlich Mucograft®, a xenogenic collagen matrix, for the treatment of multiple adjacent recession defects. Complete root coverage and an increase in the zone of keratinized tissue was obtained and a dento-gingival complex that is amenable to long-term health and stability was achieved. My patient was spared from the inevitable morbidities associated with a sub-epithelial connective tissue graft from a palatal donor site.


Dr. Daniel Gober
Dr. Daniel D. Gober received his DDS from SUNY Stony Brook School of Dental Medicine in 2010. He completed his residency in periodontics and implantology at Nova Southeastern University. Dr. Gober is board certified by the American Academy of Periodontology and is a Diplomate of the International Congress of Oral Implantology. He is also certified in the administration of IV sedation and specializes in soft-tissue procedures around both natural teeth and implants. He currently practices in Cedarhurst, NY at South Island Periodontics & Implantology, PLLC.

BIOBRIEF
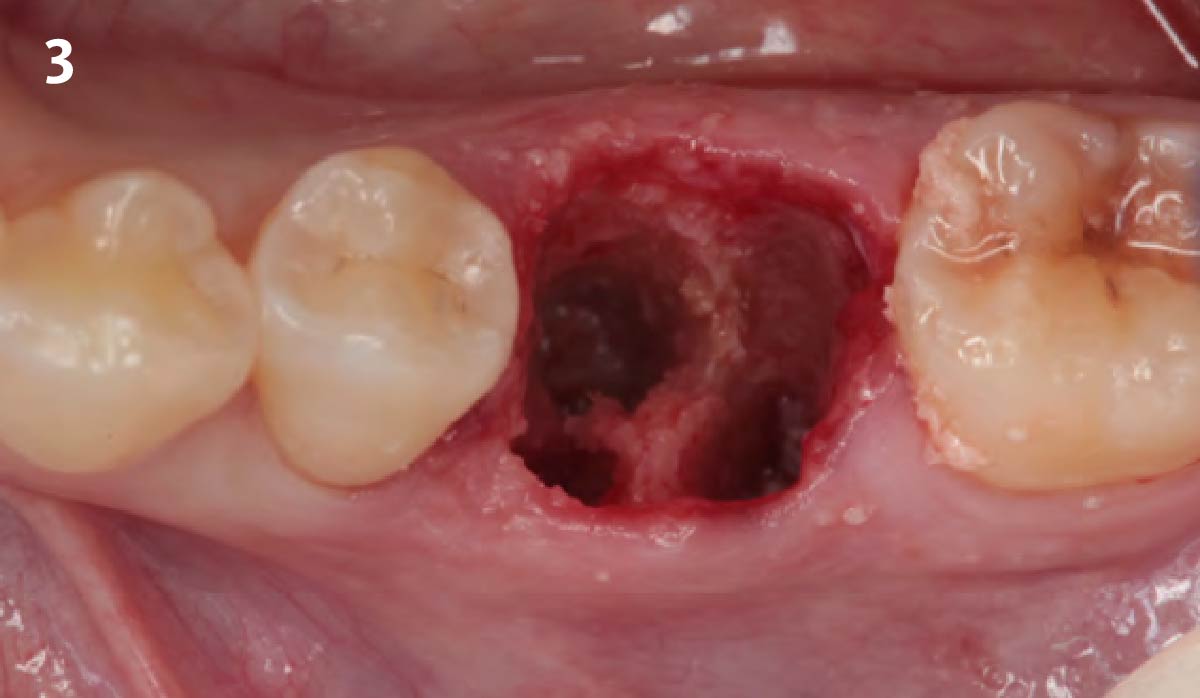
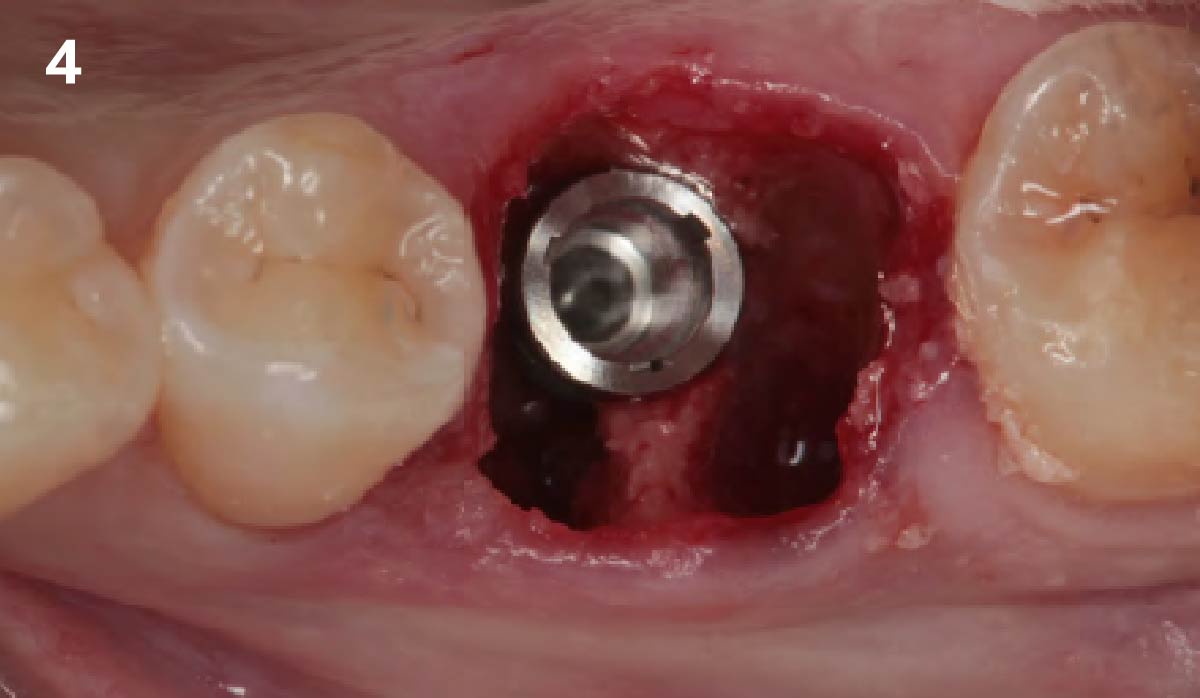
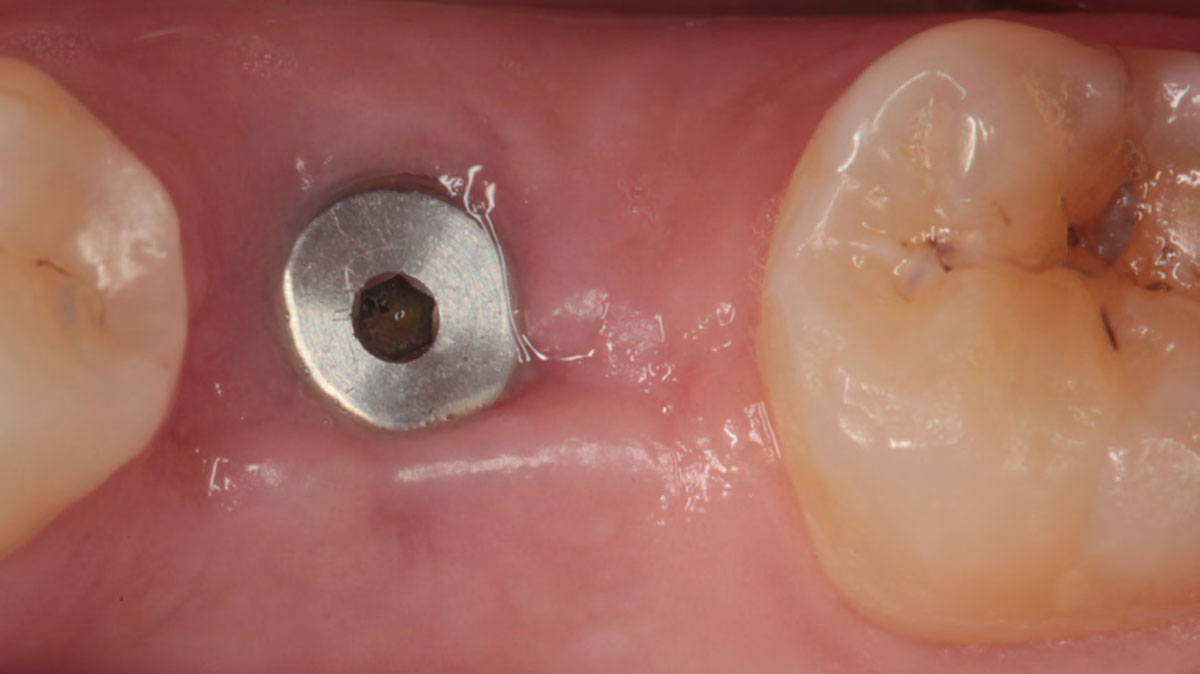
Immediate Mandibular Molar Transition


THE SITUATION
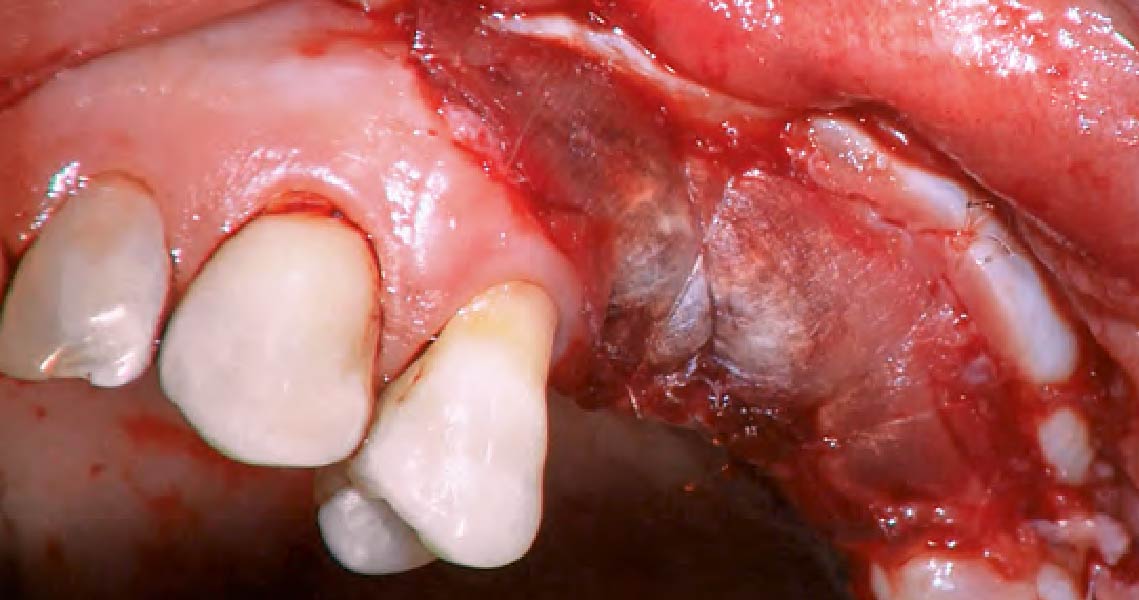
The case here is typical enough, a failing mandibular molar with a vertical sub-osseous fracture. Traditionally, the replacement process can take three or more surgical exposures (extraction and regeneration), (implant placement), (second stage exposure) and more than a year of therapy.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
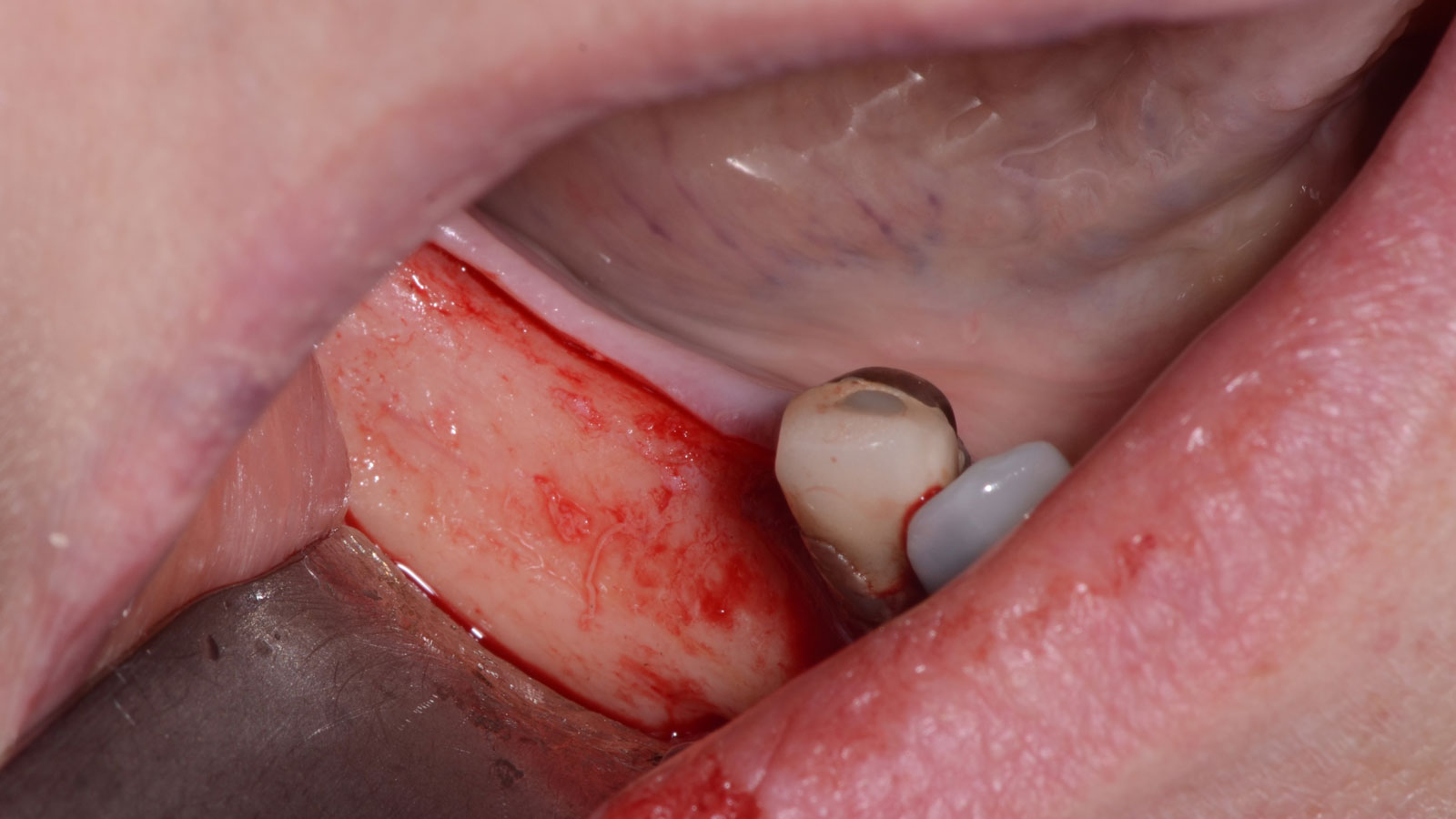
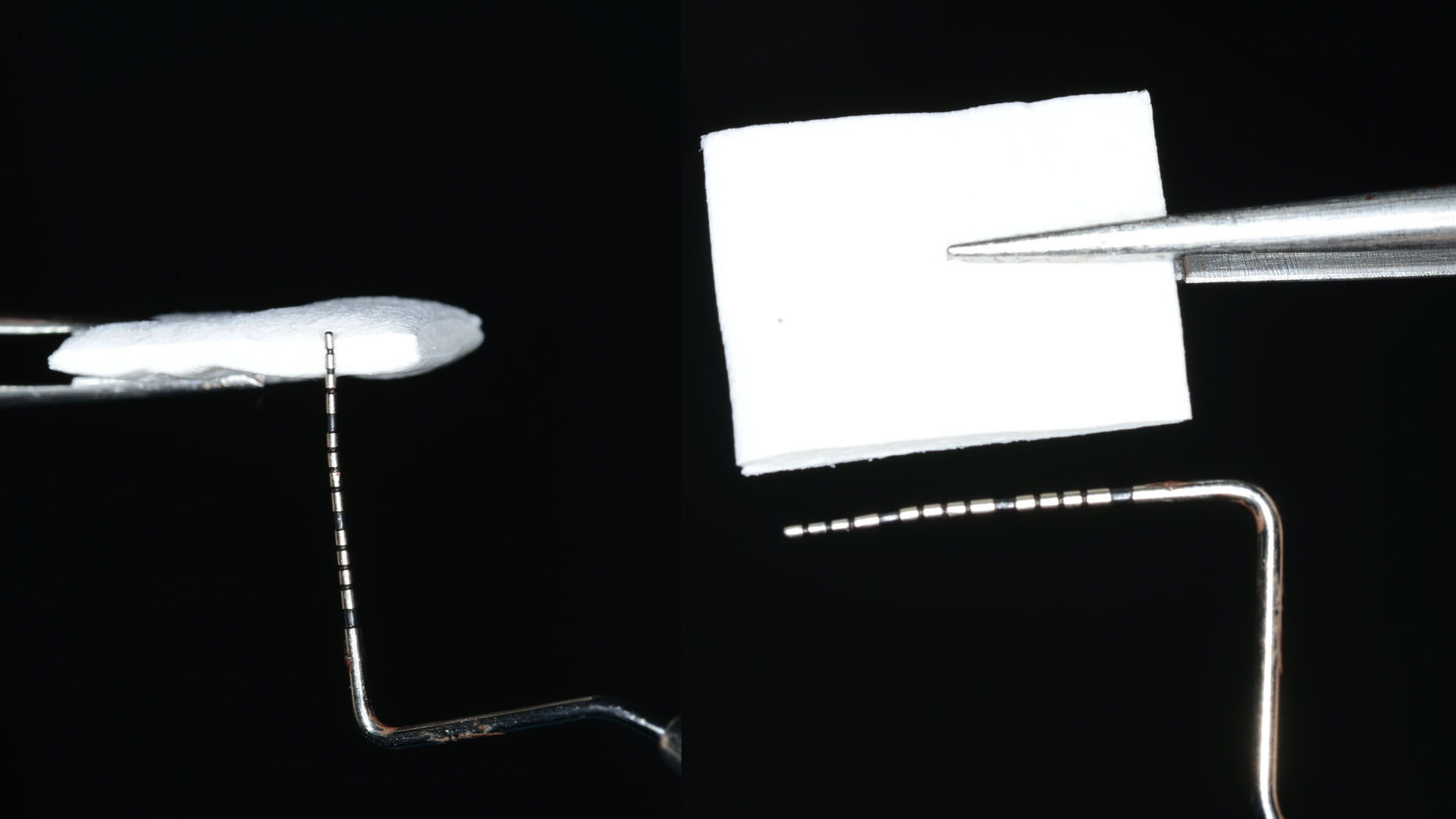
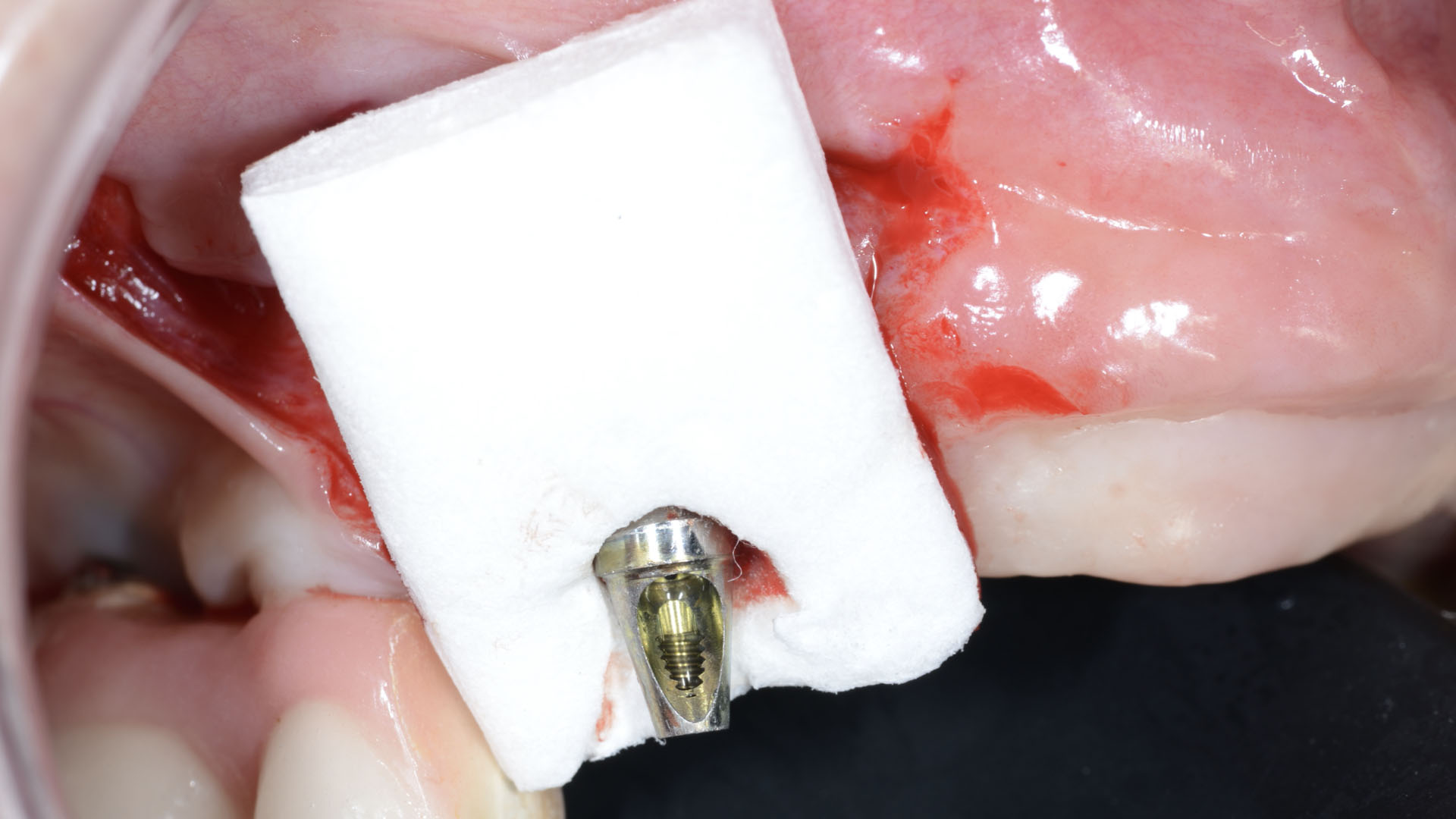
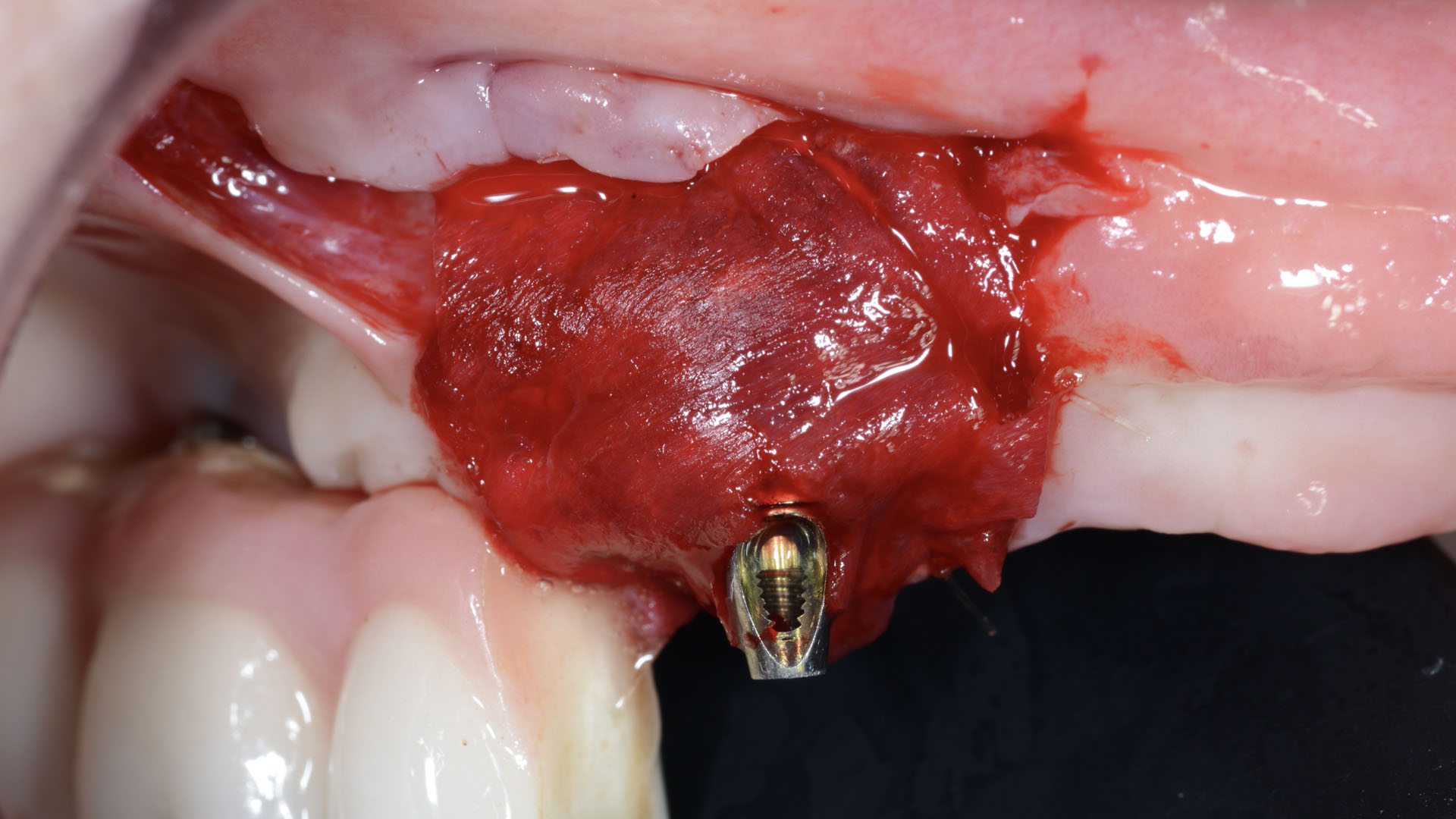
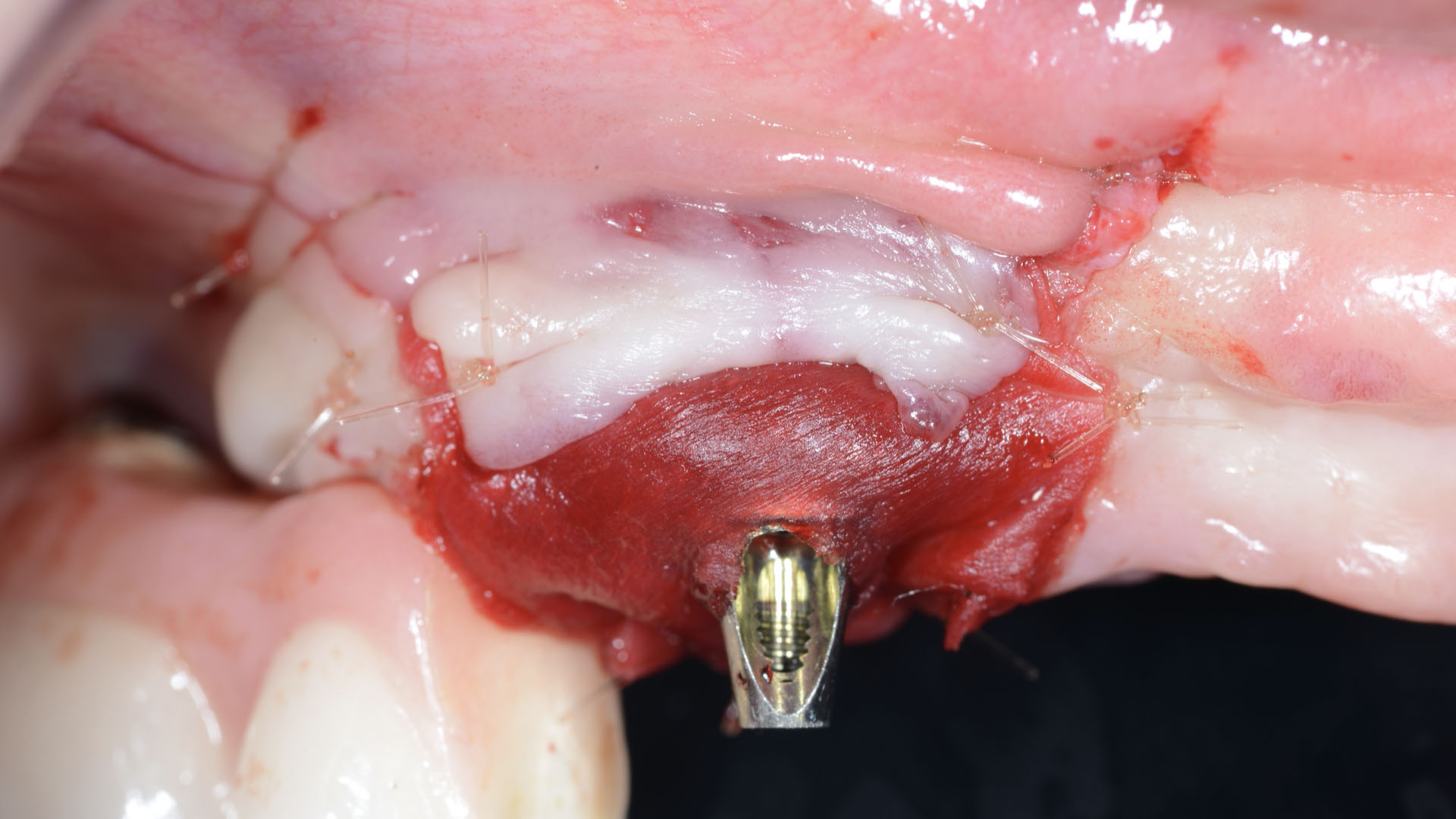
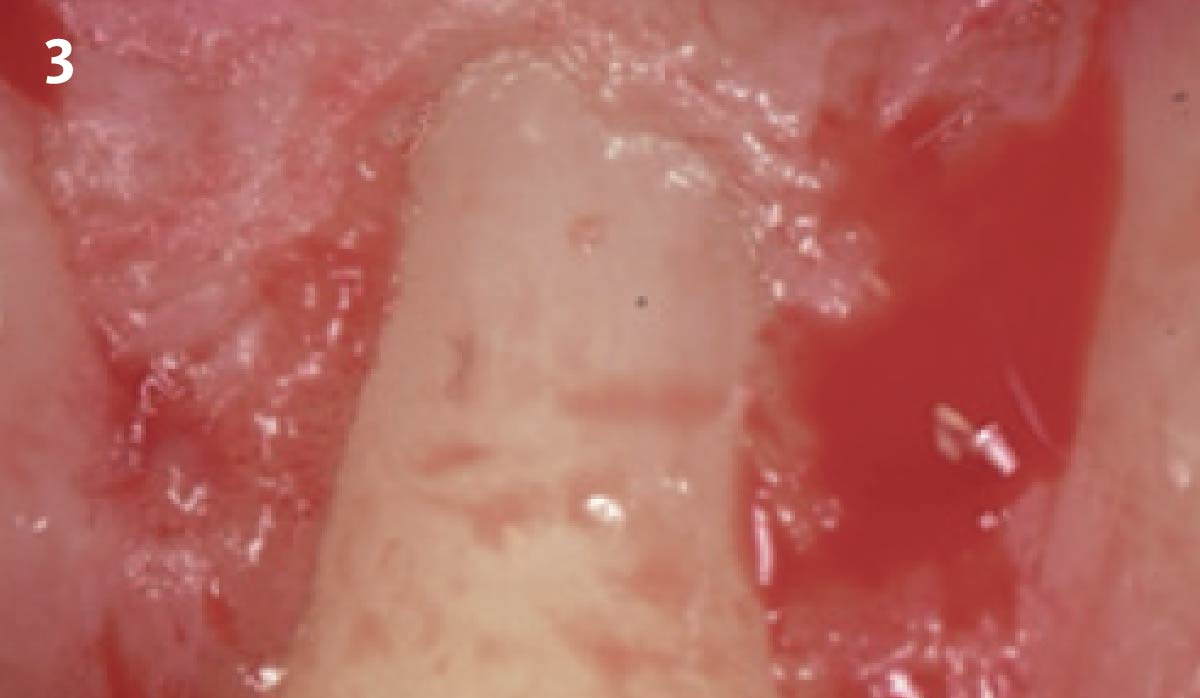
Immediate molar replacement requires atraumatic removal of the fractured tooth, careful socket debridement and development of a channel for an ideally positioned implant. The implant then needs to be placed down in the bone channel with the implant platform positioned just below the socket walls. It needs to be stable. Channel deficiency augmentation is achieved with Geistlich Bio-Oss Collagen® which is covered with a collagen matrix, Geistlich Mucograft® with the edges tucked under the gingival margins and sealed over with tissue glue.
“The patient desires an implant placement for a fractured mandibular molar, as fast as possible.”
– Dr. Peter Hunt
THE OUTCOME
This single stage replacement protocol has proven to be simple, safe and highly effective providing the socket is fully degranulated and the implant is stable and not loaded in the early healing stages. It works well when a gingiva former is immediately placed into the implant instead of a cover screw, Geistlich Bio-Oss Collagen® is packed around the implant to fill the residual socket, then covered with a Geistlich Mucograft® and sutured. There is no need for flap advancement to cover over the socket.


Dr. Peter Hunt
After graduate training on an Annenberg Fellowship at the University of Pennsylvania, dr. hunt helped start up the University of the Western Cape dental School in Cape Town, South Africa. he returned to the University of Pennsylvania where in time he became Clinical Professor of Periodontics. later he helped start up Nova Southeastern‘s dental School where he was Professor of Restorative dentistry, Post Graduate director and director of Implantology. he has had a private practice in Philadelphia focusing on implant and rehabilitation dentistry since 1981.

BIOBRIEF
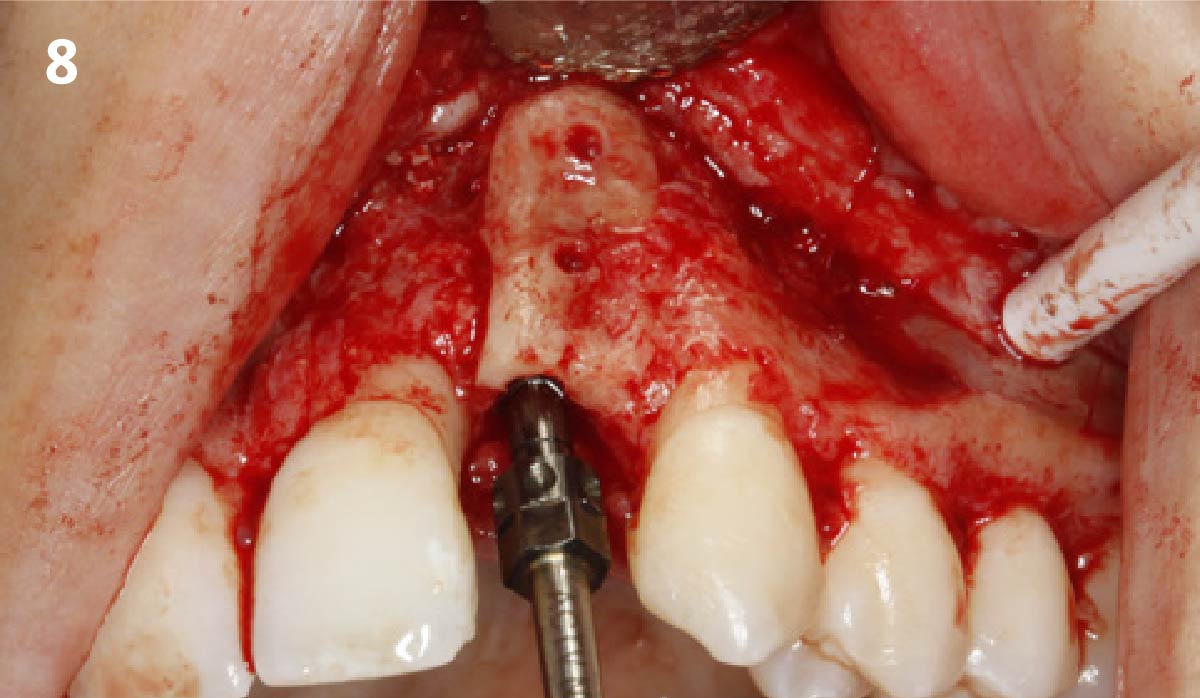
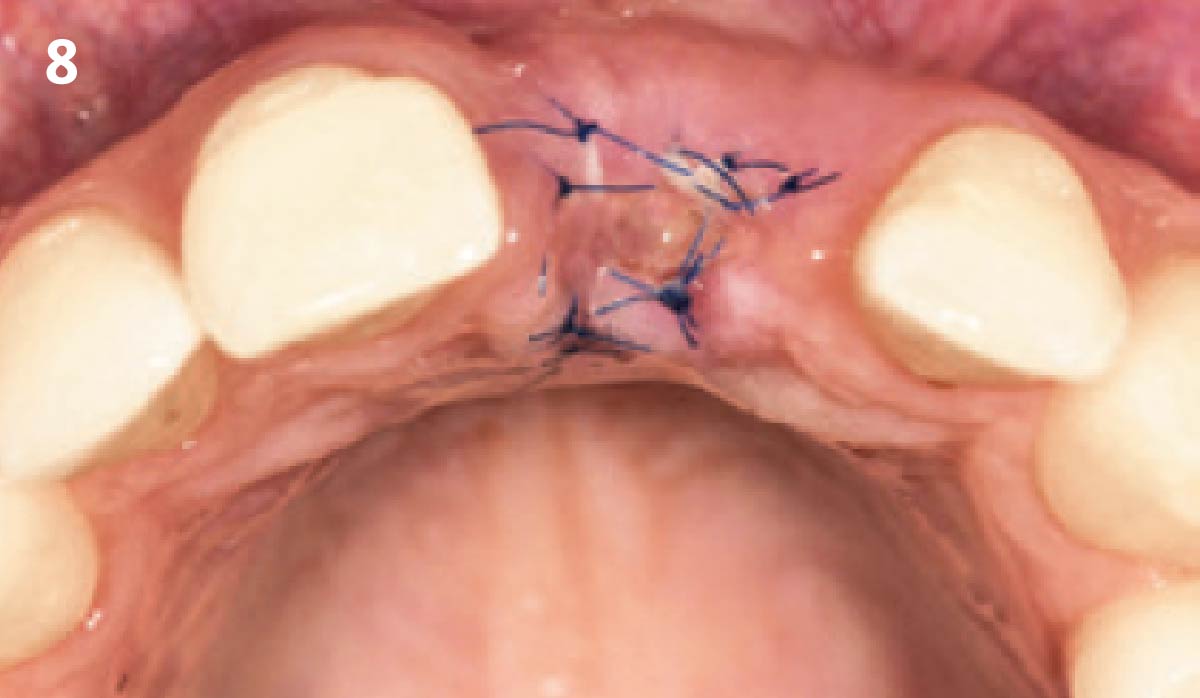
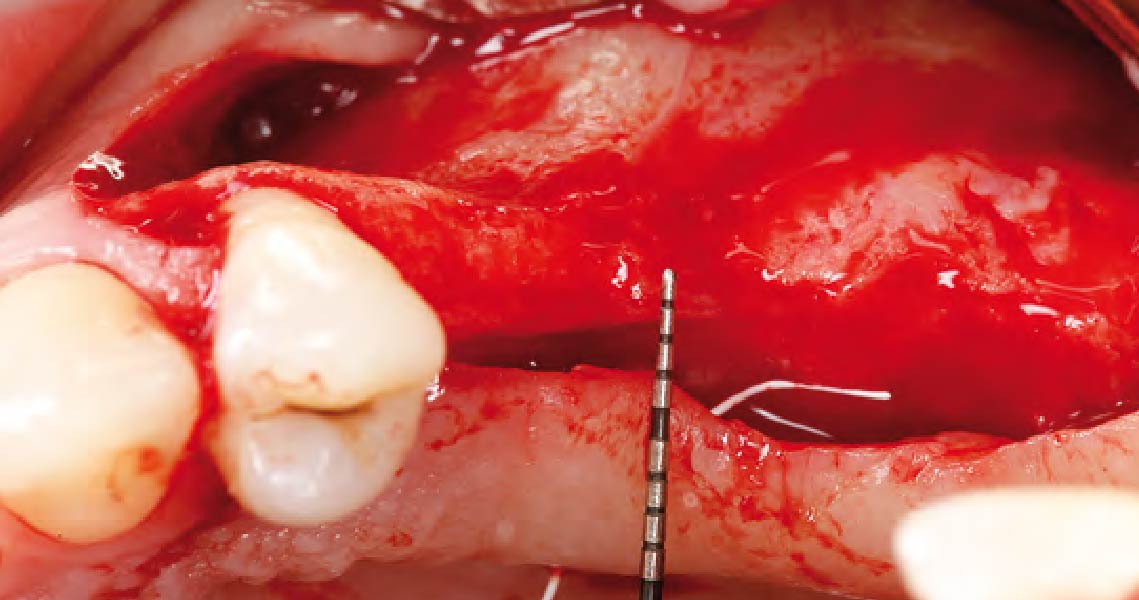
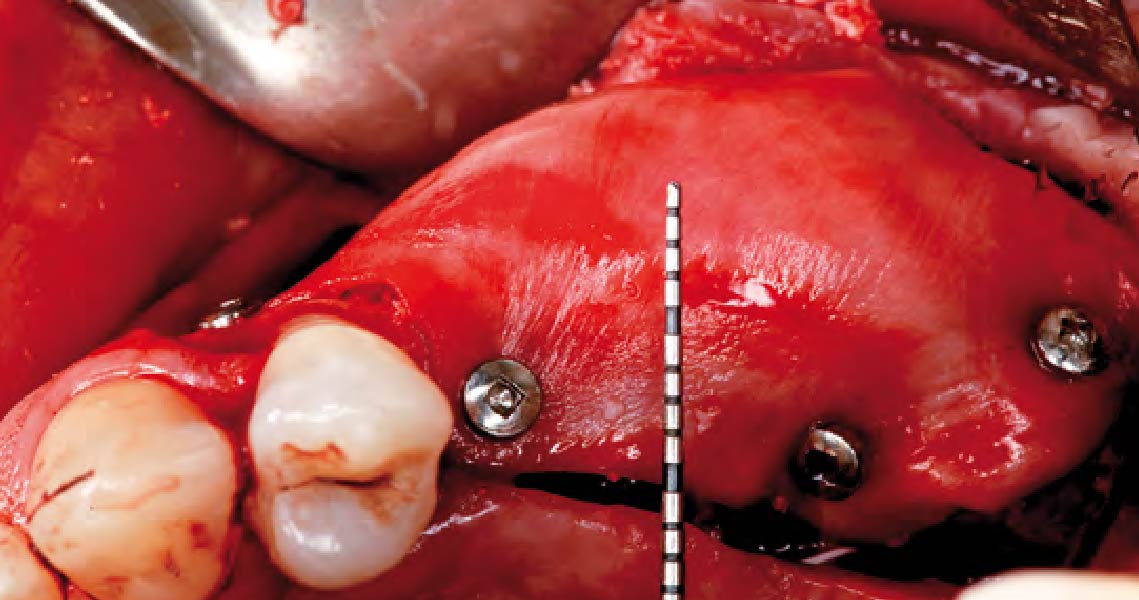
Ramal Bone Graft for Congenitally Missing Maxillary Lateral Incisor

THE SITUATION
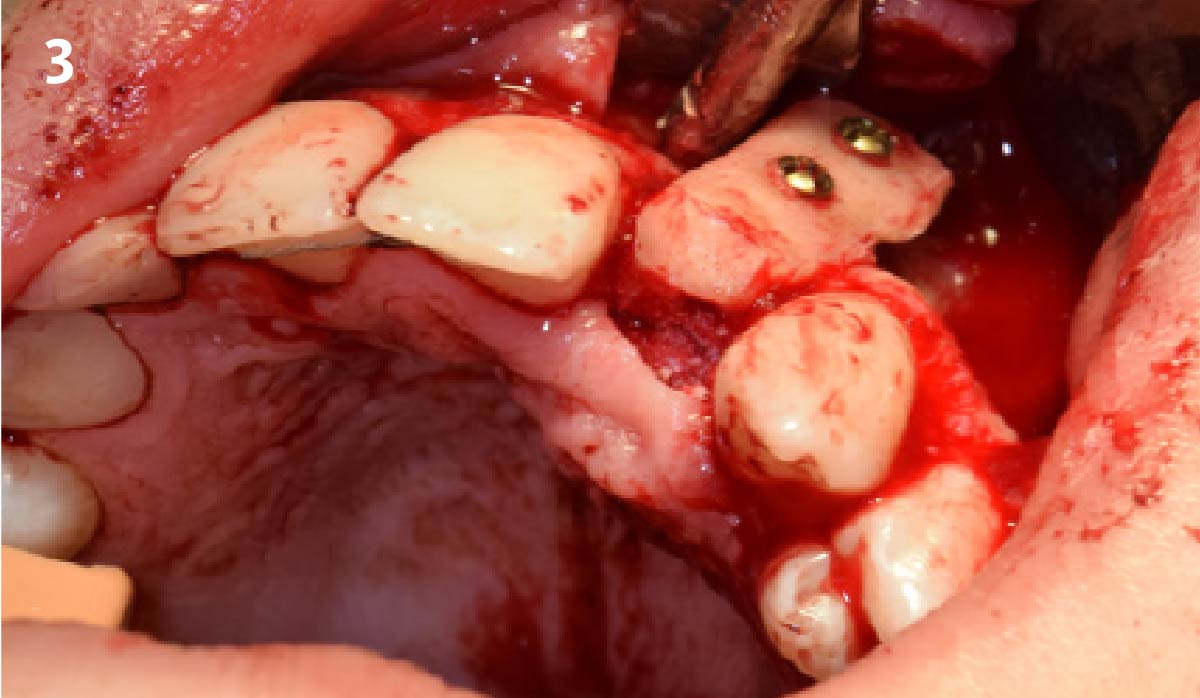
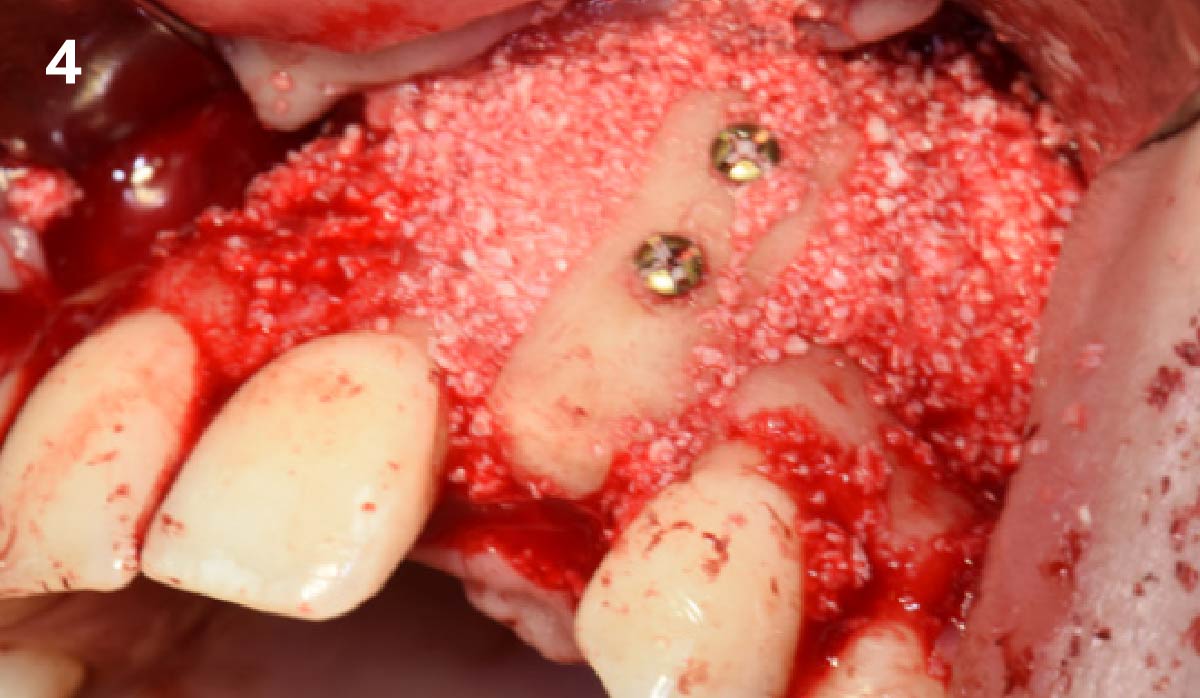
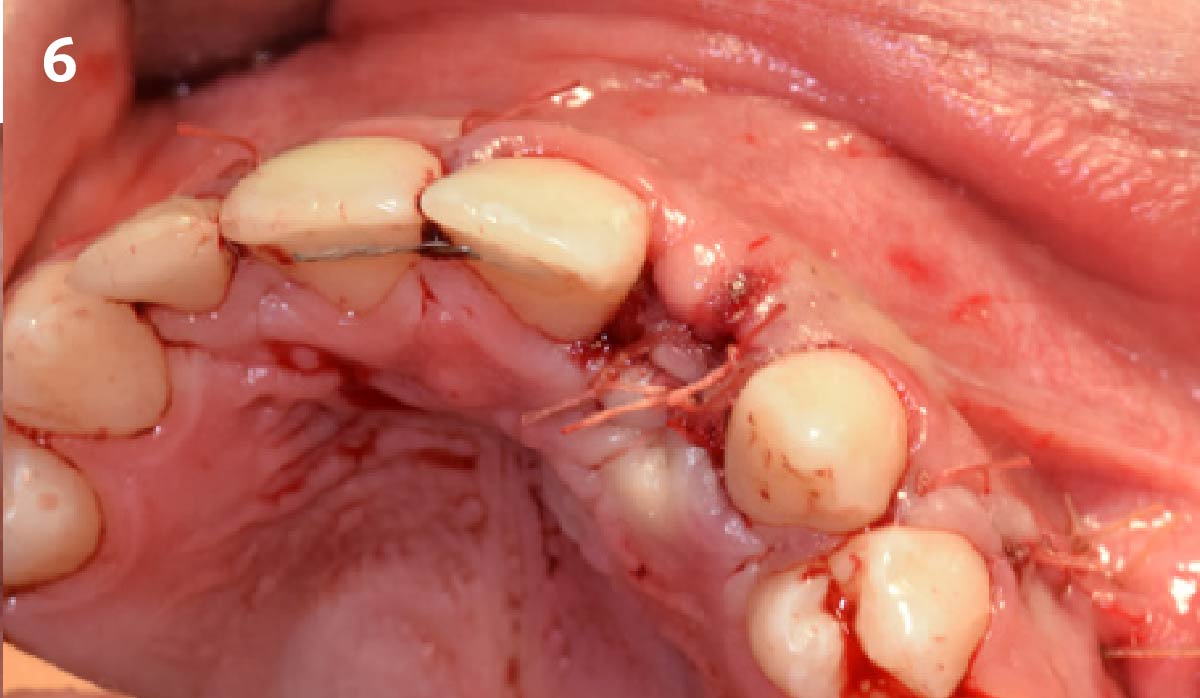
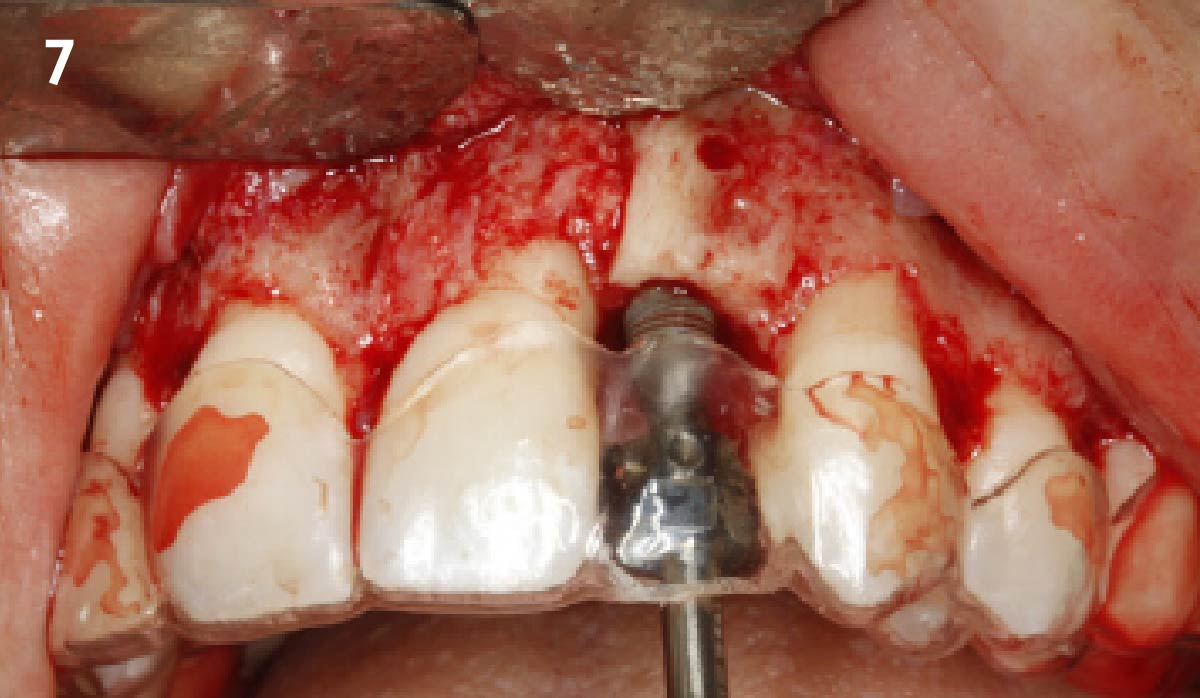
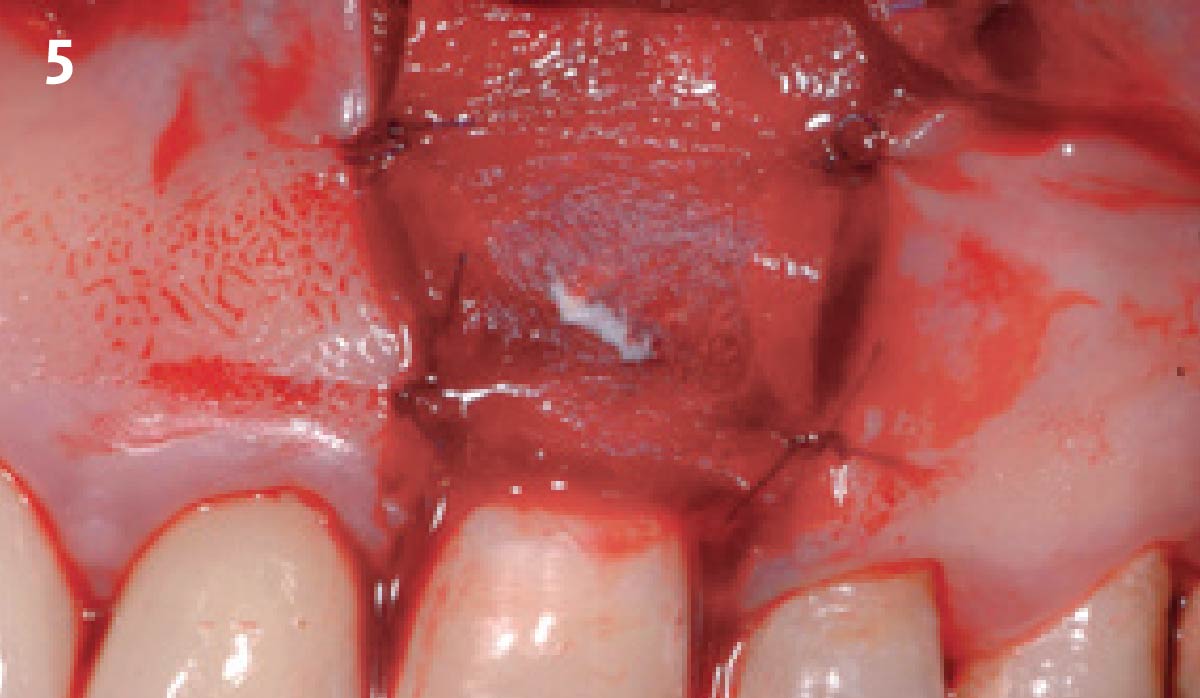
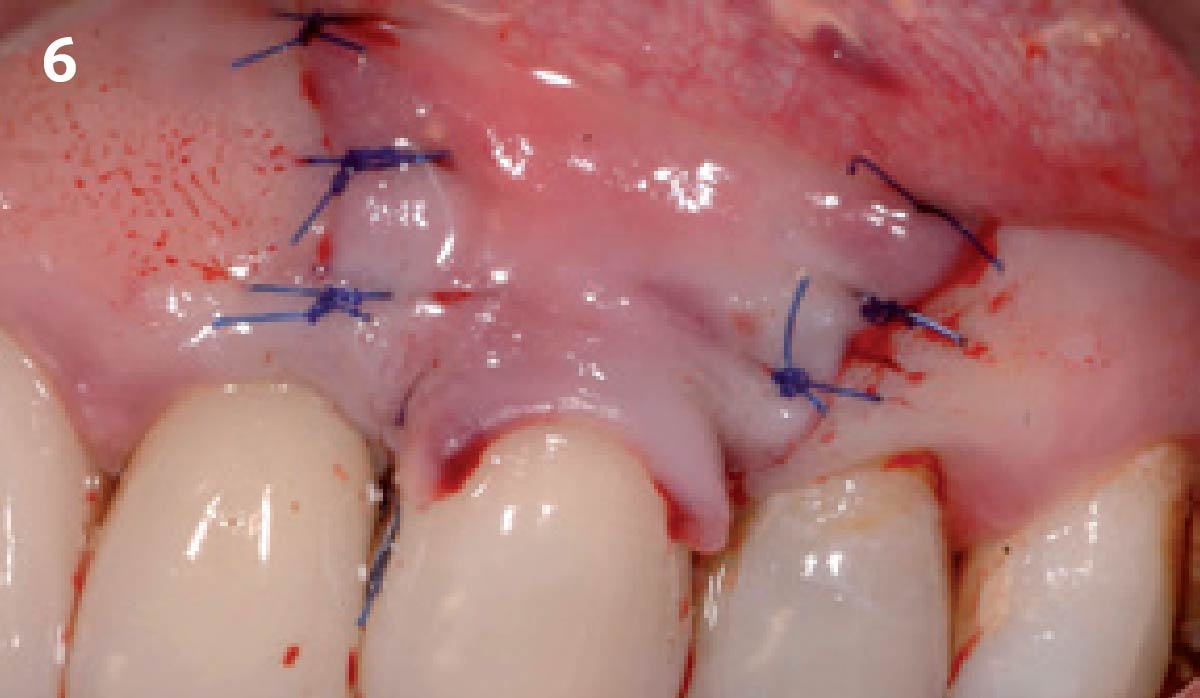
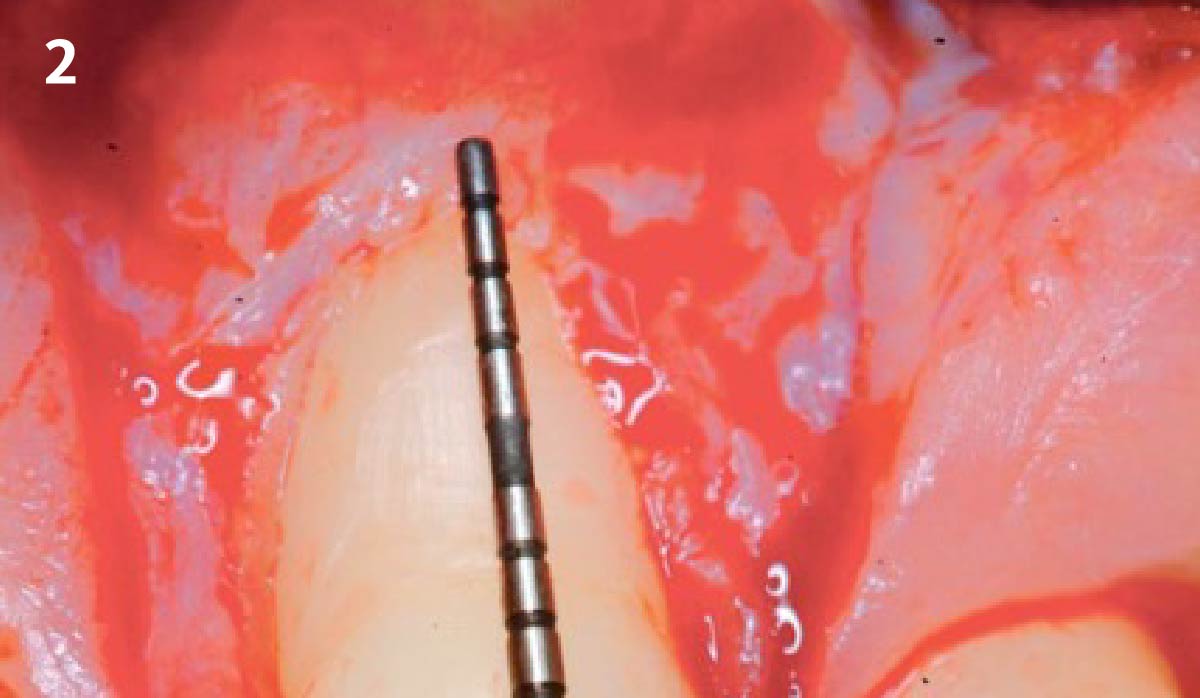
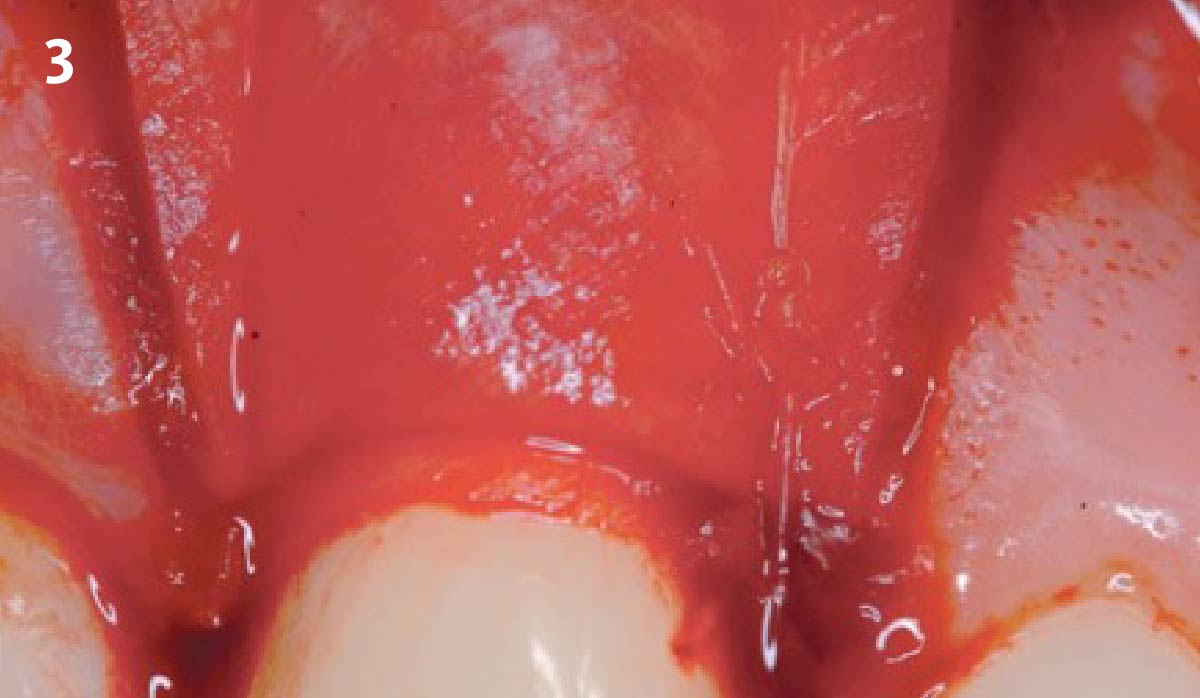
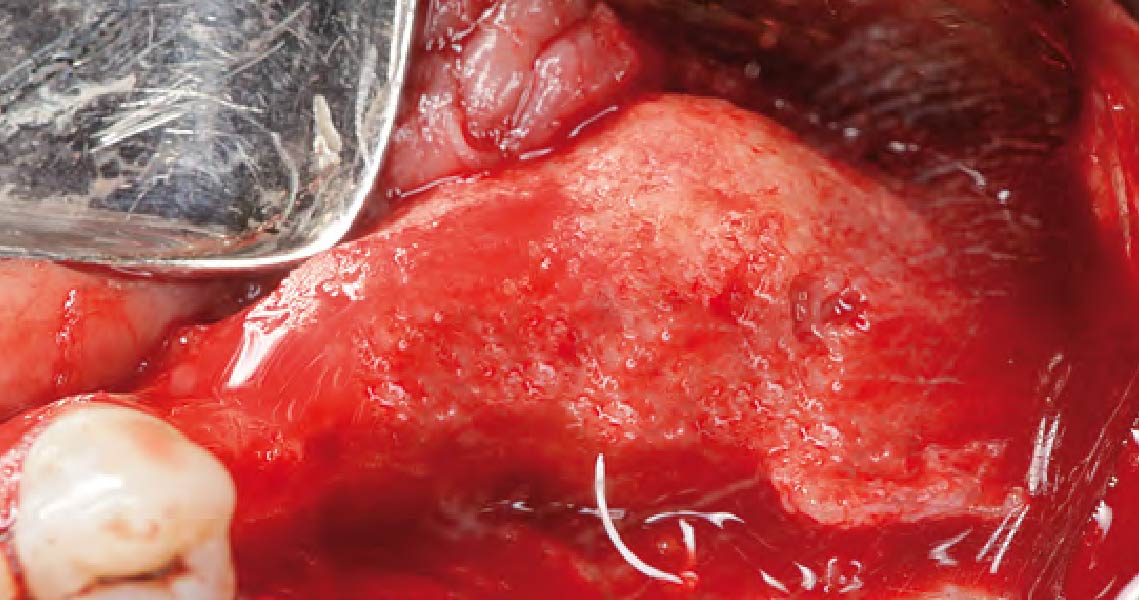
An 18-year-old female presented with a congenitally missing tooth #10. The patient previously sought care by another provider and had undergone guided bone regeneration with allograft and subsequent implant placement with additional grafting at the time of implant placement. The implant ultimately failed and was removed prior to my initial consultation. An examination revealed maximal incisal opening, within normal limits, missing #10 with 6 mm ridge width. In addition there was a significant palpable cleft-like depression on the facial aspect of the ridge, adequate attached tissue but reduced vertical height in relation to adjacent dentition and attached tissue. Previous surgeries resulted in extensive fibrous tissue with scarring at site #10. Plan: A ramal bone graft is indicated at the congenitally missing site #10 with Geistlich Bio-Oss® and Geistlich Mucograft® matrix utilized for ridge augmentation prior to secondary implant placement.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
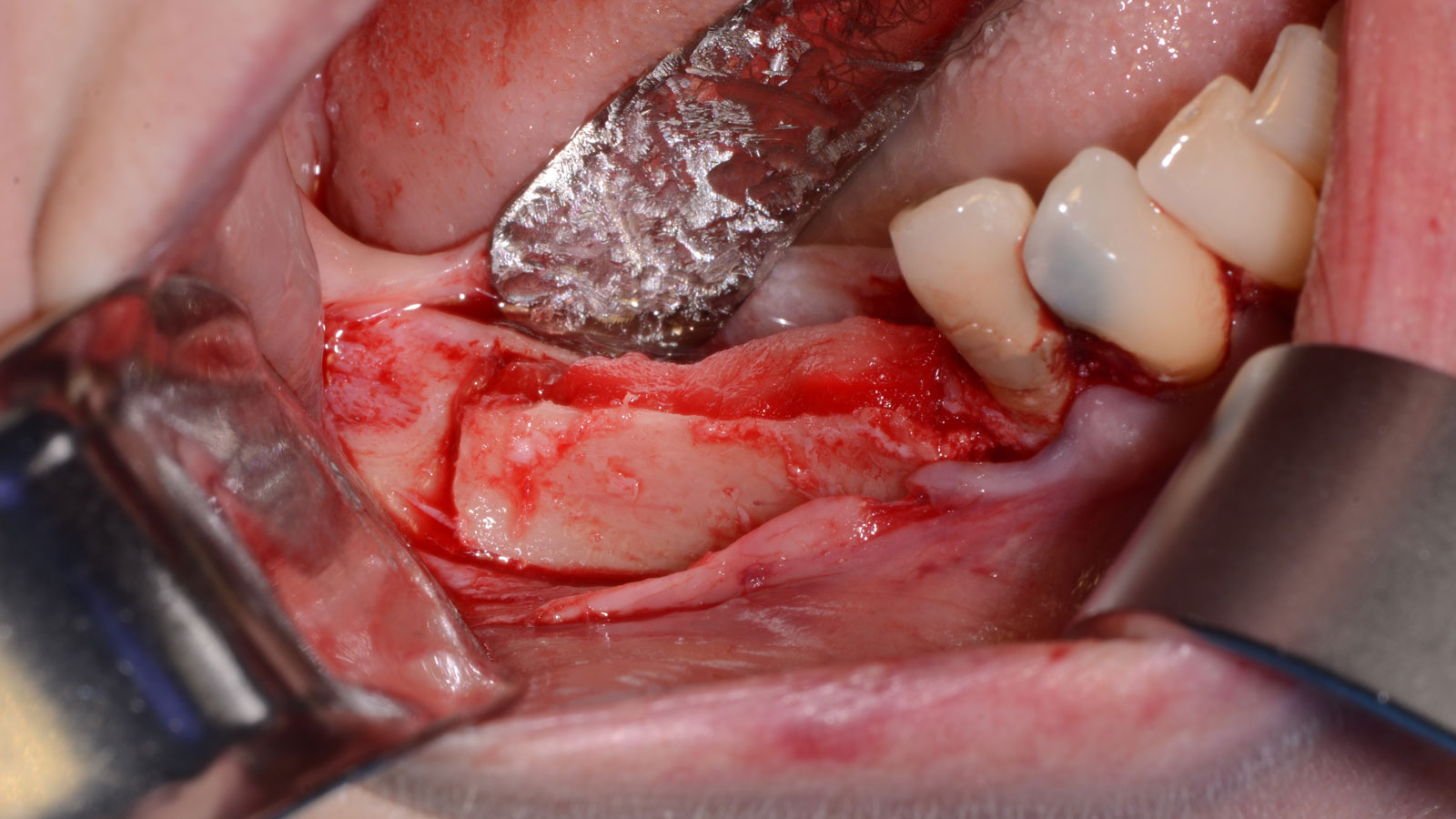
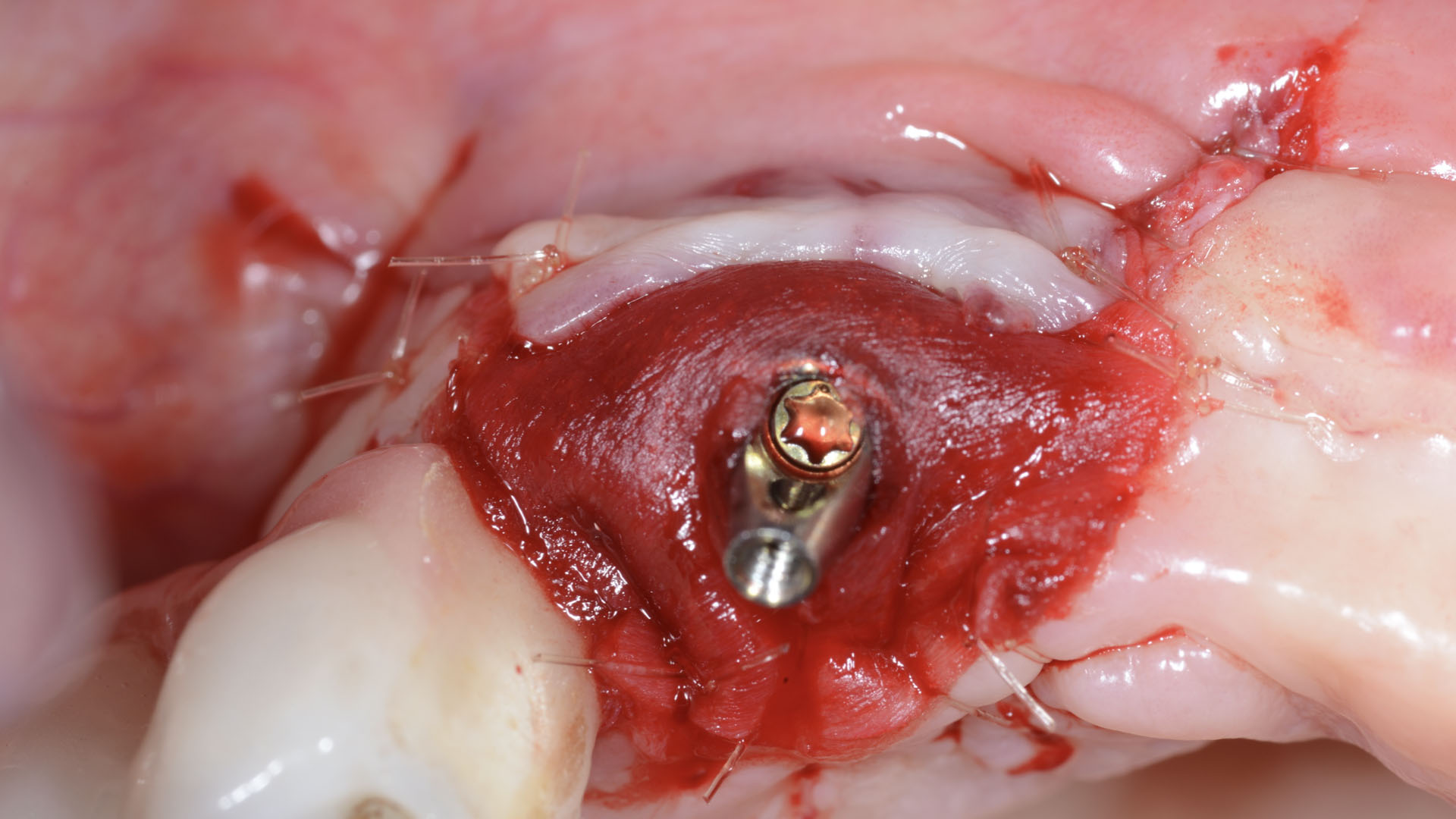
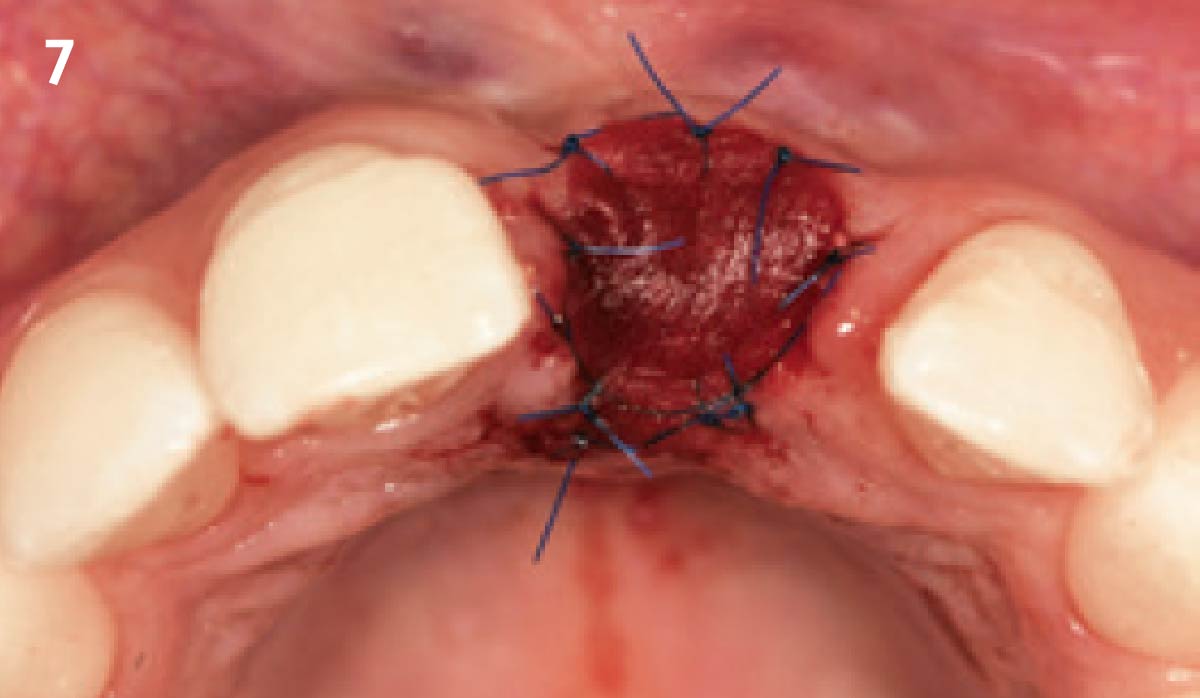
The goals for this patient are to reconstruct the osseous foundation and provide a matrix for improvement with the overlying soft tissue. Specifically, a coordinated multidisciplinary plan was established with the restoring dentist, periodontist and oral surgeon. A plan for idealized anterior cosmetic prosthetic restoration was established. Sequencing of treatment was established. Surgical phase one included a ramal bone graft to site #10 and Essix type temporary prosthesis for immediate post-operative phase followed by a temporary Maryland bridge. Surgical phase two included implant placement and simultaneous crown lengthening and osteoplasty. This stage was done with immediate provisionalization.
“This is a young patient with a congenitally missing incisor that has high esthetic concerns and has had multiple failed surgical attempts that is now presenting for definitive management.”
THE OUTCOME
This case was dependent upon adequate hard-tissue reconstruction combined with soft-tissue manipulation to eliminate scar tissue and provide esthetic recontouring. Obtaining an adequate autogenous graft combined with Geistlich Bio-Oss® at the periphery of the onlay graft is essential for anterior-posterior and vertical augmentation. Utilizing a Geistlich Mucograft® matrix at the ridge crest to help contain the particulate graft and improve the soft-tissue profile for subsequent immediate provisionalization and re-contouring of the surrounding soft tissue played a significant role in the esthetic success.


Dr. Richard E. Bauer, III
Oral and Maxillofacial Surgeon – University of Pittsburgh
Richard E. Bauer, III, DMD, MD is a graduate of the University of Pittsburgh Schools of Dental Medicine and Medicine. Dr. Bauer completed his residency training in Oral and Maxillofacial Surgery at the University of Pittsburgh Medical Center. Dr. Bauer has served on multiple committees for the American Association of Oral and Maxillofacial Surgery (AAOMS). He is a full-time faculty member and Residency Program Director at the University of Pittsburgh in the department of Oral and Maxillofacial Surgery and his practice is focused on dental implants and corrective jaw surgery. He has been active in research with focus on bone regeneration and virtual applications for computer assisted planning and surgery.

BIOBRIEF
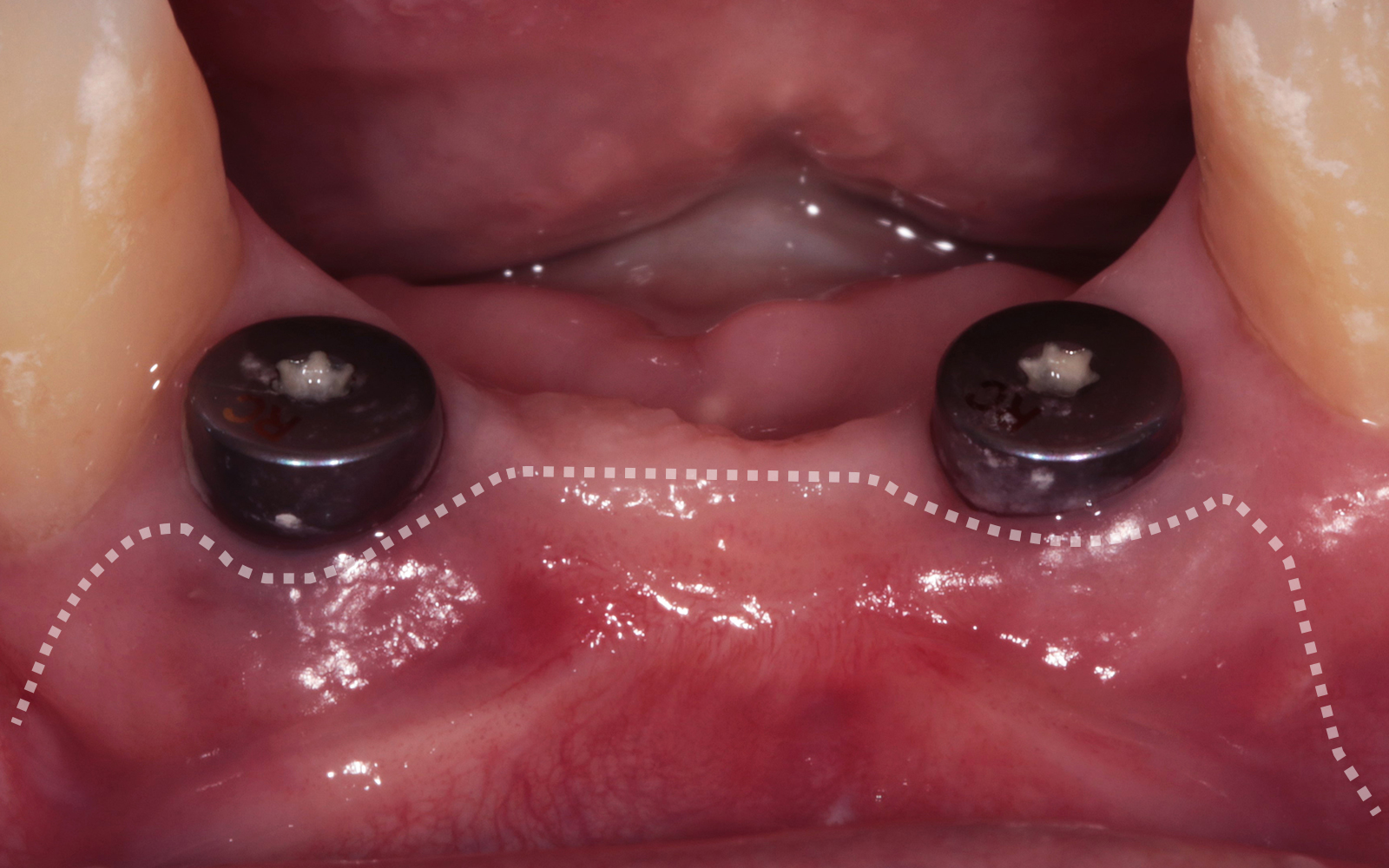
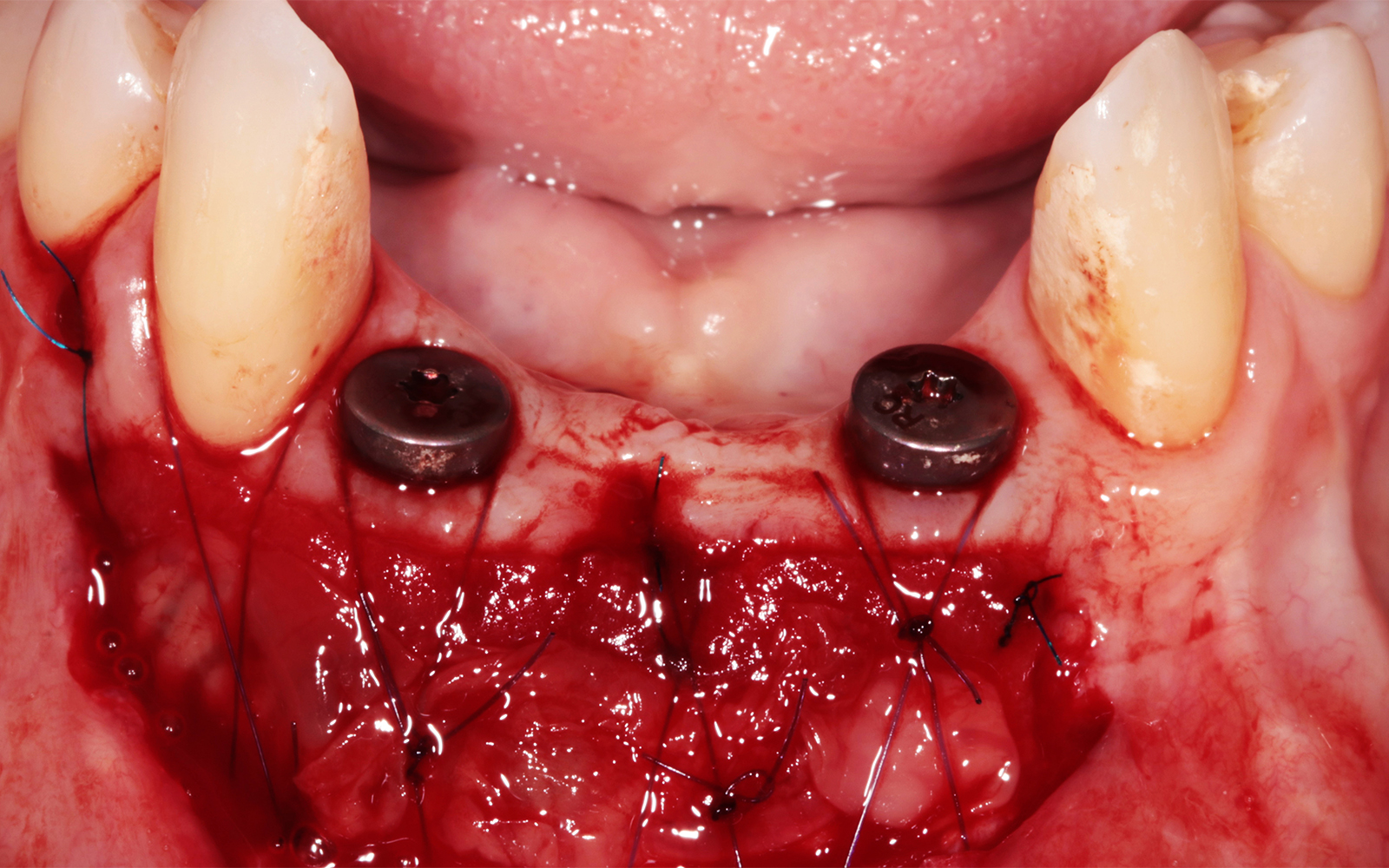
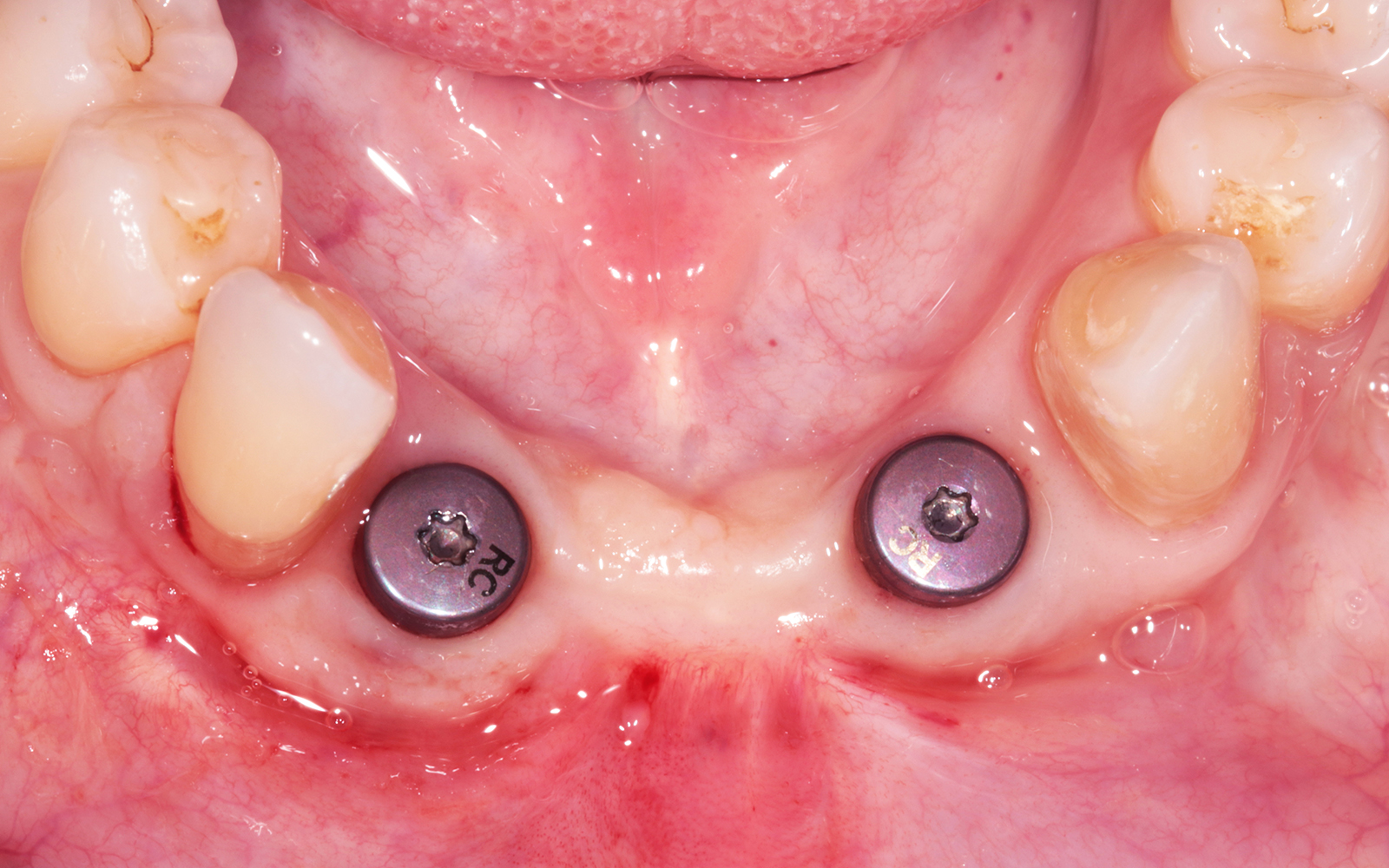
Enhance Periodontal Phenotype with Geistlich Mucograft® for Soft Tissue Augmentation


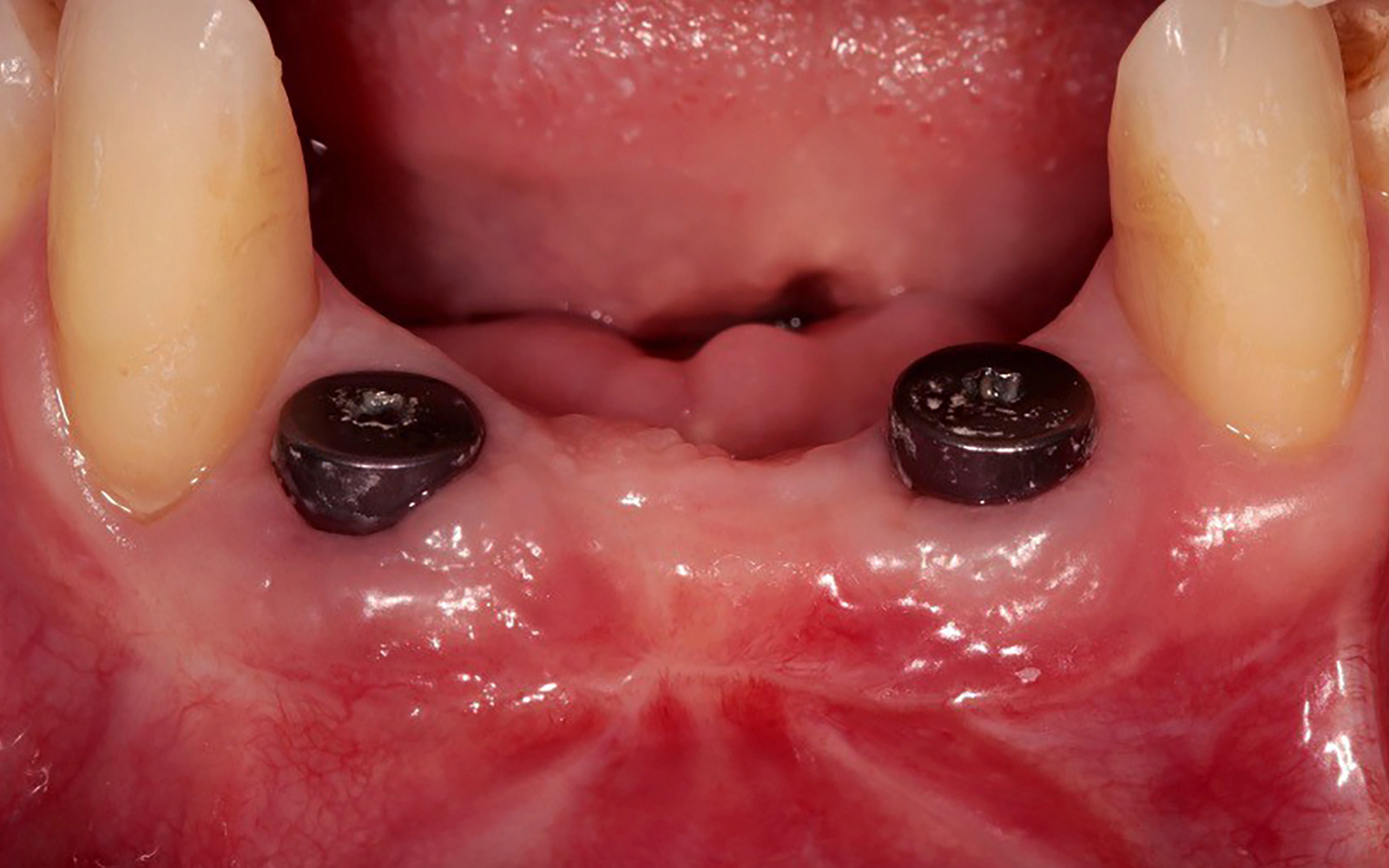
THE SITUATION
A healthy, non-smoking, 37- year-old female presented for second stage surgery at implant sites #23 and #26. Limited keratinized tissue width and gingival thickness can be appreciated in the edentulous ridge, and the patient can be classified as having a thin periodontal phenotype. Additionally, the patient states she experiences sensitivity, and the tissue feels “tender” when brushing. The patient hopes to address her needs in a minimally invasive manner.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system Heavy smoker |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
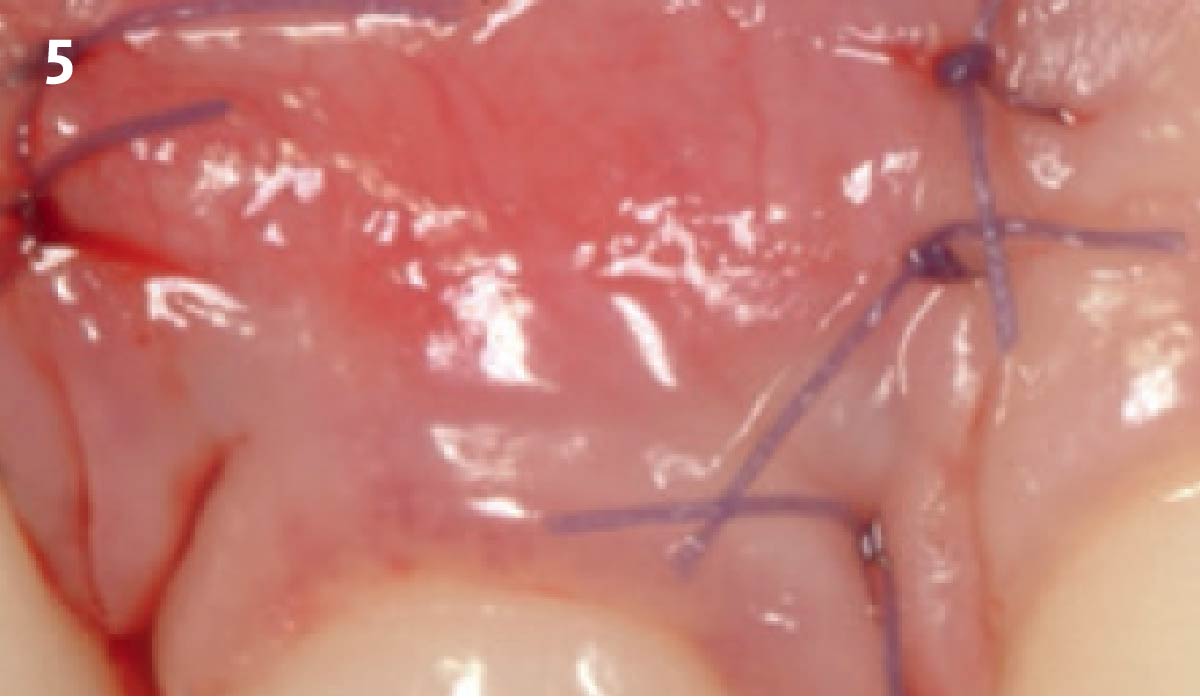
The aim of treatment was to enhance the existing periodontal phenotype from that of one which is thin, with limited keratinized tissue, to one that is thick and maintains an adequate band of attached keratinized tissue. Geistlich Mucograft® was used in conjunction with a PRF membrane, in order to provide optimal wound healing, due to its chemotactic and angiogenic properties.
A viable option that allows for reduced patient morbidity, adequate functional necessity, and ideal esthetics.
THE OUTCOME
Dual application of platelet-rich fibrin (PRF) and a xenogenic collagen matrix, Geistlich Mucograft®, led to successful augmentation of the edentulous ridge. At one-year, the tissues appear healthy, and an increased keratinized tissue width and gingival thickness can be appreciated. By using this soft tissue alternative, the patient was able to avoid post-operative morbidity from a second surgical site, and the chief complaint was addressed.


Allison Rascon, D.D.S., M.S.
Dr. Allison Rascon was born and raised in Miami, Florida. She received her Bachelor of Science in Biomedical and Health Sciences from the University of Central Florida. She received her DDS from New York University, where she graduated with honors in Periodontics and was inducted into the Omicron Kappa Upsilon National Dental Honor Society in 2020. She then went on to receive a Certificate in Periodontics and Master of Science in Oral Biology from the University of Pennsylvania. Currently, she is board-eligible by the American Academy of Periodontology. She is an active member of the AAP, AO, OF, and ADA. Aside from her active participation in organized dentistry, she is also passionate about her research in periodontal and peri-implant regeneration. Dr. Rascon was a recipient of the George J. Coslet Memorial Scholarship in 2021 and 2022. During her residency, she was awarded the Best Oral Clinical Presentation Award at the Academy of Osseointegration Annual Meeting in 2022 and was the recipient of the Northeastern Society of Periodontists Tannenbaum/ Schoor Resident School Competition Award for 2023. Currently, Dr. Rascon works in private practice in Manhattan, NY.

BIOBRIEF
Clinical Efficacy of Geistlich Mucograft® in Regeneration of Oral Mucosa Combined with the Surgical Treatment of Peri-implantitis in Implants with Lack of Keratinized Tissue



THE SITUATION
Adult patient, non-smoker and without relevant systemic history, attends to clinic referring peri-implant tissue inflammation, bleeding and brushing discomfort around her implant in the upper jaw. Clinically peri-implant pocket depth > 5 mm, bleeding and suppuration on probing were observed. Furthermore, the implant presented < 2 mm of keratinized mucosa and radiographic horizontal bone loss.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system Heavy smoker |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
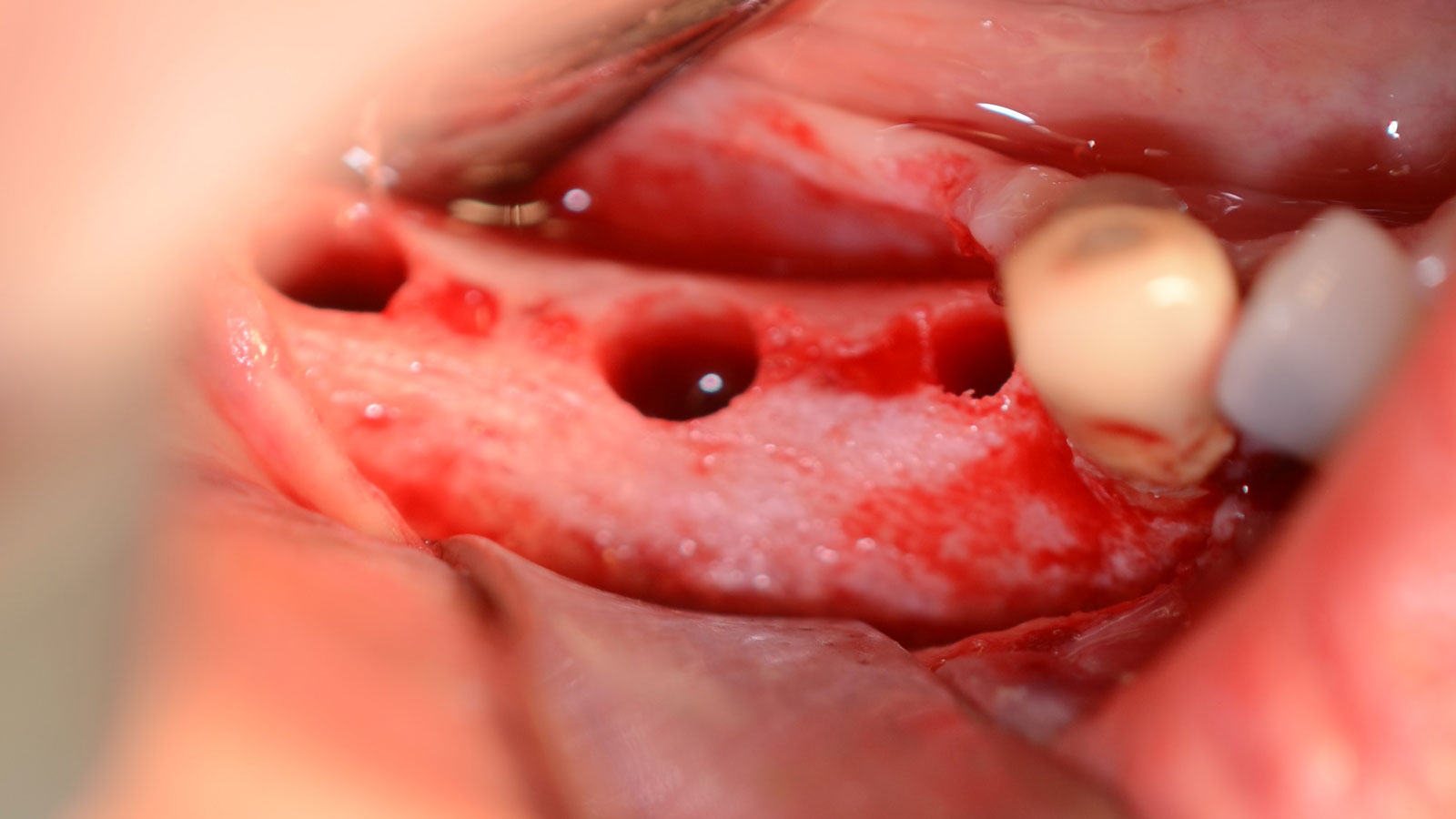
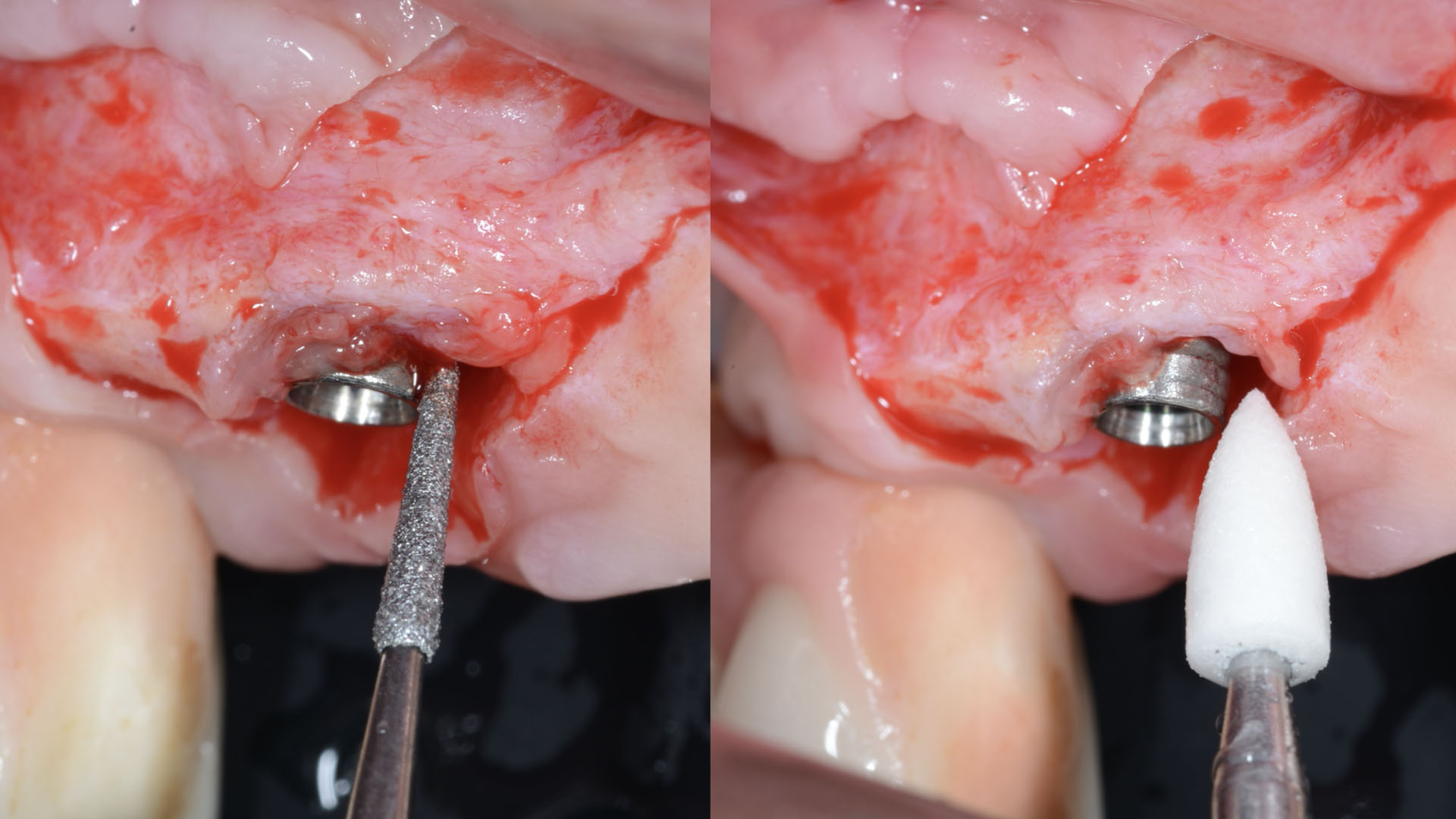
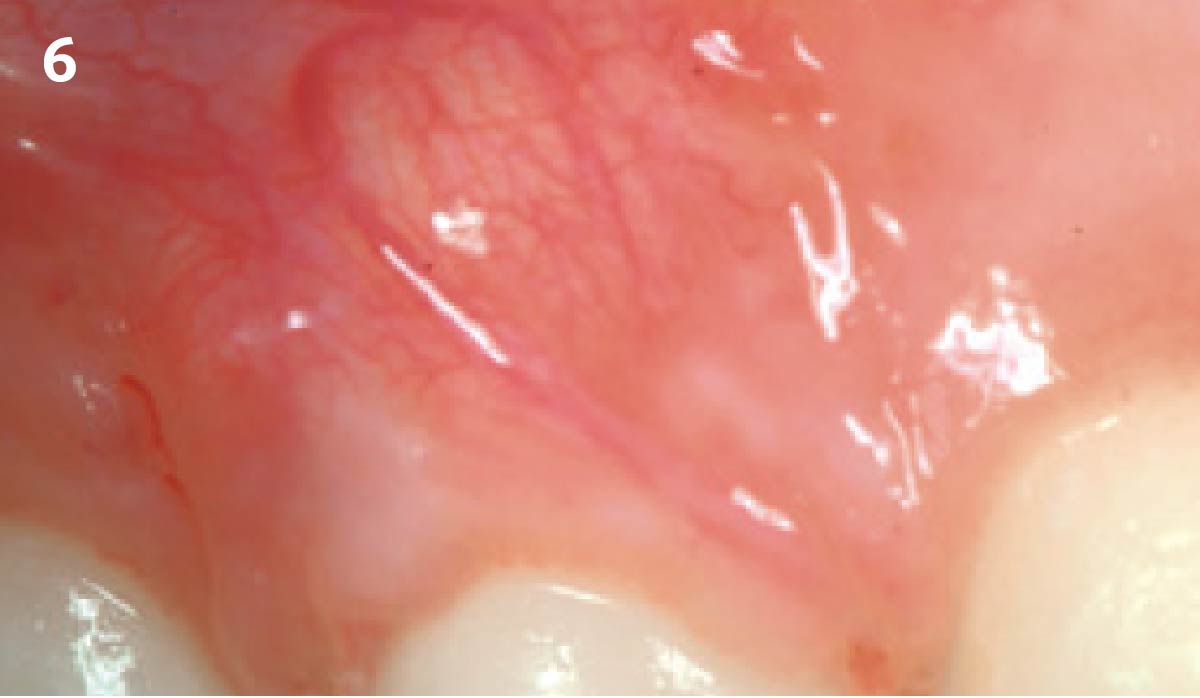
THE APPROACH
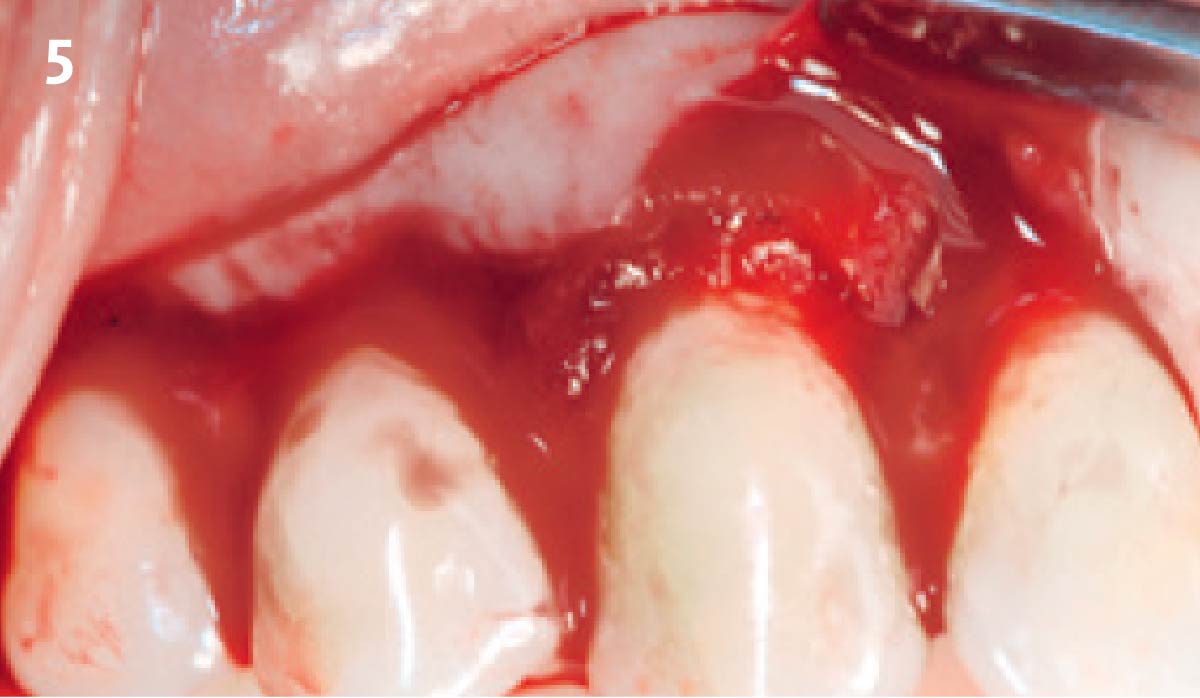
Intrasulcular incision was made and a mucosal partial thickness flap was raised. The recipient site was prepared by sharp disection in order to create a periosteal bed free of any muscle attachment. Peri-implant granulation tissue was removed and implantoplasty was performed. Finally, Geistlich Mucograft® was used to support the gain of keratinized tissue. Thus, the collagen matrix was sutured with the resulting flap apically at the base of the newly created vestibulum.
Absence of > 2 mm of keratinized mucosa was associated with peri-implant soft-tissue inflammation, bleeding and discomfort on brushing.
THE OUTCOME
After two years follow-up, the successful outcome can be observed in terms of clinical peri-implant parameters, gain of keratinized mucosa without significant graft shrinkage and stability of vertical position of the mucosal margin.


Dr. Alberto Ortiz-Vigón
- DDS from the University of the Basque Country
- MSc and PhD in bone regeneration from the University Complutense of Madrid (UCM)
- Master in Periodontology and Implant dentistry from the EFP
- Research fellowship at the University of Gothenburg
- MBA from the Deusto Business School
- Assistant professor and clinical researcher at UCM and ThinkingPerio Research
- PerioCentrum Clinic in Bilbao
- Co-founder of ARC Healthtech Innovation Holding
- Socially engaged & NGO co-founder of Smile is a Foundation

Dr. Erik Regidor Correa
- DDS from the University of the Basque Country
- MSc from the U. of the Basque Country
- Master in Periodontology and Implant Dentistry U. of the Basque Country
- PhD student in the U. of the Basque Country
- Assistant professor and clinical researcher ThinkingPerio Research

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE
CONCLUSIONS:
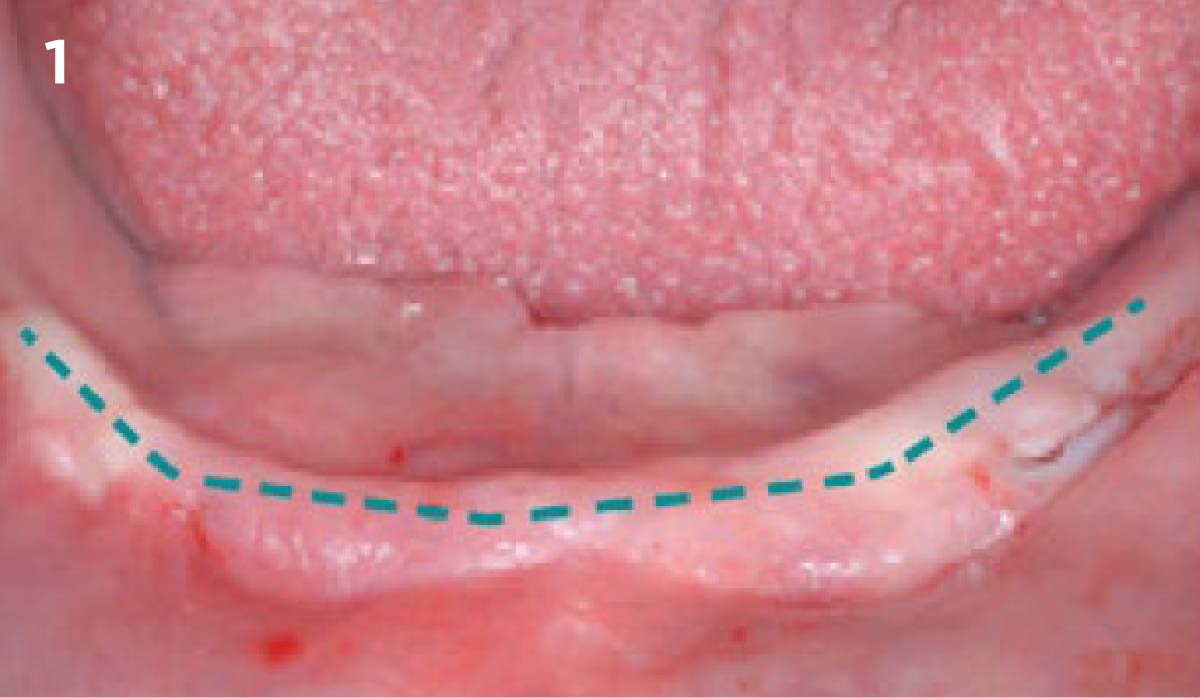
- Geistlich Mucograft® with a keratinized tissue strip was utilized to increase vestibular depth and gain additional keratinized tissue.
- Augmentation of severely atrophied alveolar ridge provided sufficient bone for implant placement 8 months following augmentation.