NEW EBOOK: How to Master Bone Regeneration with Digital Innovation. Download Today!
Product: Geistlich Bio-Oss®

BIOBRIEF
Horizontal Ridge Augmentation with a Layered Allograft-Xenograft Approach


THE SITUATION
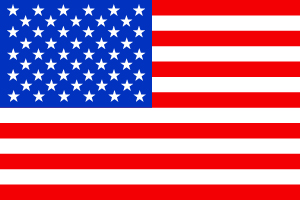
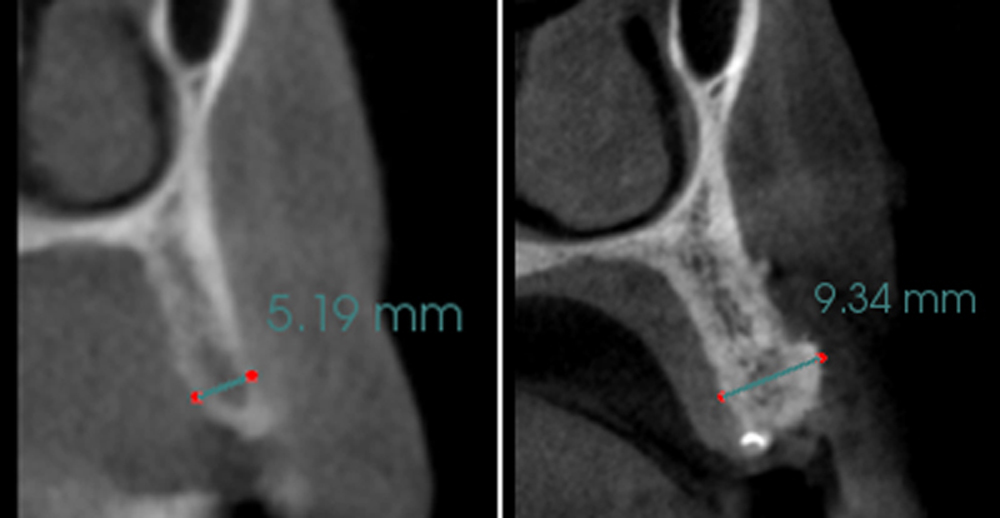
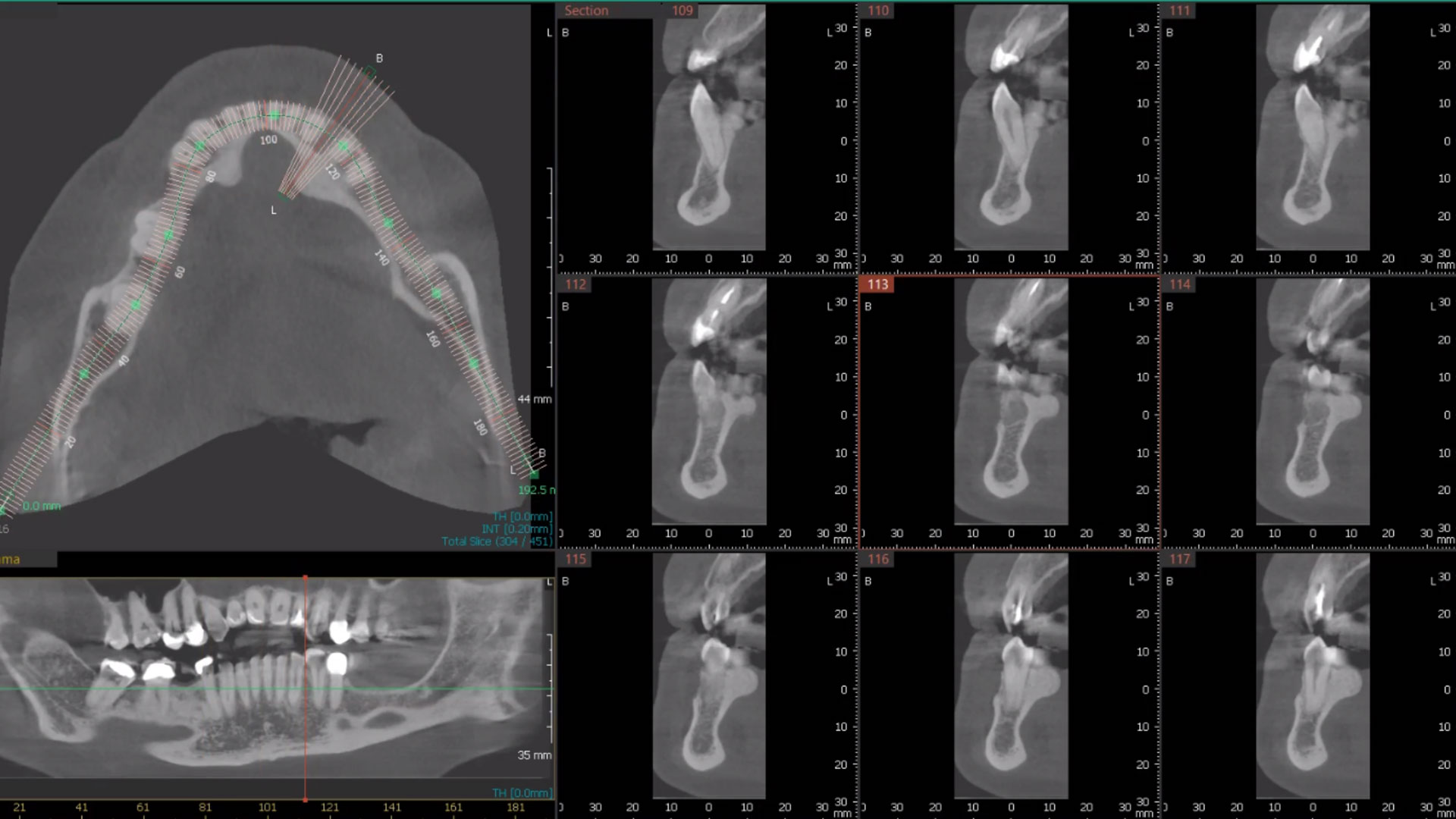
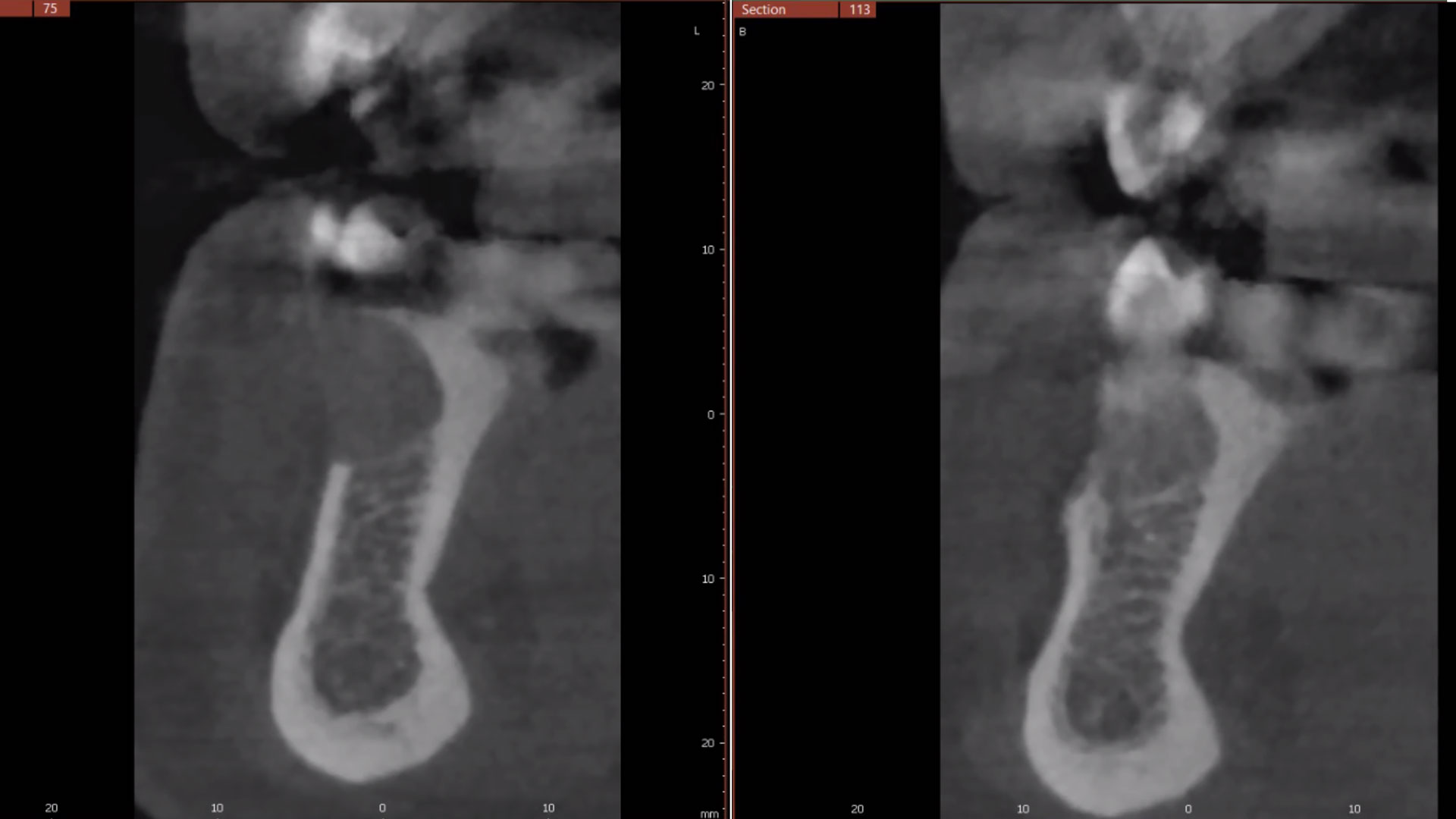
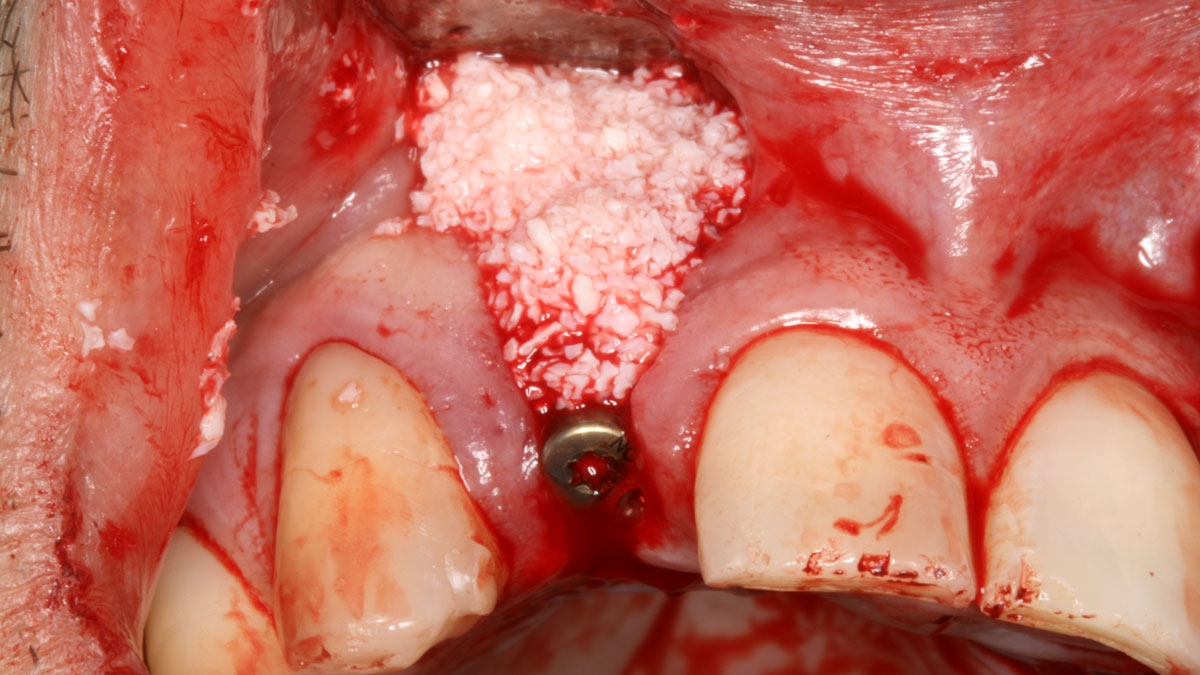
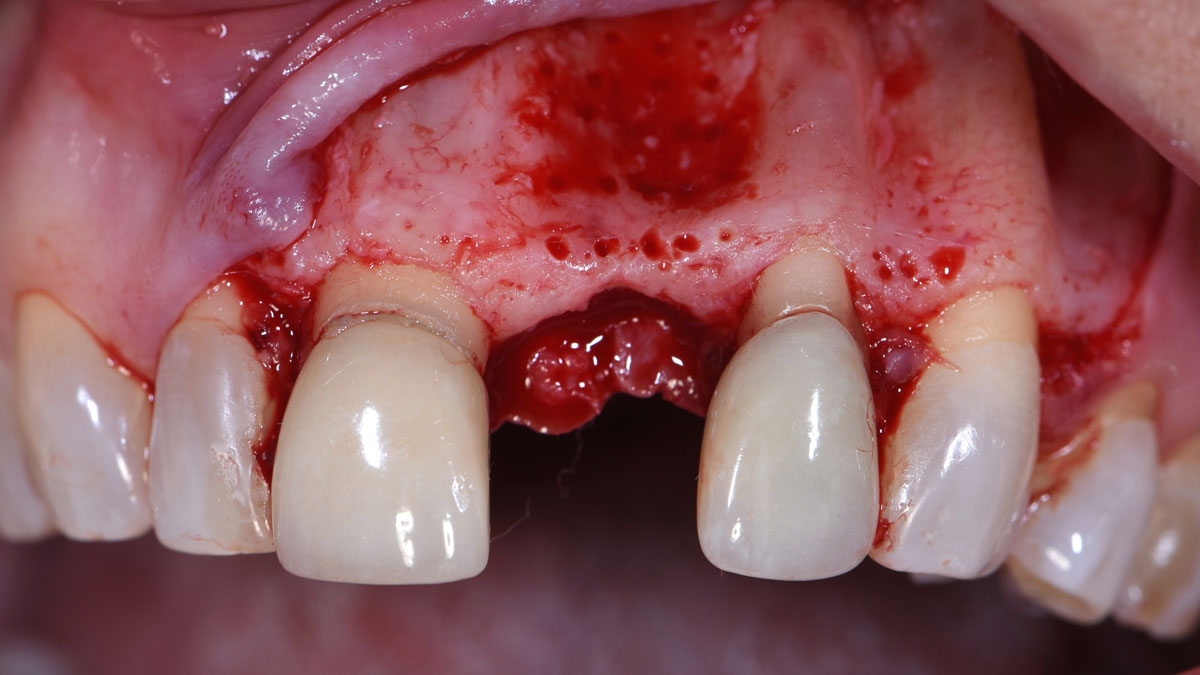
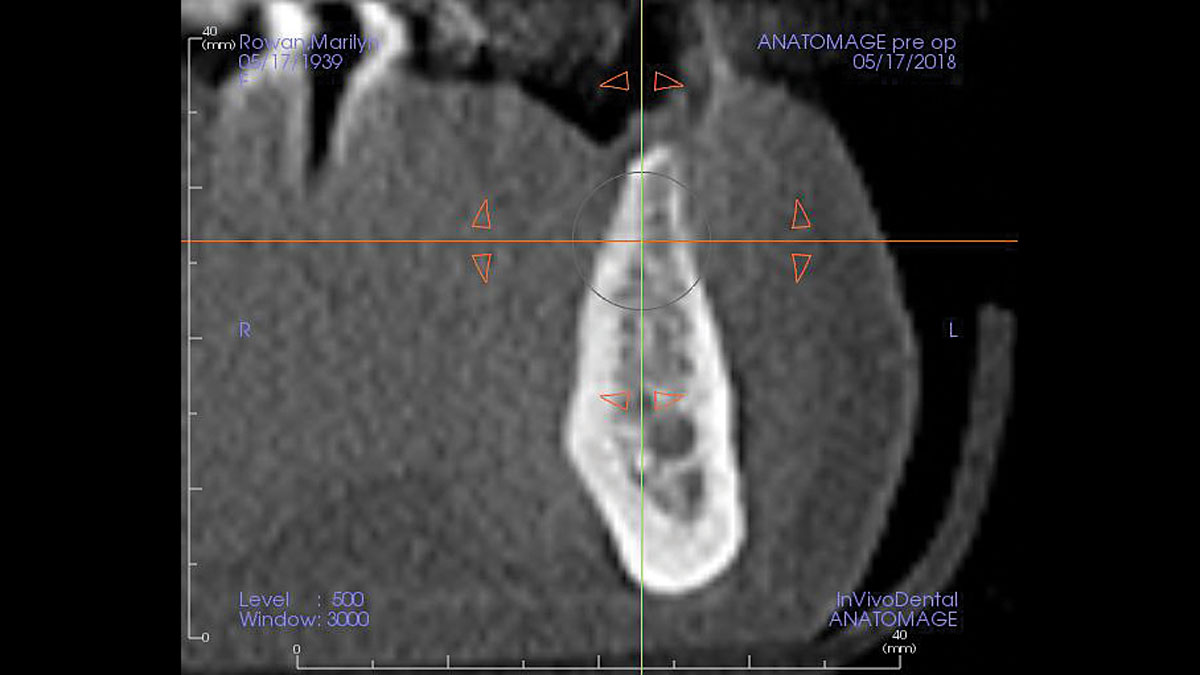
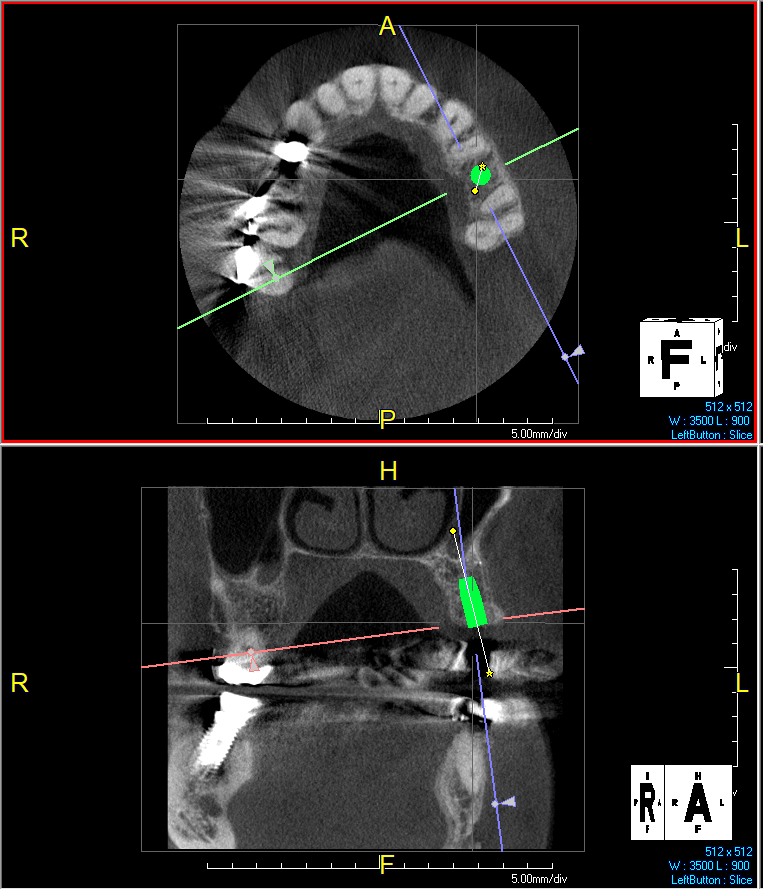
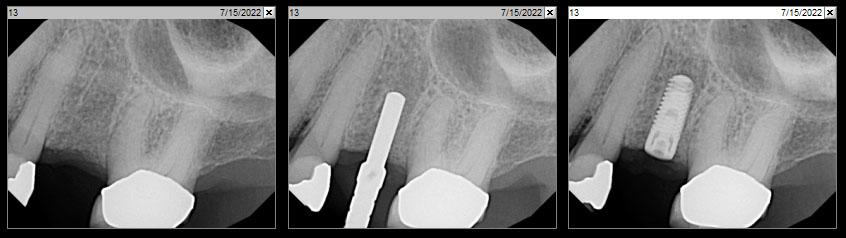
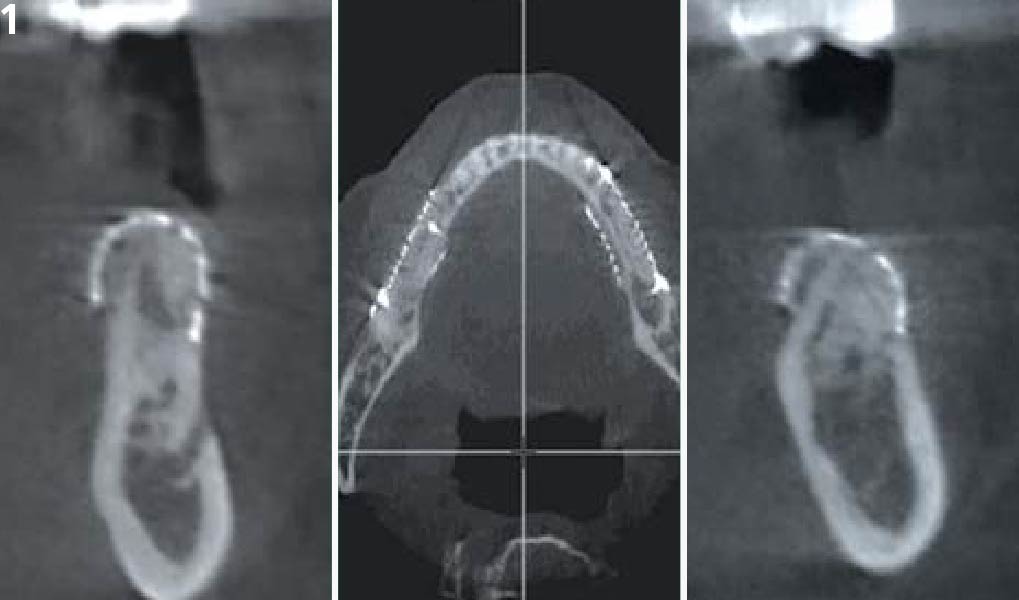
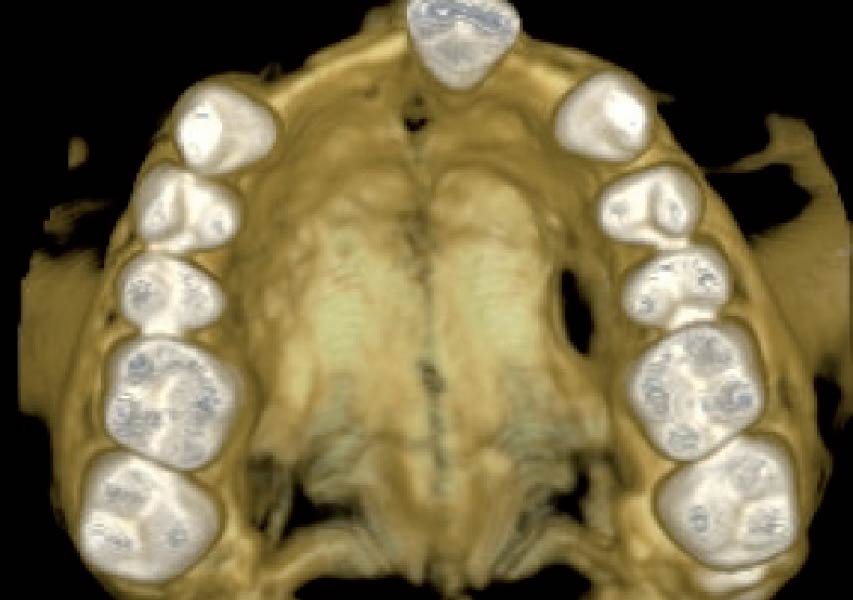
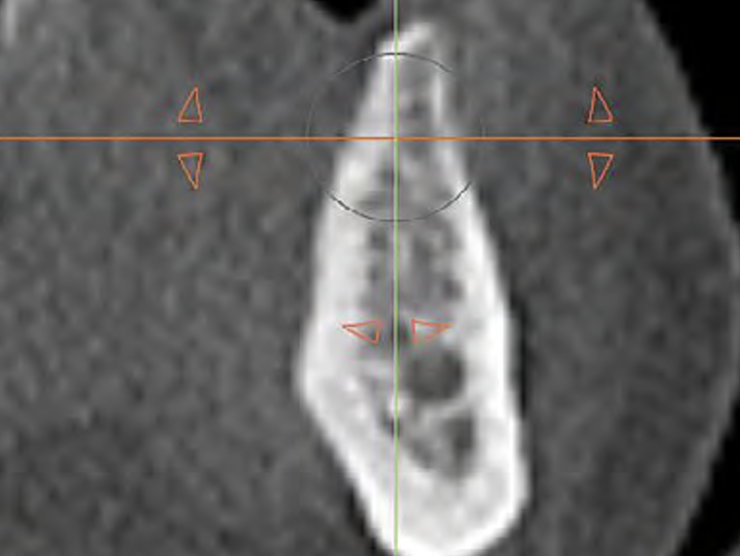
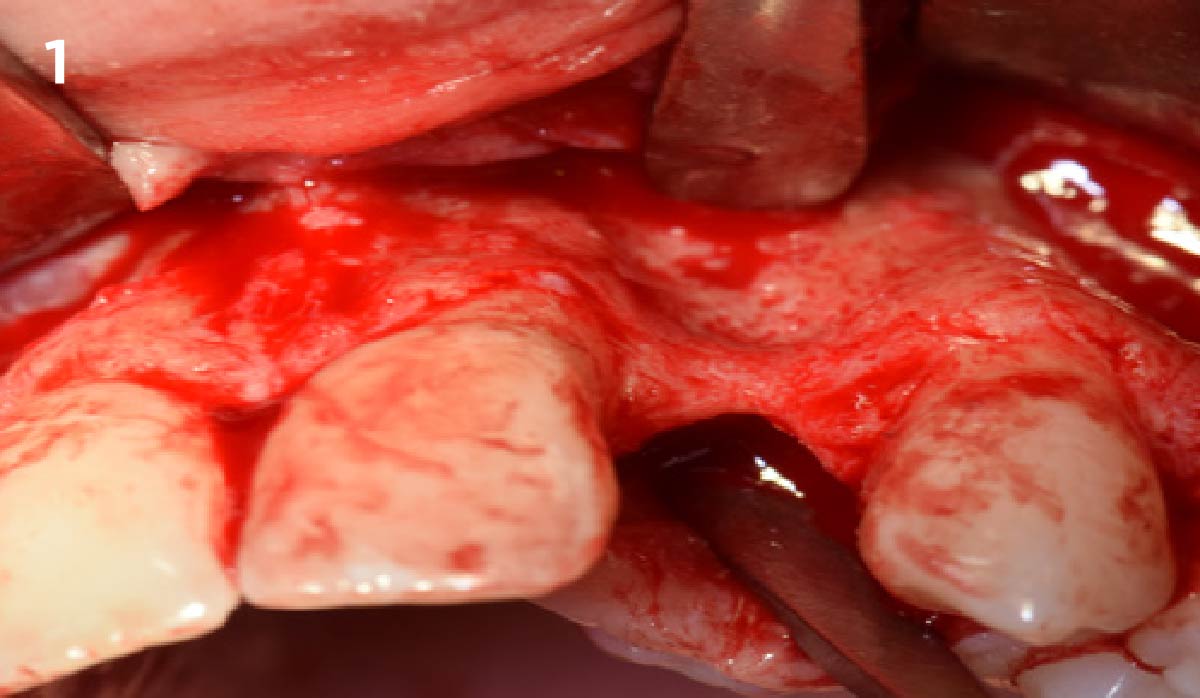
The patient presented to the clinic for a dental implant in the tooth #12 location. Clinical evaluation revealed a ridge deficiency. A Cone Beam Computed Tomography (CBCT) scan was taken, confirming insufficient ridge width for implant placement. As a result, the site was treatment planned for horizontal ridge augmentation.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
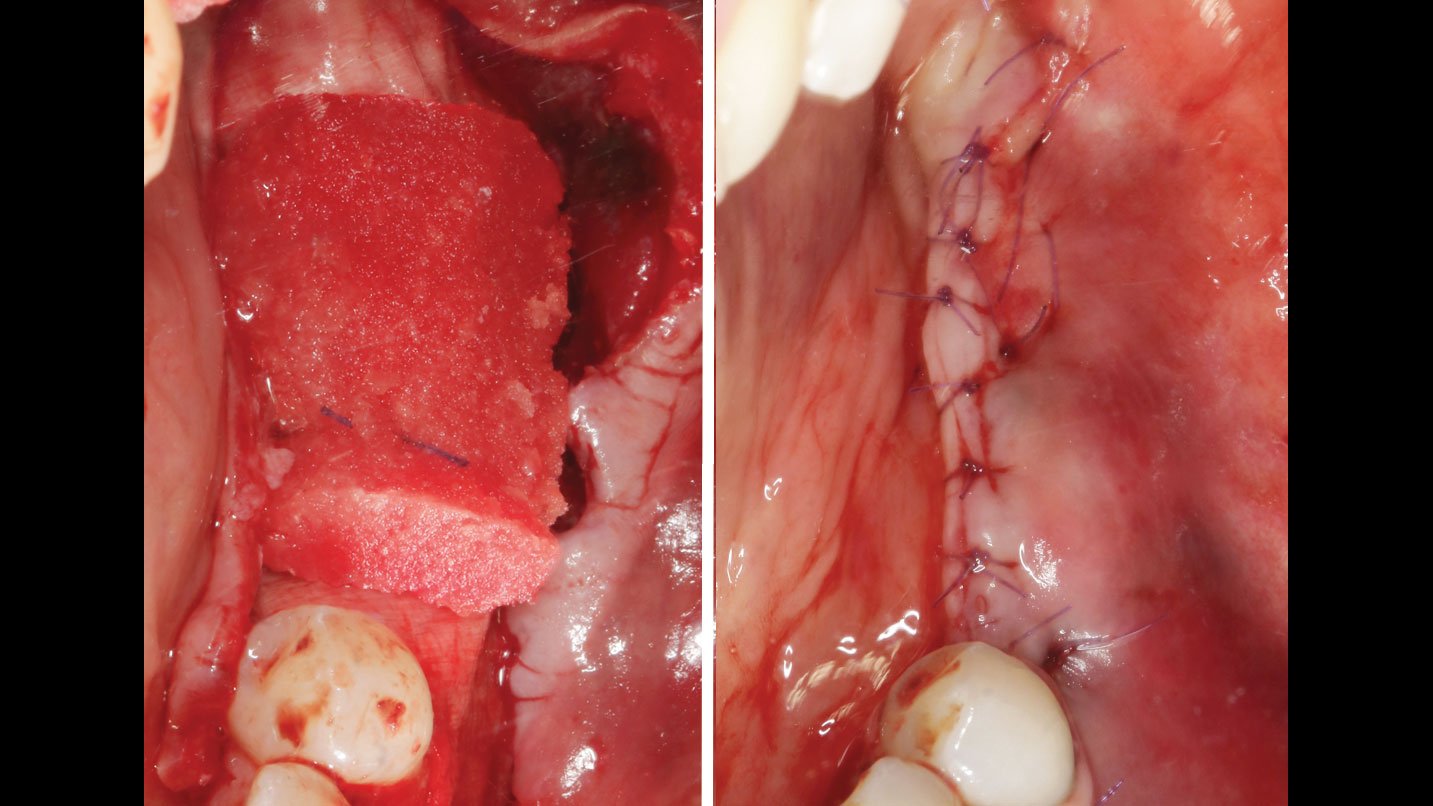
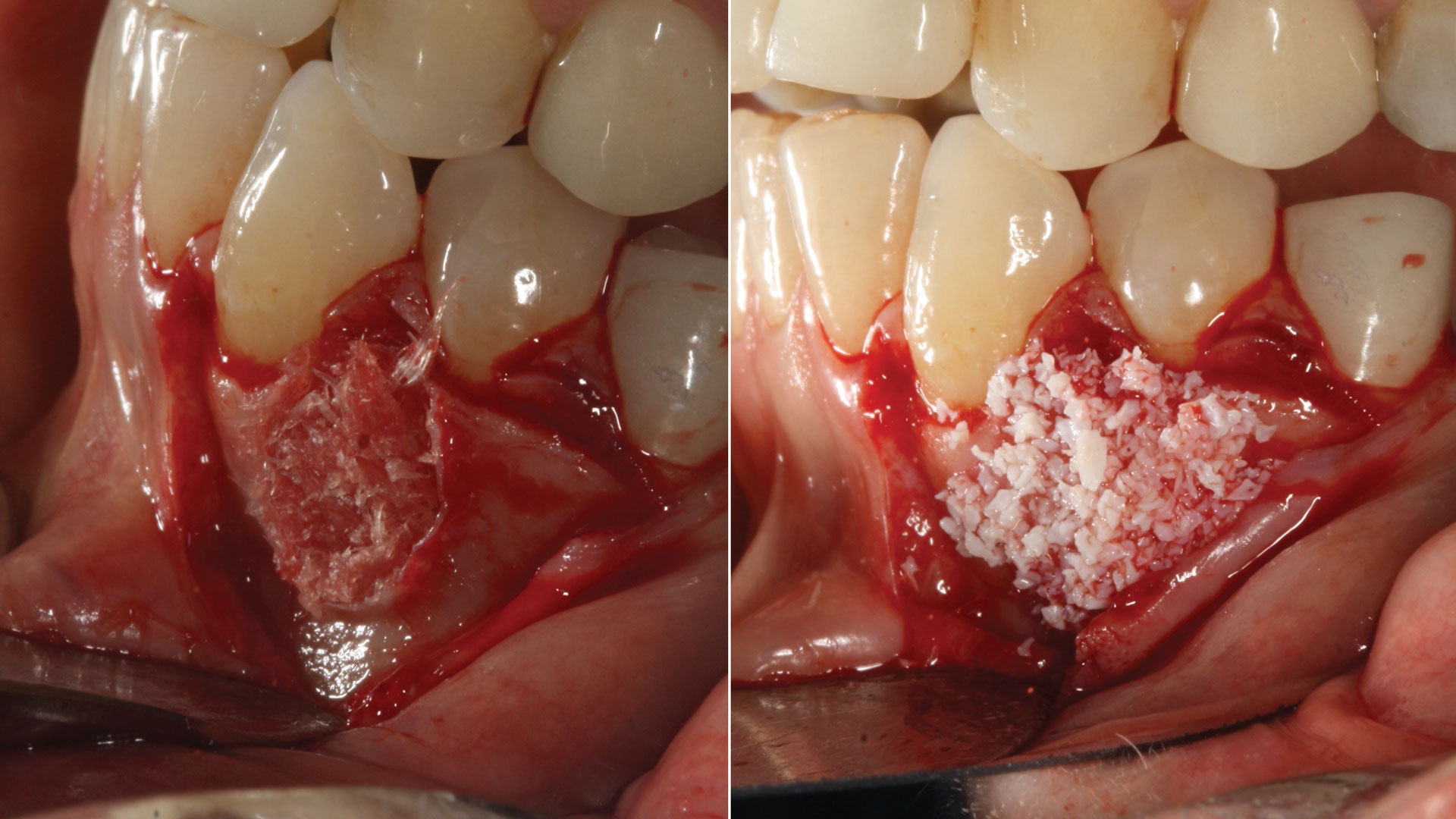
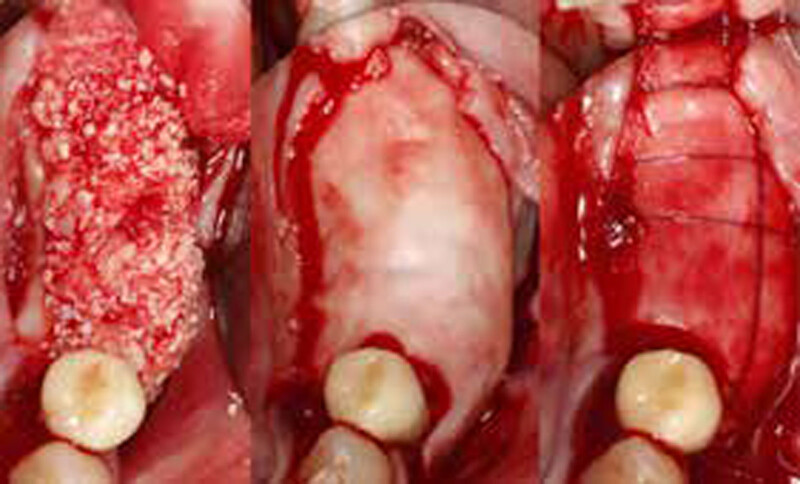
THE APPROACH
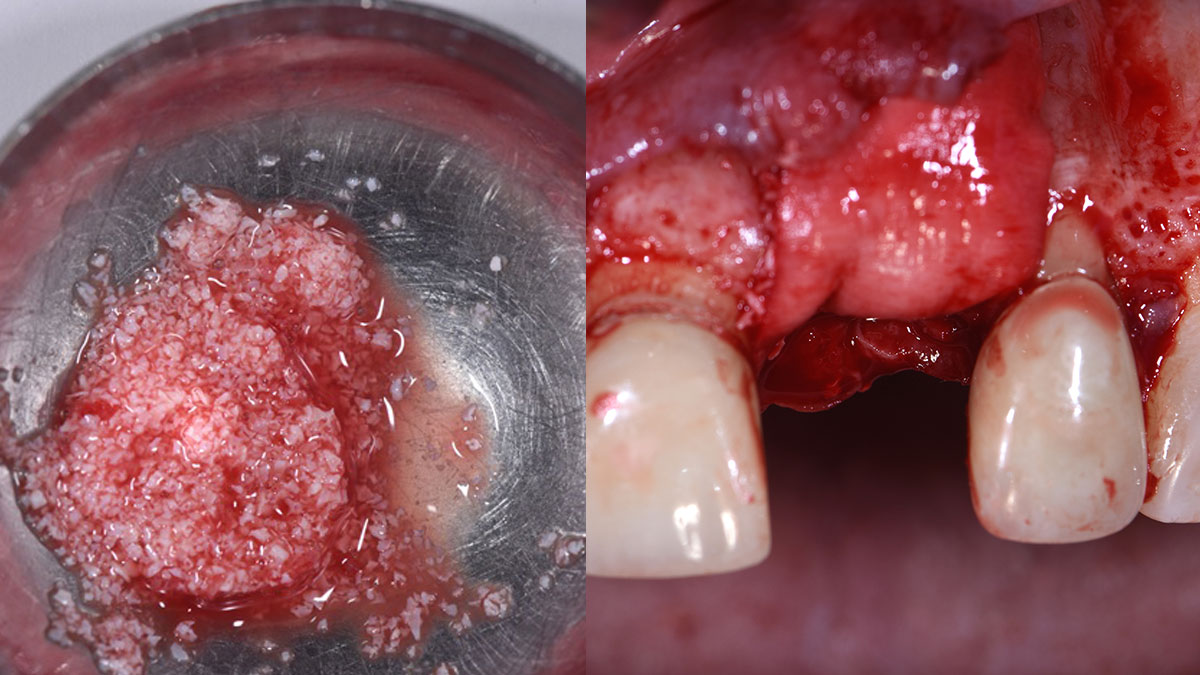
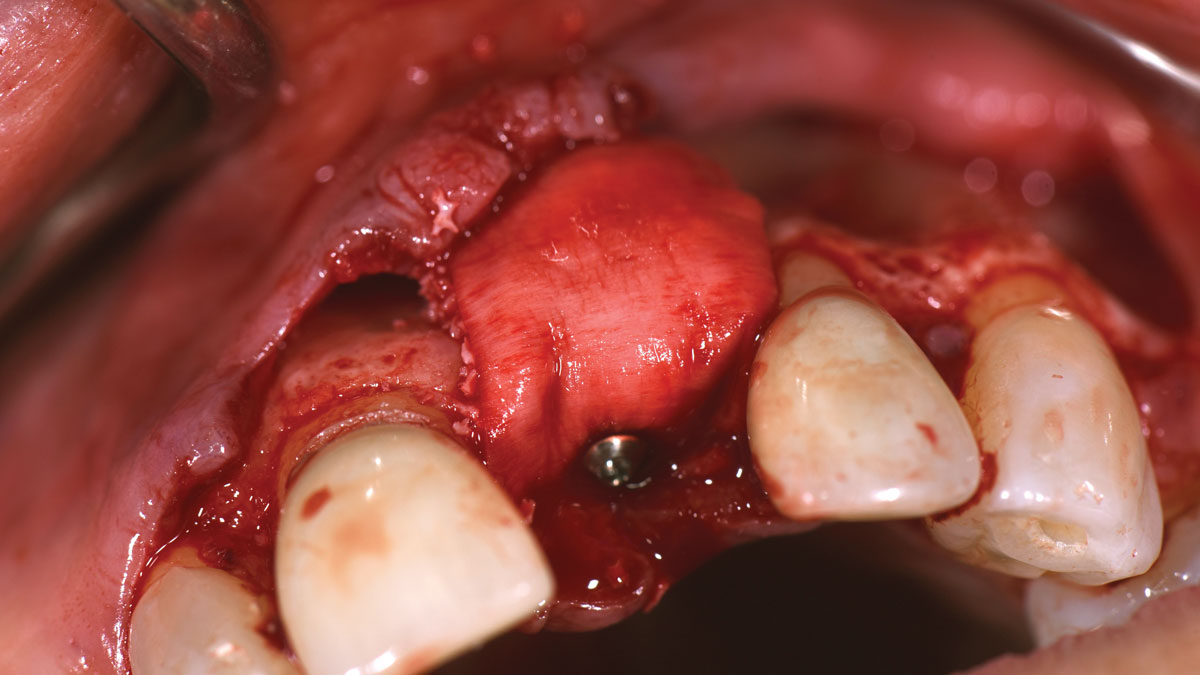
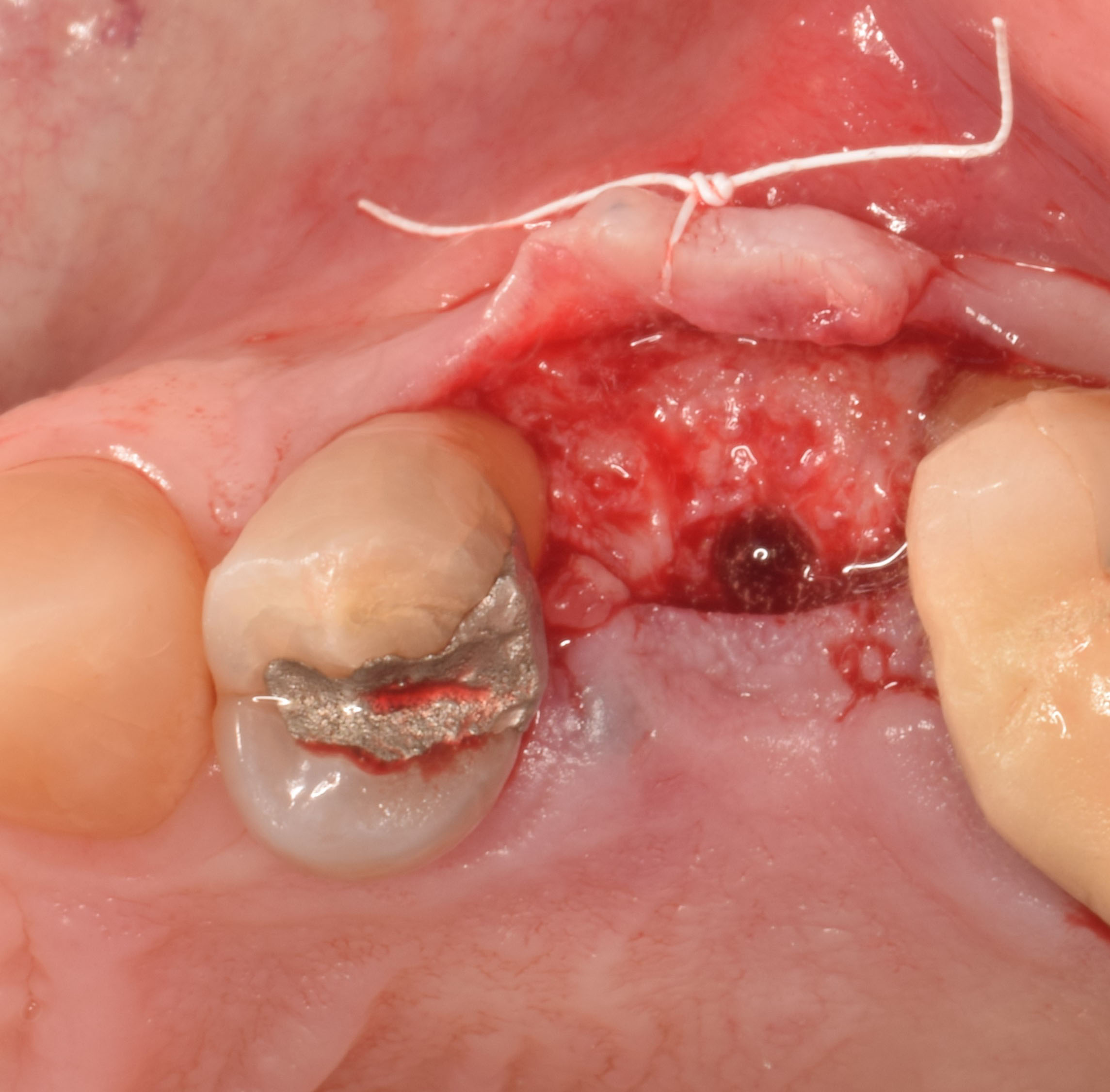
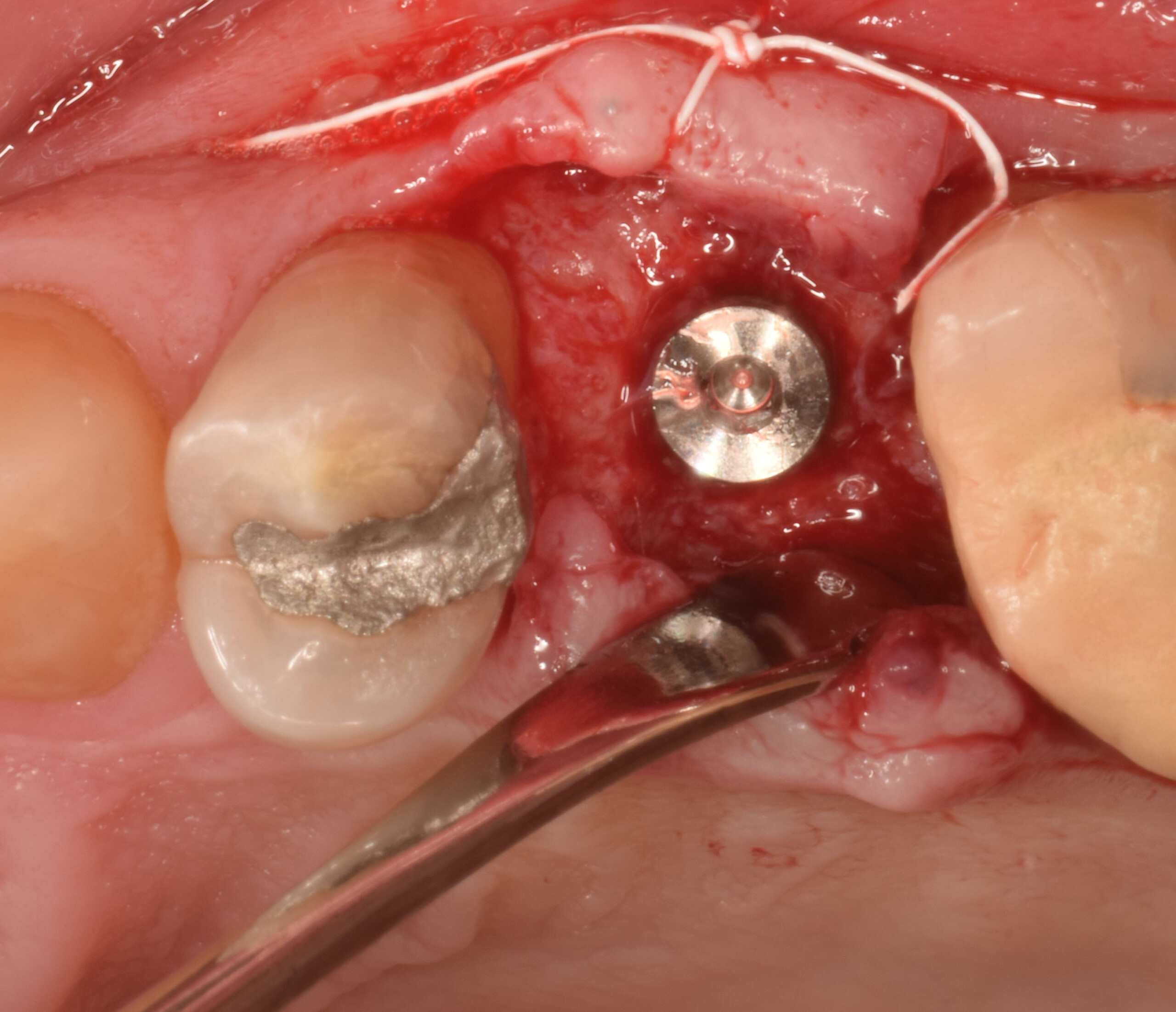
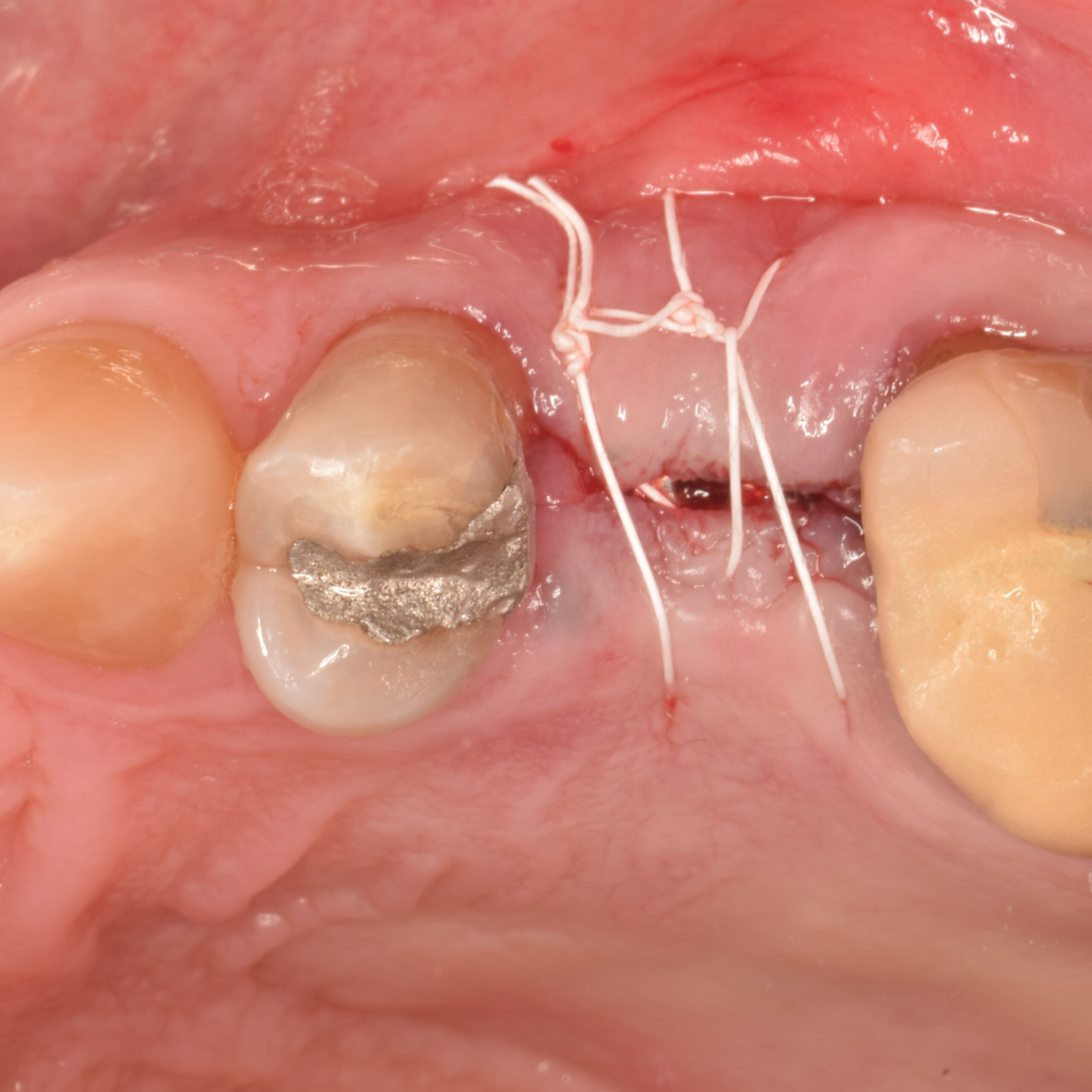
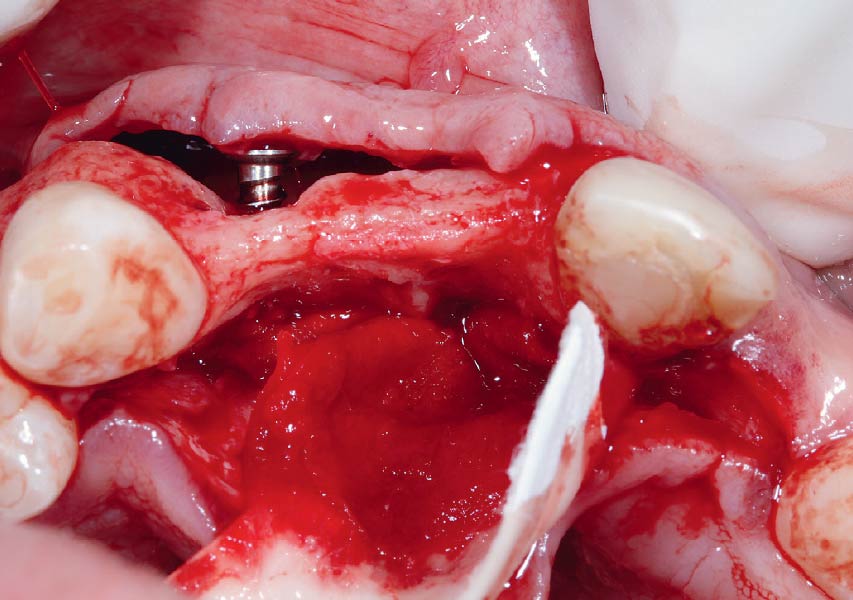
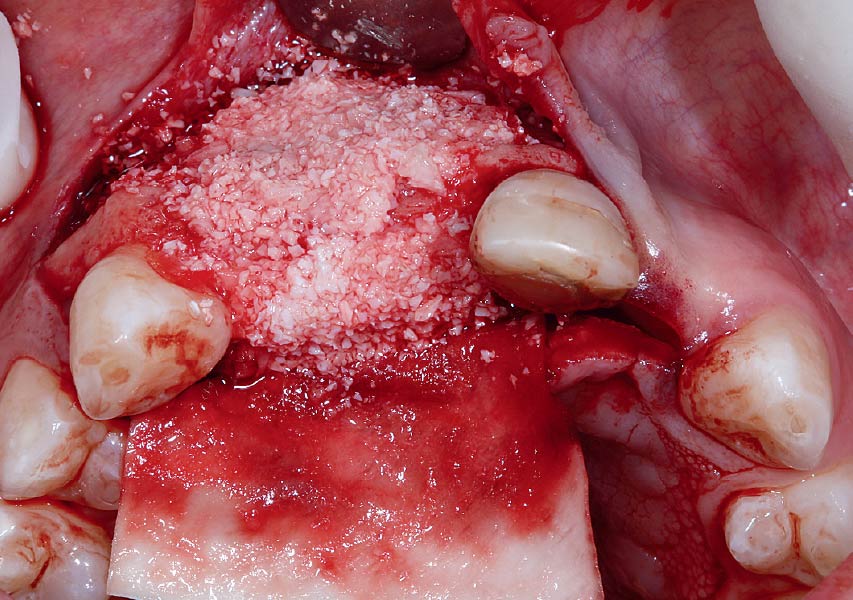
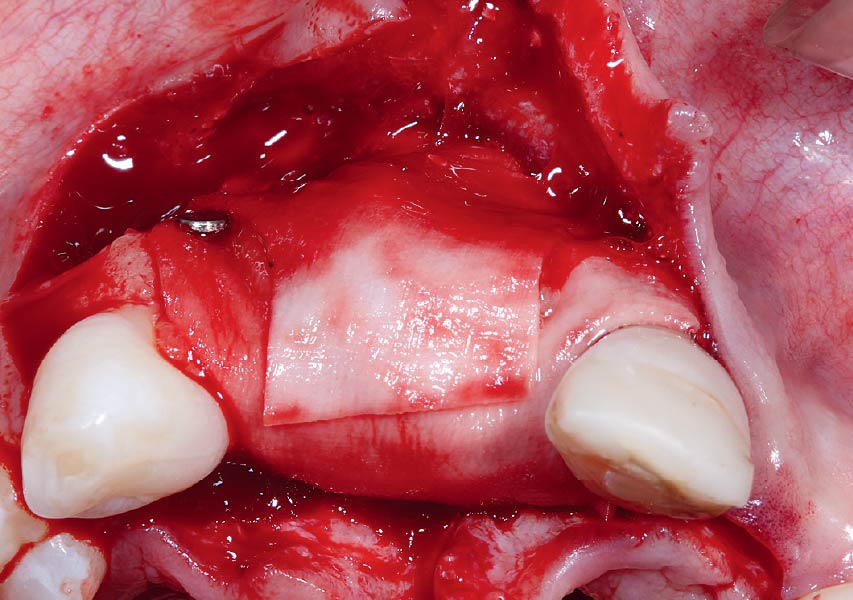
Horizontal ridge augmentation was performed using a horizontal layering technique. An inner layer of demineralized freeze-dried bone allograft (DFDBA), featuring vallos® demineralized cortical particles (to promote osteoinduction), was followed by an outer layer of deproteinized bovine bone, Geistlich Bio-Oss® (to maintain space and volume). The graft was contained with a native bilayer collagen membrane, Geistlich Bio-Gide®, and secured with titanium pins (tacks).
“By horizontally layering two distinct bone graft materials—Geistlich Bio-Oss® and vallos®—this approach was designed to tailor the regenerative environment, harnessing the unique osteoinductive potential of the allograft and the long-term space-maintaining properties of the xenograft to optimize both early bone formation and dimensional stability.”
— Eswar Kandaswamy, BDS, MS
THE OUTCOME
The 6-month post-operative CBCT evaluation demonstrated sufficient ridge width for restoratively driven implant placement, a result achieved through the utilization of vallos® and Geistlich Bio-Oss® bone graft materials.


Eswar Kandaswamy, BDS, MS
Dr. Eswar Kandaswamy, BDS MS, is an Assistant Professor at Louisiana State University Health Sciences Center, School of Dentistry. He earned his Dental Degree from Sri Ramachandra University, India, and practiced general dentistry for two years. He then completed his specialty training in Periodontics and a Master of Science at The Ohio State University.

Amber Kreko, DDS
Dr. Amber Kreko, DDS is a third-year Periodontics resident at Louisiana State University School of Dentistry, soon to earn her Master of Science. With a foundation in dental hygiene and six years of clinical practice in Southeast Louisiana,she returned to LSU for her DDS. Her comprehensive background enriches her approach to periodontal care. Upon graduation, she will transition to private practice.

BIOBRIEF
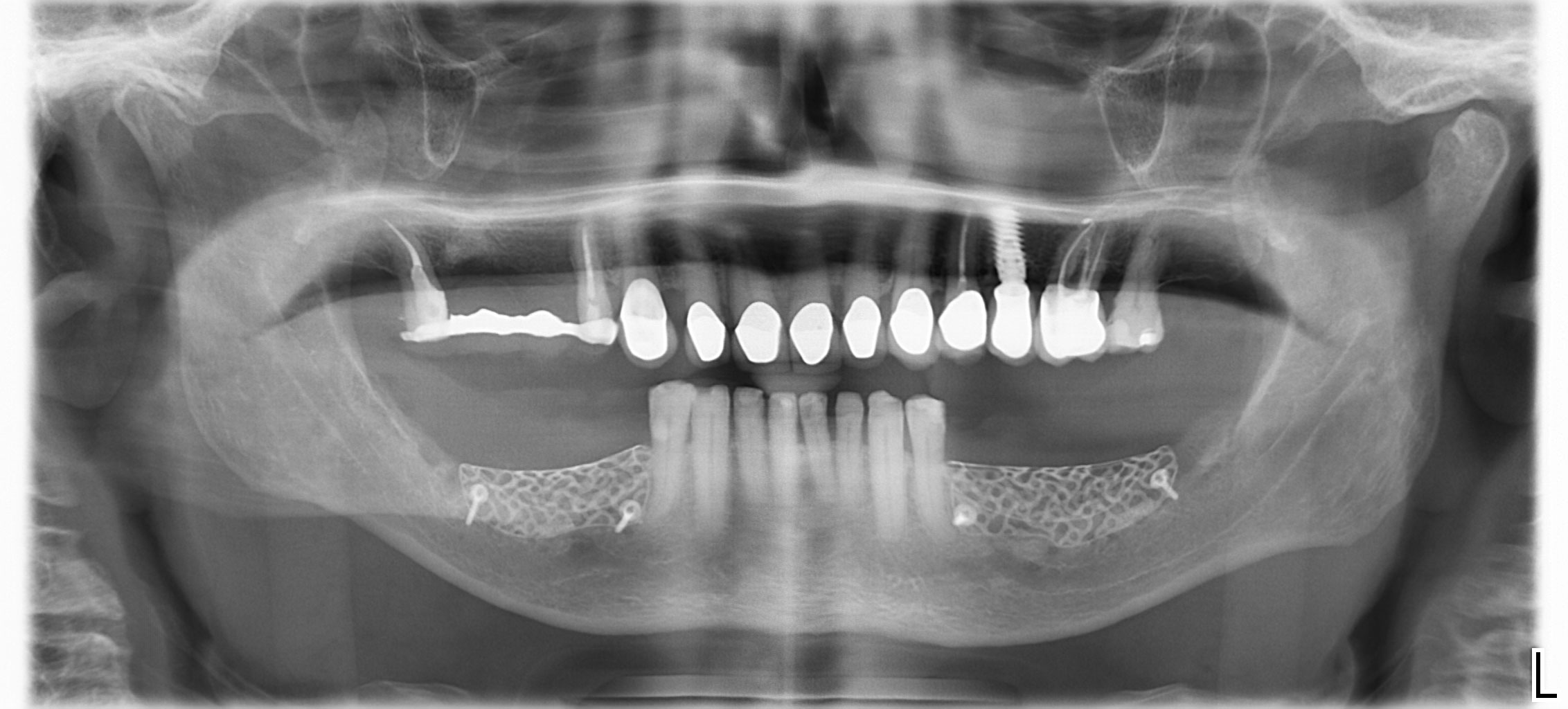
Lateral and Vertical Bone Regeneration with Simultaneous Soft Tissue Augmentation


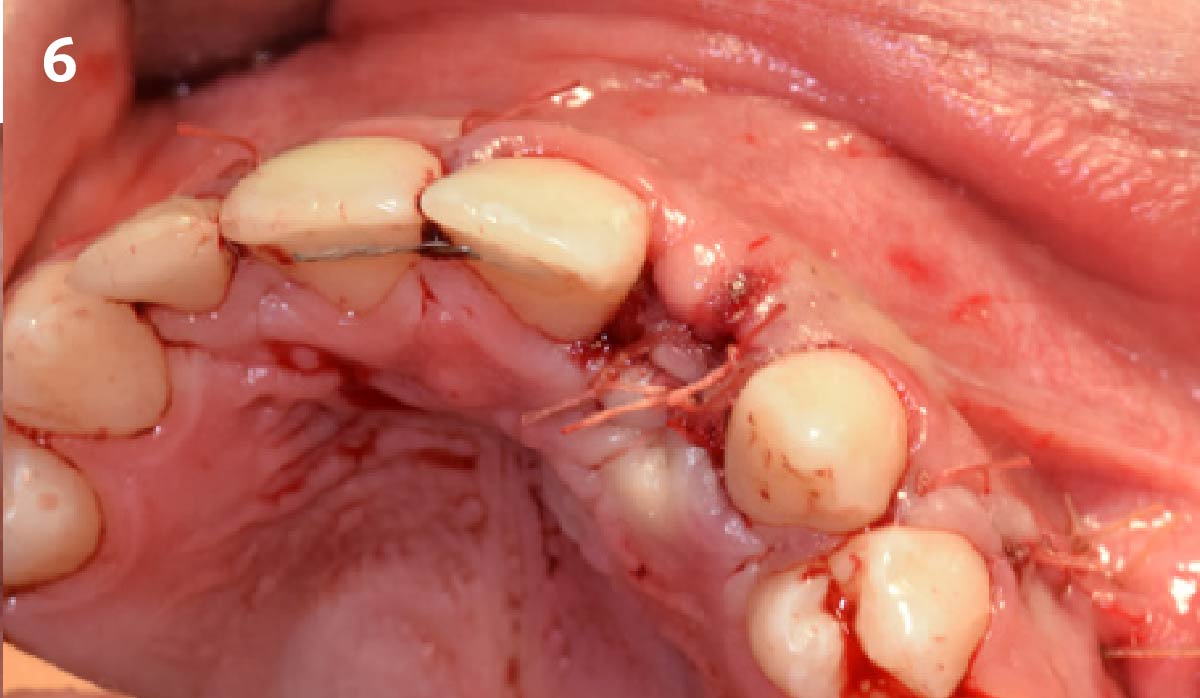
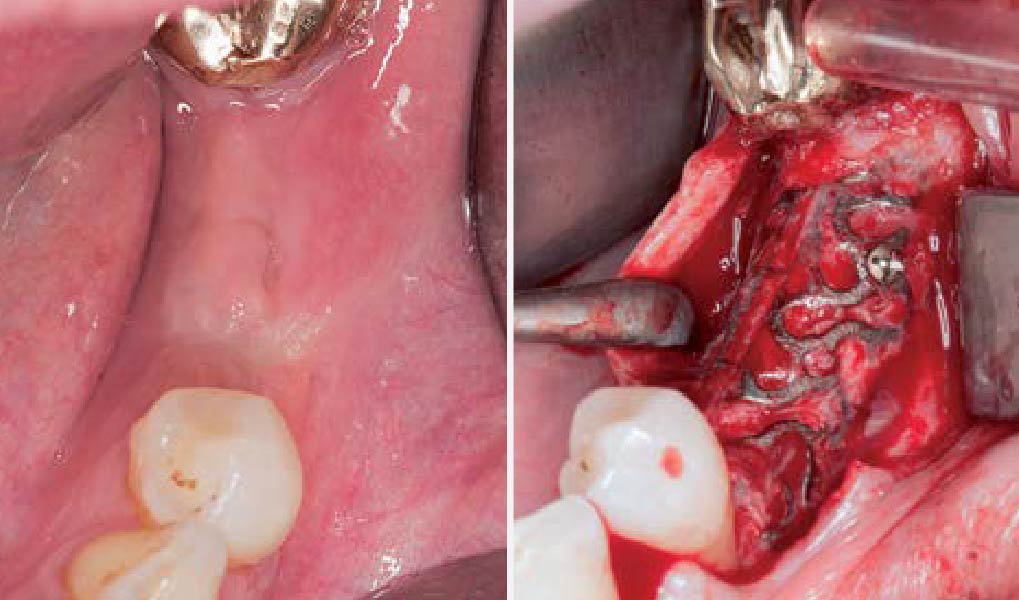
THE SITUATION
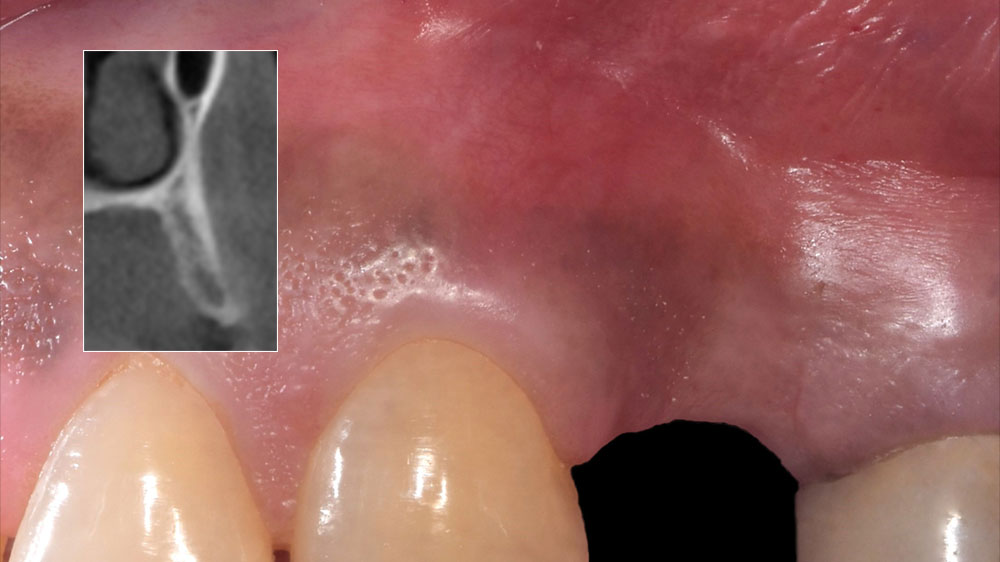
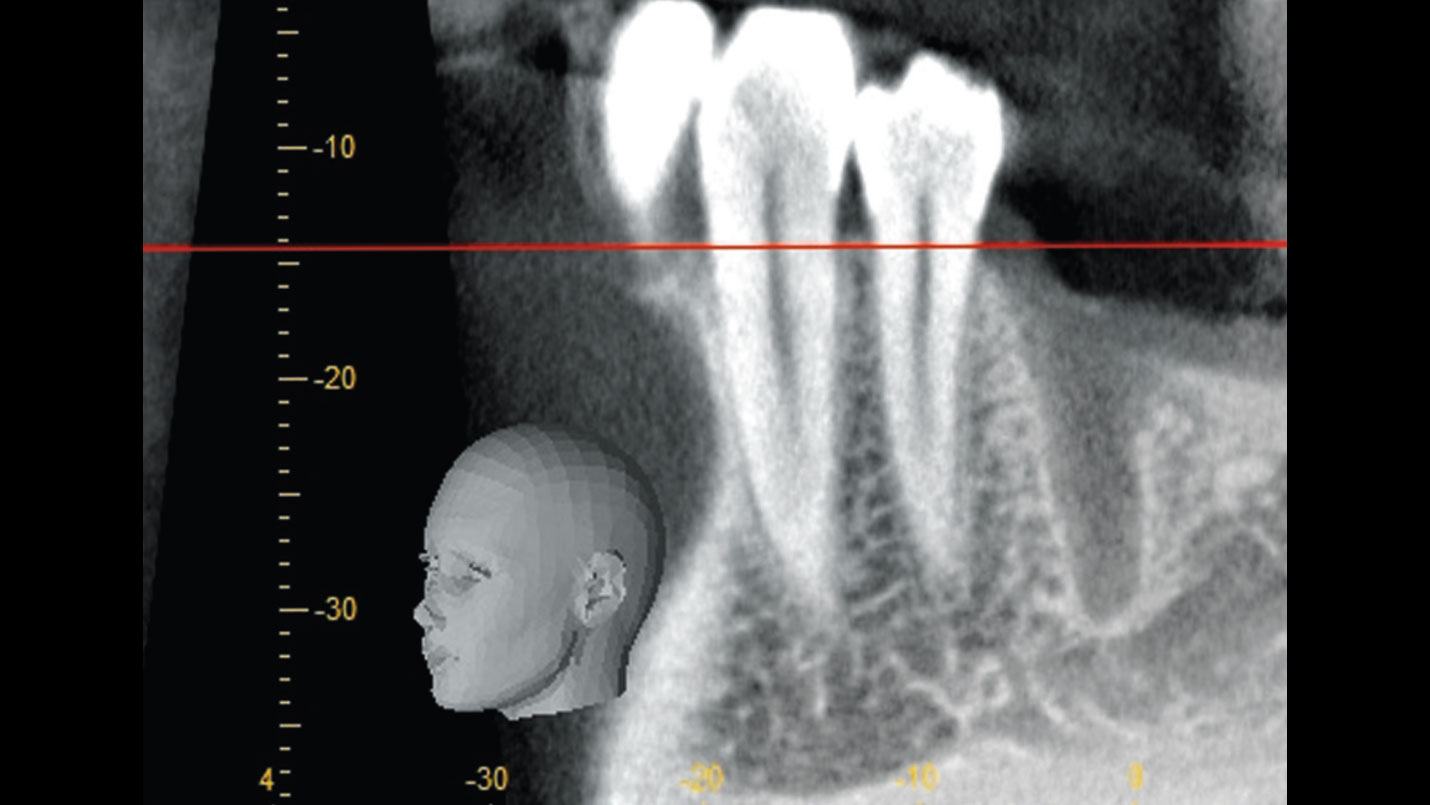
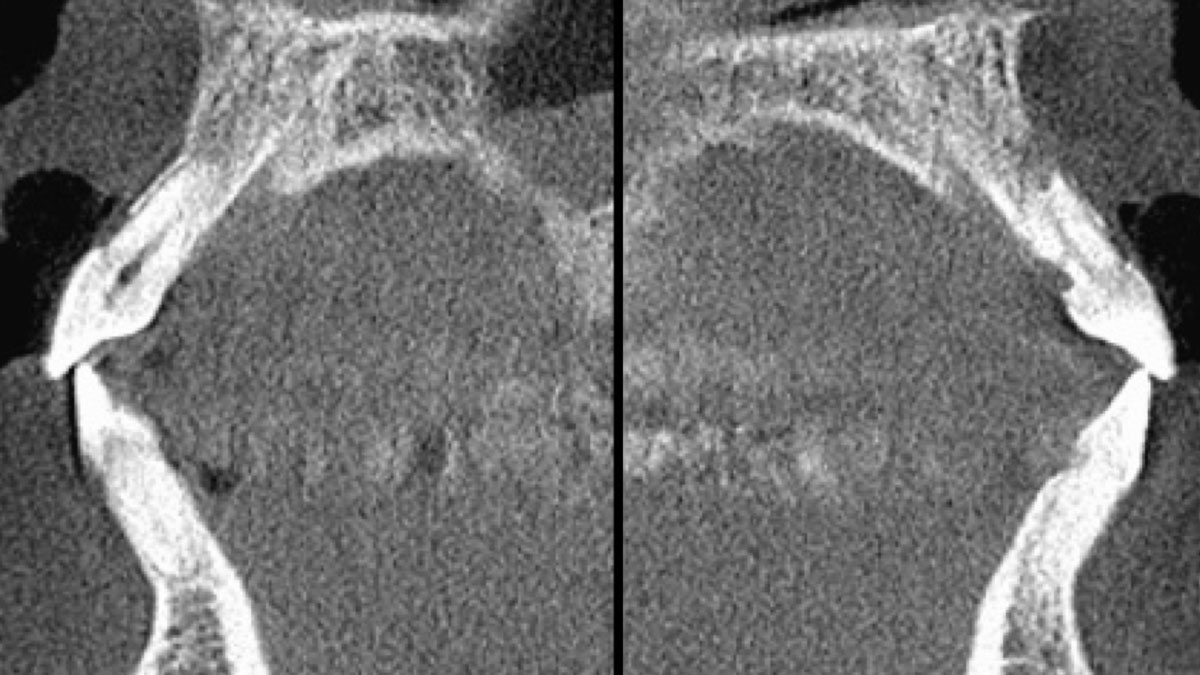
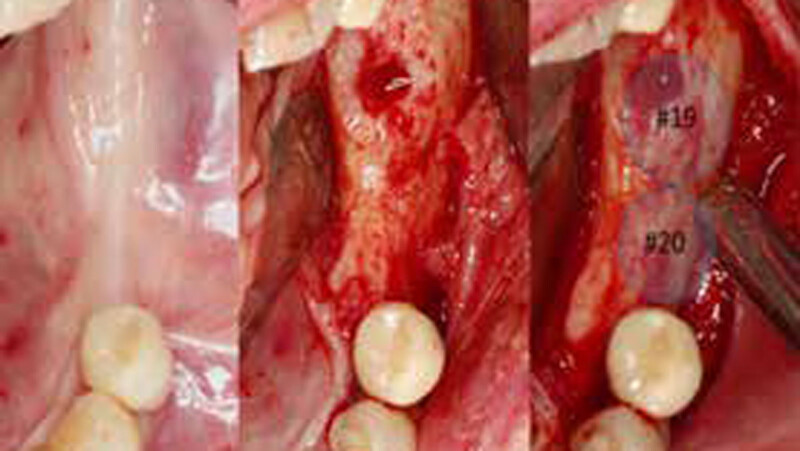
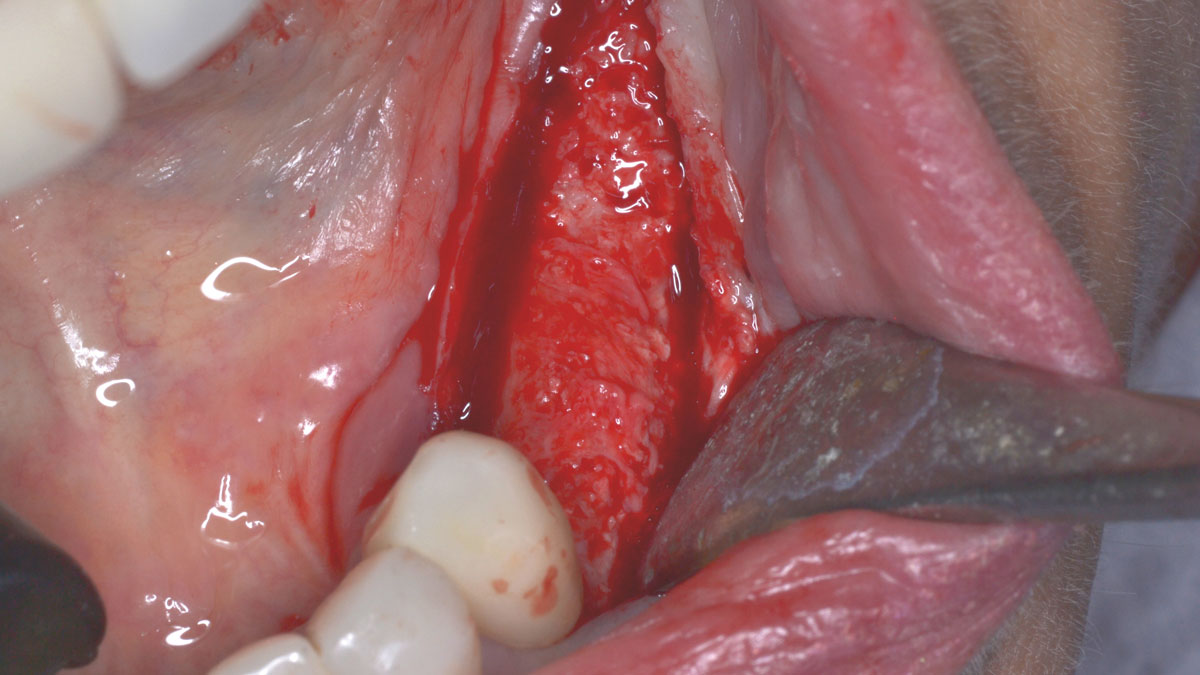
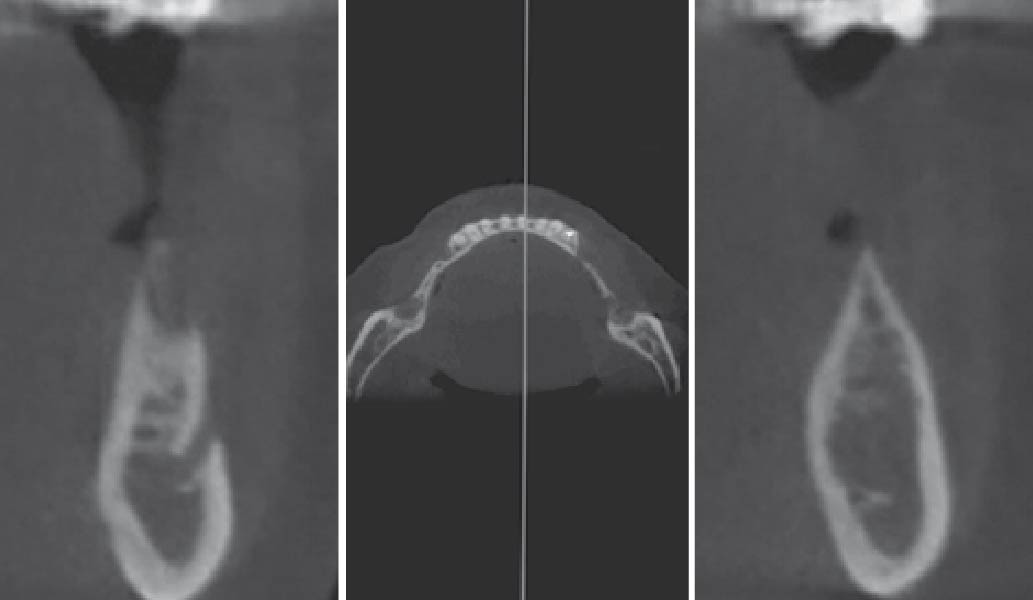
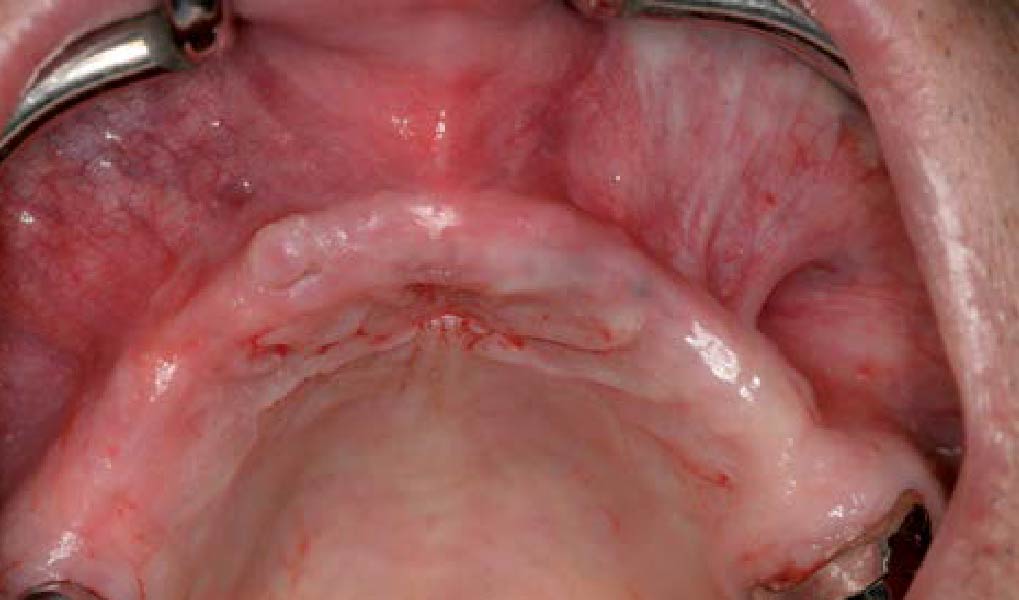
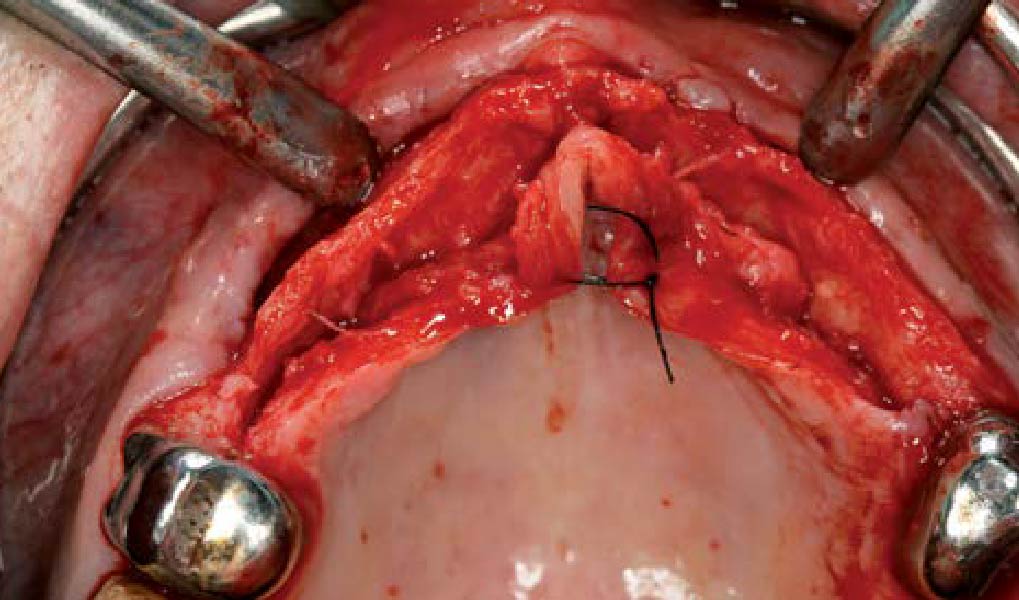
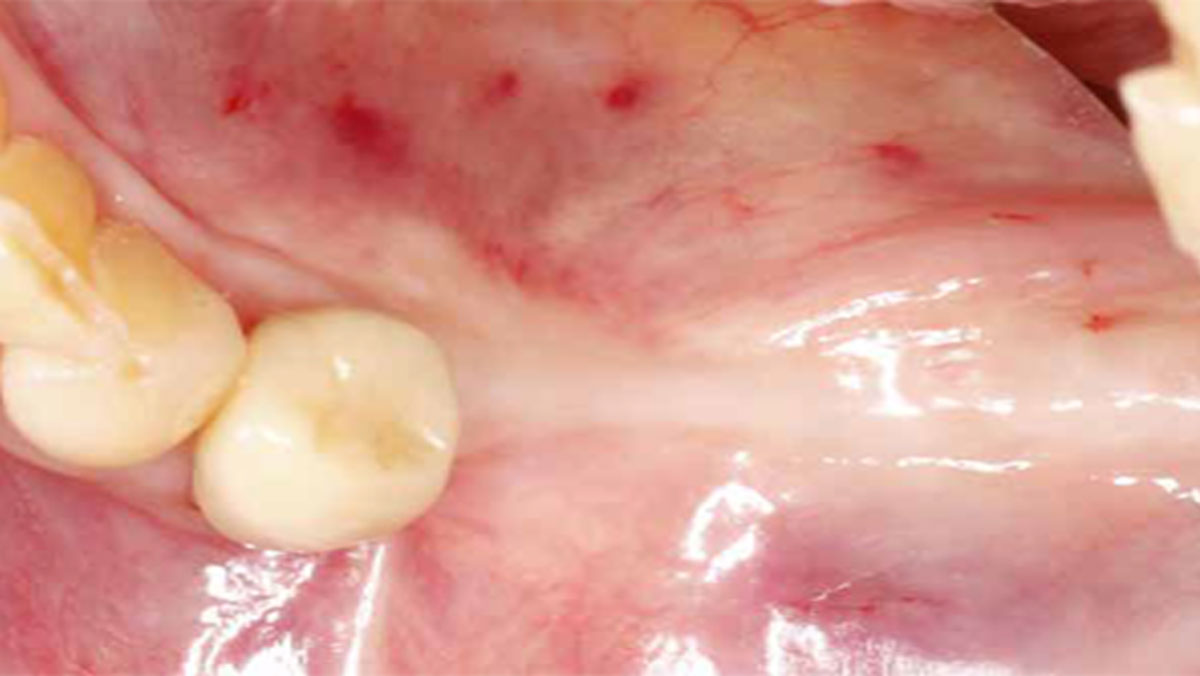
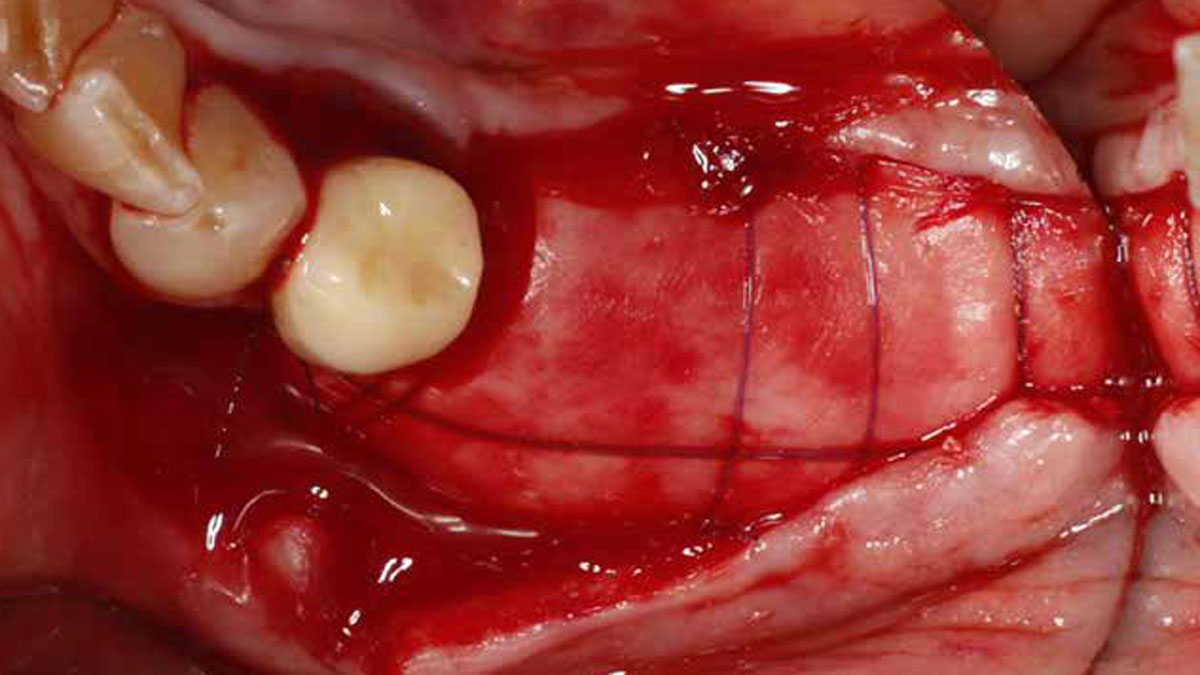
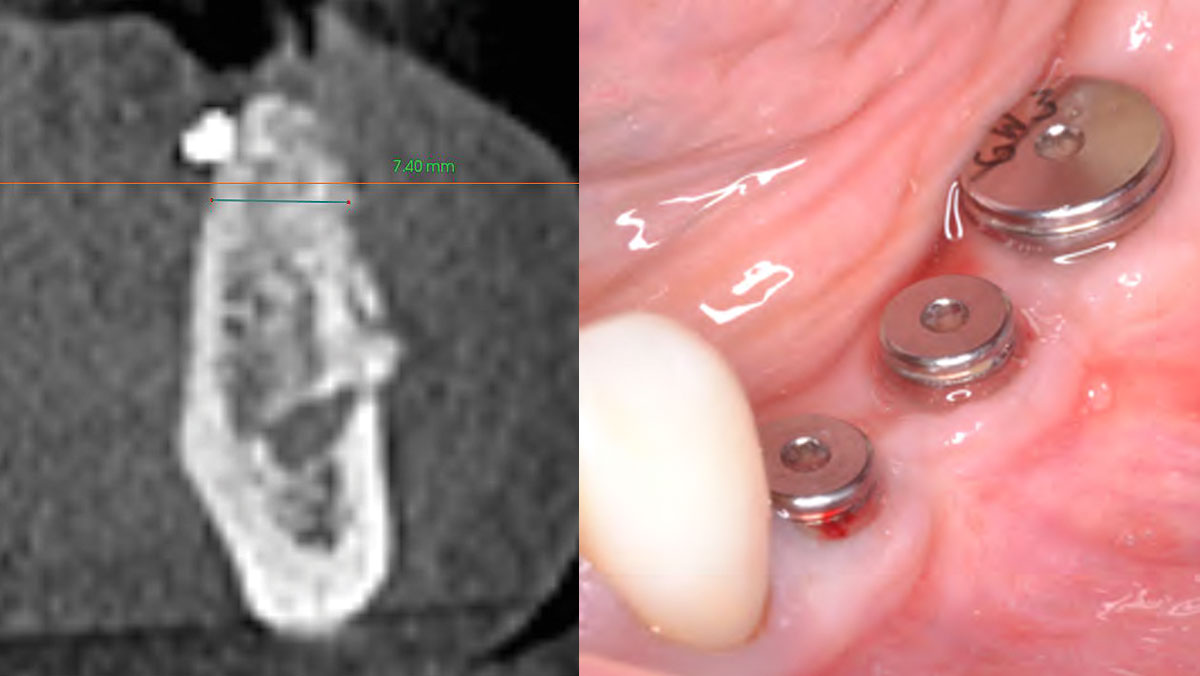
After extraction of the periodontally damaged tooth #20 the preoperative Cone-Beam Computed Tomography (CBCT) imaging shows reduced vertical bone volume in the area of tooth #s 18 – 20. A lateral and vertical bone regeneration was necessary.
The goal of treatment was a late implant placement after bone regeneration and creation of stable periimplant soft tissue for long-term implant preservation.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
Additional Risk Factors: Roots were divergent, and intra-radicular bone (septal bone) was excellent, with more than 5 mm of remaining apical bone to achieve optimal primary stability.
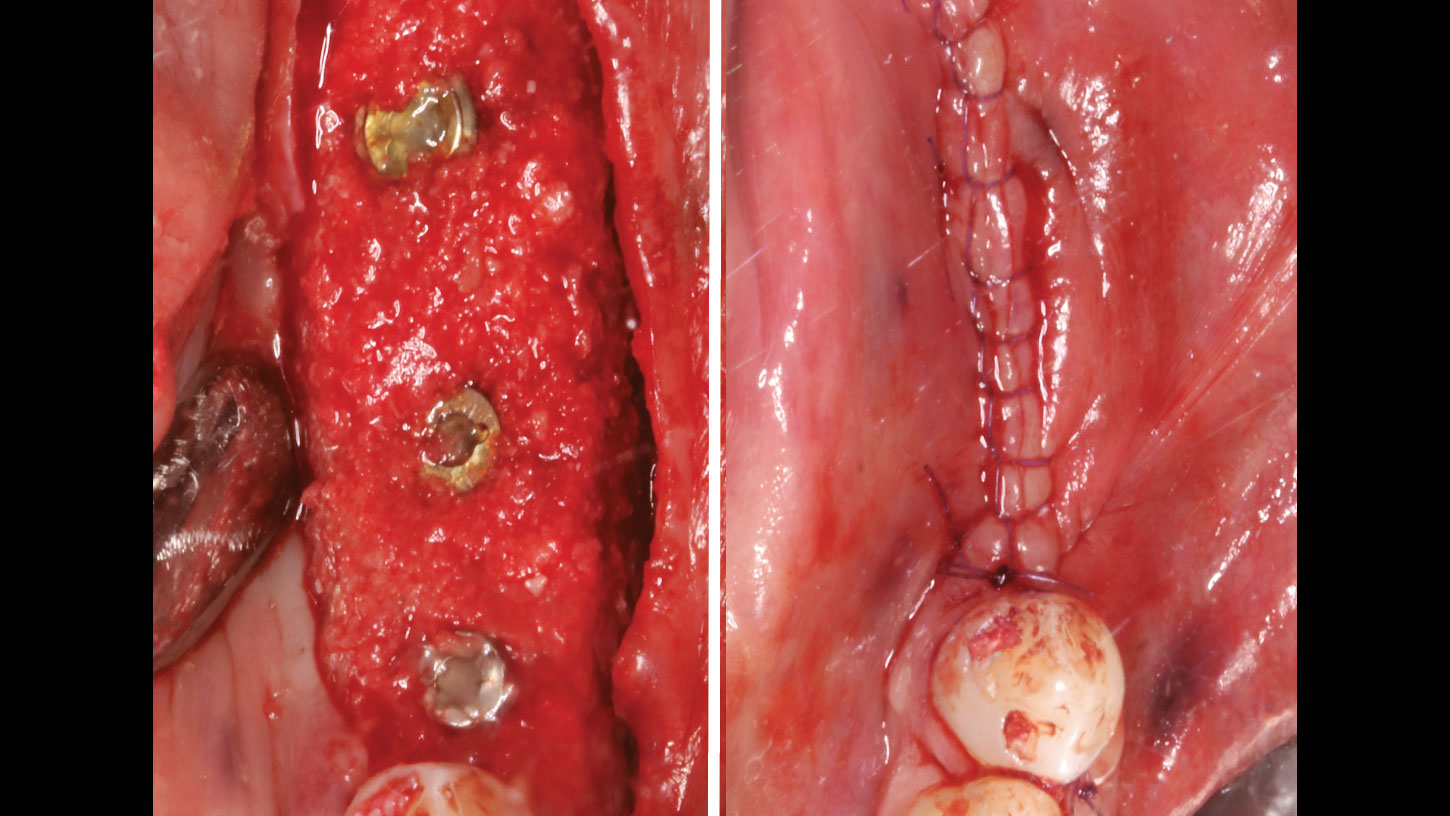
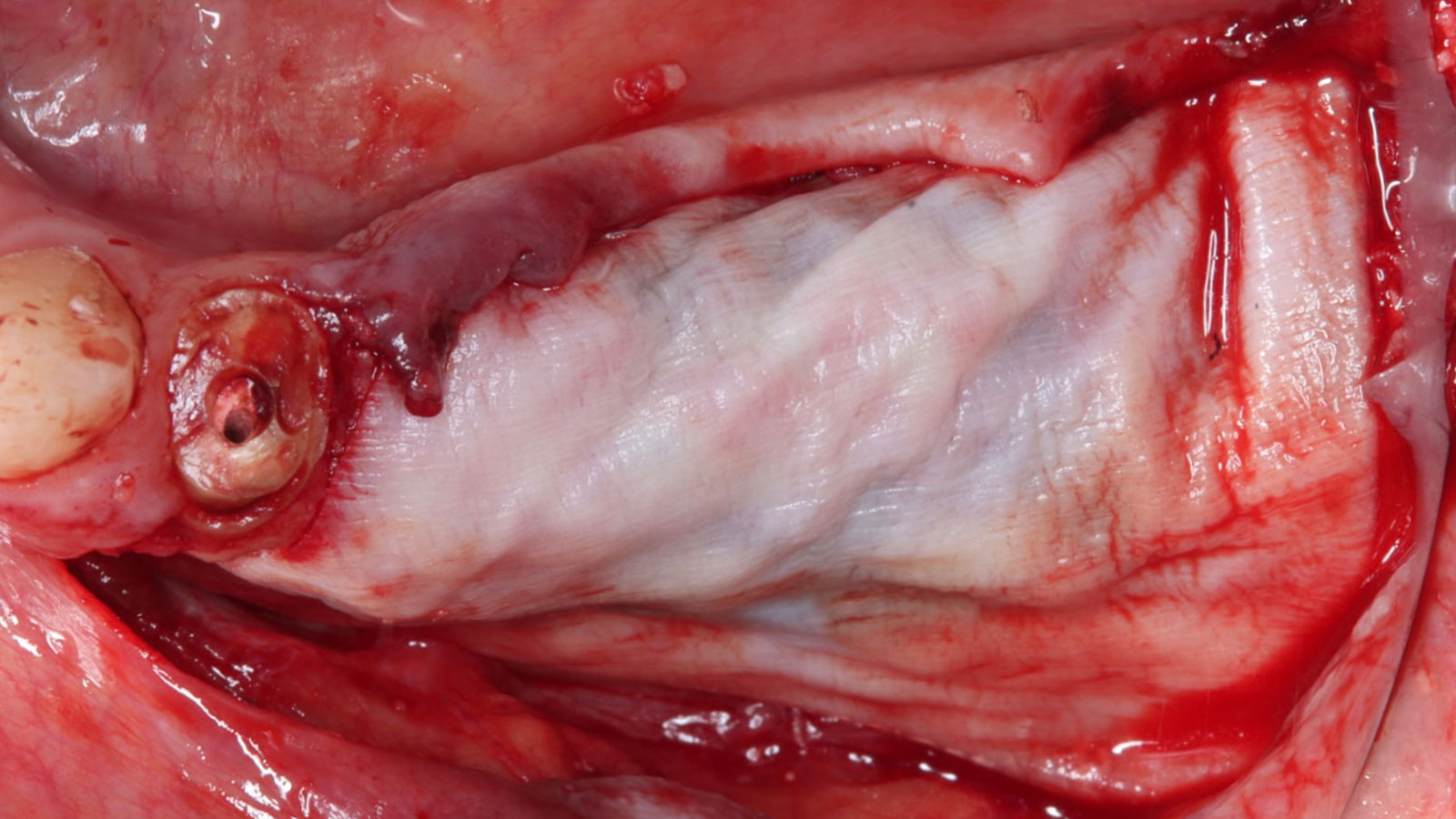
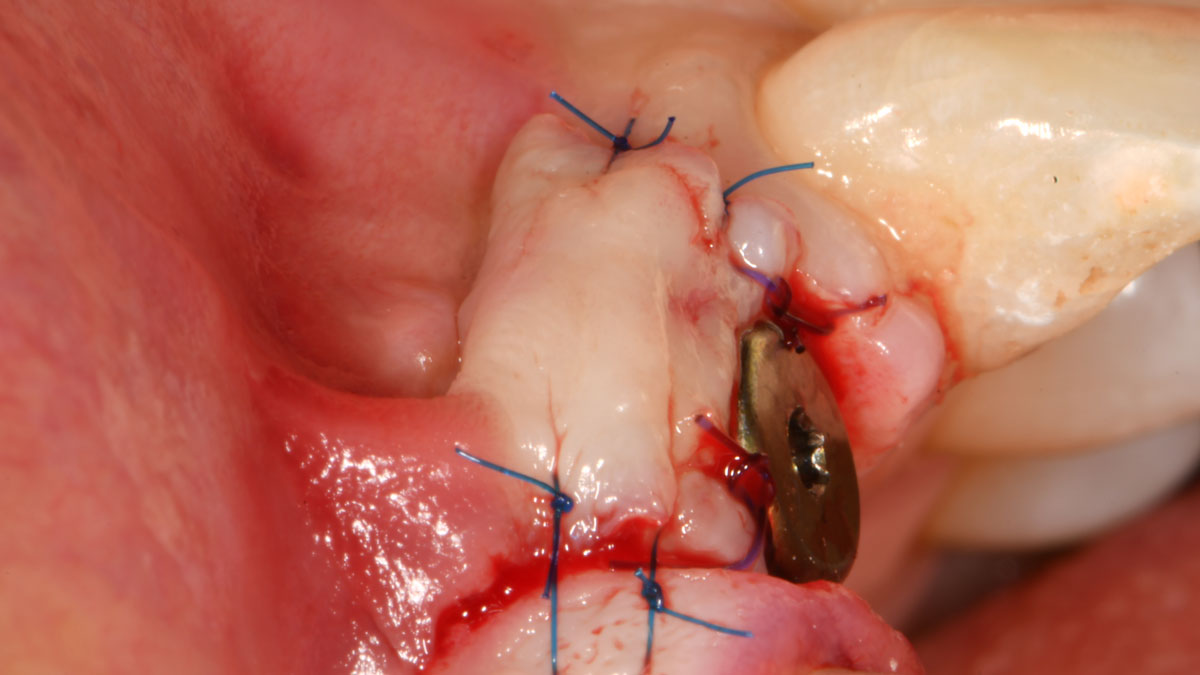
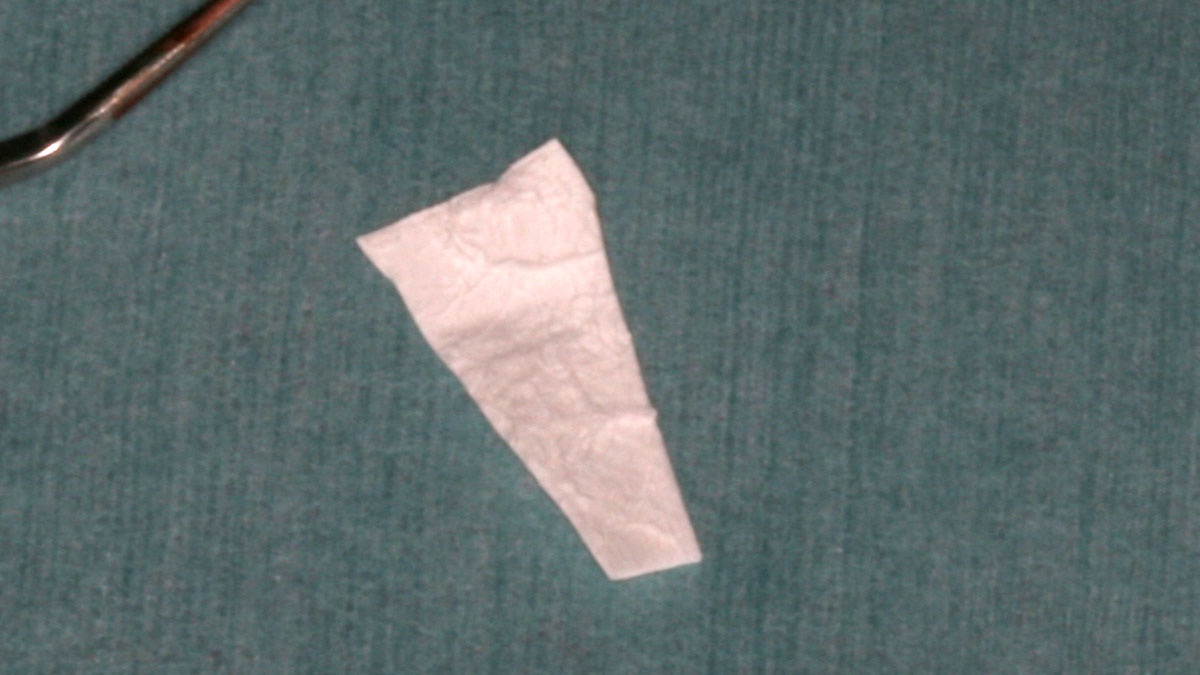
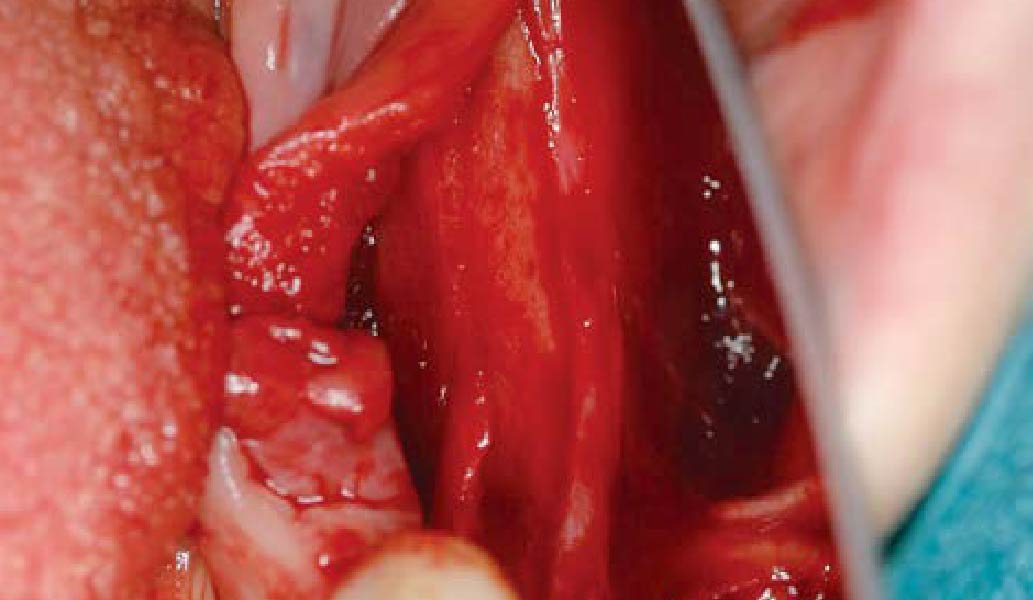
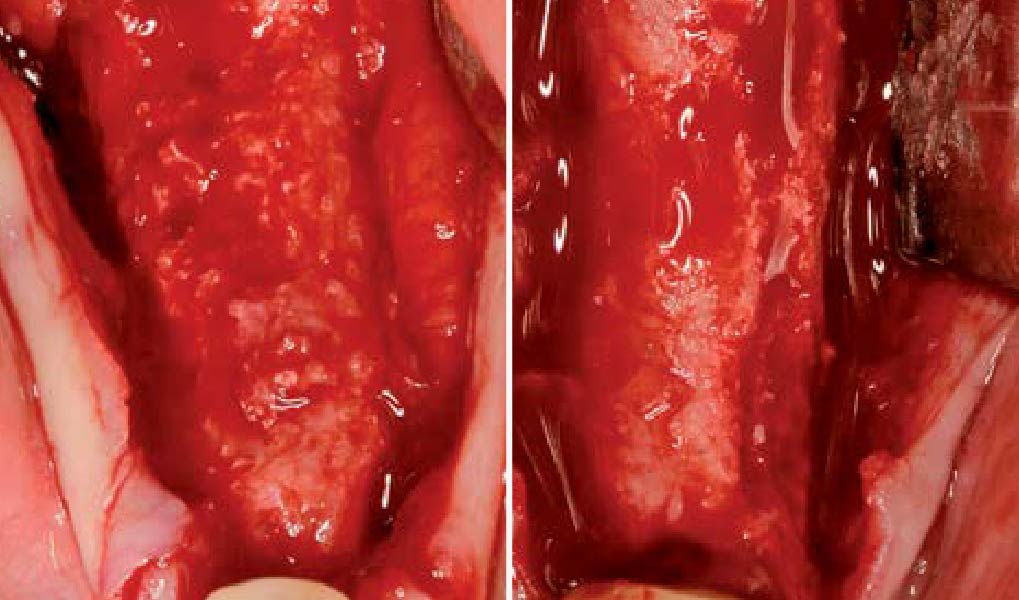
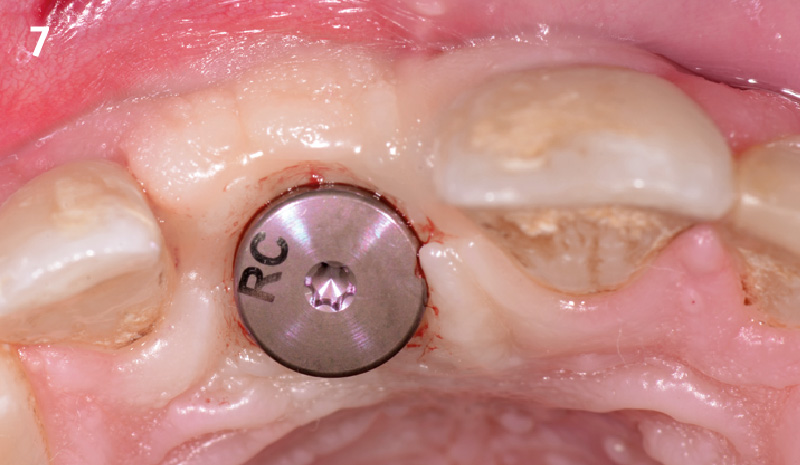
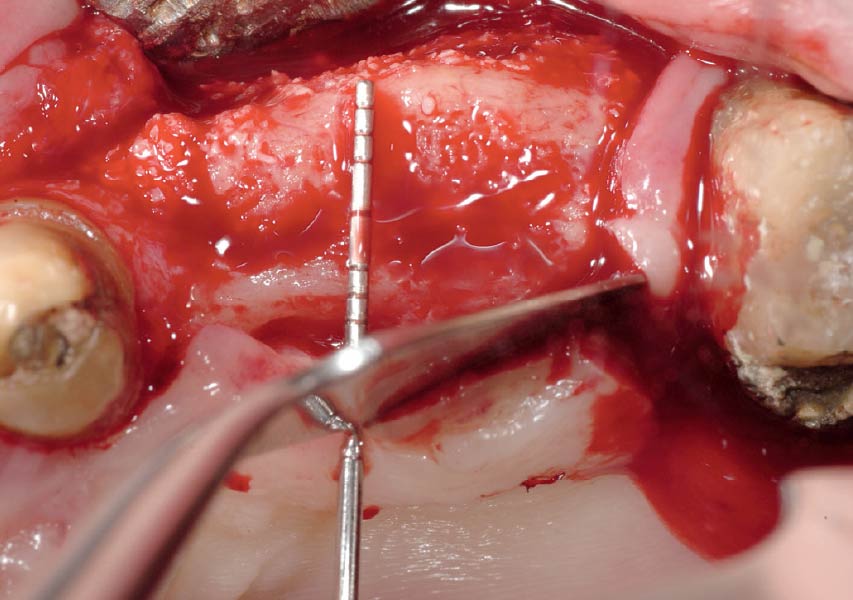
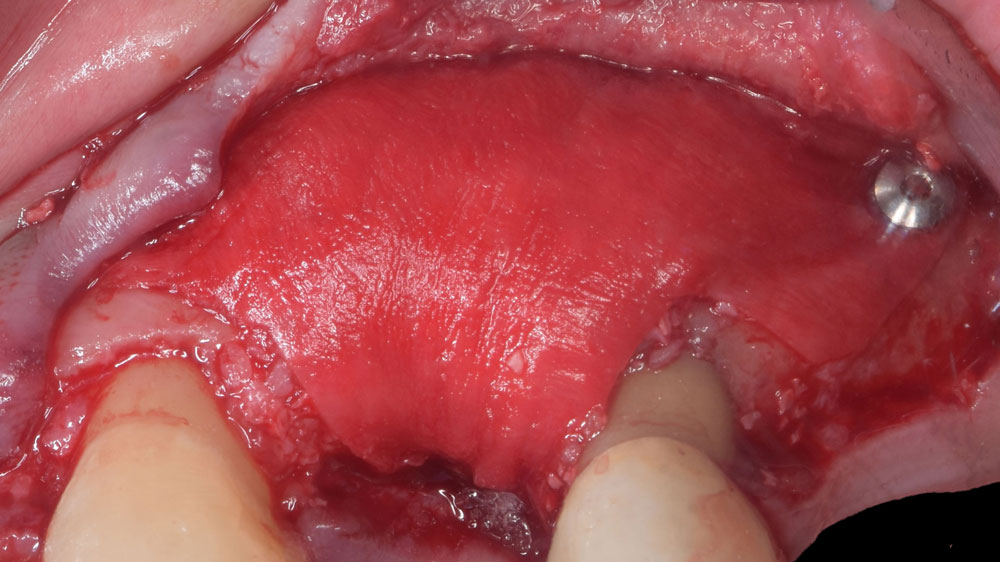
THE APPROACH
A customized bone regeneration procedure utilizing Yxoss CBR®. Followed by coverage of the graft with Geistlich Bio-Gide® for the purpose of Guided Bone Regeneration (GBR). Soft tissue thickening using Geistlich Fibro-Gide®. Delayed implantation into the augmented tissue. A vestibuloplasty with Geistlich Mucograft® for the regeneration of keratinized mucosa.
“Using the Geistlich Fibro-Gide® matrix enabled concurrent augmentation of hard
— Arnd Lohmann, MSc
and soft tissues without any postoperative complications. At the same time, the soft
tissue thickening facilitated floor of the mouth surgery and vestibuloplasty.”
THE OUTCOME
Treatment resulted in approximately 5 mm of vertical bone regeneration. The potential occurrence of a dehiscence associated with a wound opening and exposure of Yxoss CBR® was able to be prevented with Geistlich Fibro-Gide®.
On one hand, the quality of the peri-implant soft tissue was improved by the
soft tissue thickening with Geistlich Fibro‑Gide® and, on the other, by increasing the width of keratinized mucosa with Geistlich Mucograft®. The treatment method chosen resulted in a reduced invasiveness and morbidity by avoiding a donor site for sourcing a transplant.


Arnd Lohmann, MSc
Dr. Arnd Lohmann is a recognized specialist in implantology and periodontology. He earned his dental license in Hamburg in 2002, completed his doctorate in 2003, and has been a partner at a private practice in Bremen since then.
With a Master of Science in Implantology (2007), he specializes in dental implantology and bone augmentation. He is an active speaker at national and international congresses, leads the Bremen study group of the German Society of Oral Implantology (DGOI), and is a member of DGOI, DGZI, and DGI. His practice is equipped with state-of-the-art technology, ensuring high-quality patient care.

BIOBRIEF
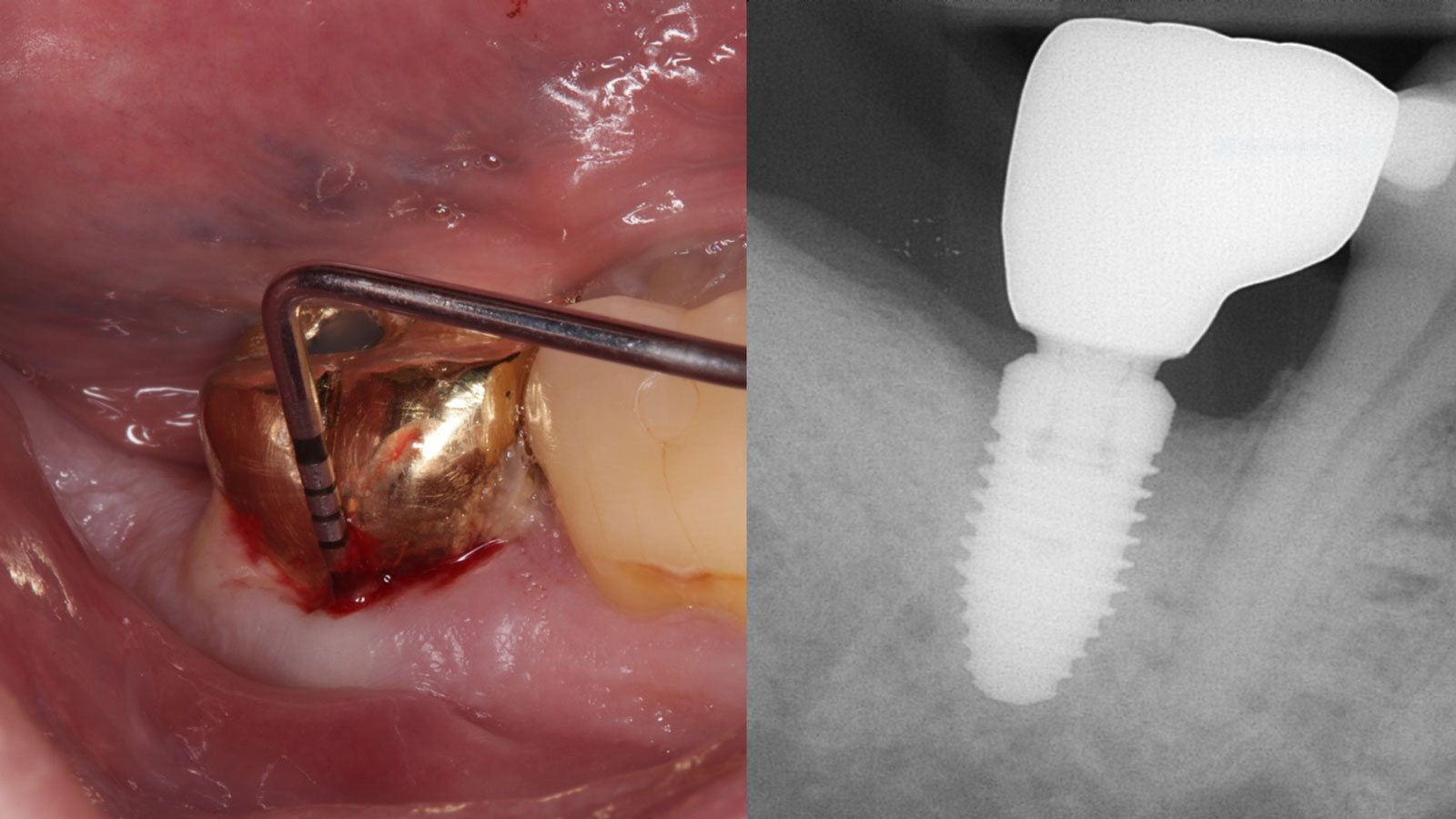
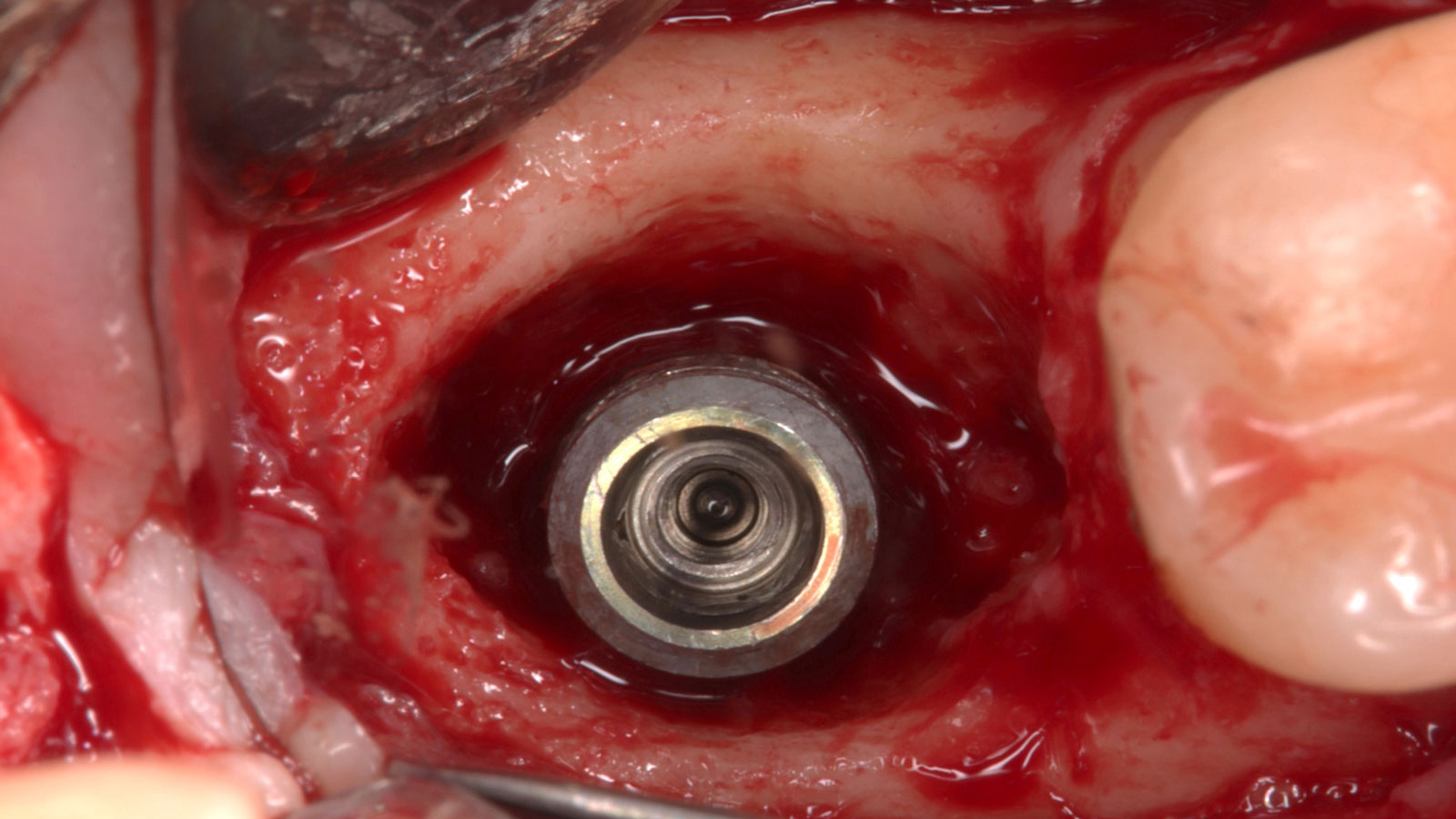
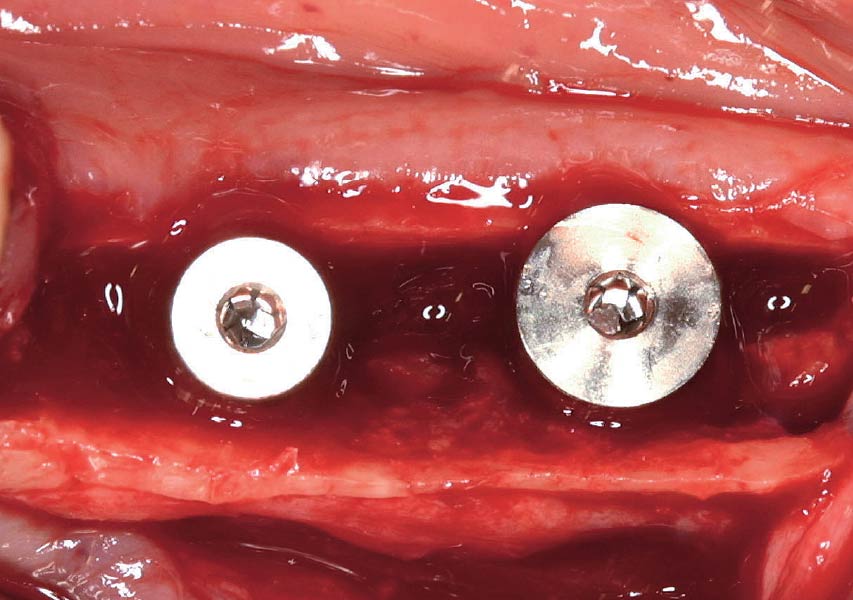
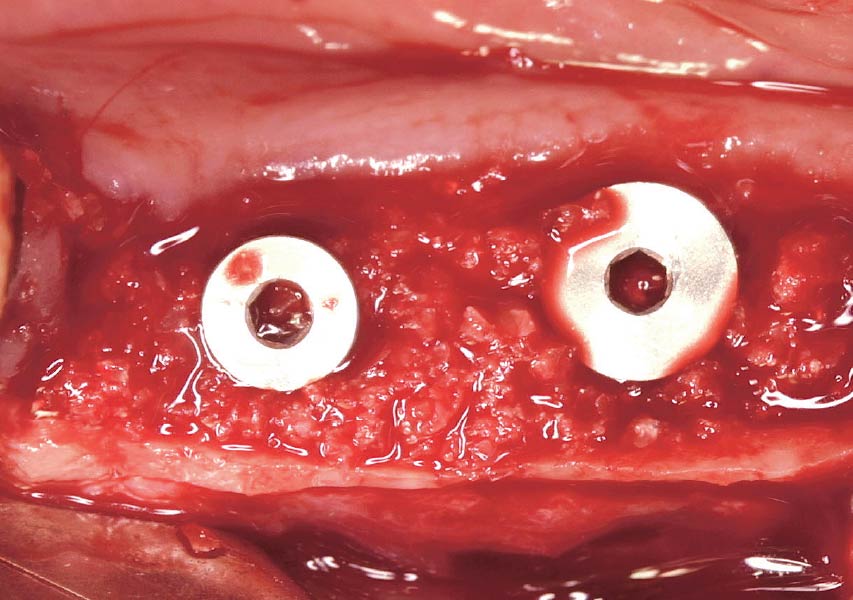
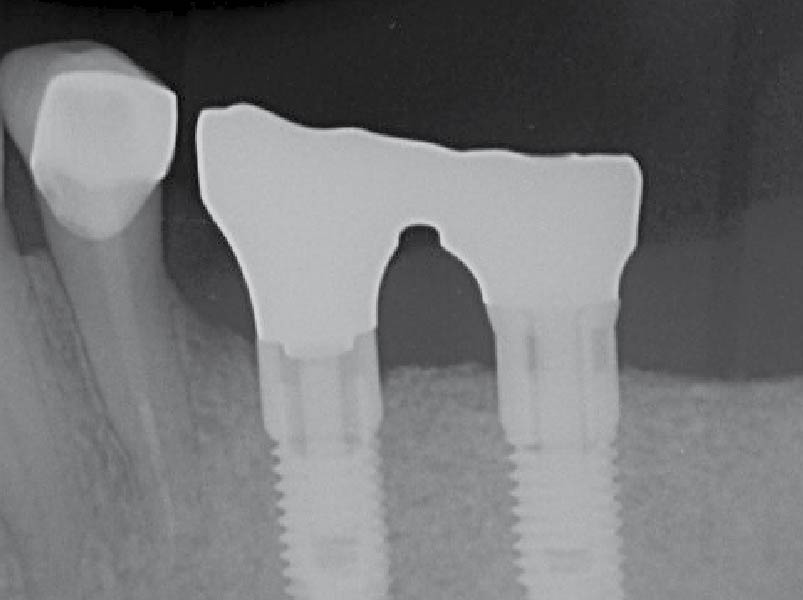
Prosthetic-Surgical Approach to Regenerative Treatment for Peri-Implantitis


THE SITUATION
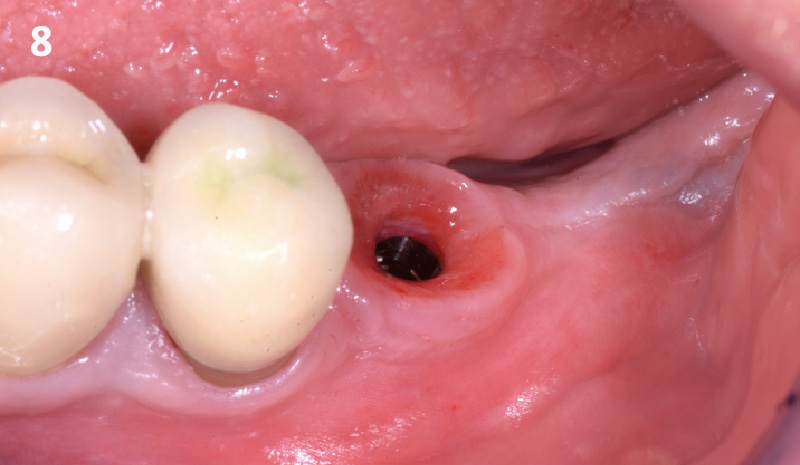
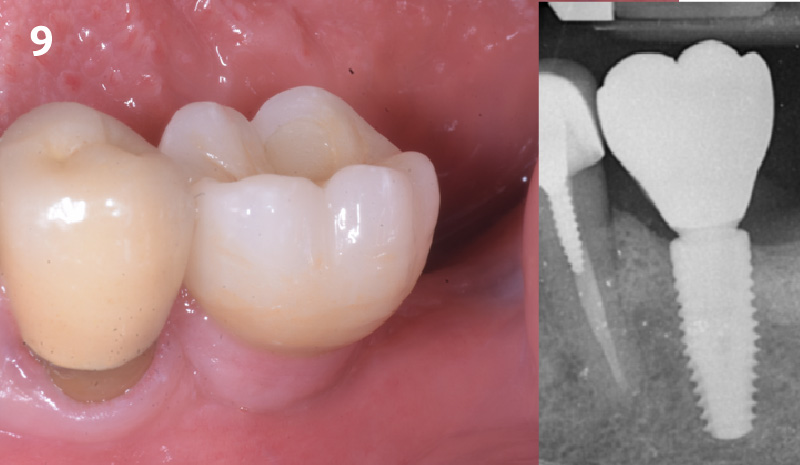
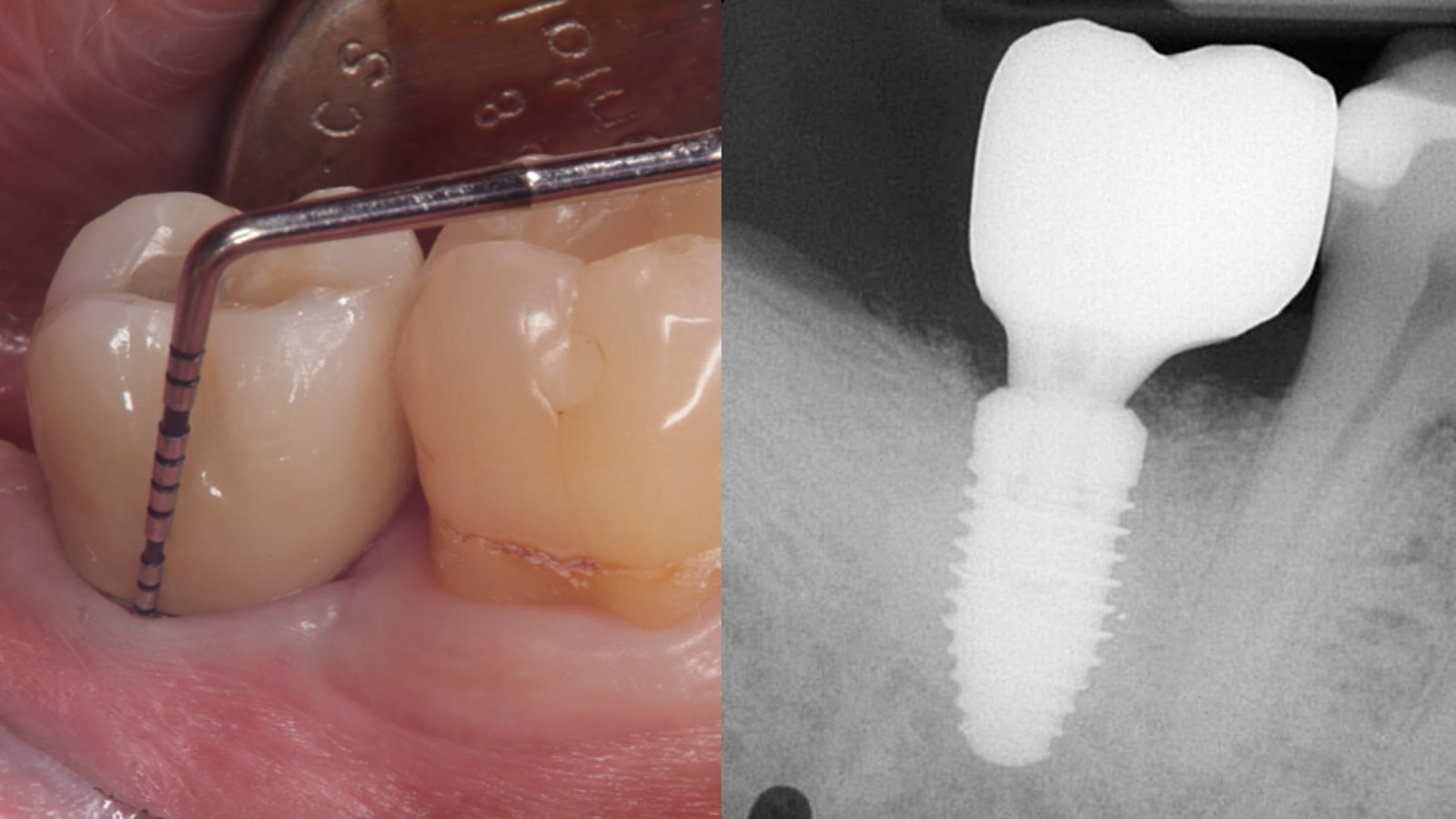
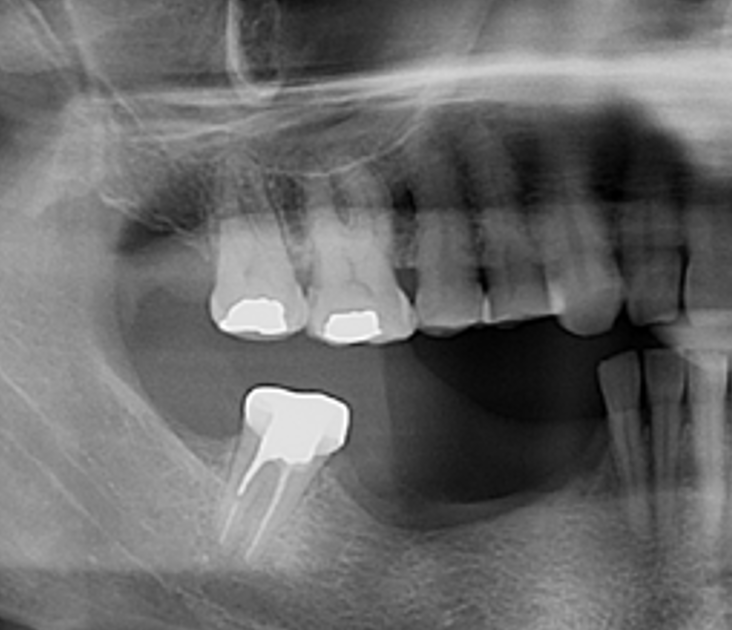
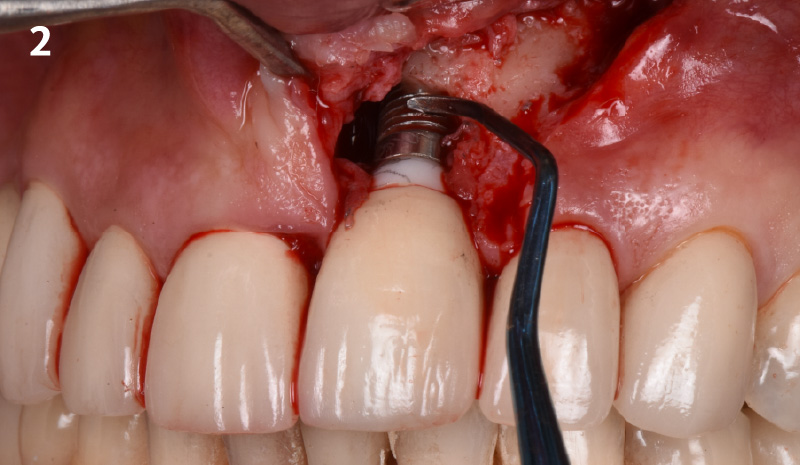
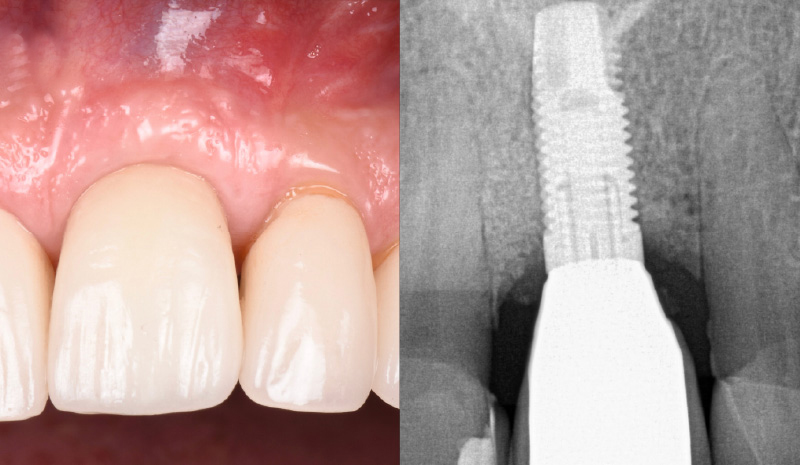
A 68-year-old male patient, who received an implant in tooth position #31 about 8 years prior, presented for an examination. He reports bleeding during brushing around the implant and some discomfort. Clinically, there was severe vertical bone loss, profuse bleeding on probing, and deep probing depths, but no pain. The condition was diagnosed as peri-implantitis according to the 2018 classification.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Infection at implant sight | None | Chronic | Acute |
| Restorative status of adjacent tooth | Intact | Restored | |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
Additional Risk Factors: The patient exhibited bleeding on probing and deep pocket depths. He also reported occasional marijuana use and was inconsistent with periodontal maintenance and oral hygiene visits.
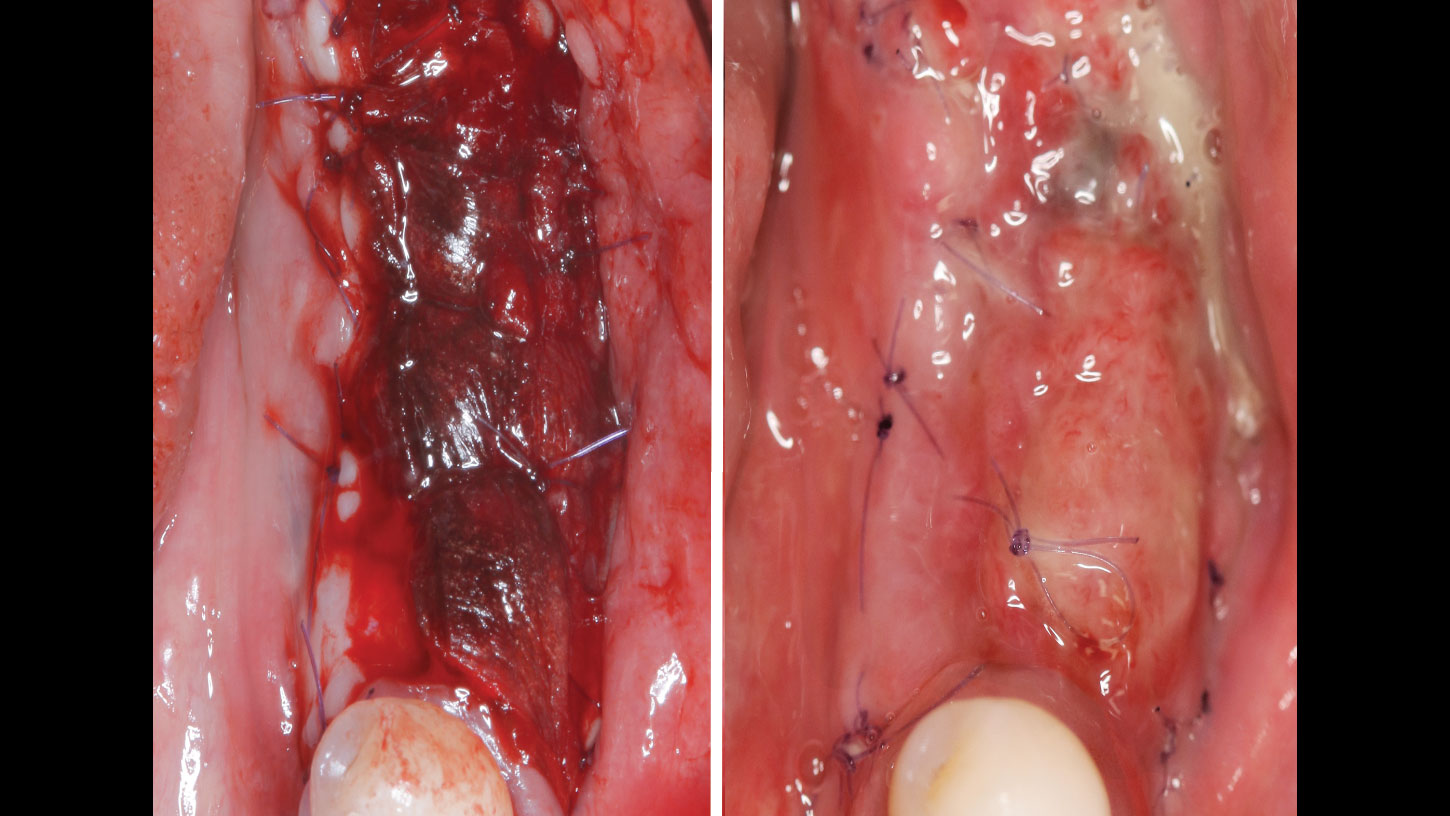
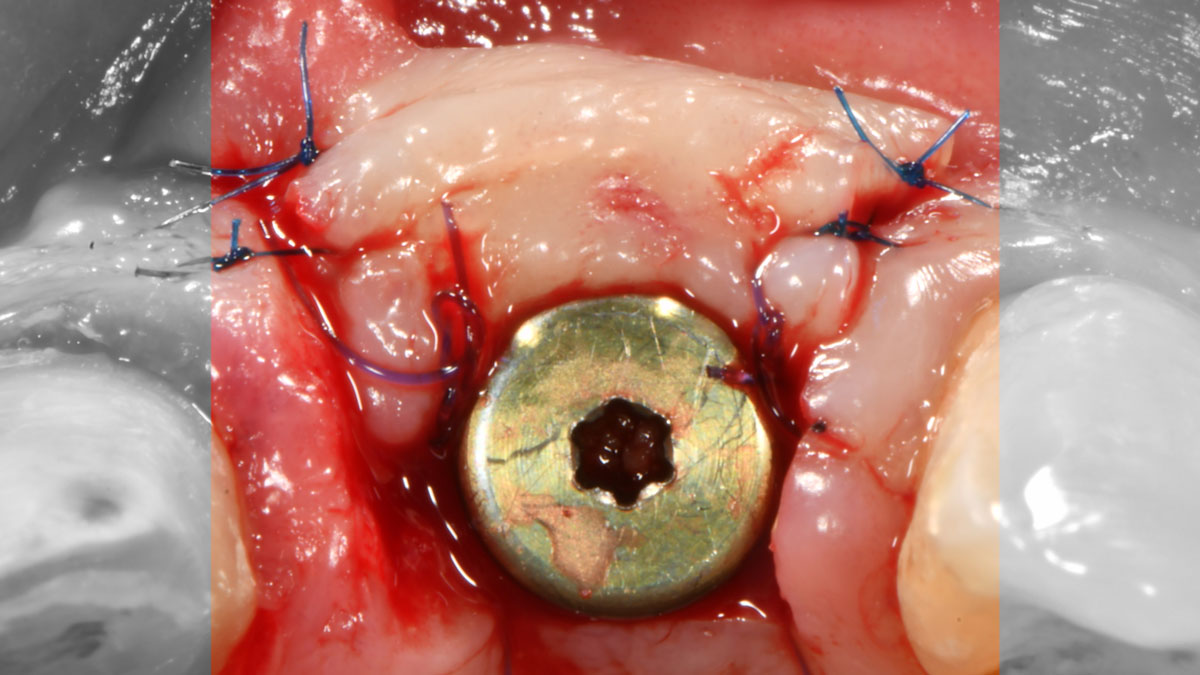
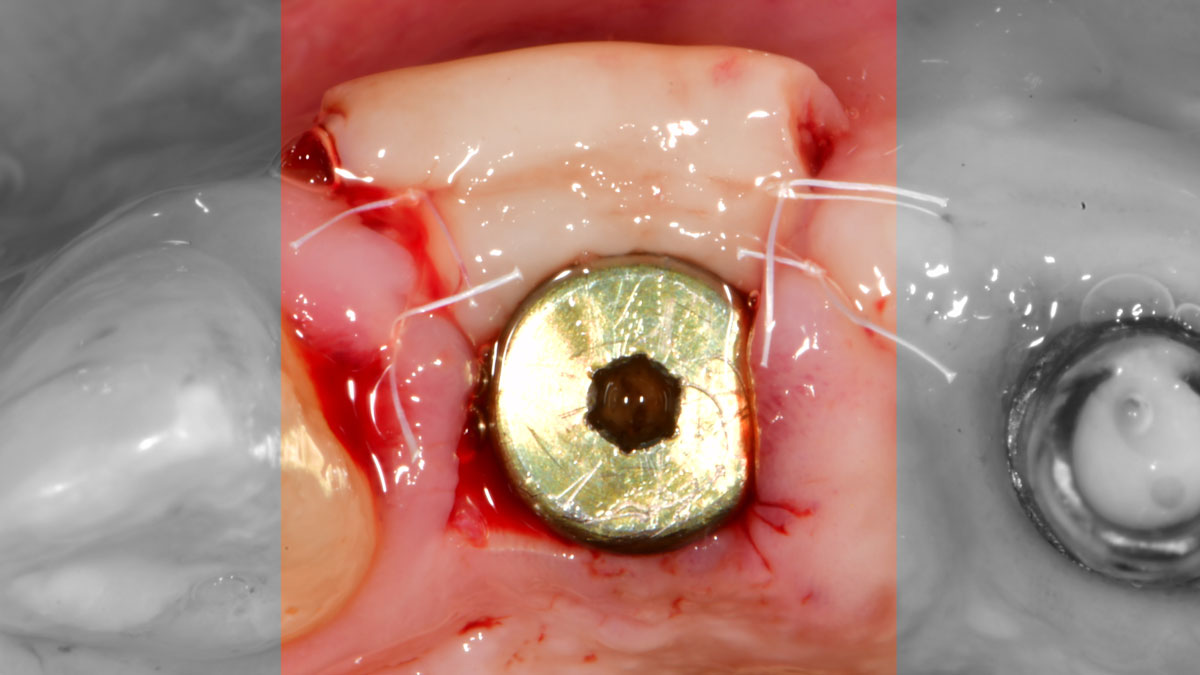
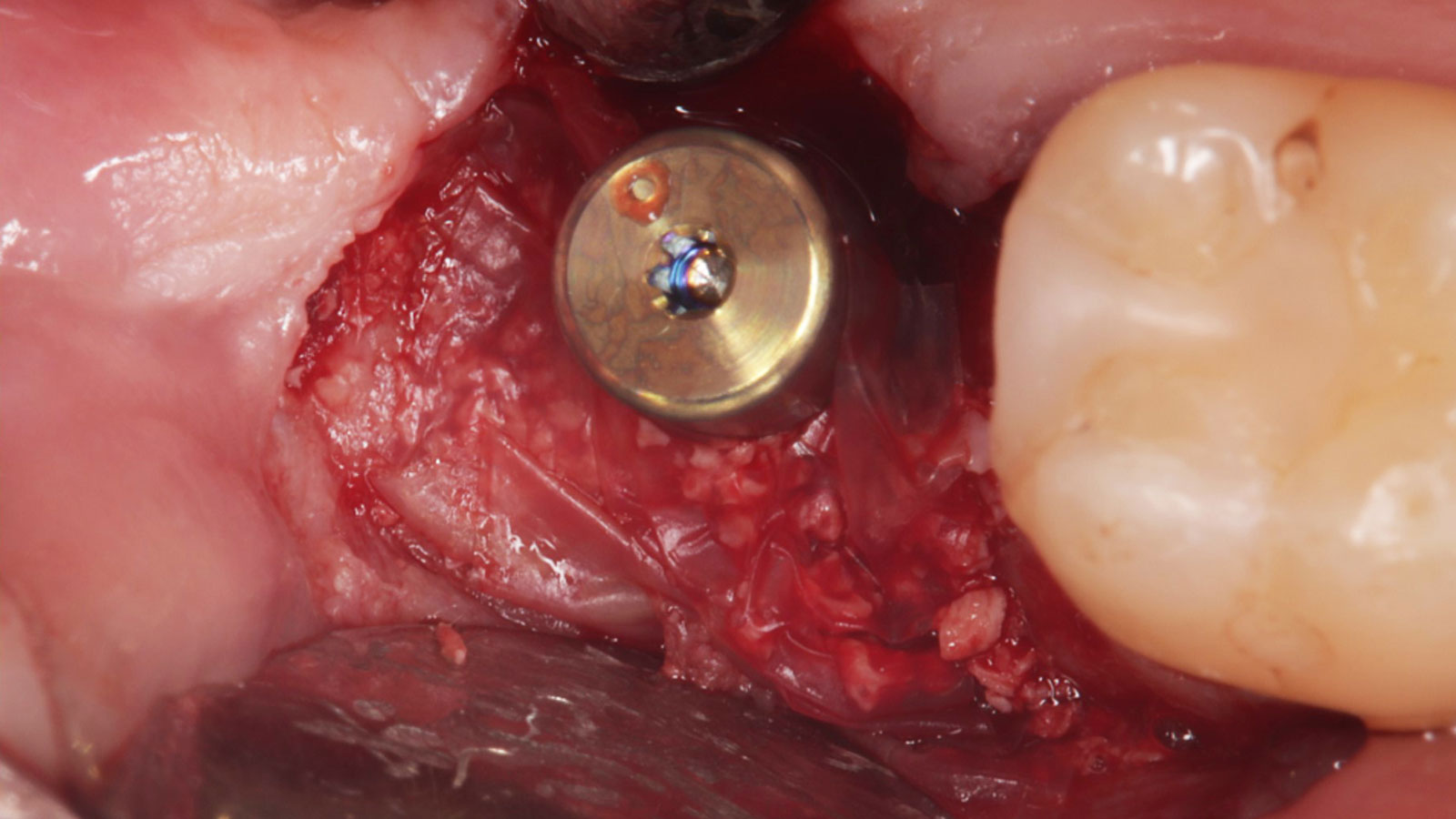
THE APPROACH
The treatment goals were to eliminate peri-implant infection, regenerate lost hard and soft tissues, and ensure long-term implant stability. A closed regenerative approach was utilized, including crown removal, thorough implant decontamination with Perioflow®, an airpolishing technology, application of the correct bone grafting materials (Geistlich Bio-Oss®, vallos® and GEM 21S®), enclosed healing, and fabrication of a new crown to facilitate hygiene.
“The implant presented with significant bone loss, deep probing depths, and bleeding on probing, placing it at risk of failure and requiring intervention to preserve function and longevity.”
— Andrea Ravidà, DDS, MS, PhD
THE OUTCOME
At the two-year follow-up, clinical and radiographic assessments showed disease resolution, complete bone gain, and stable peri-implant tissues. Probing depths were within healthy ranges, and no bleeding on probing was observed, confirming the long-term success of the treatment.

Andrea Ravidà, DDS, MS, PhD
Dr. Andrea Ravidà is the Director of the Graduate Periodontics Program in the department of Periodontics at the University of Pittsburgh. He conducts clinical research focusing on peri-implantitis, periodontitis and short implants. He has published more than 70 peer-reviewed articles and conference abstracts/presentations related to periodontics and implant therapy. He is section editor of the International Journal of Oral Implantology and the Journal of Translational Medicine.

Anu Viswanathan DDS, MDS
Dr. Anu Viswanathan is a Diplomate of the American Board of Periodontology and Implant Dentistry. She earned her Doctor of Dental Surgery degree from the University of Colorado School of Dental Medicine in 2019. Dr. Viswanathan completed a Certificate in Periodontics and earned a Master of Dental Science at the University of Pittsburgh School of Dental Medicine. She also obtained a Certificate in IV Sedation. Dr. Viswanathan is currently in private practice in Shoreline, Connecticut.

BIOBRIEF
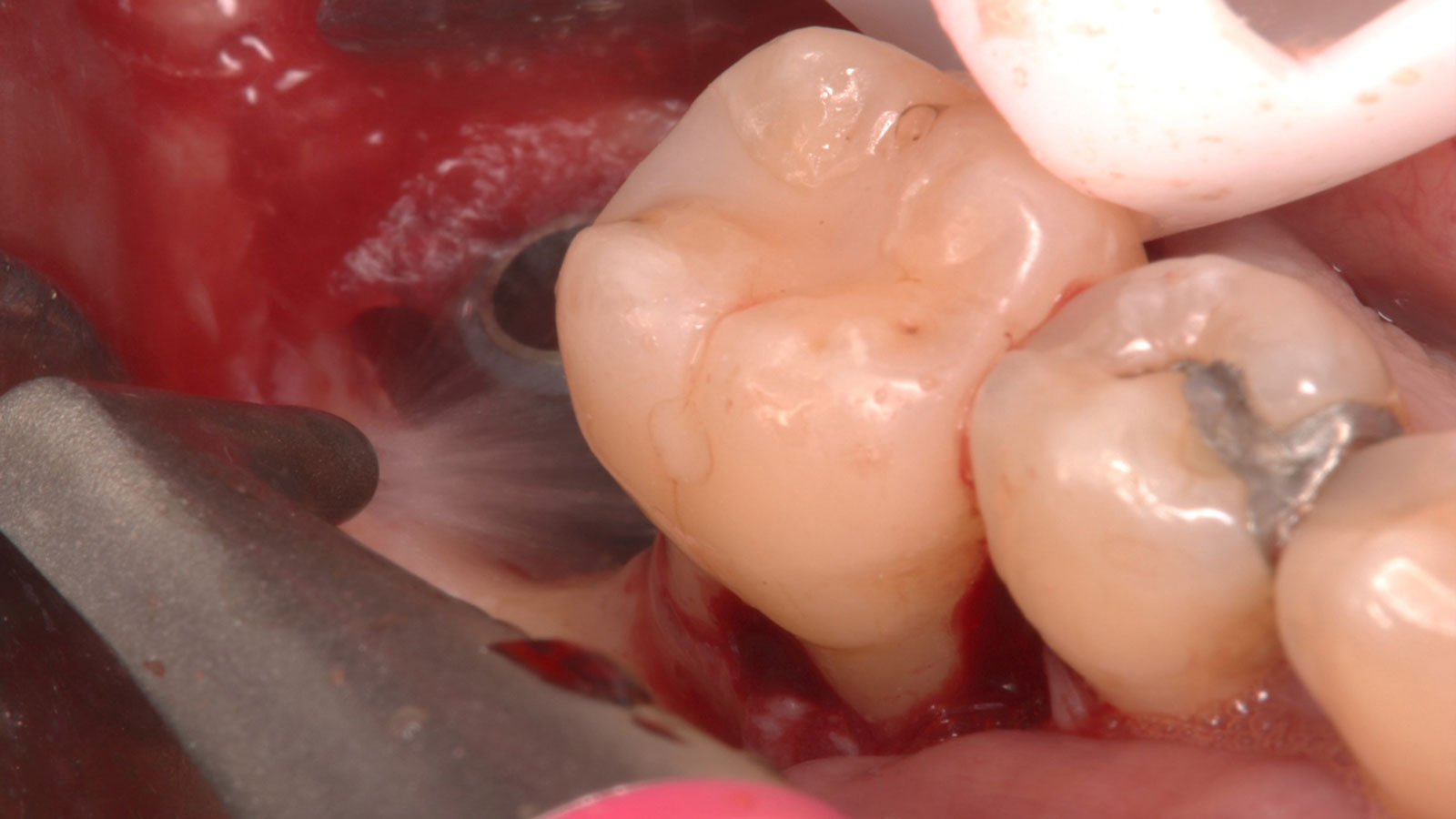
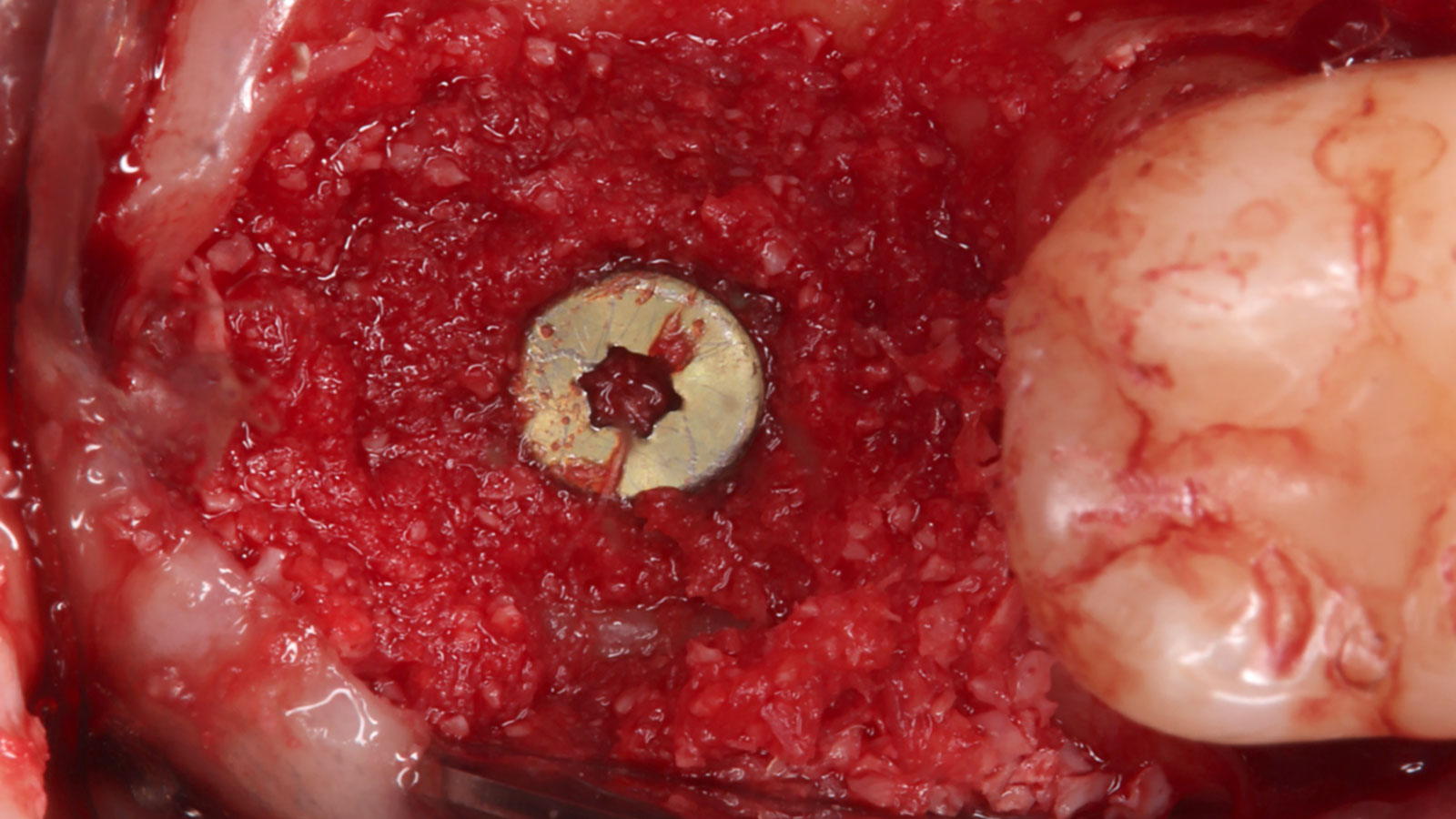
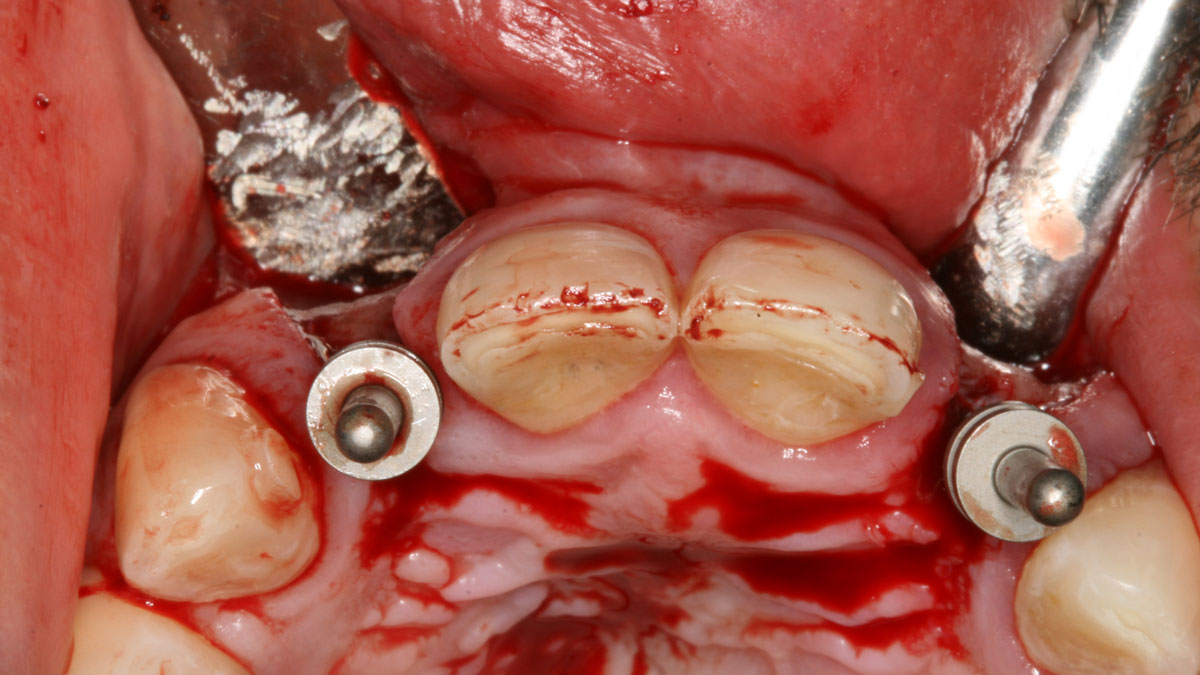
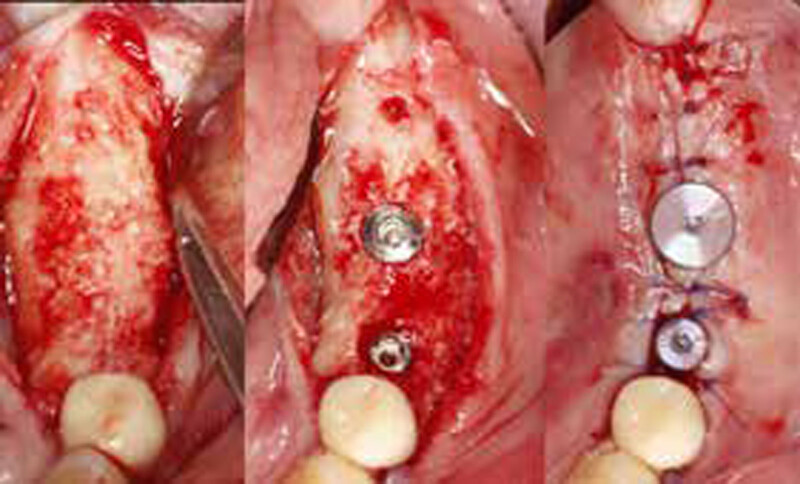
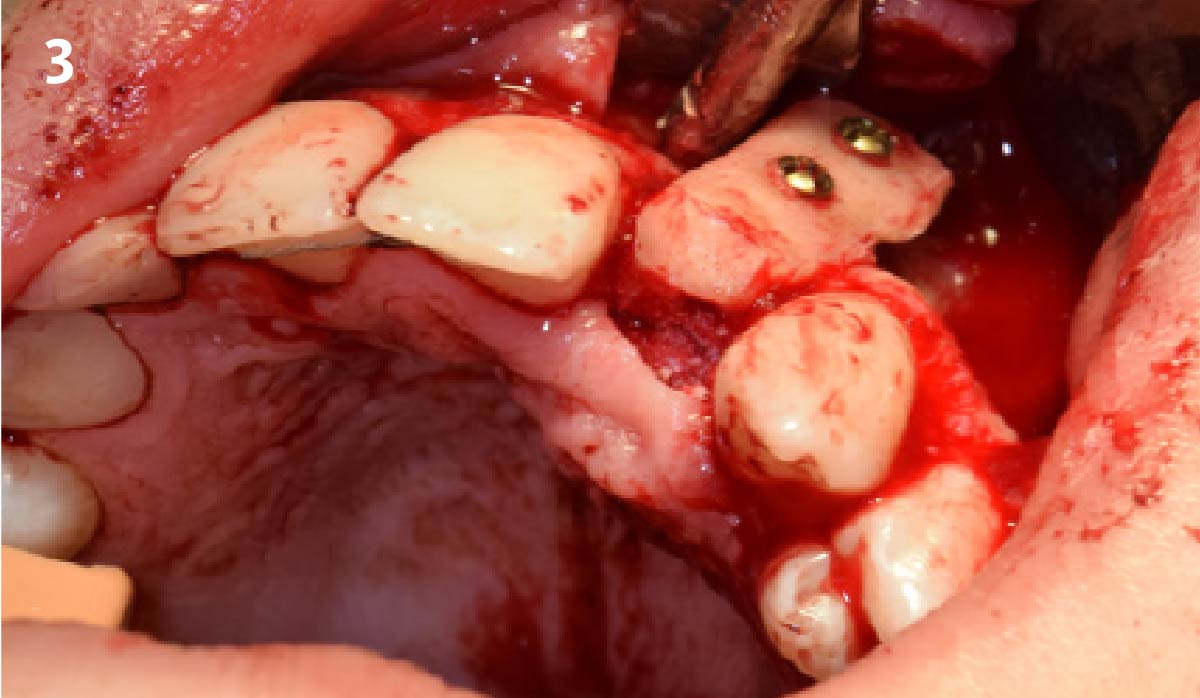
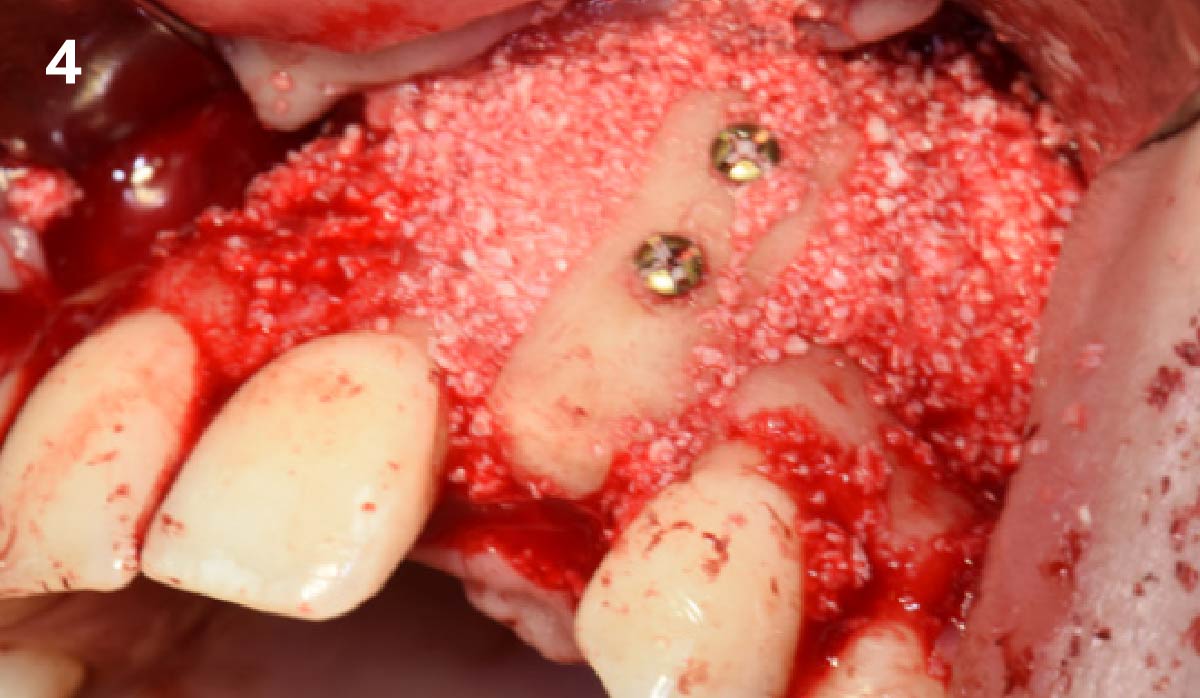
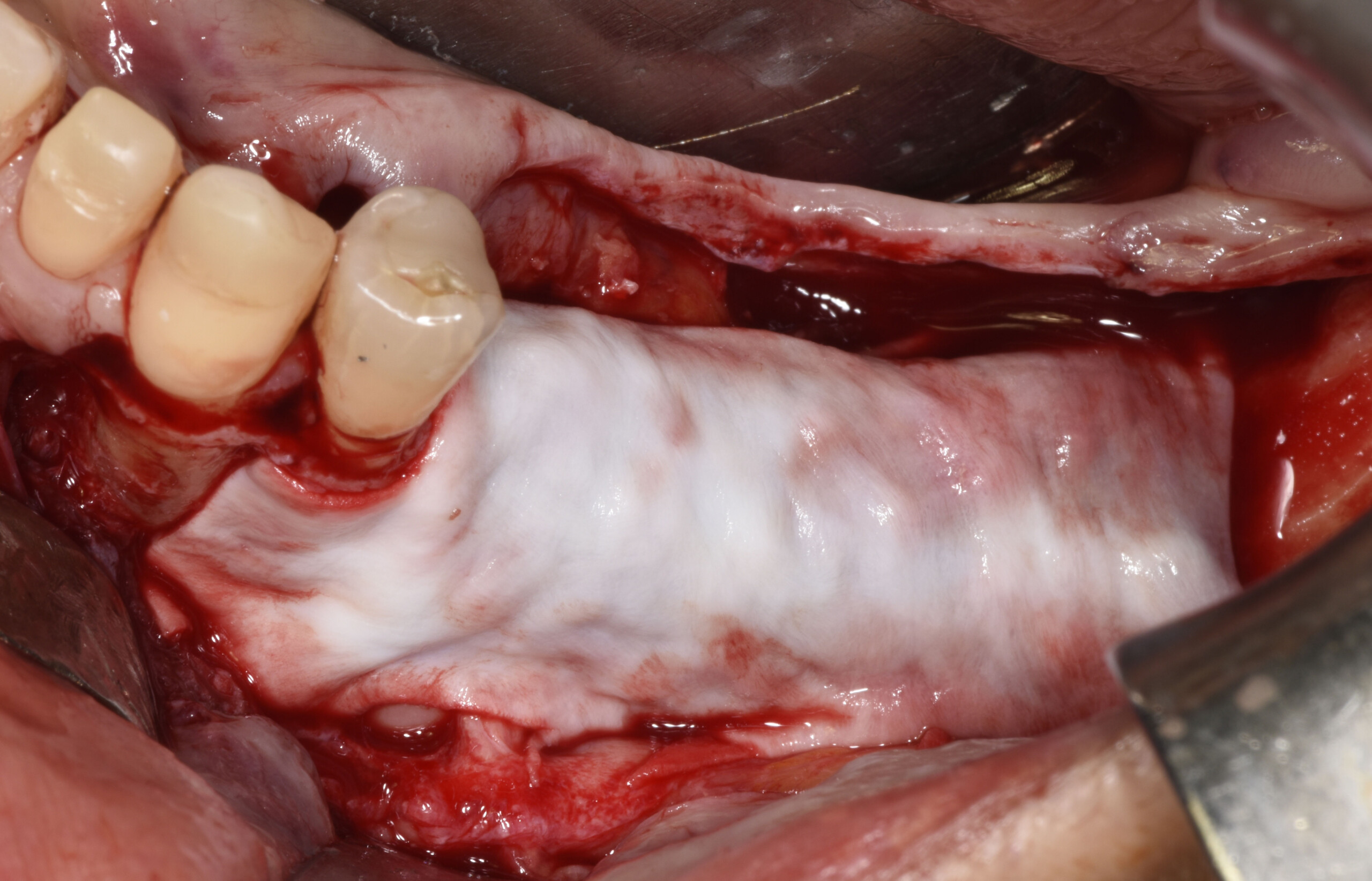
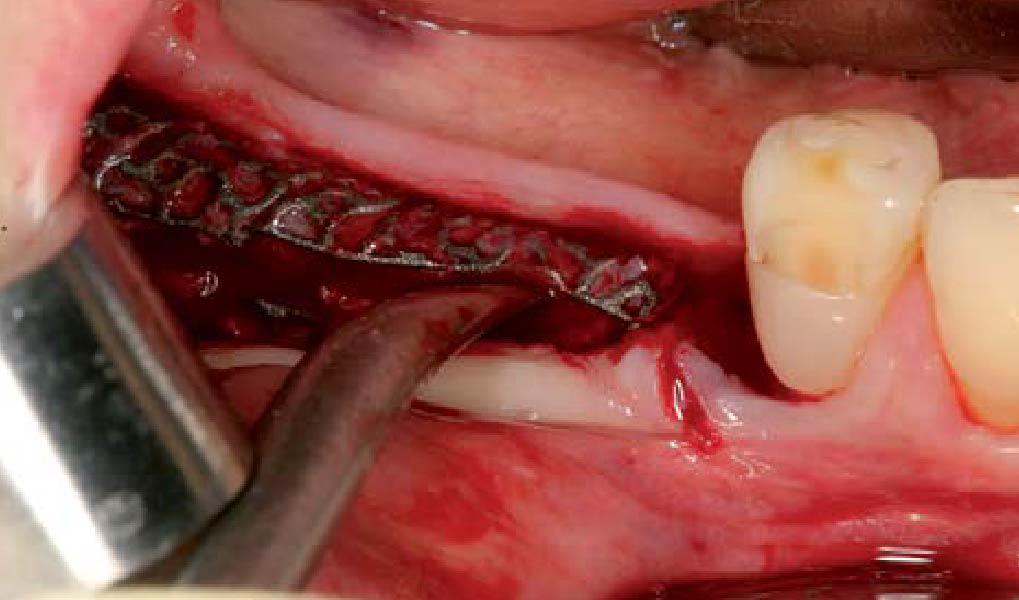
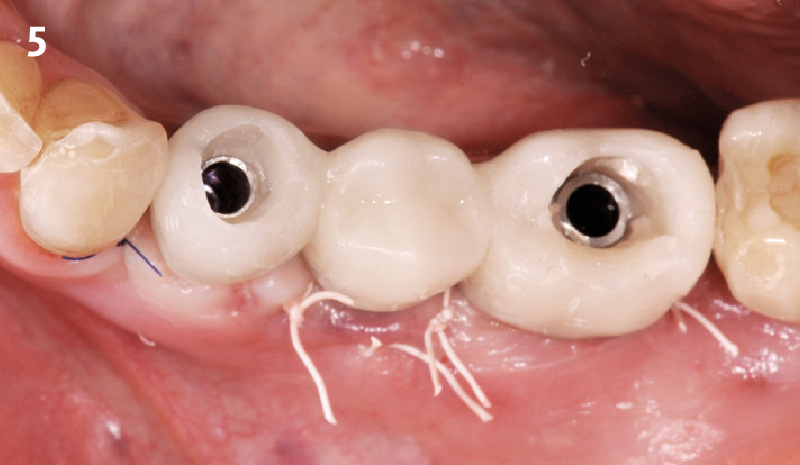
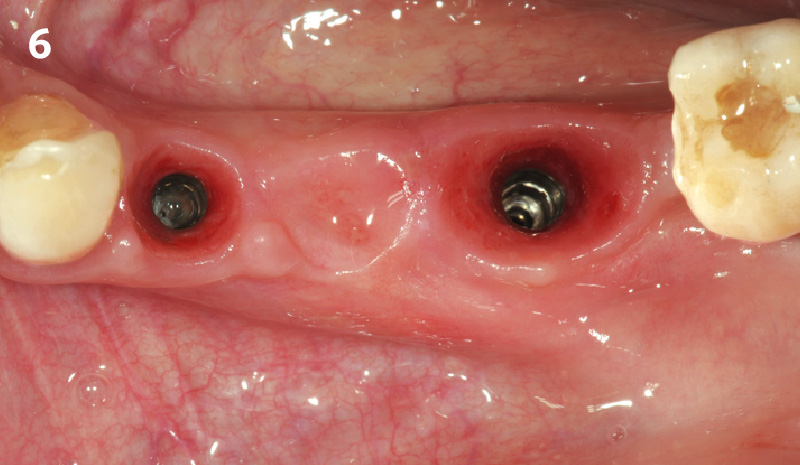
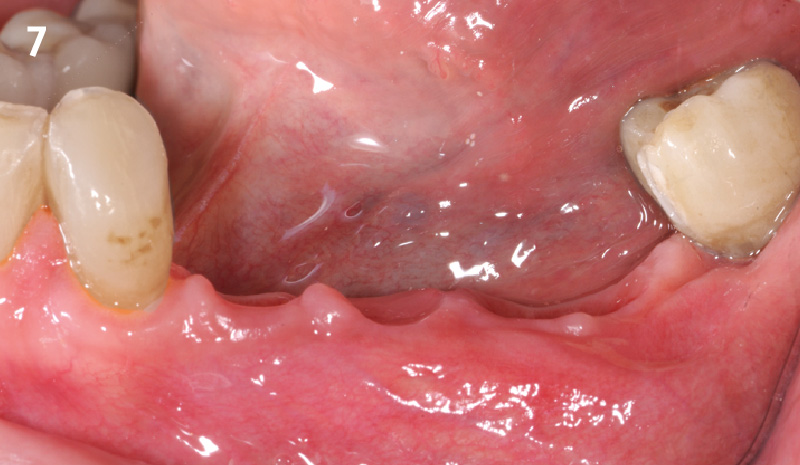
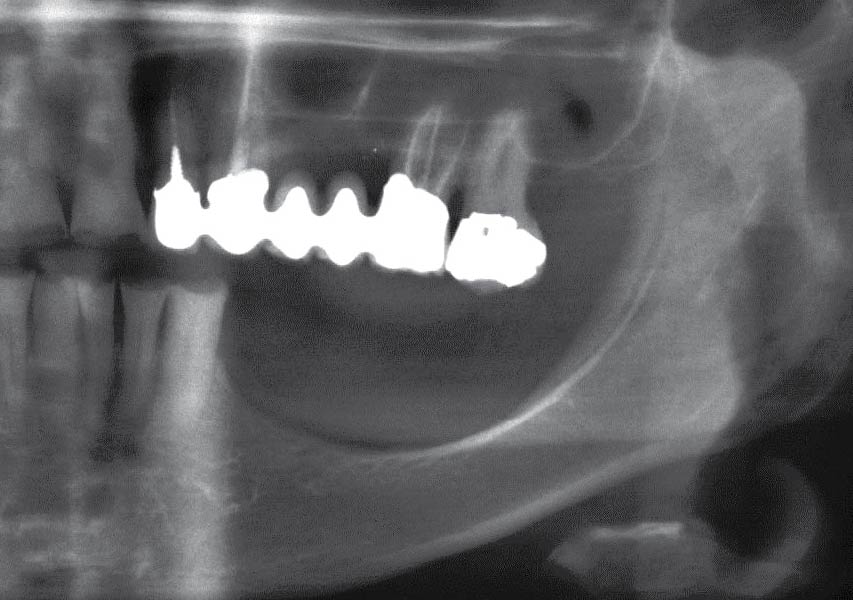
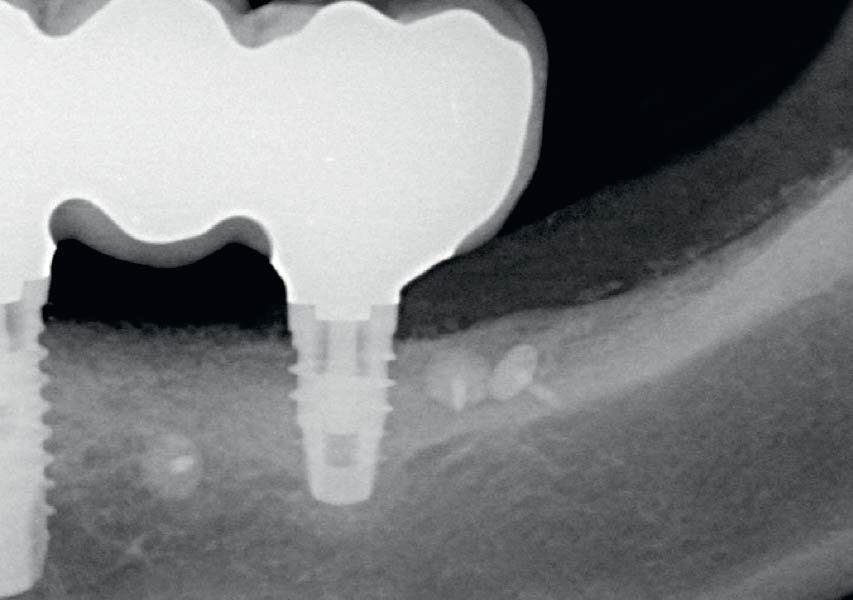
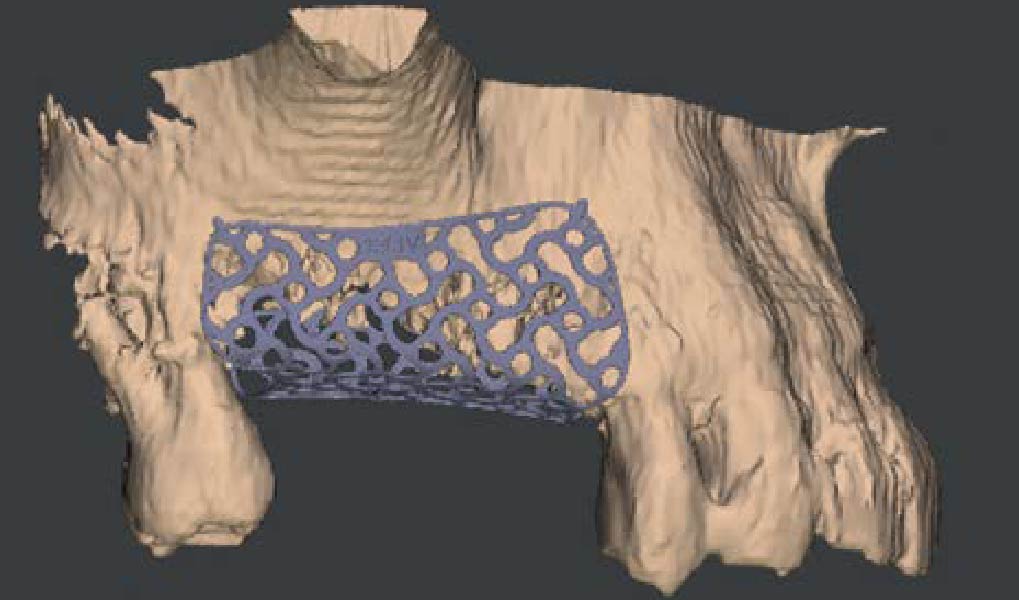
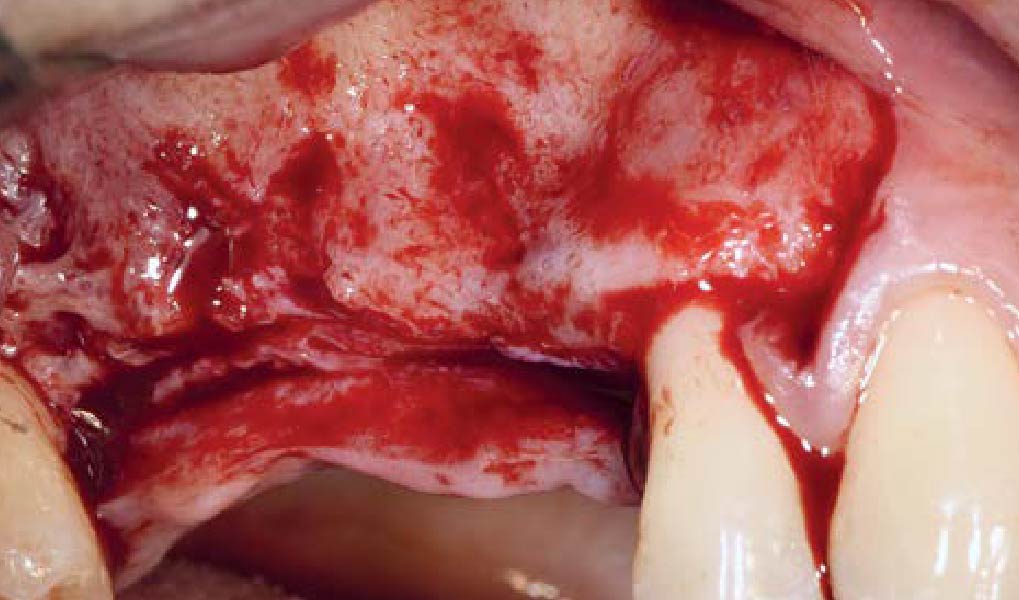
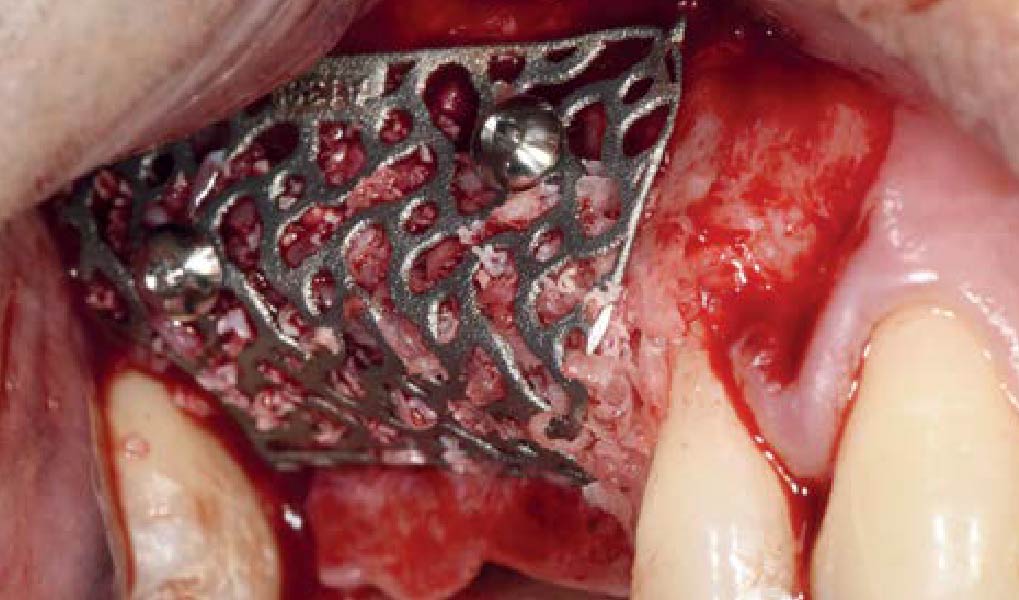
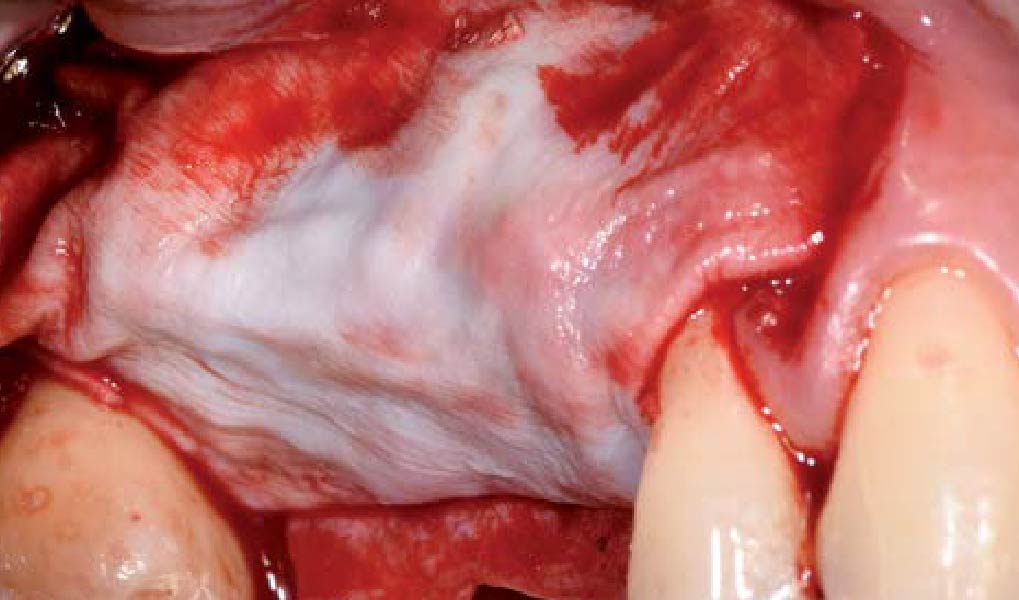
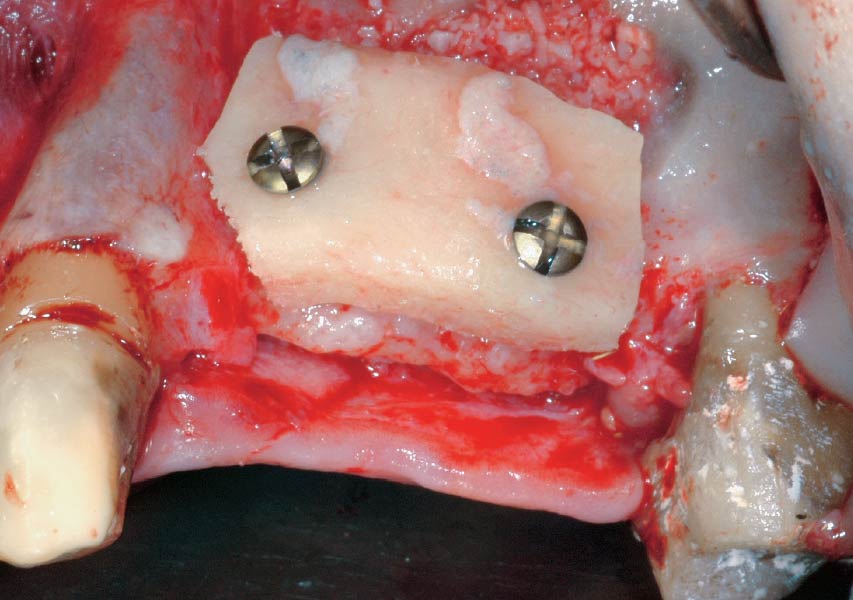
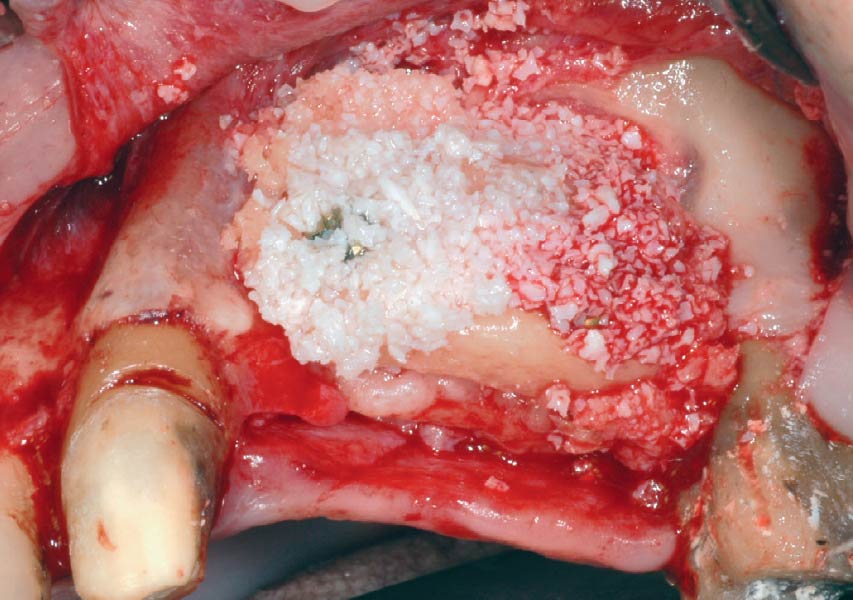
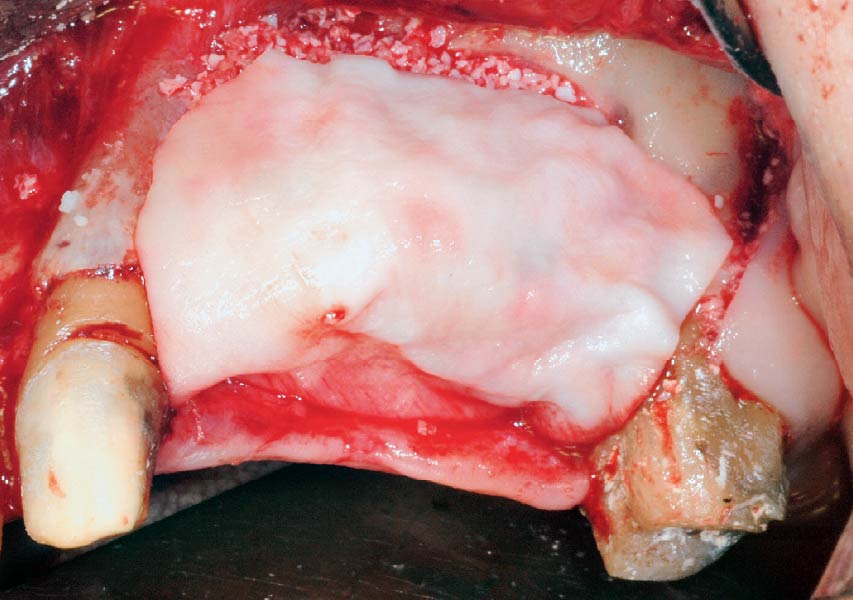
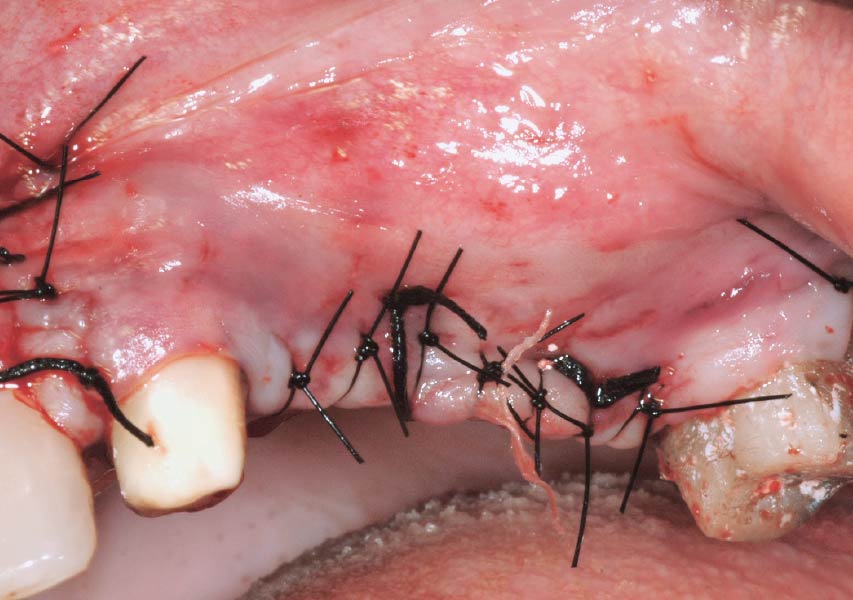
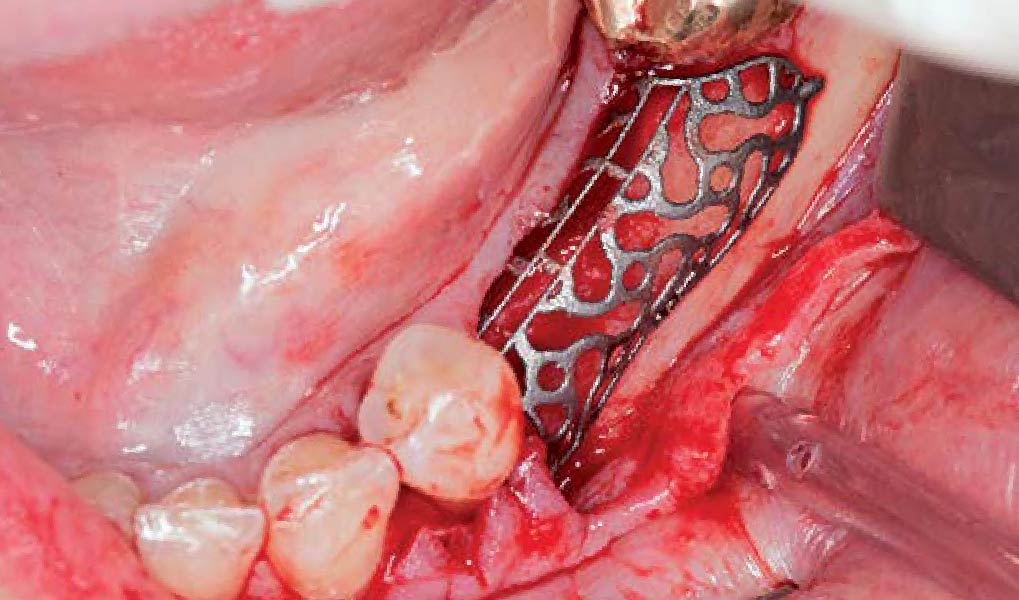
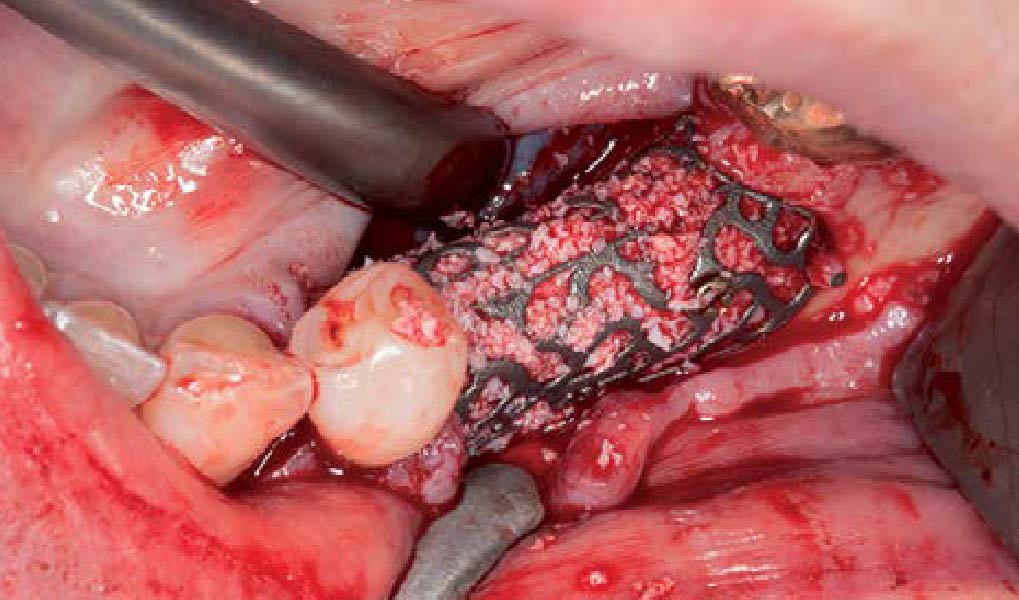
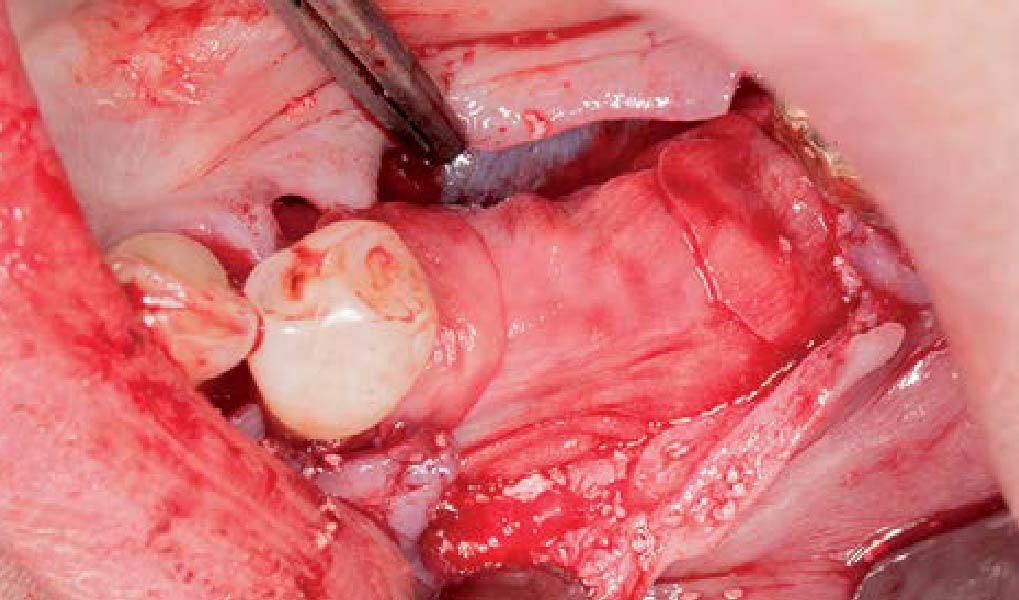
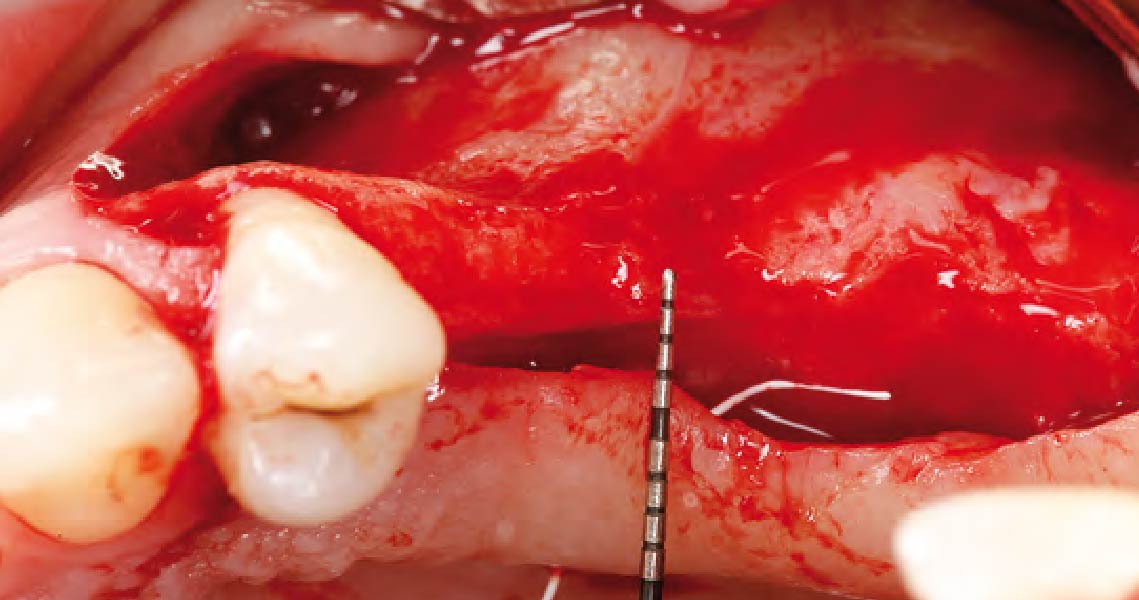
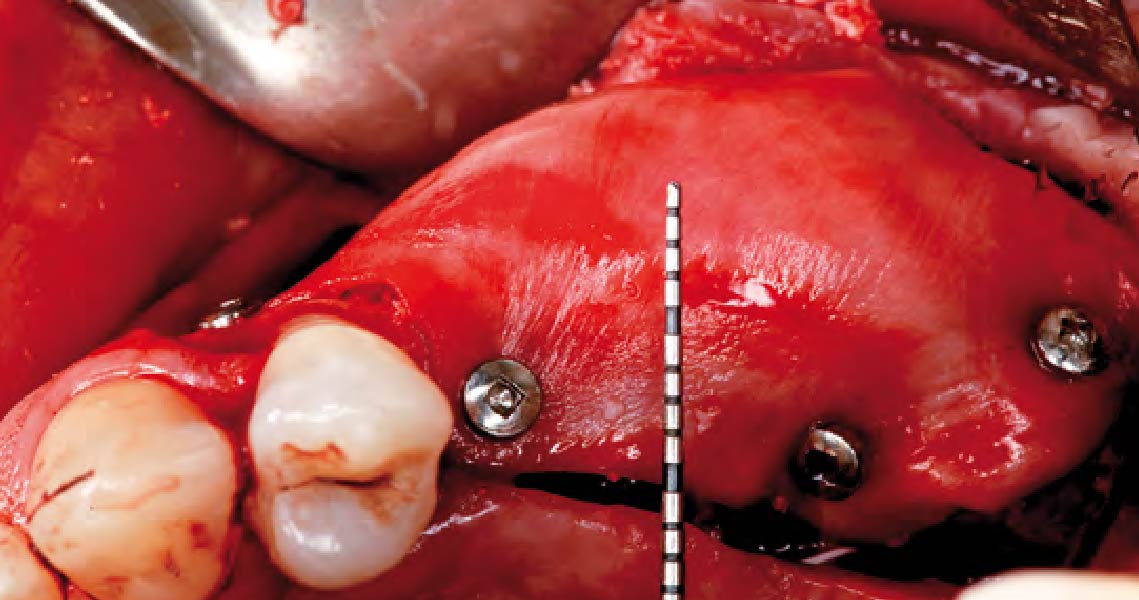
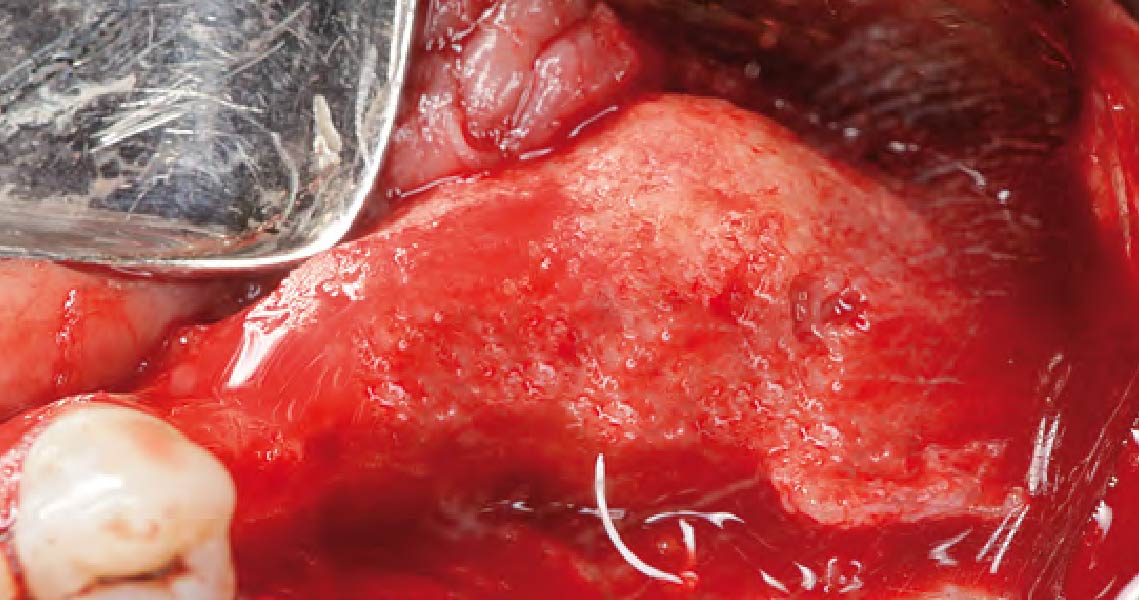
Mandibular Ridge Augmentation Using Customized Titanium Mesh

THE SITUATION
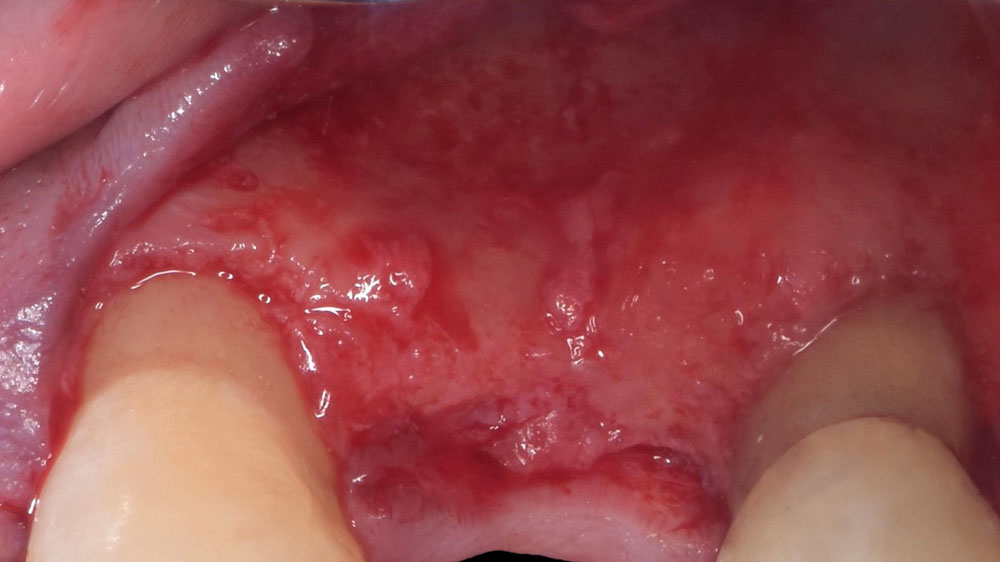
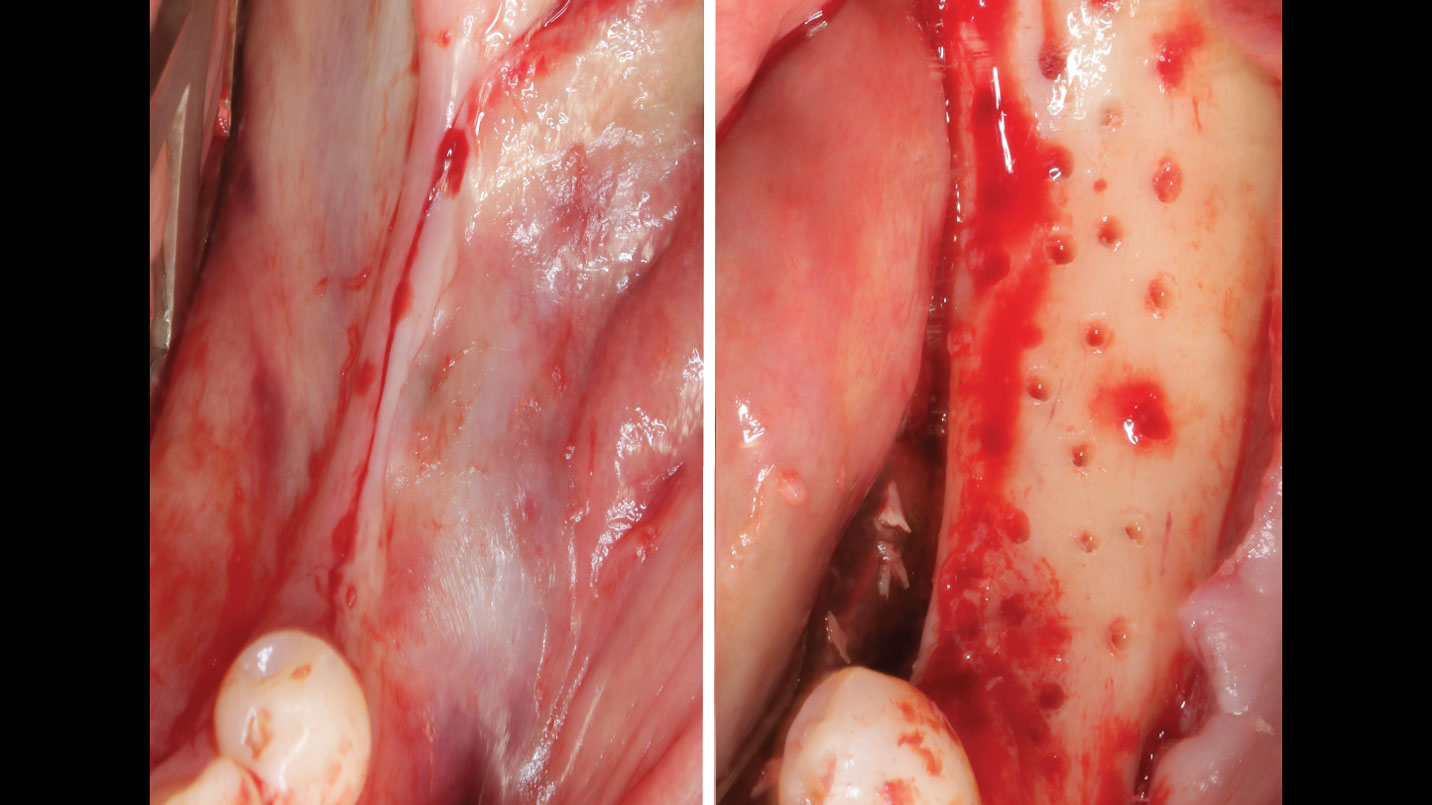
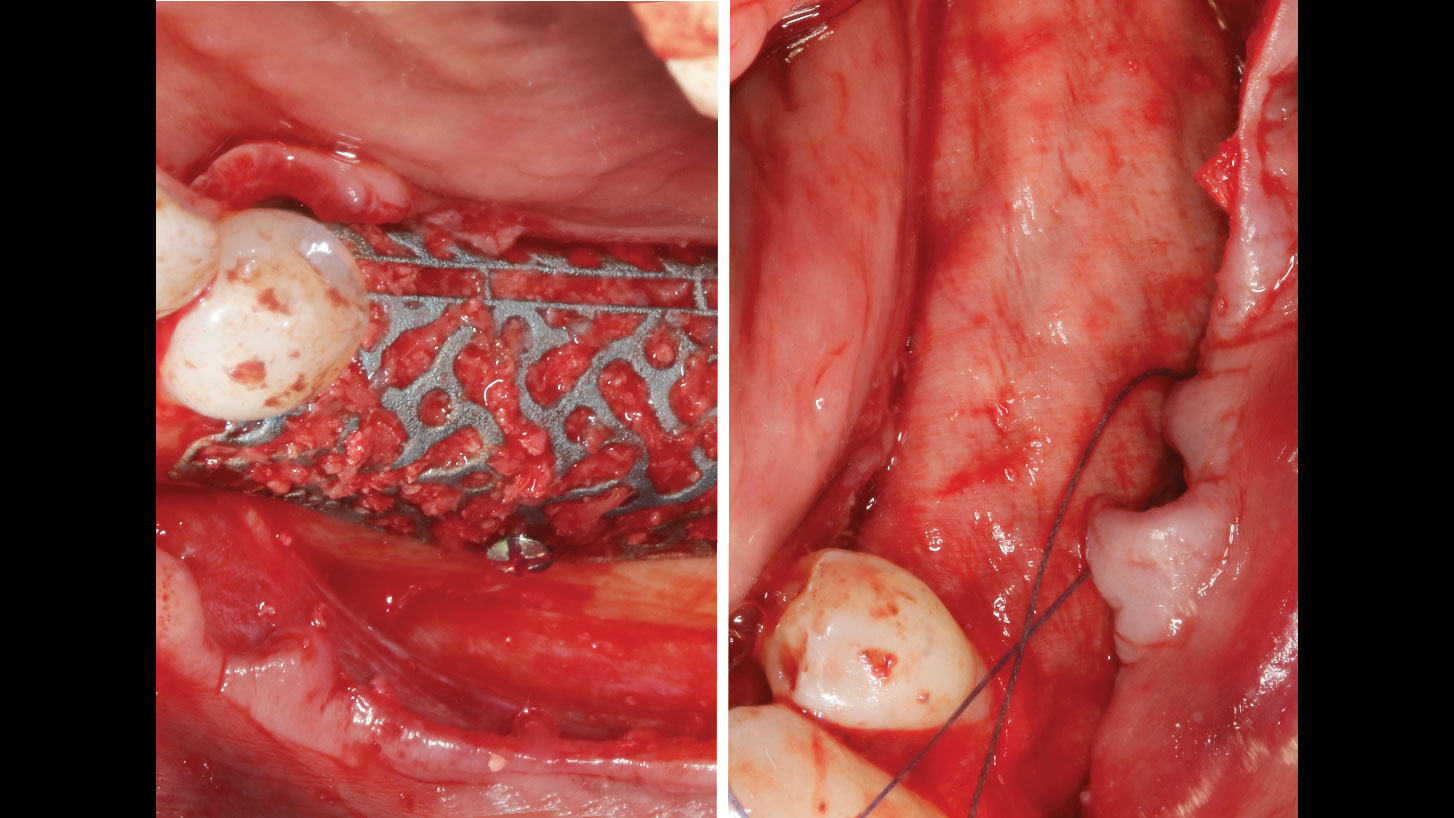
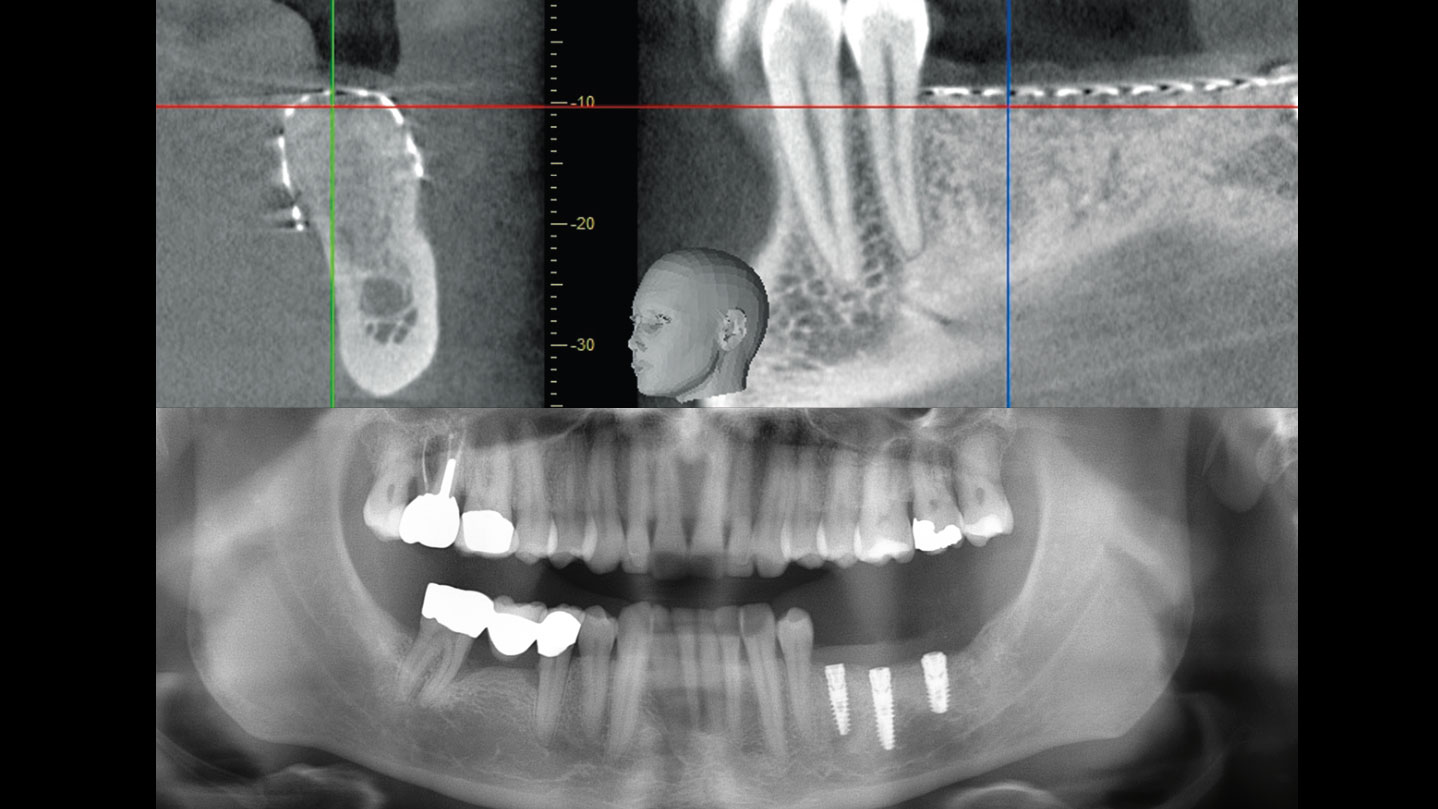
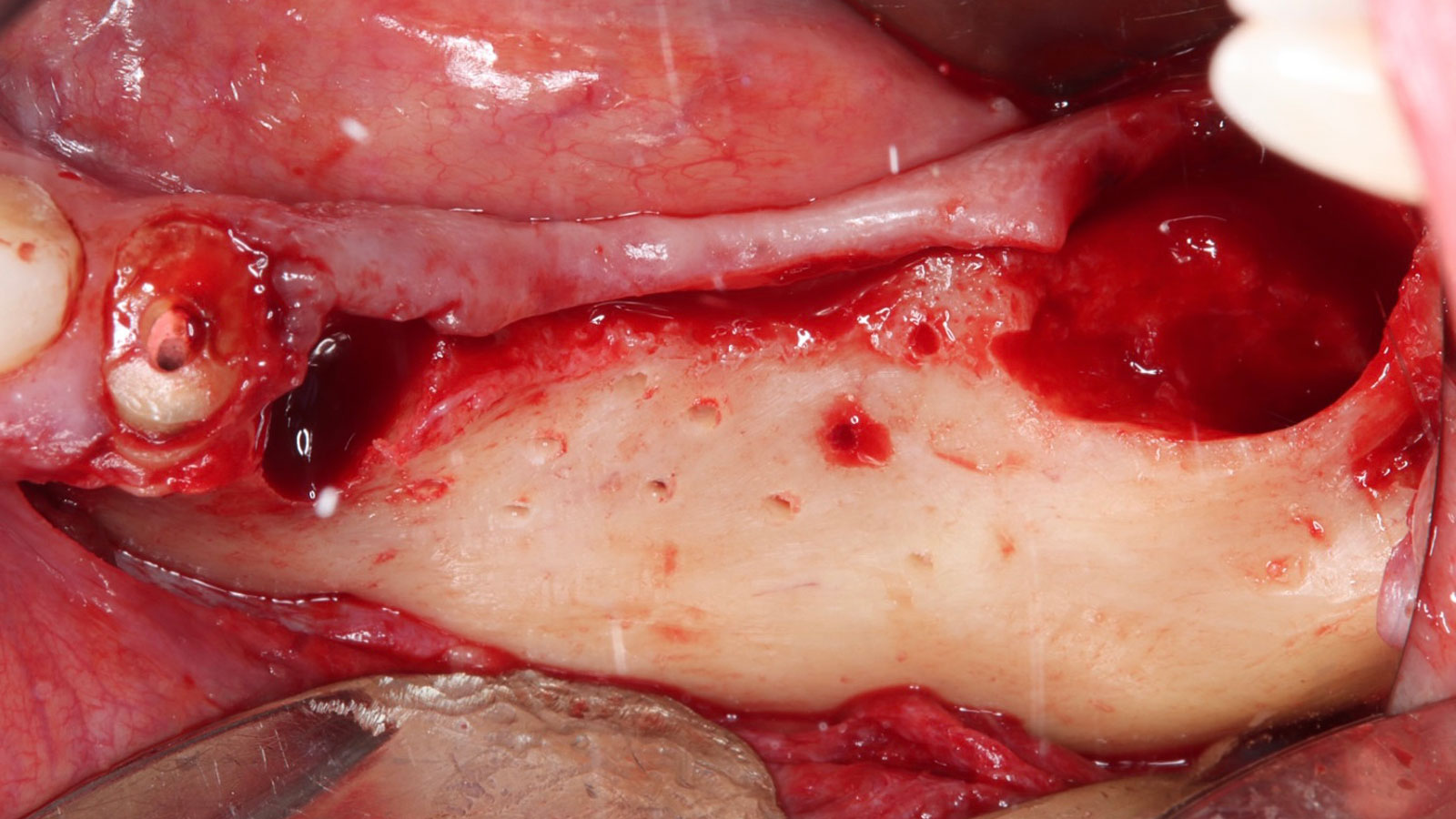
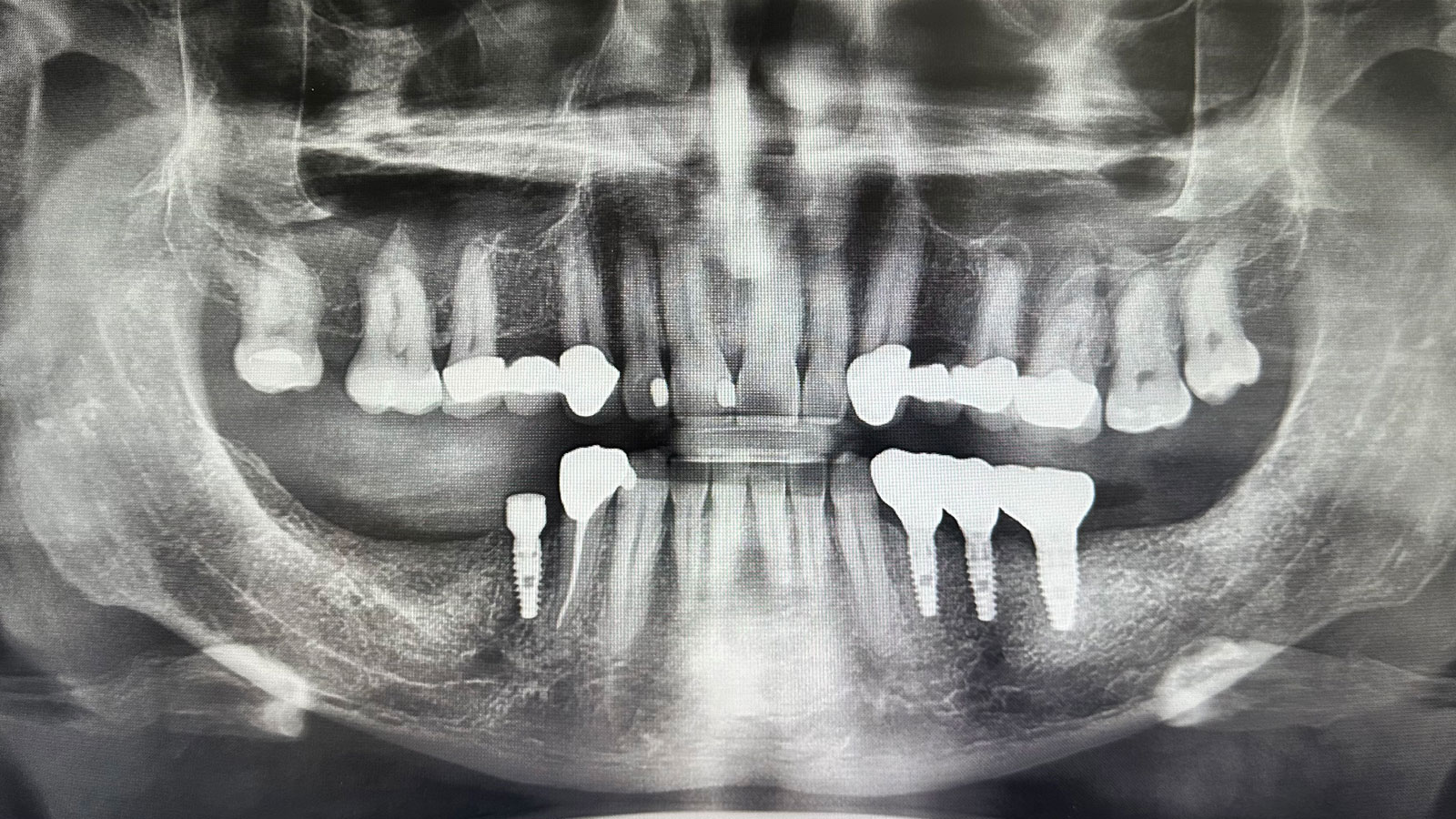
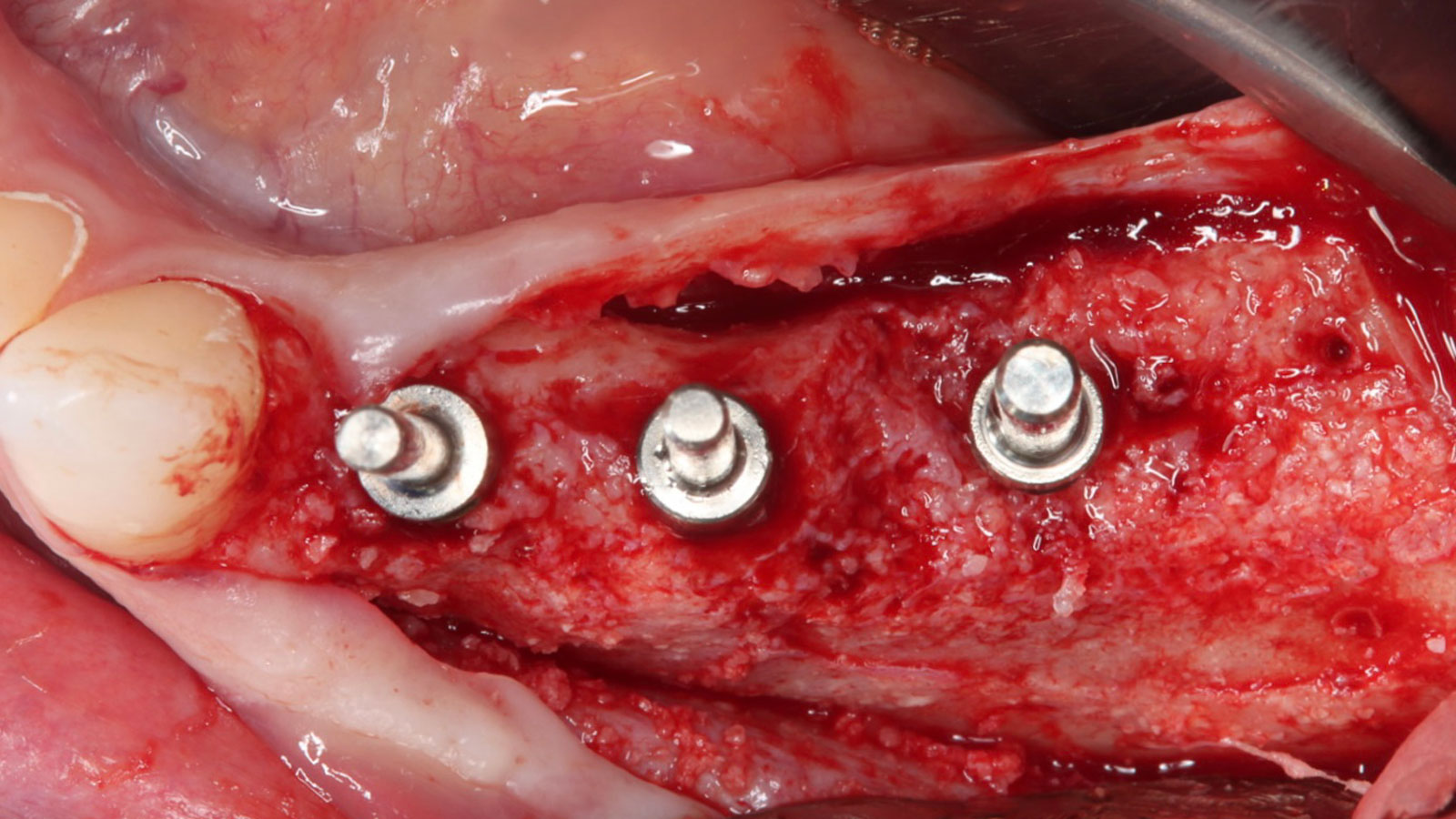
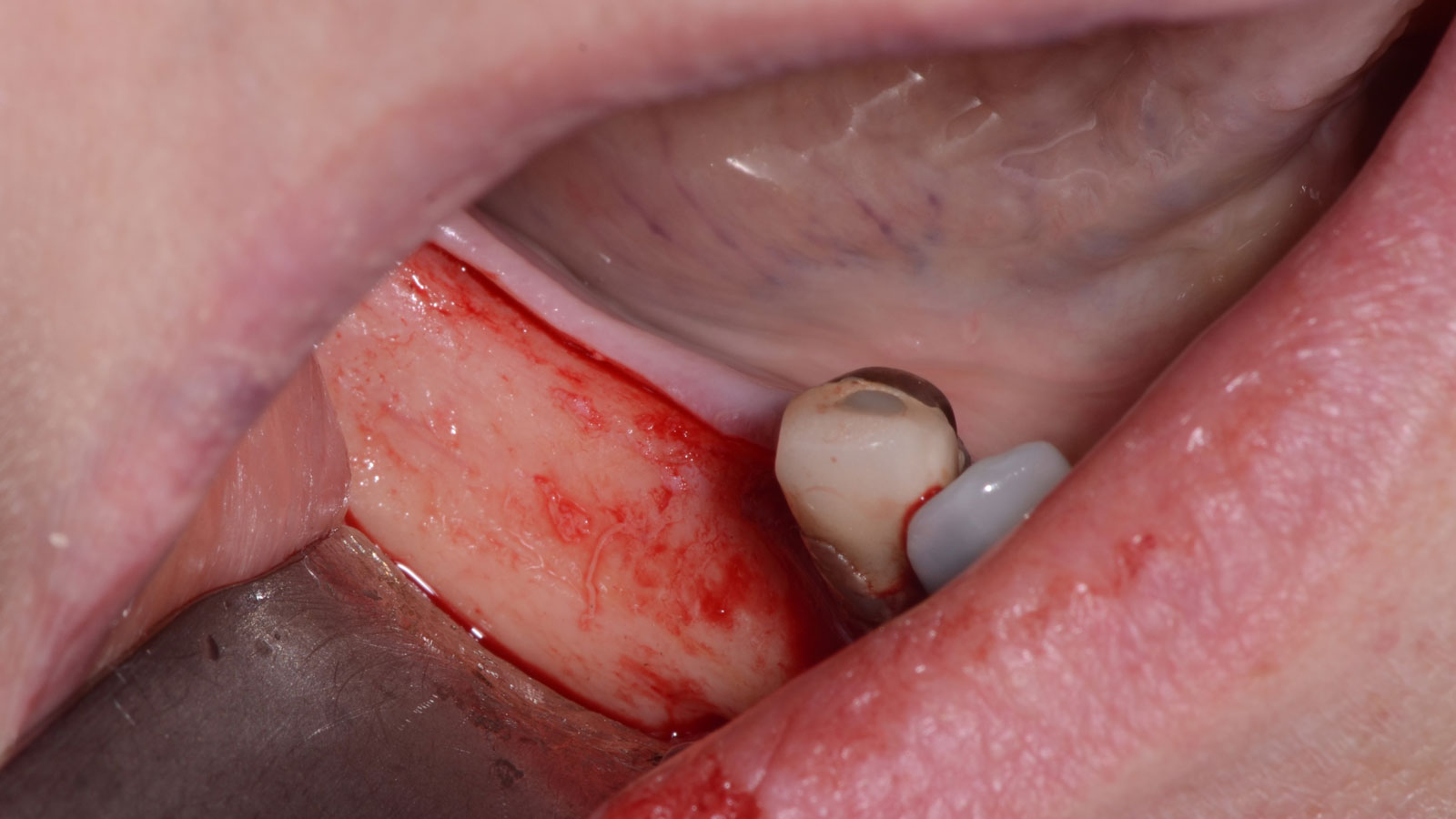
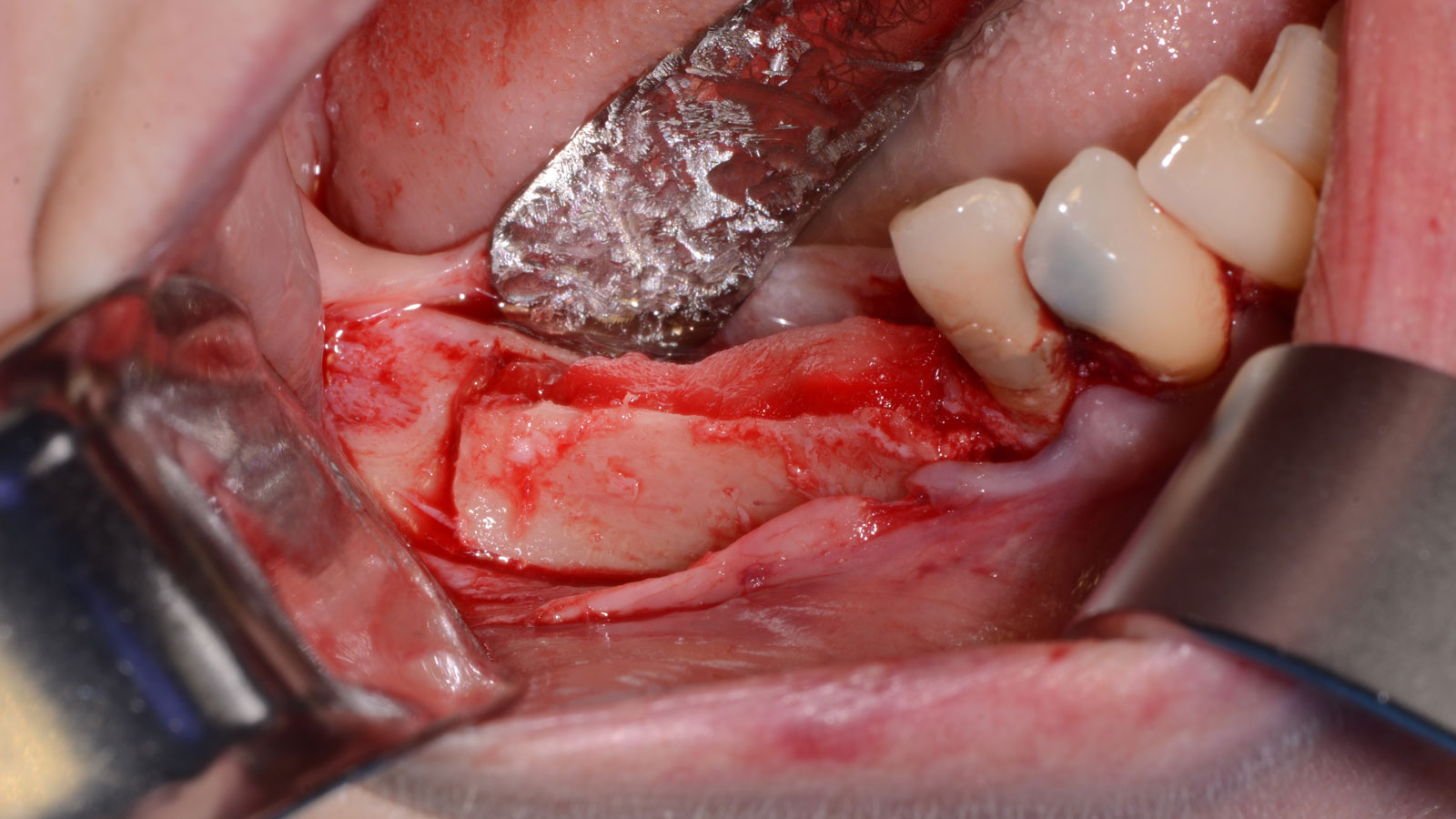
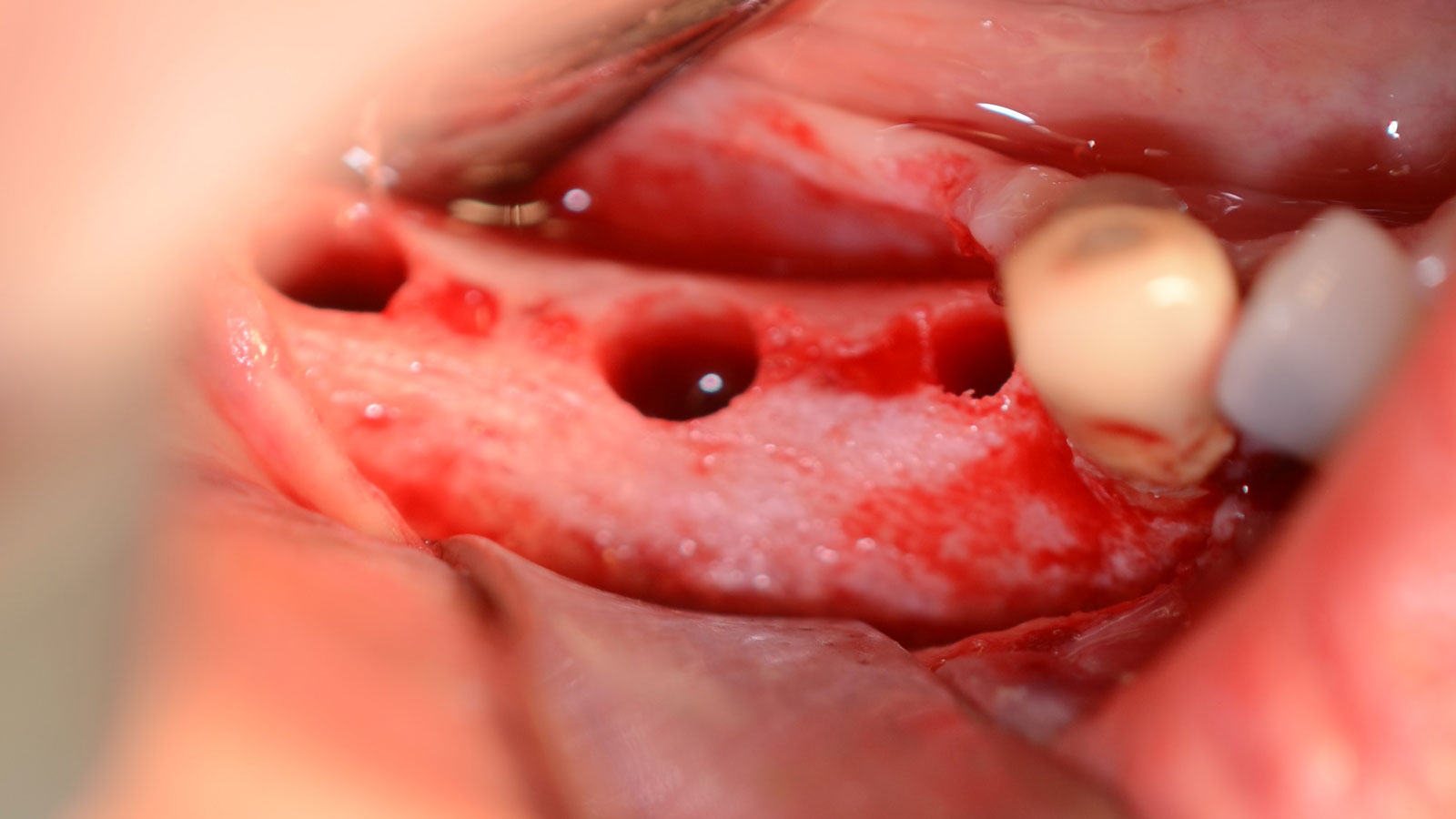
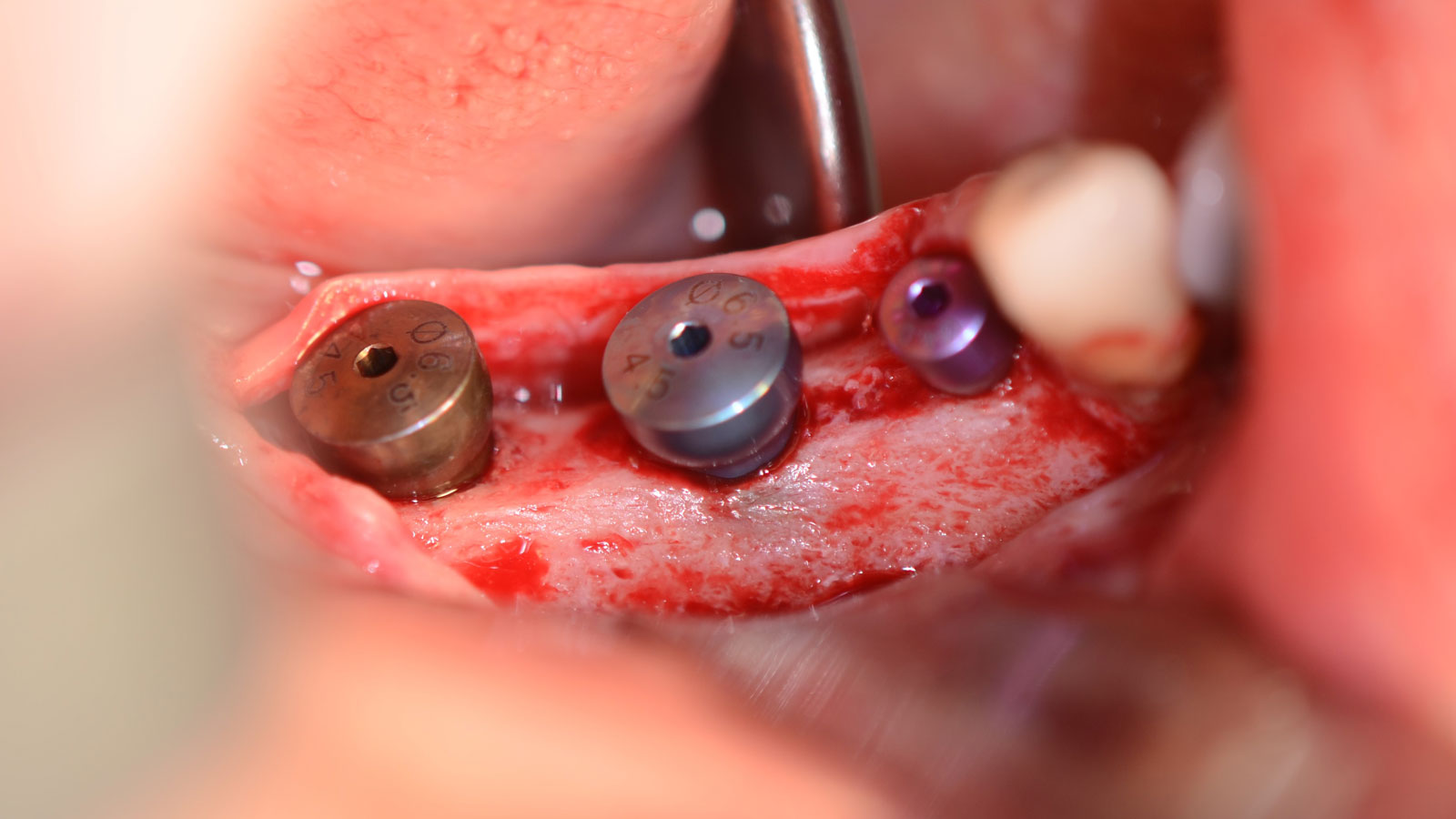
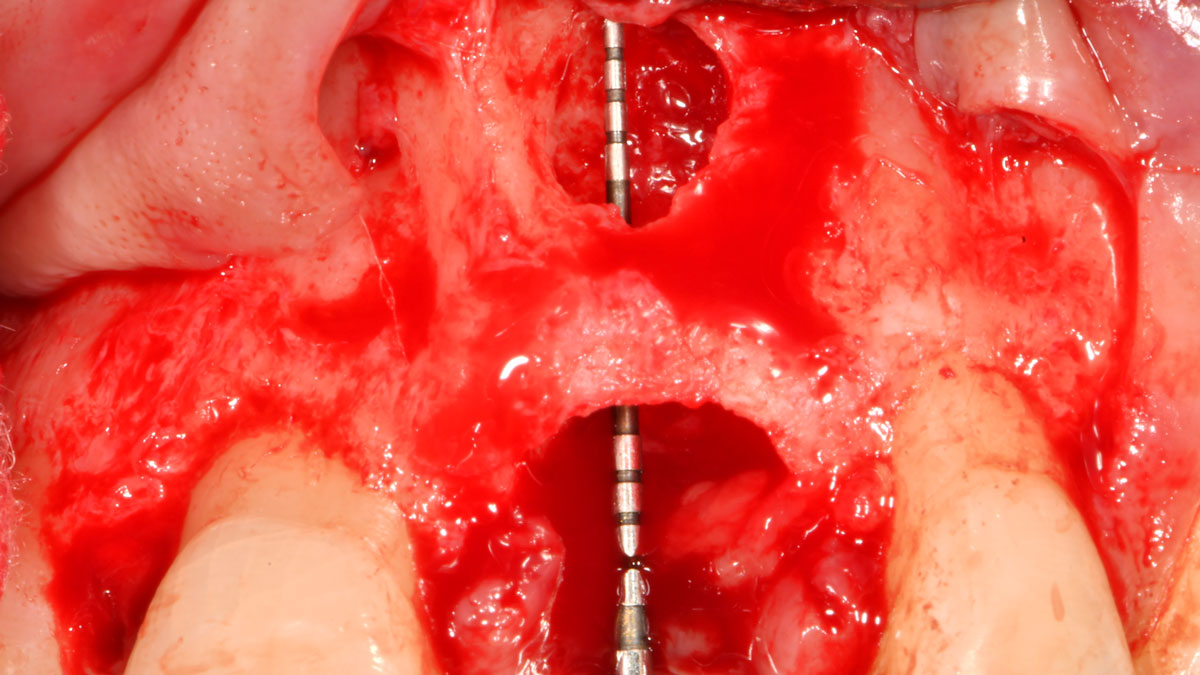
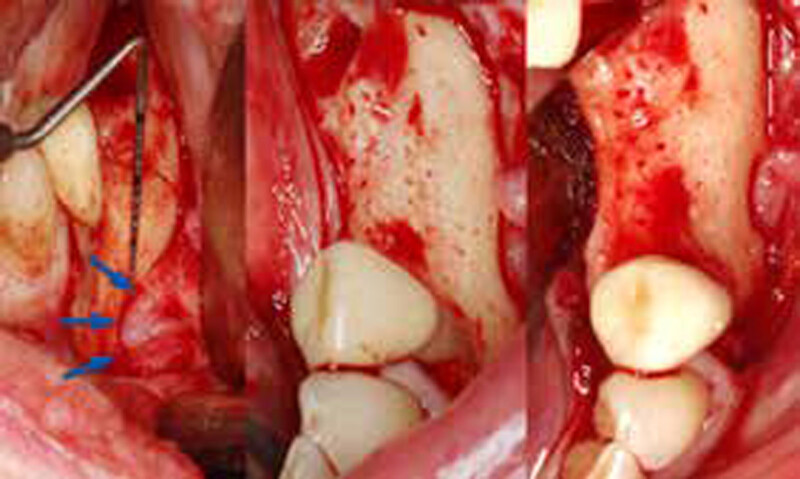
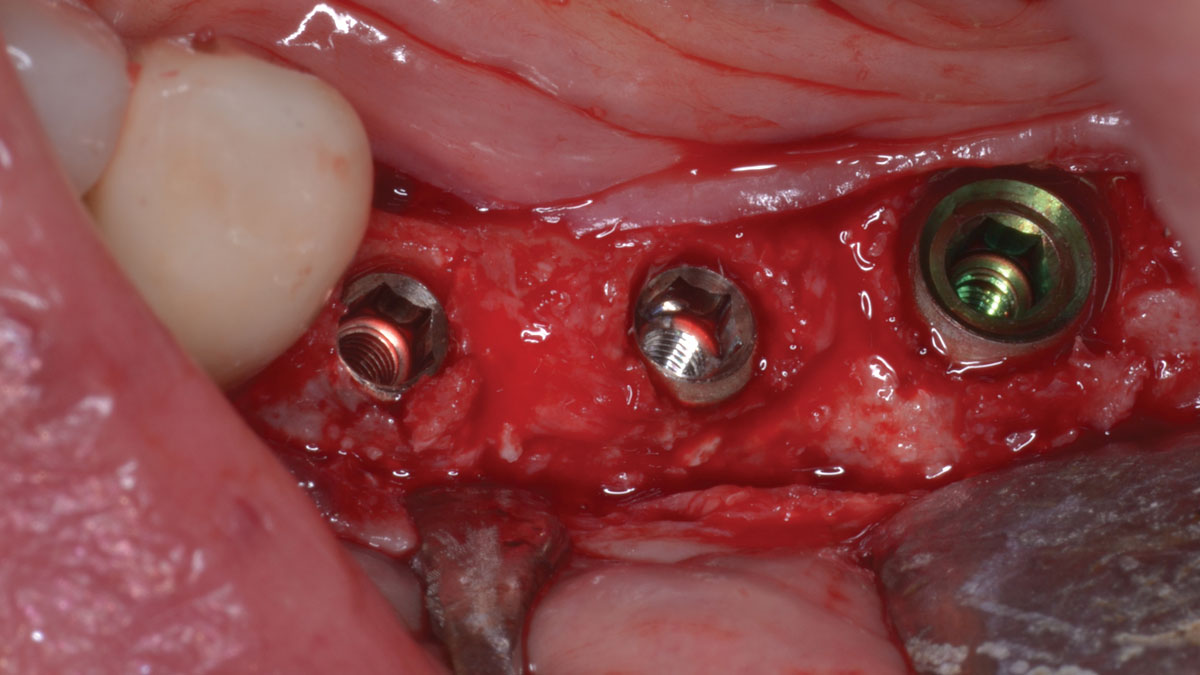
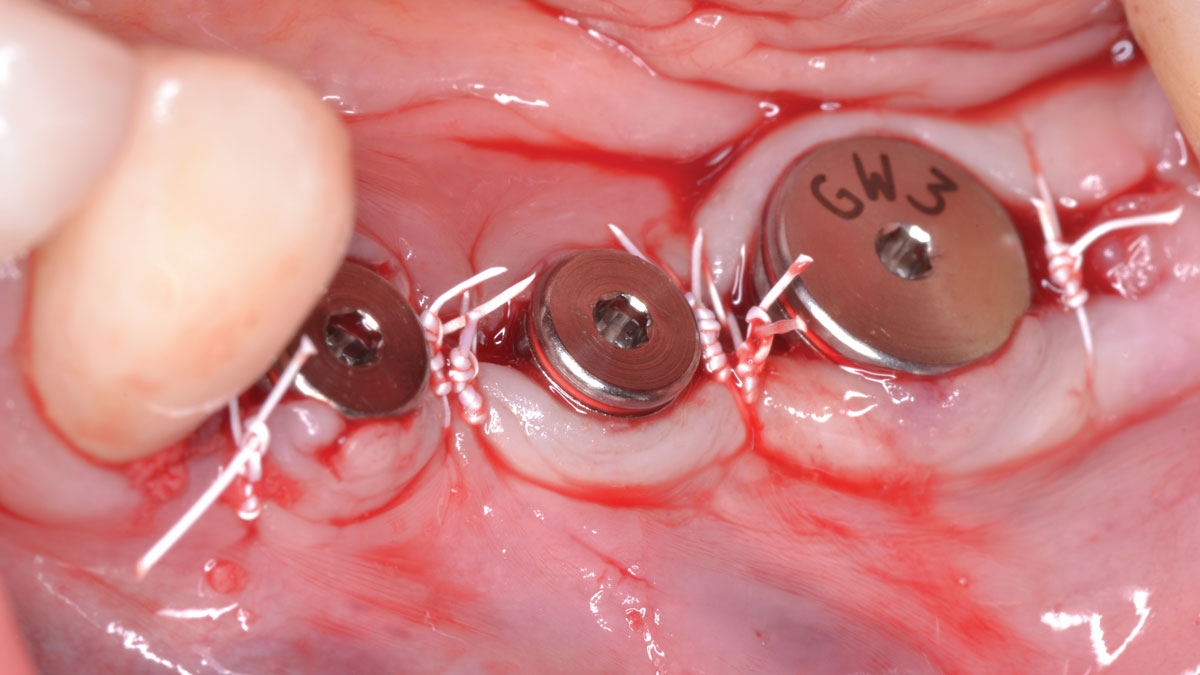
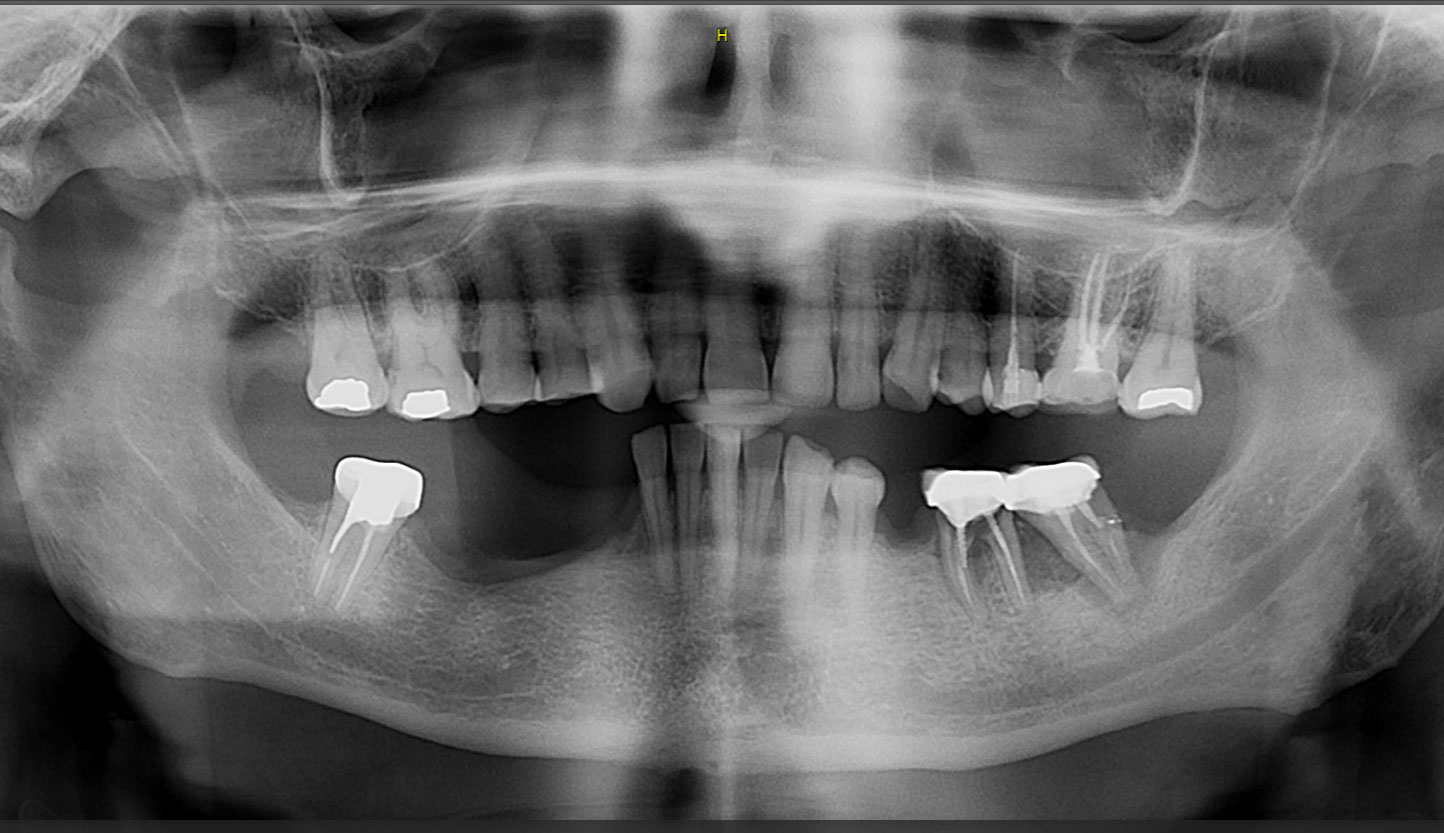
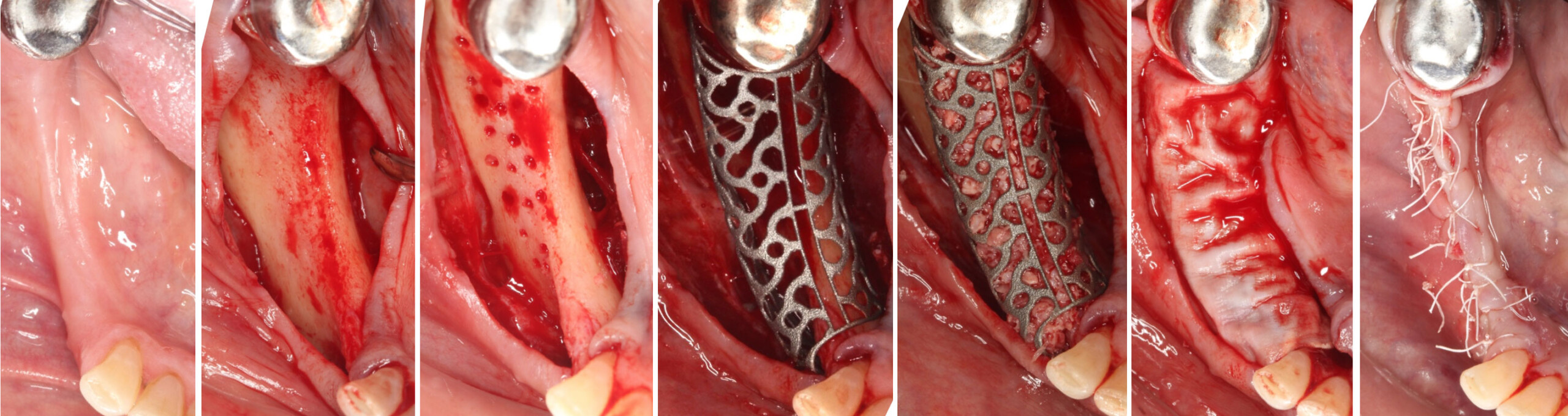
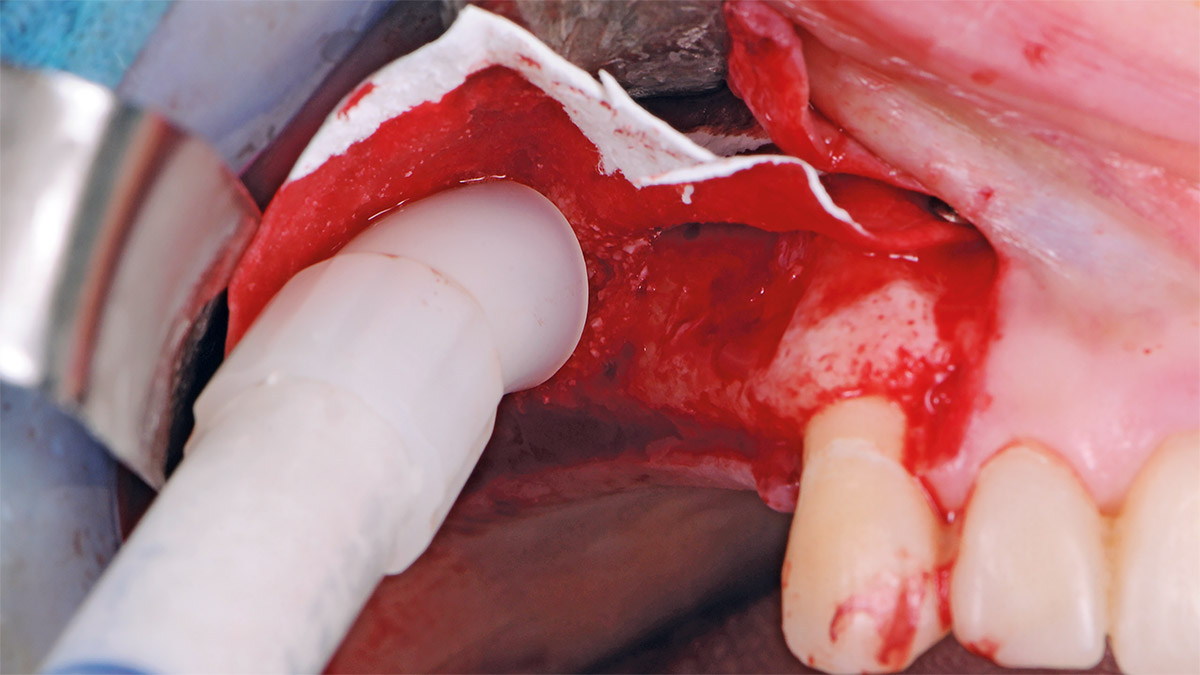
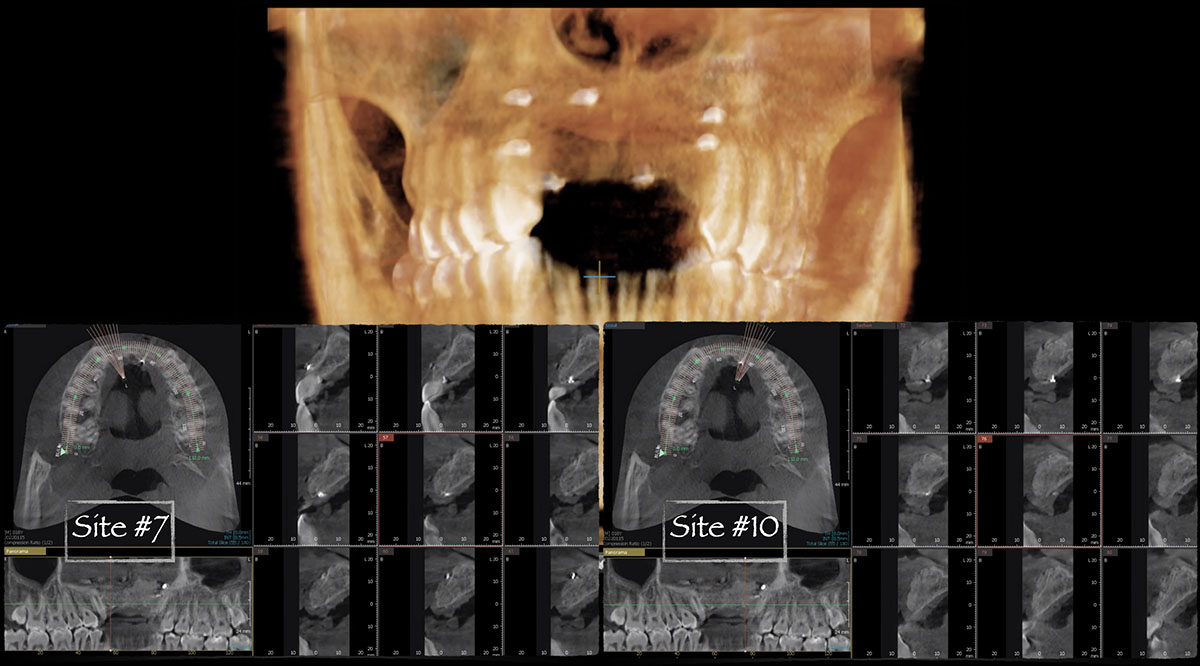
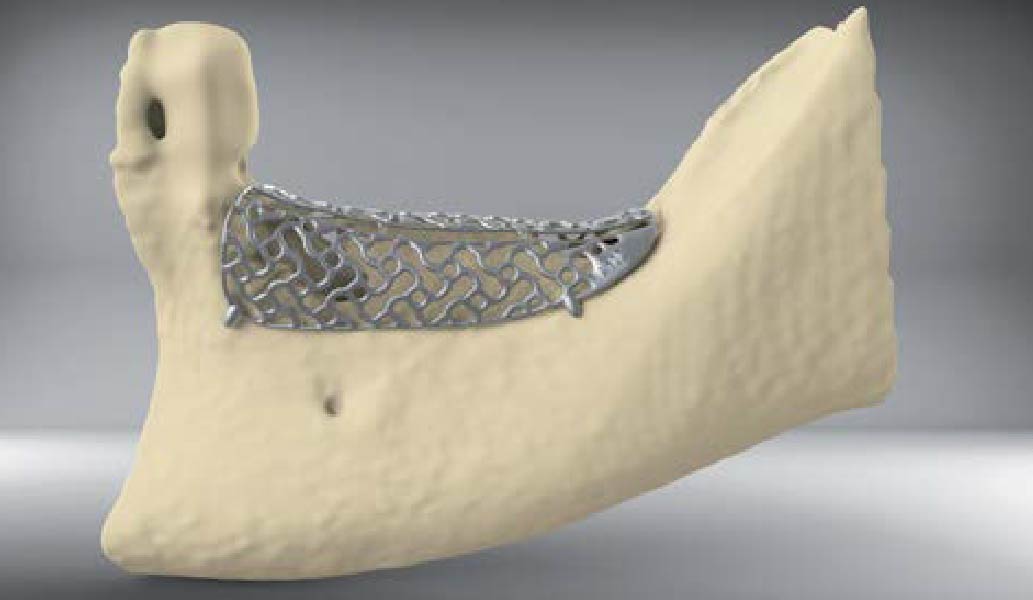
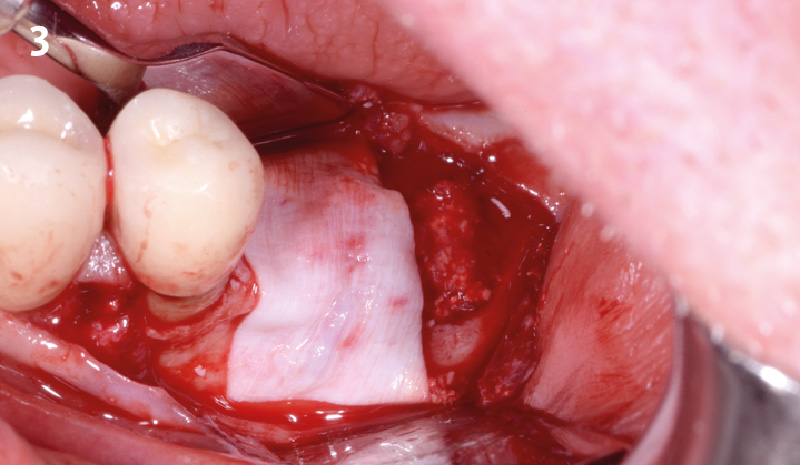
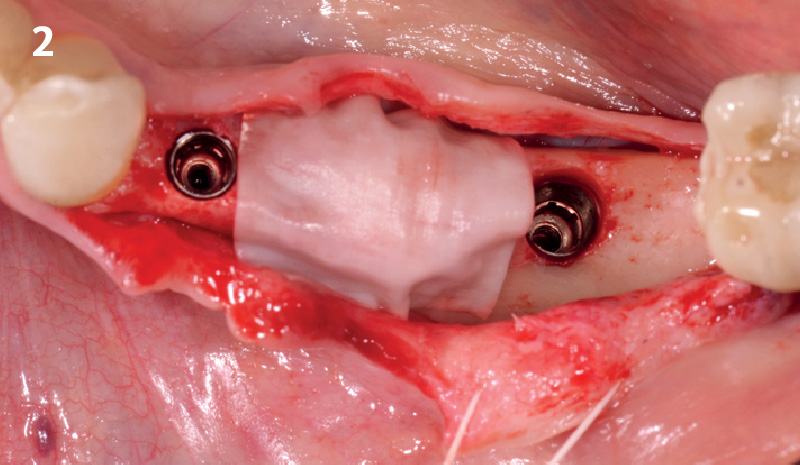
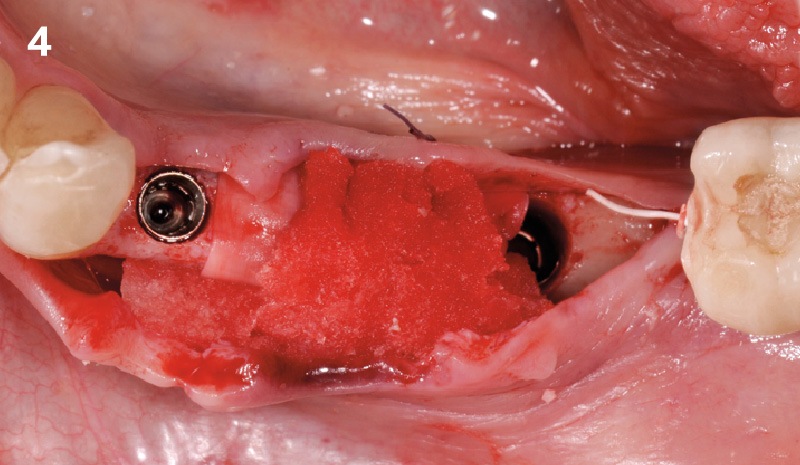
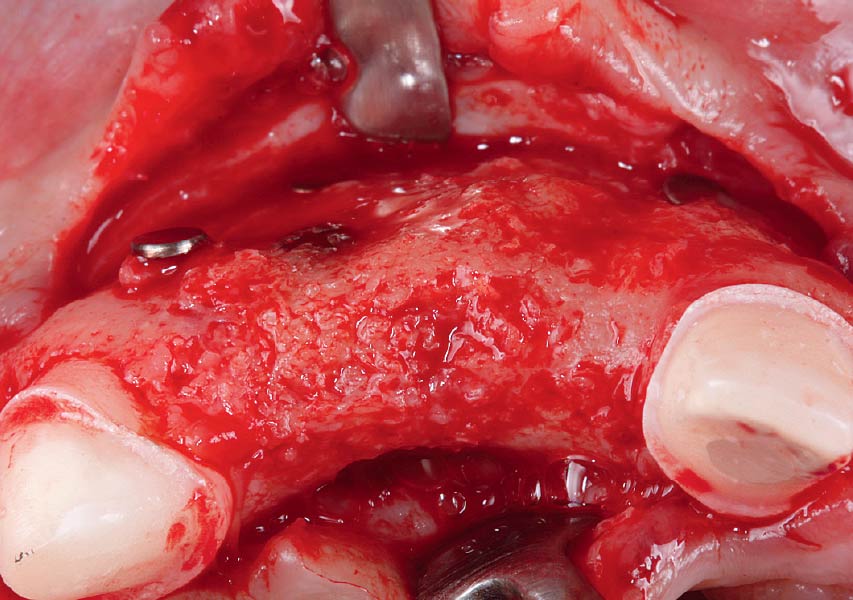
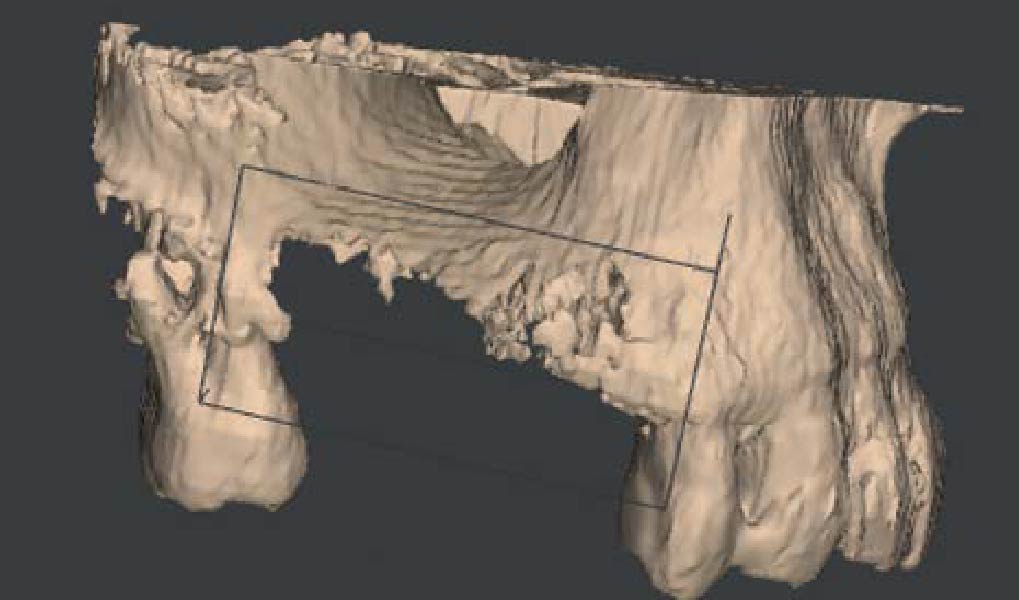
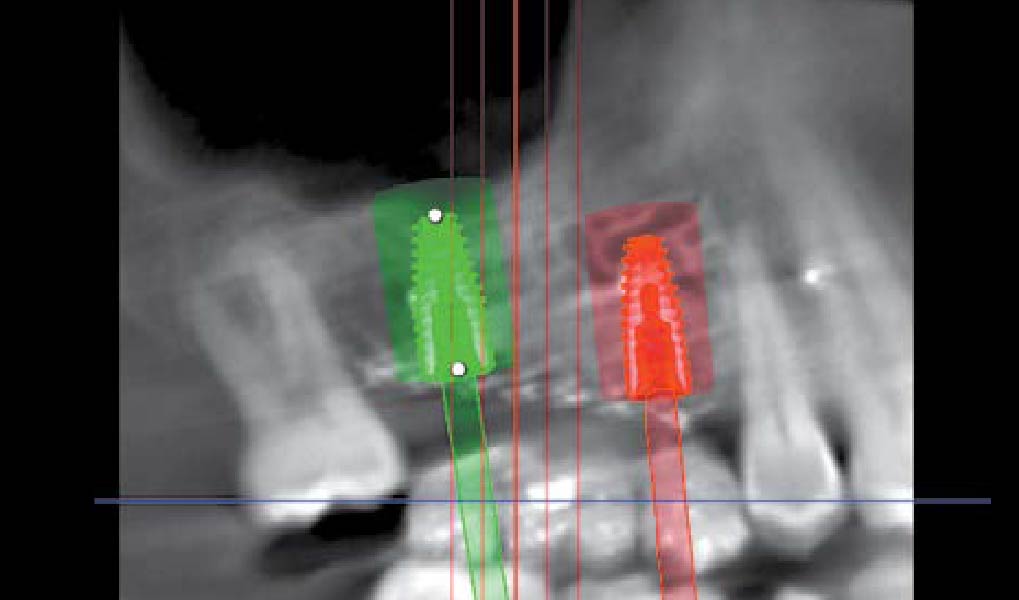
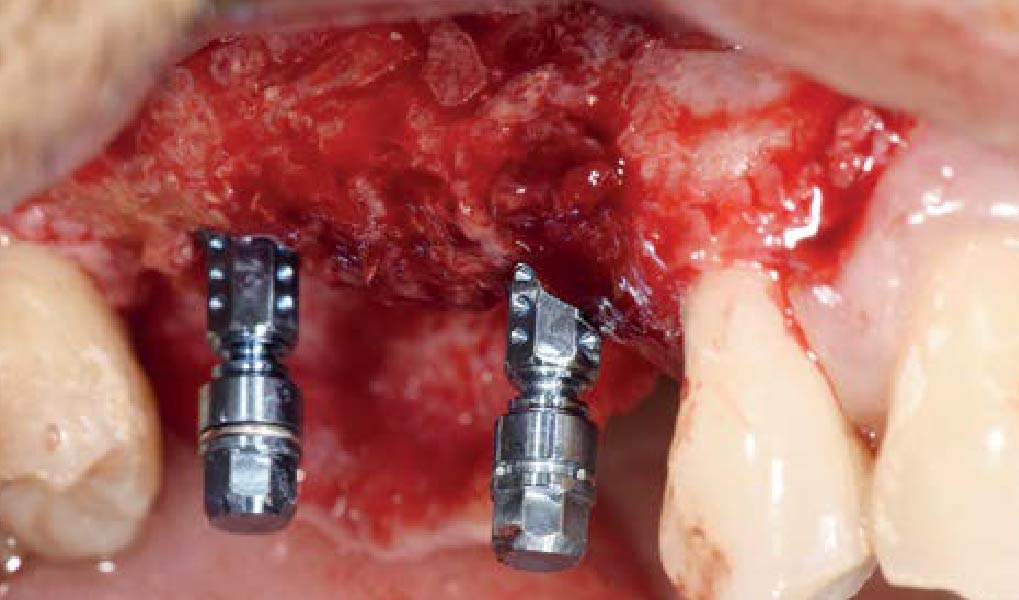
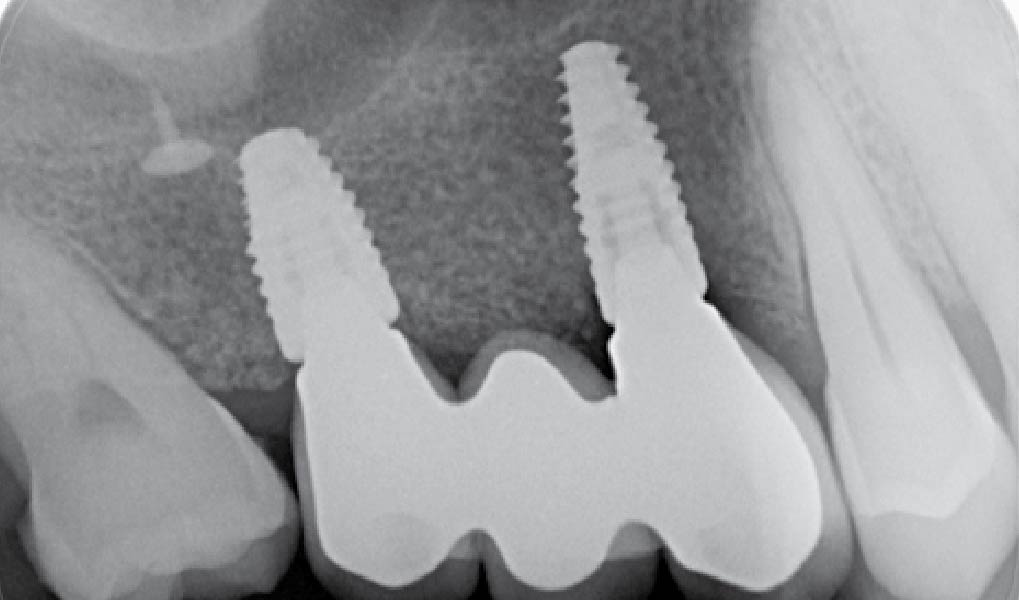
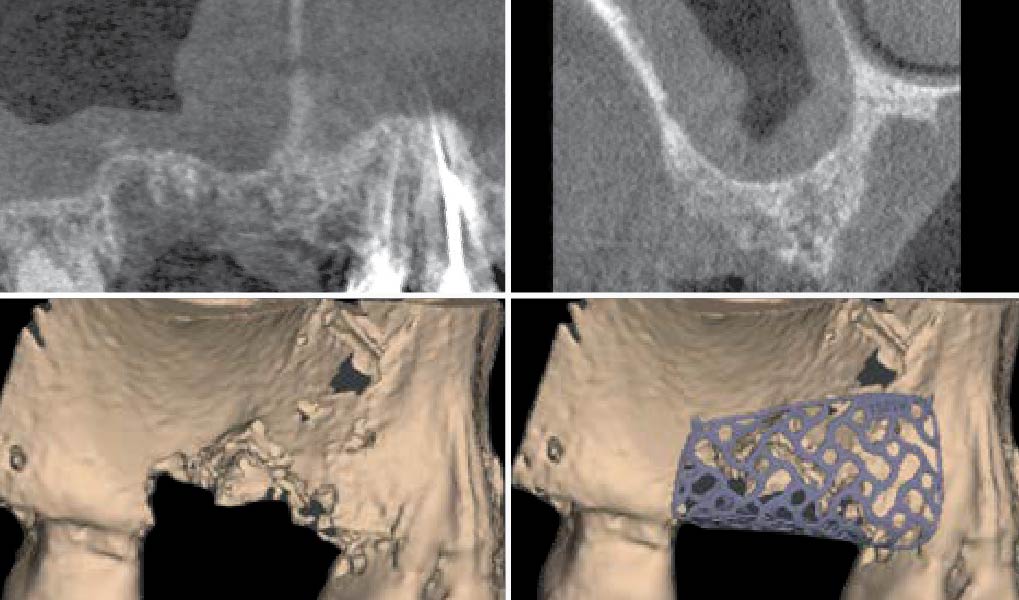
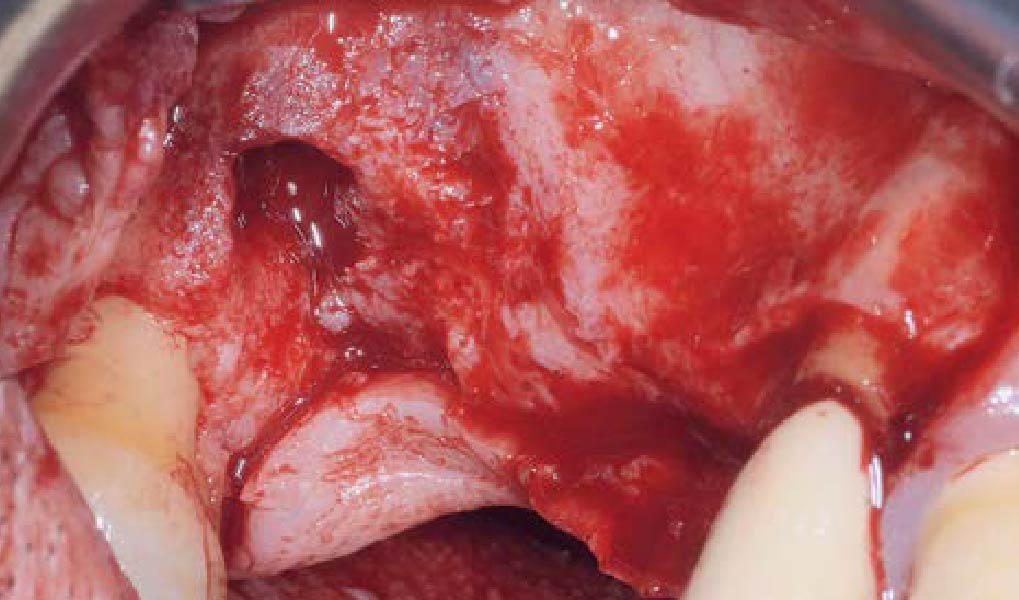
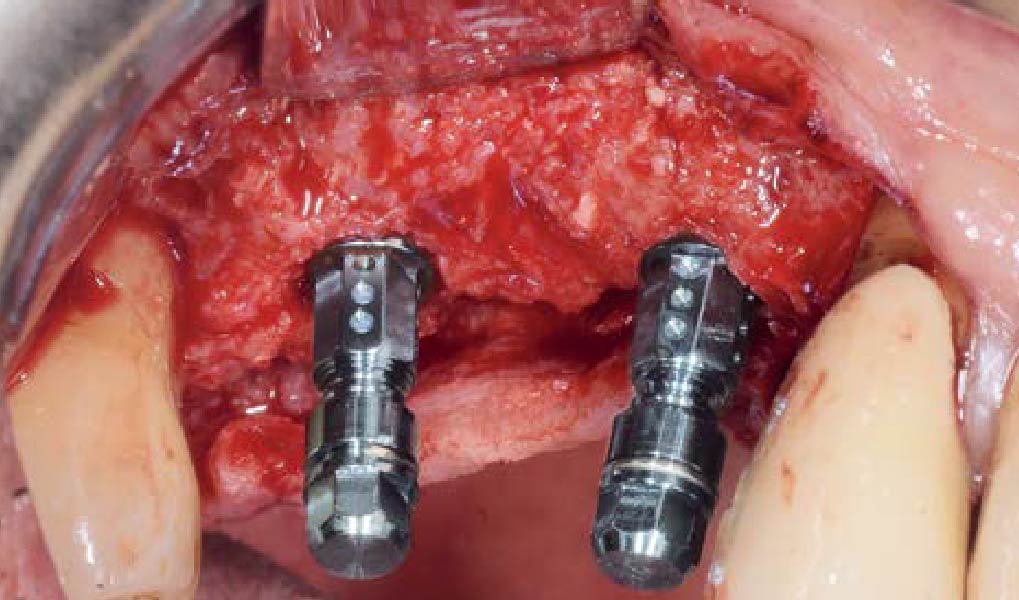
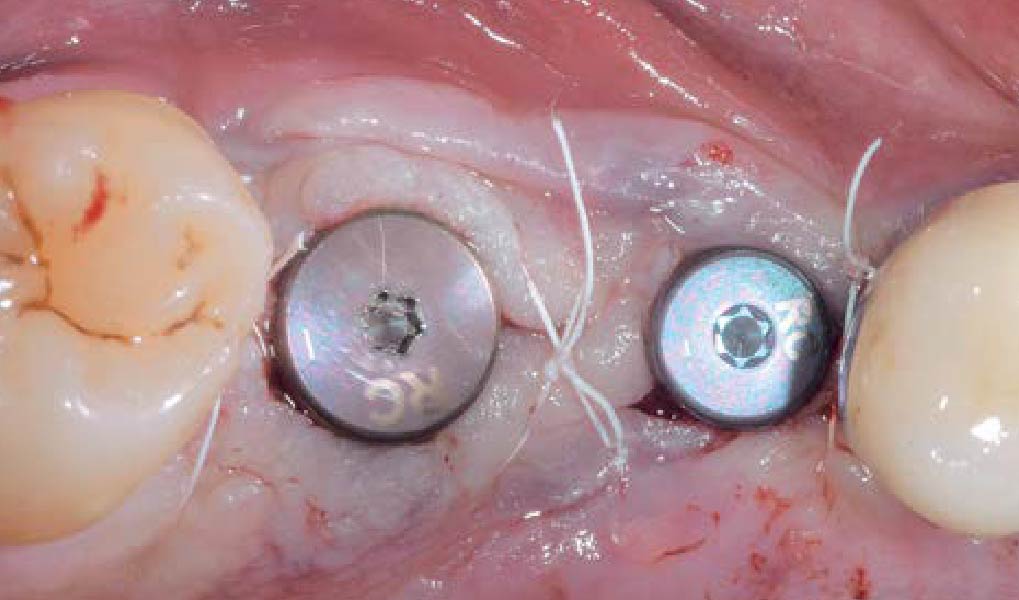
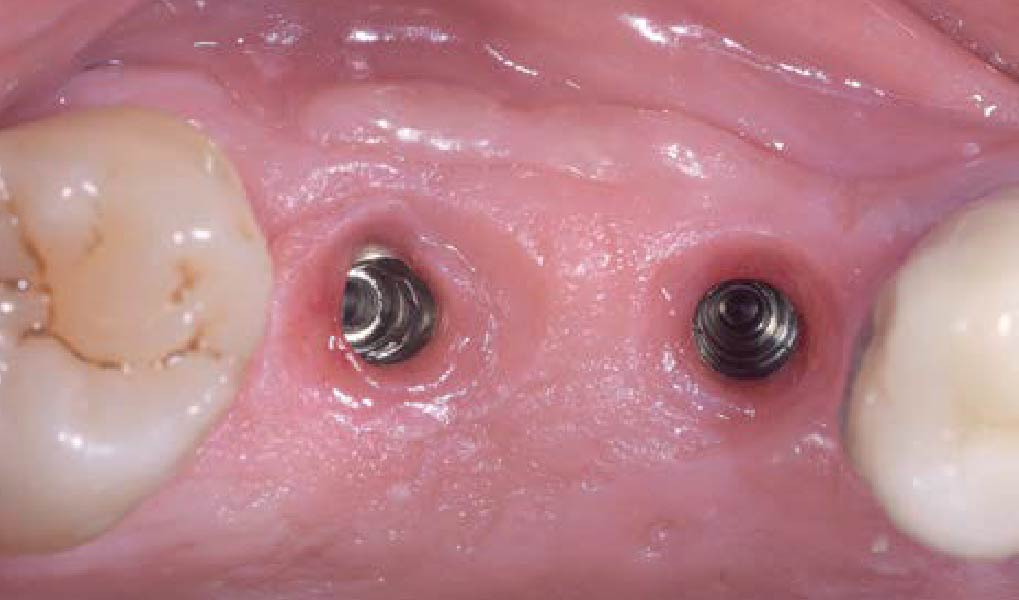
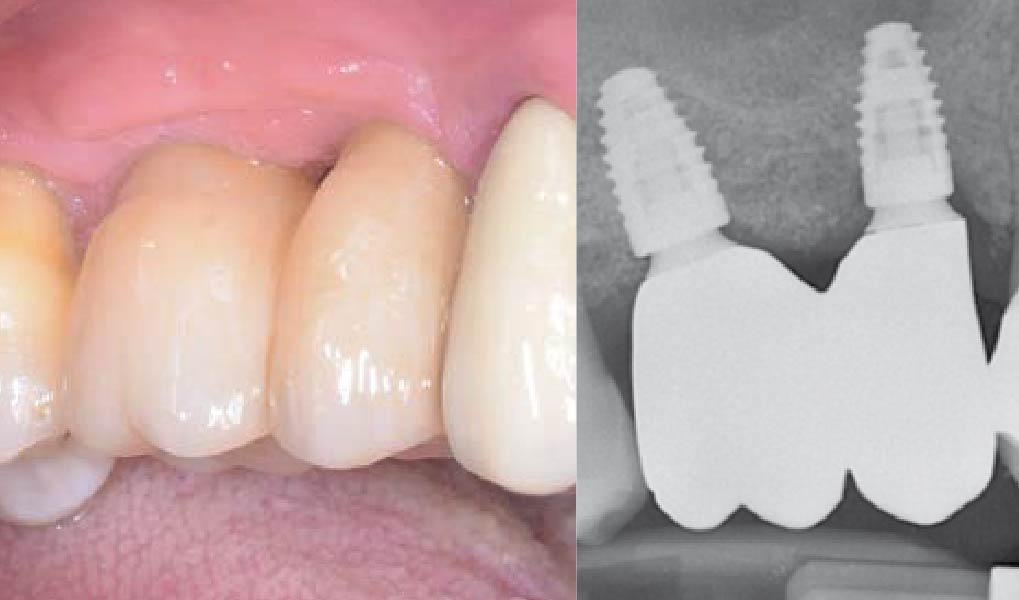
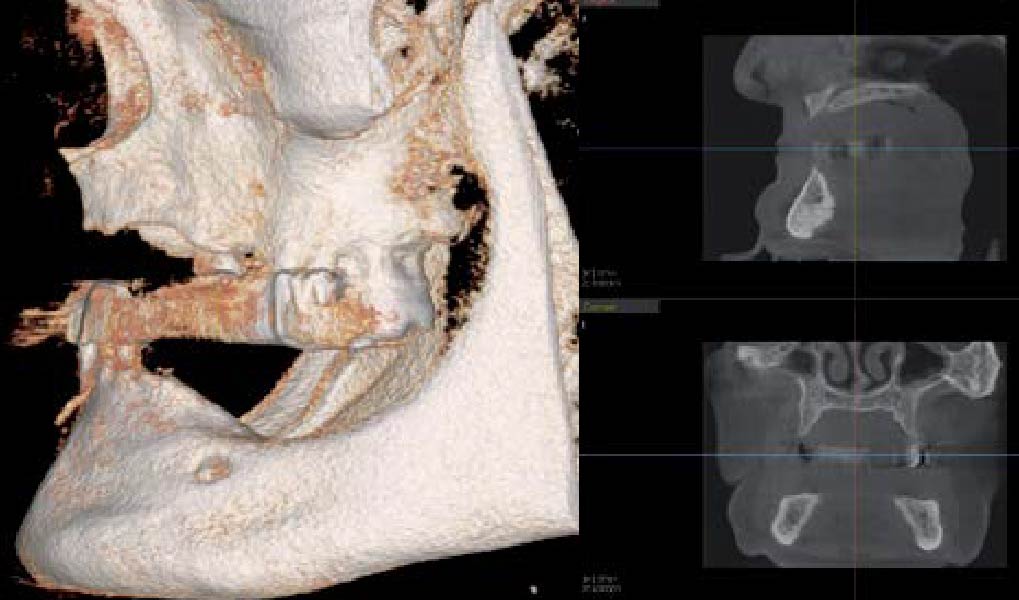
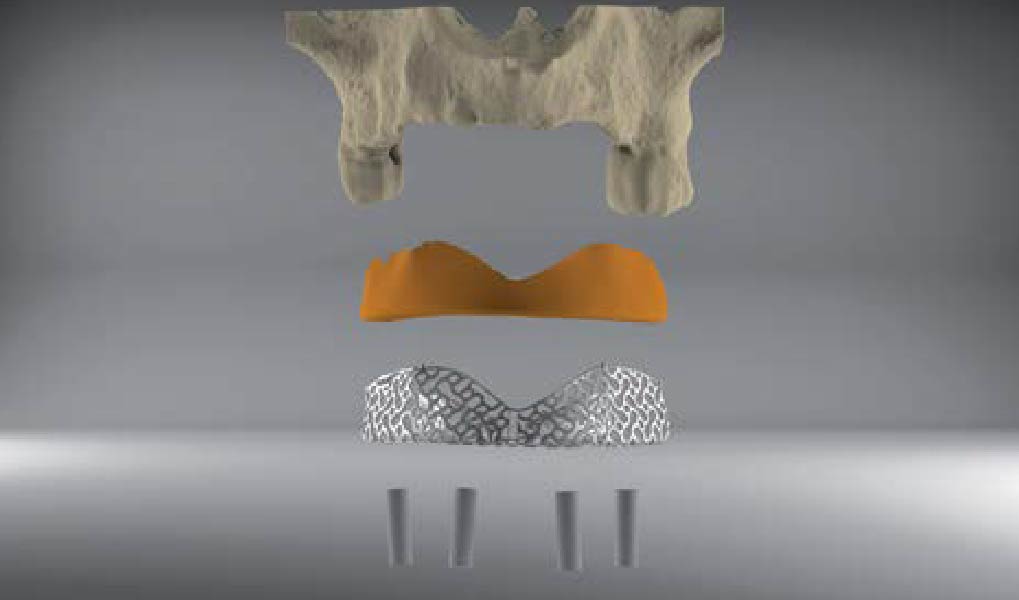
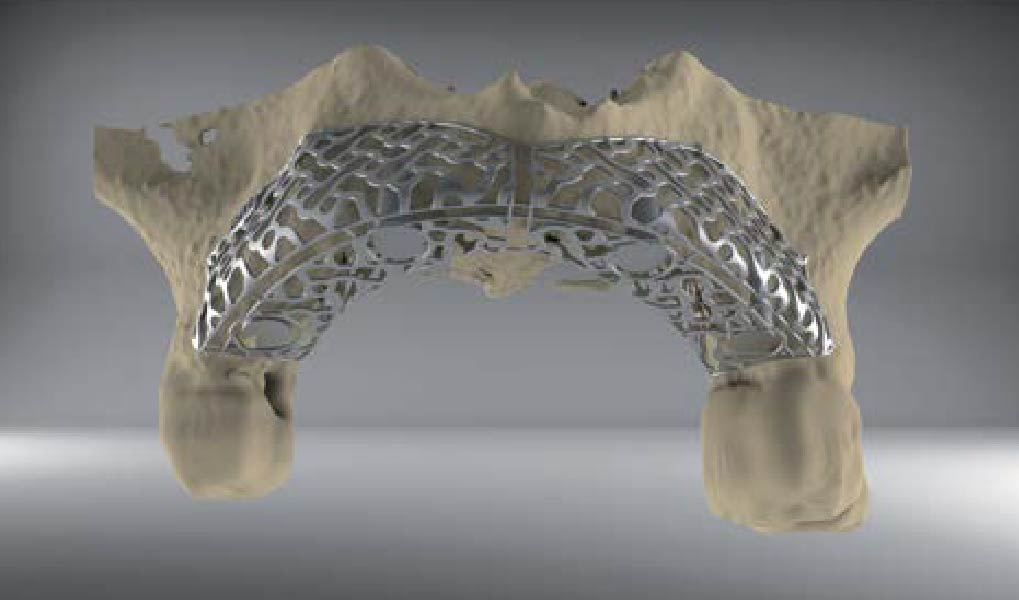
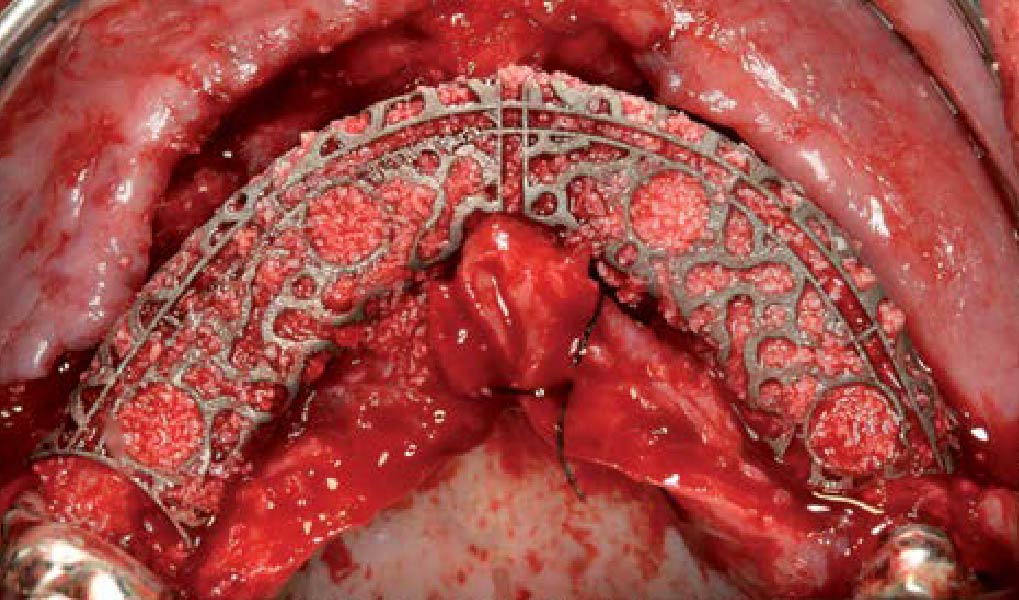
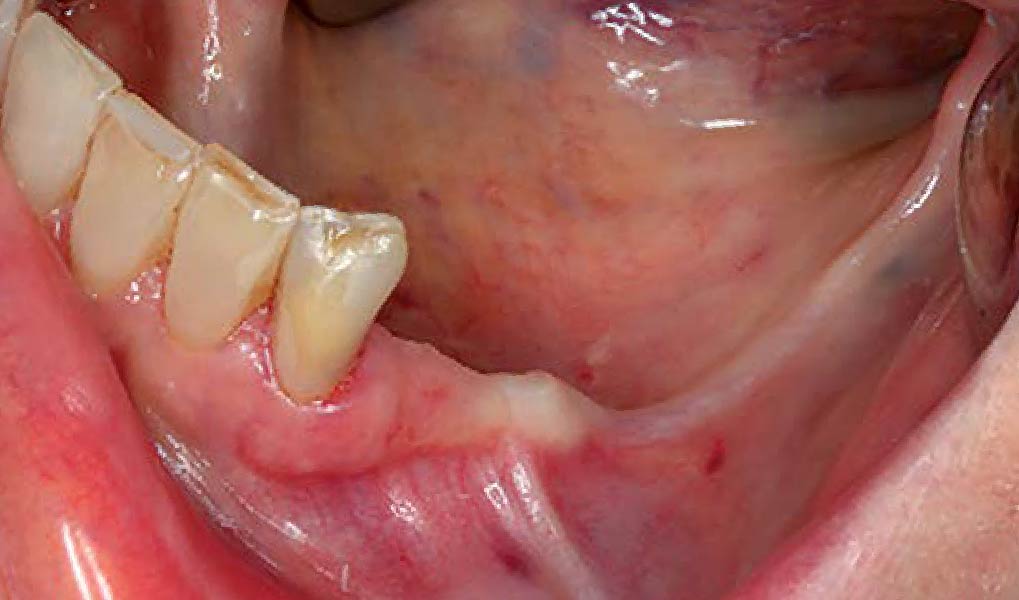
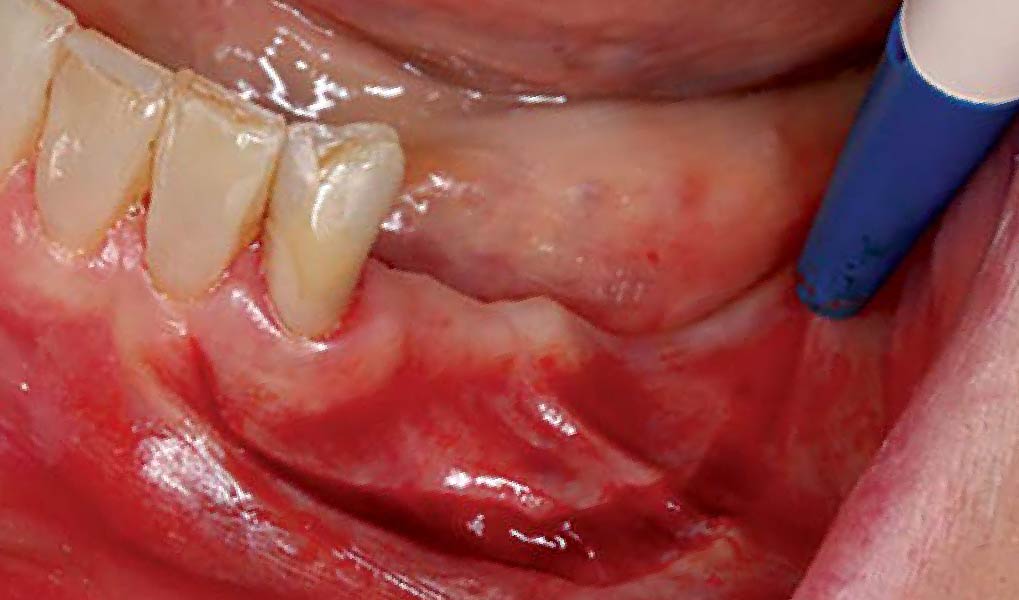
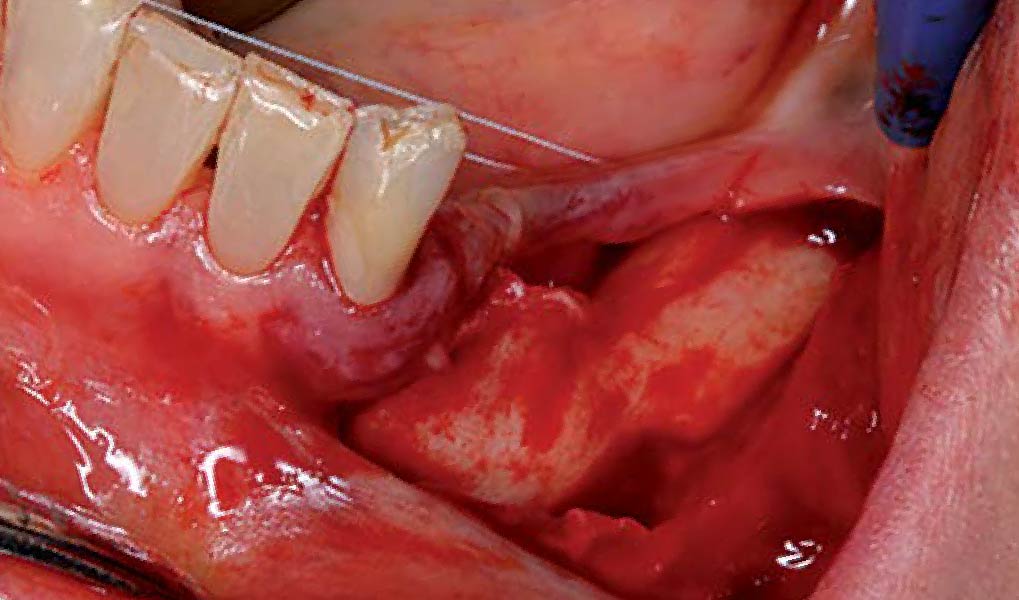
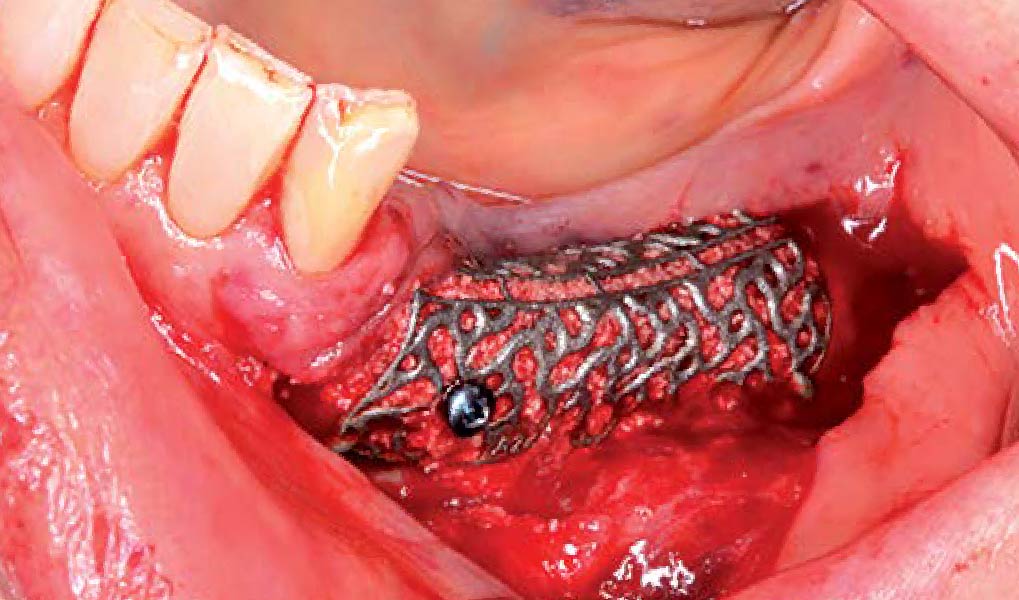
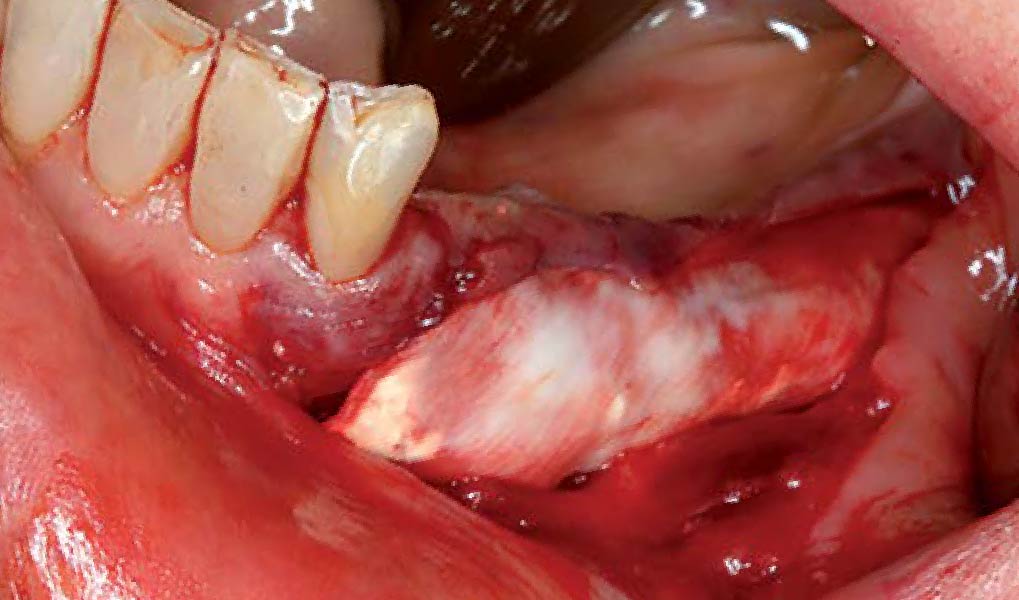
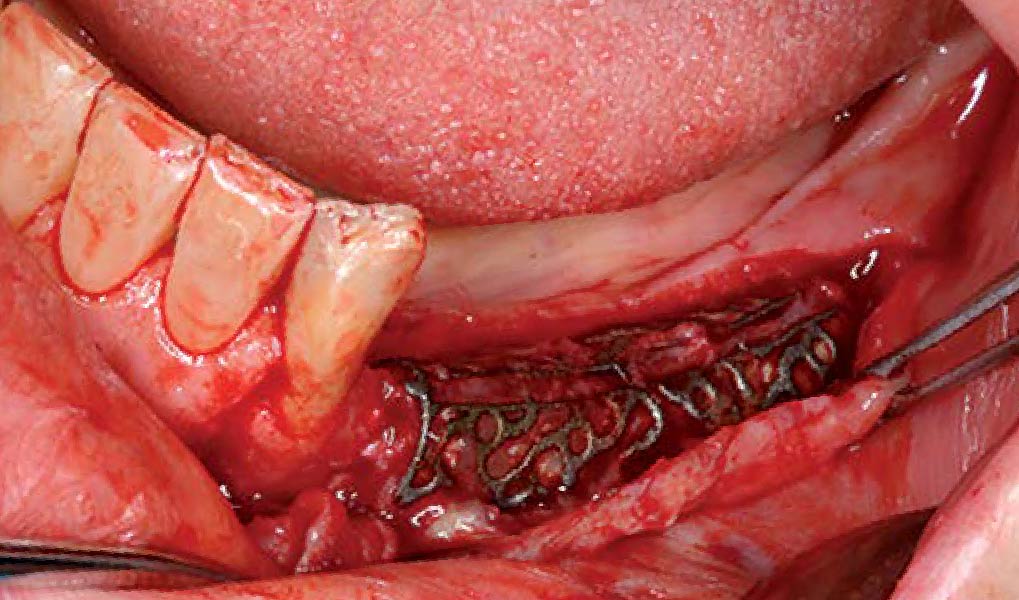
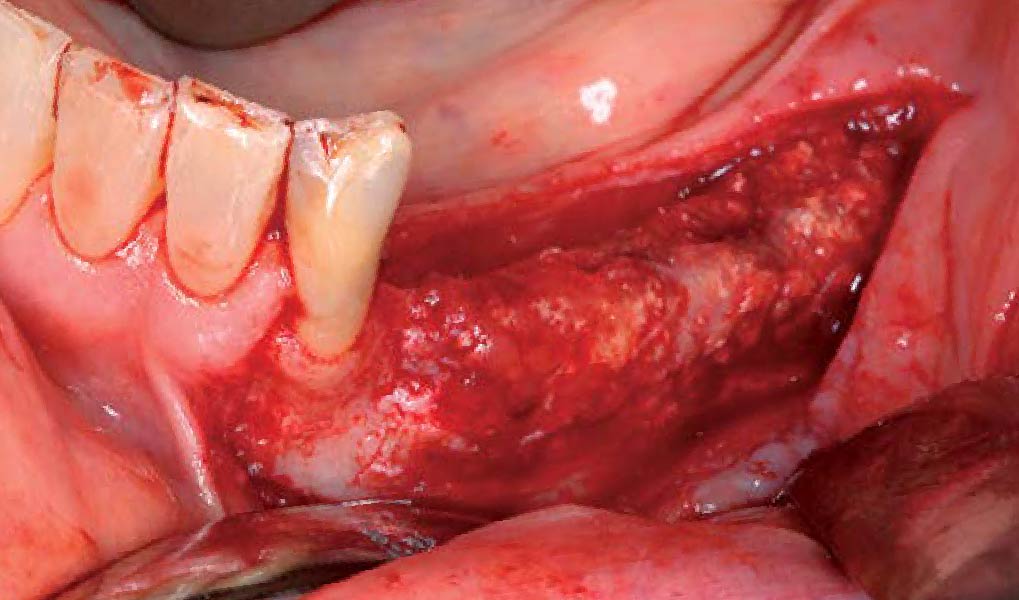
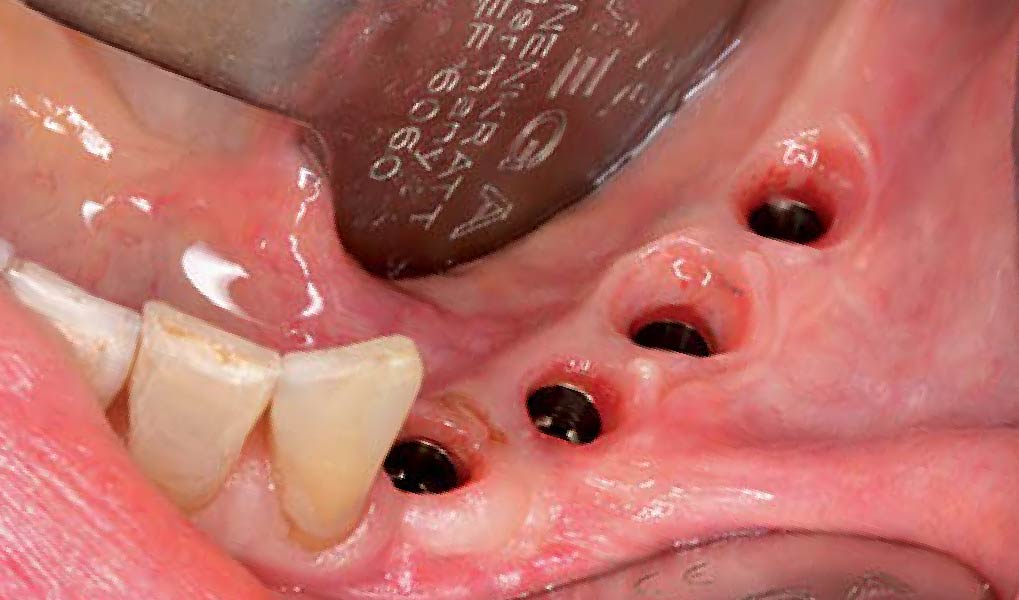
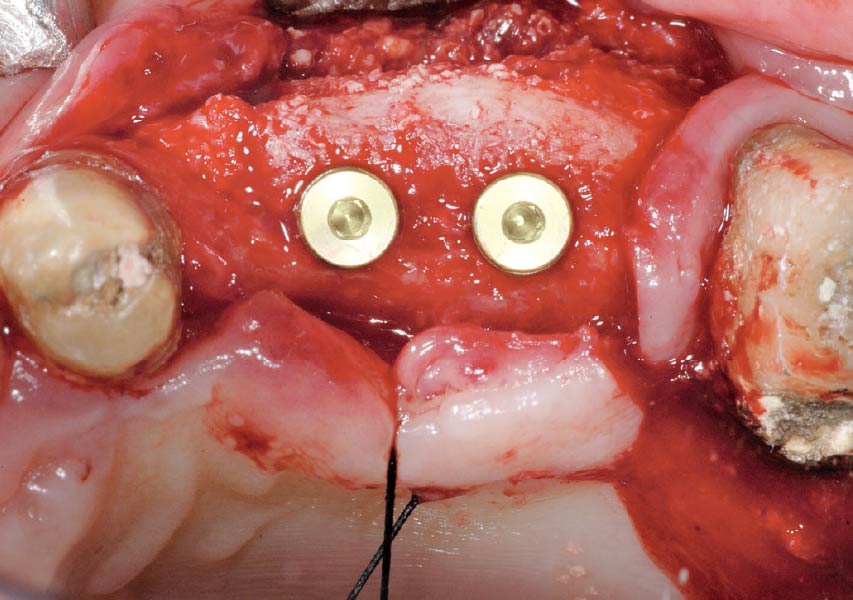
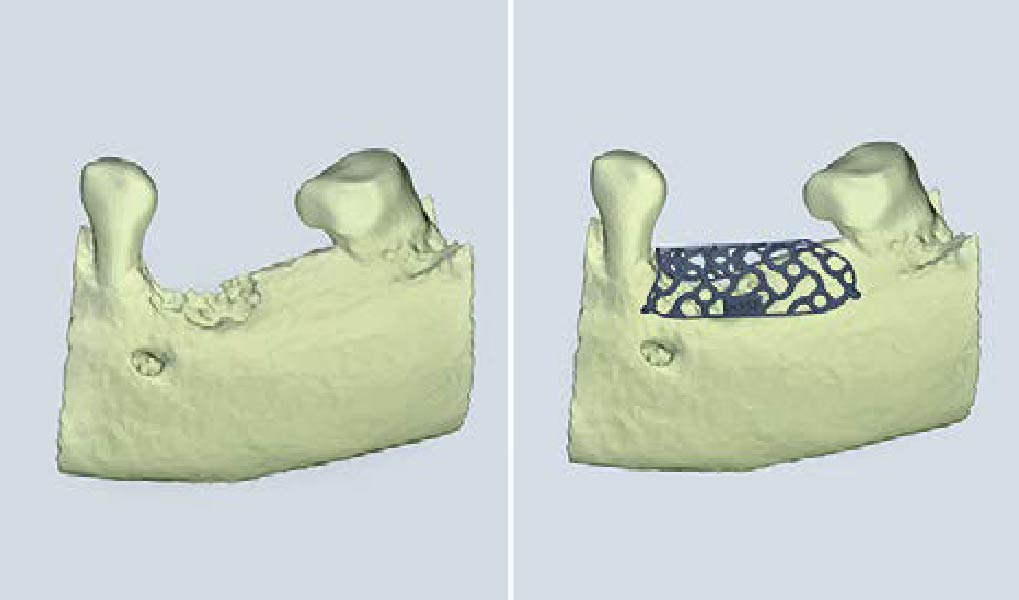
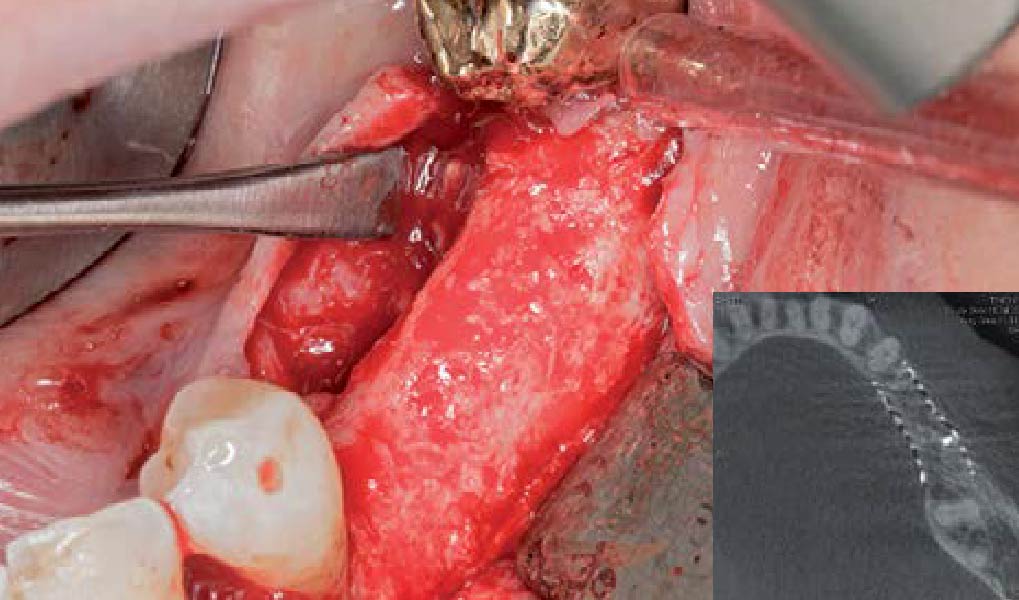
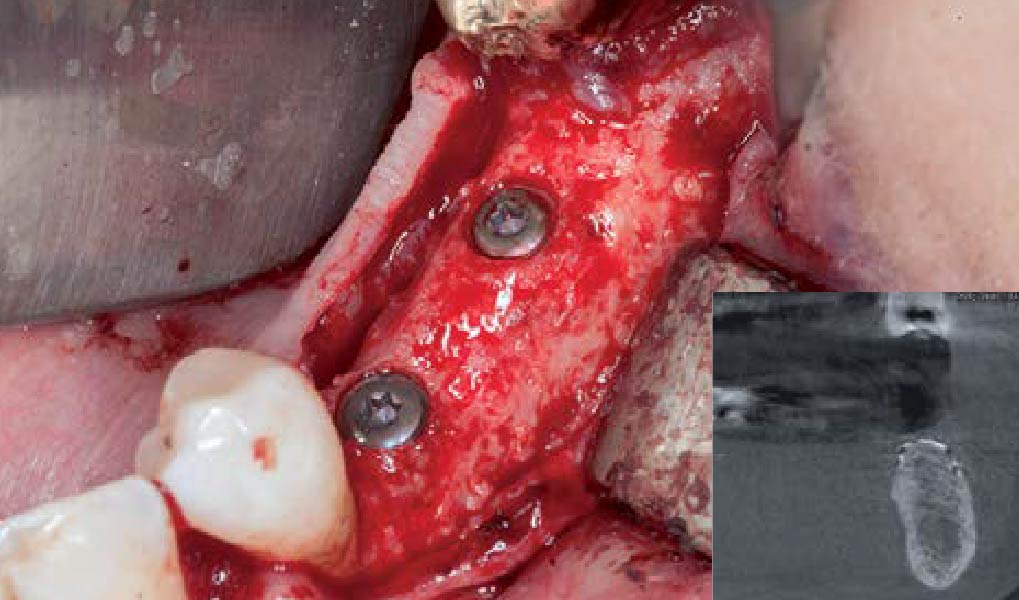
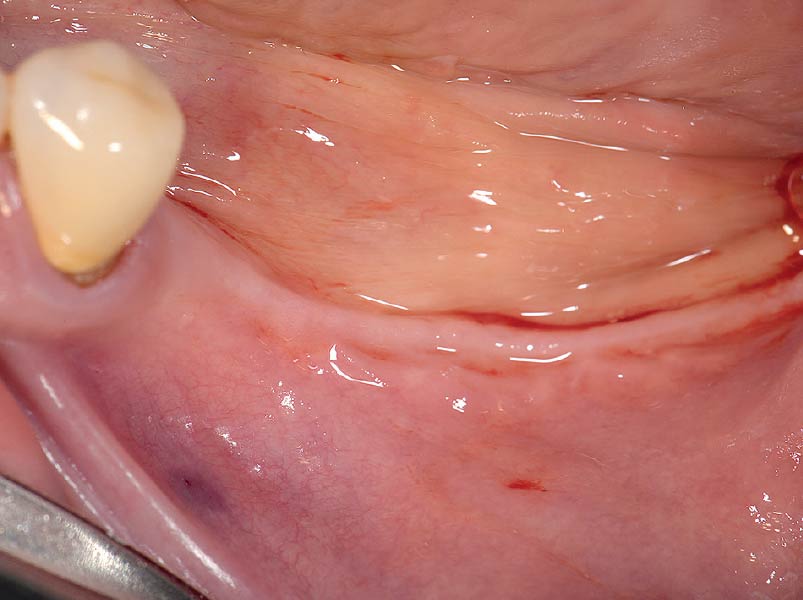
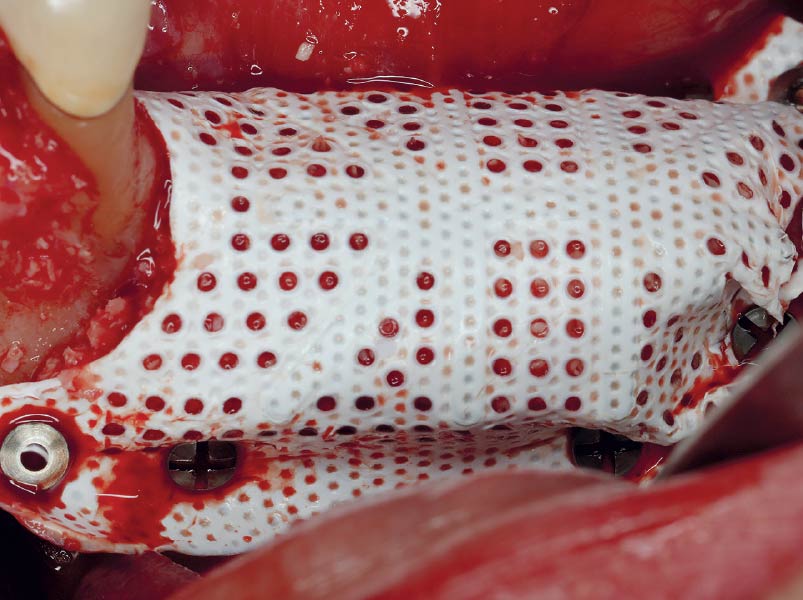
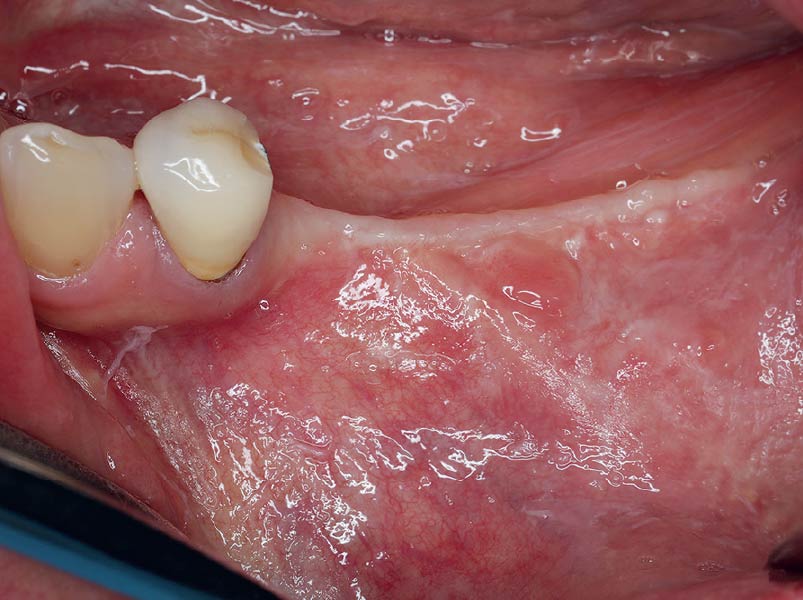
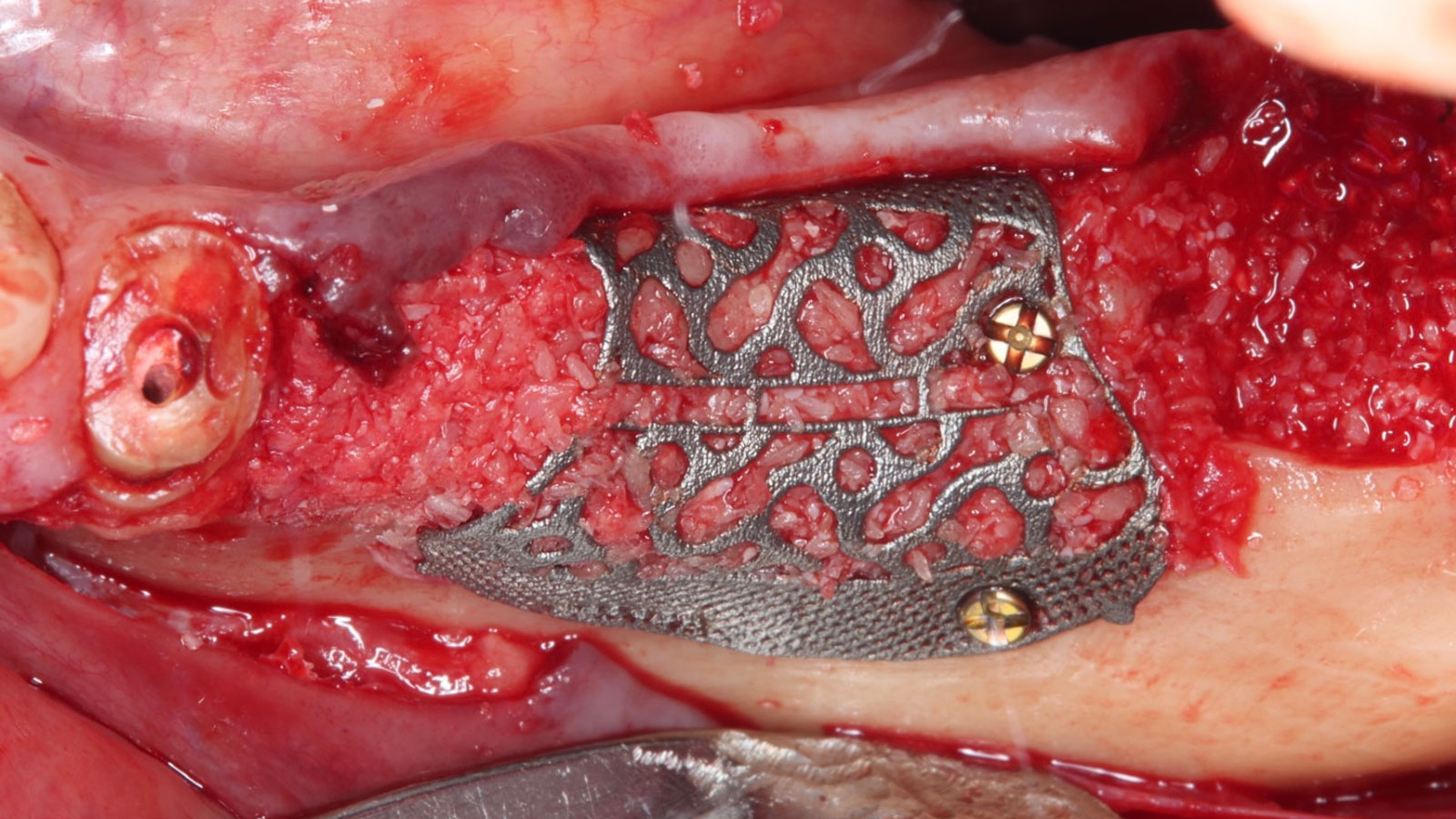
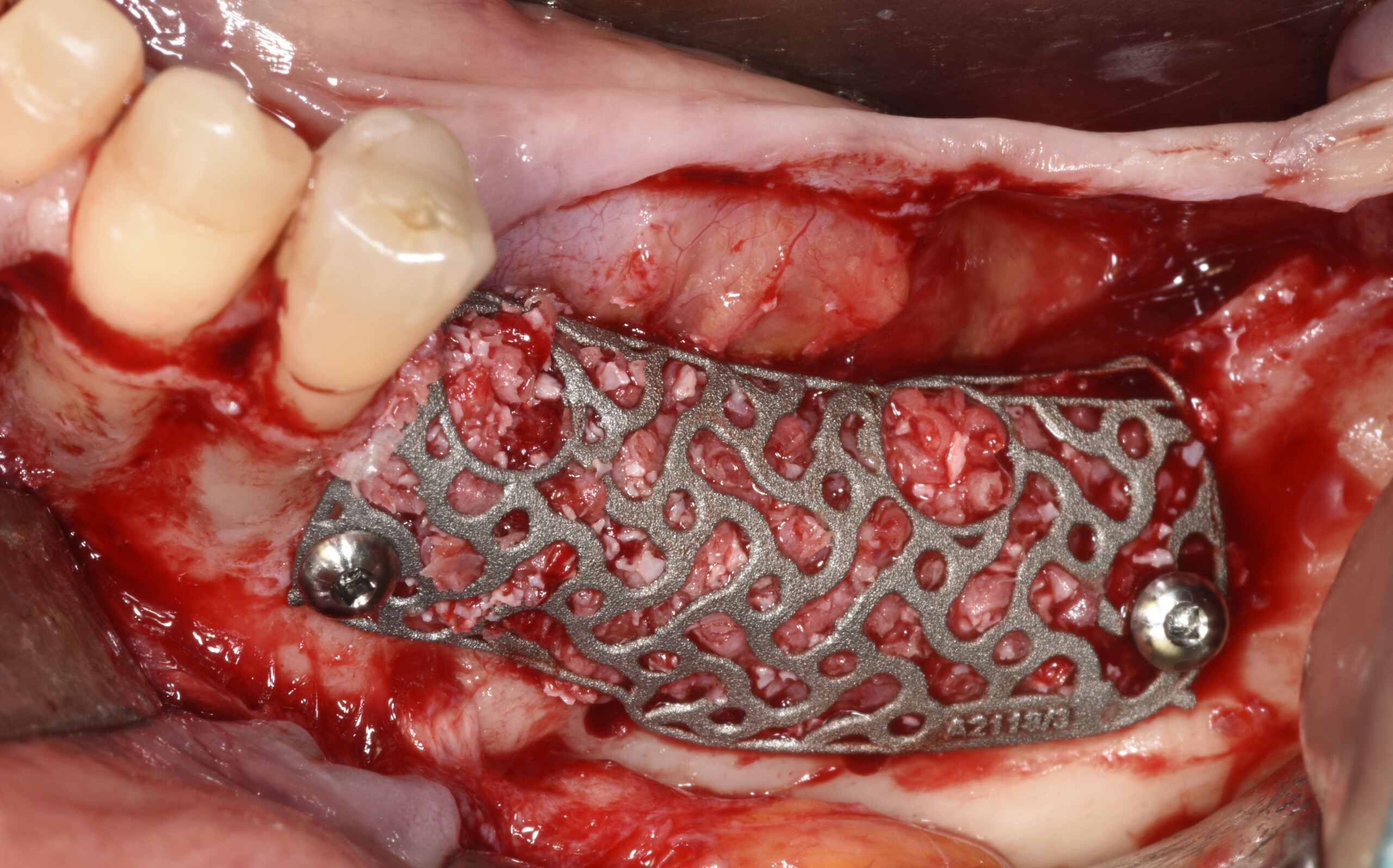
A 60-year-old healthy male presented with a failing lower left bridge. Due to a long history of missing teeth, he had a significantly atrophic mandibular ridge. We decided to use a customized titanium mesh to achieve the necessary vertical and horizontal bone augmentation for dental implant rehabilitation.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
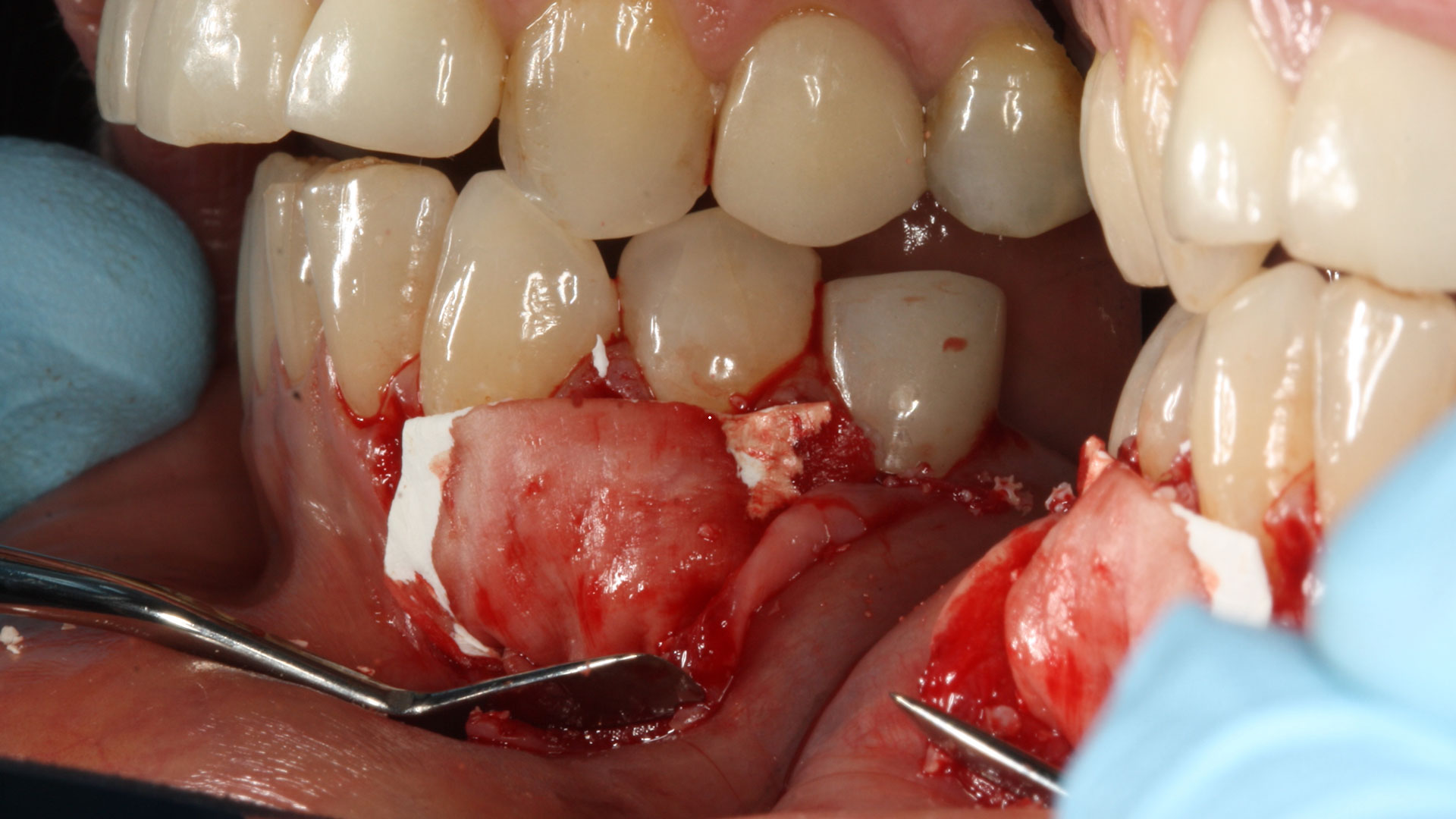
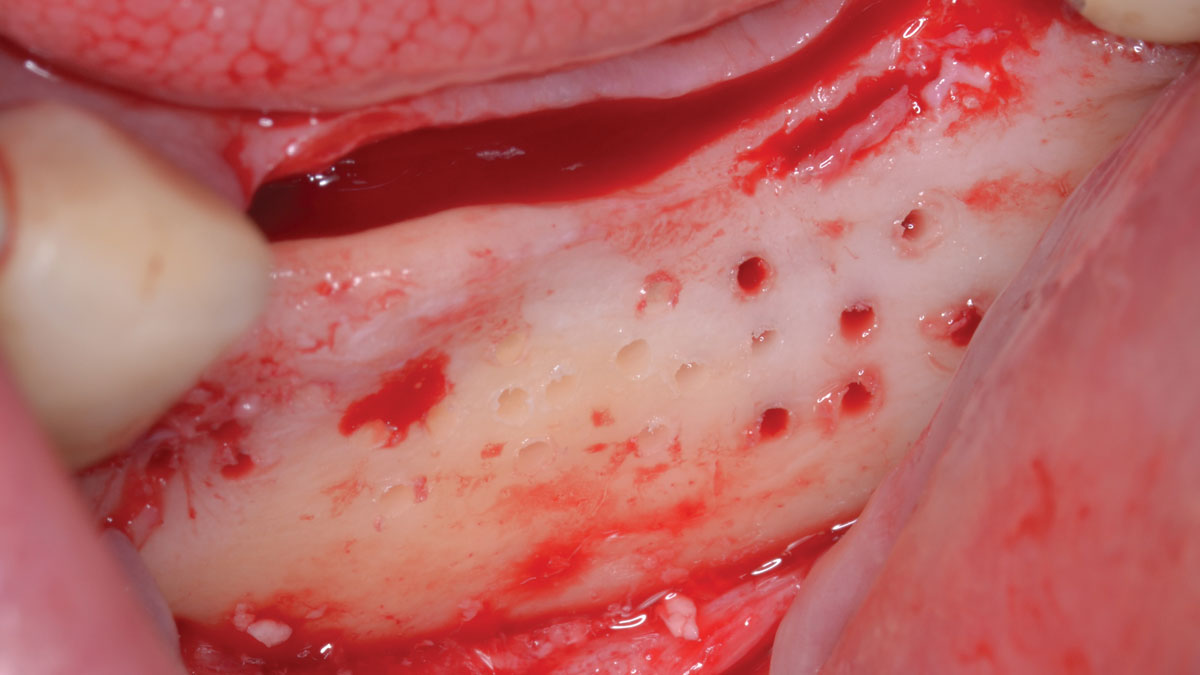
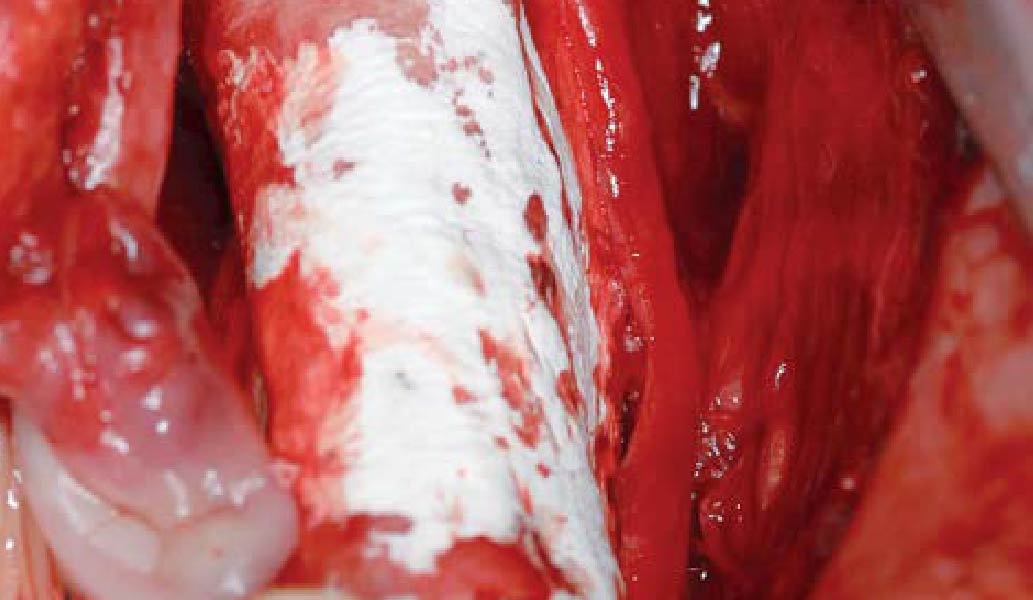
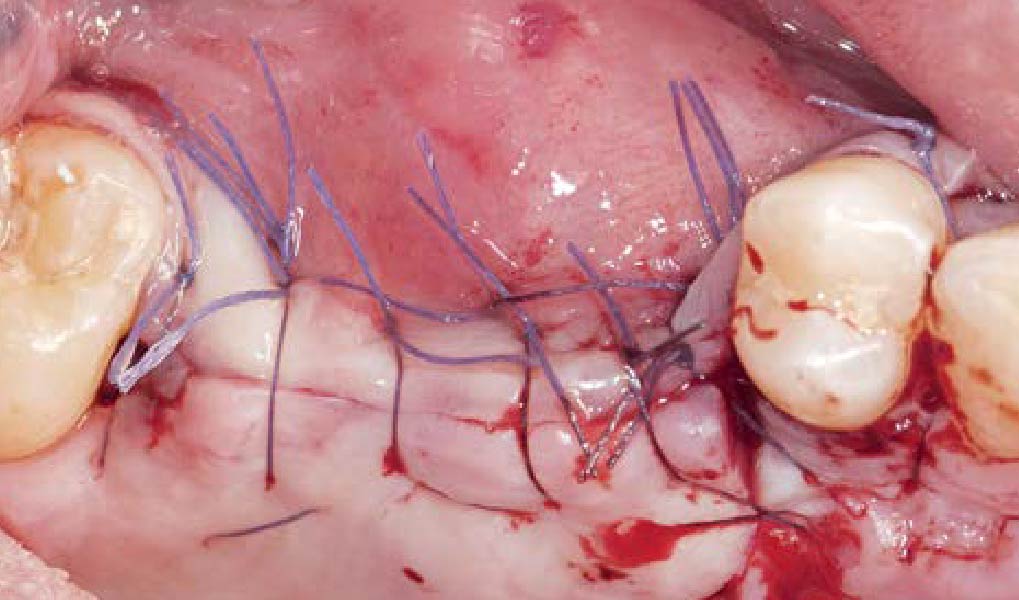
THE APPROACH
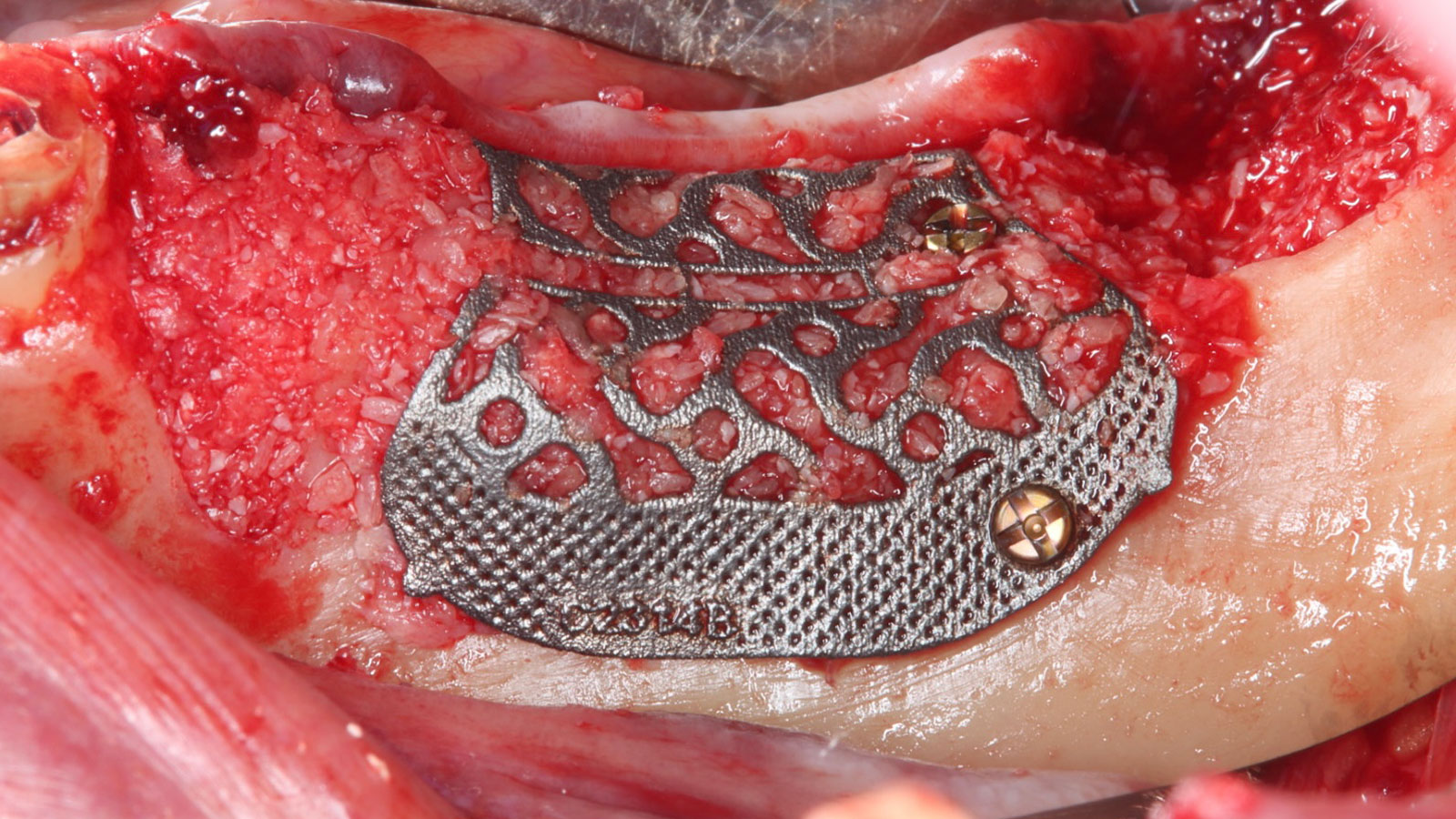
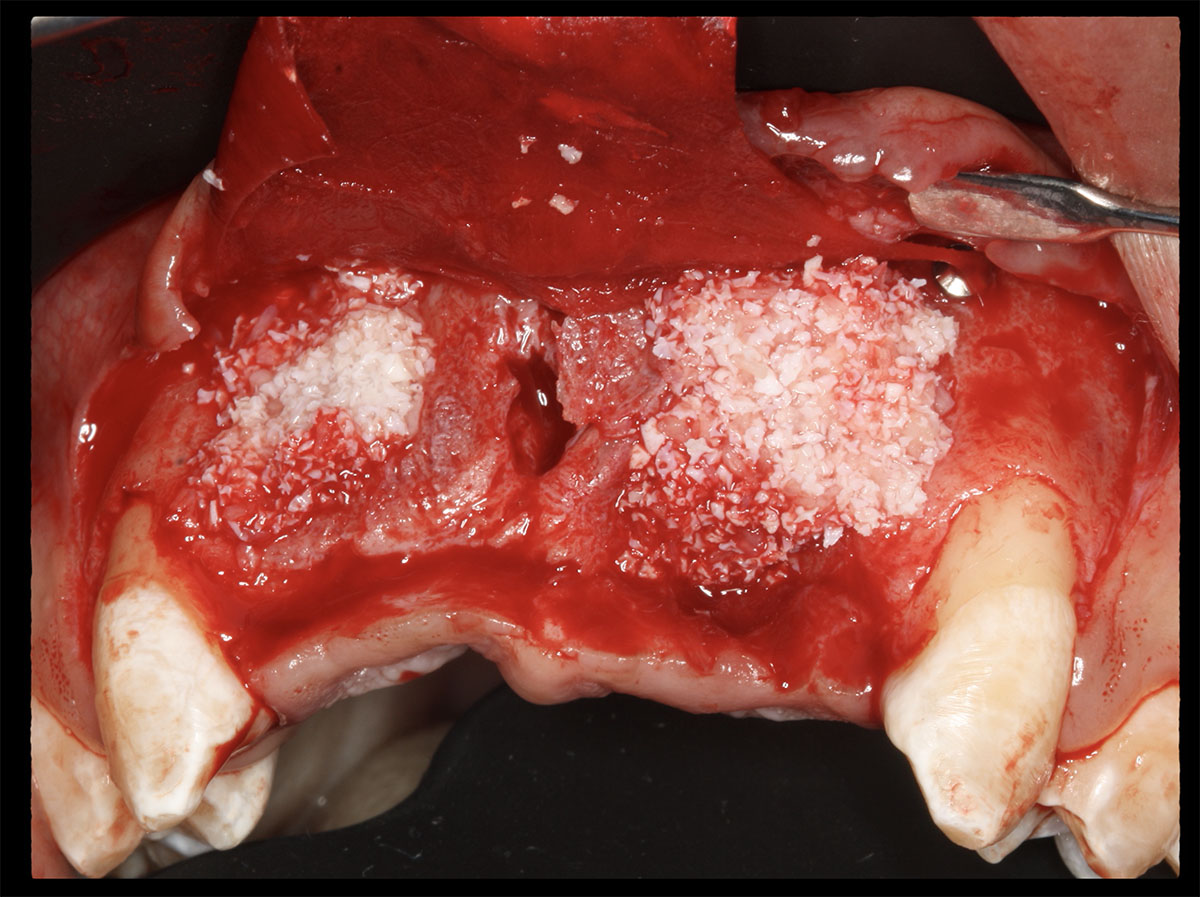
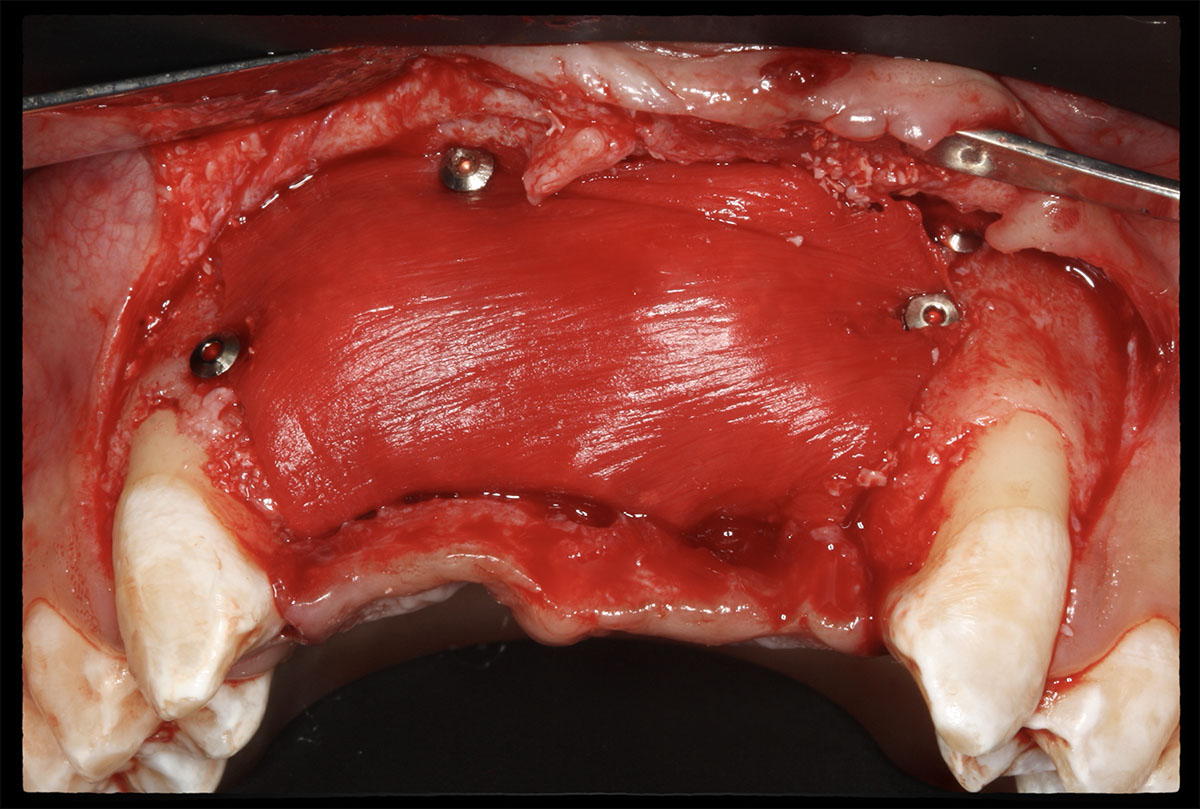
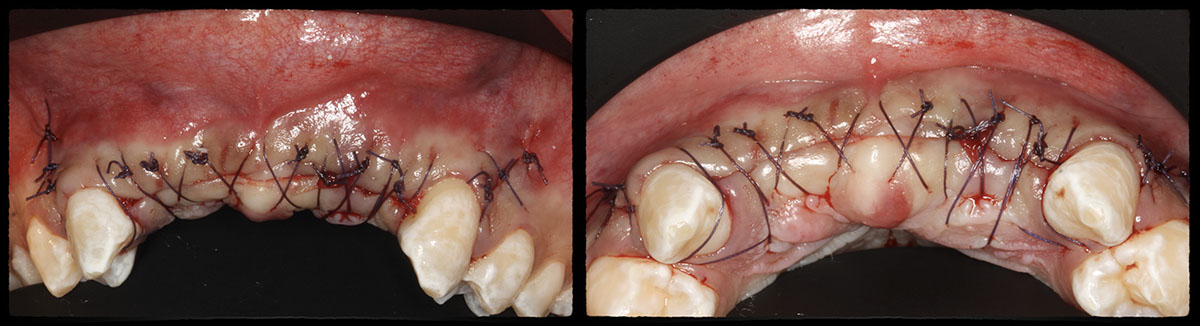
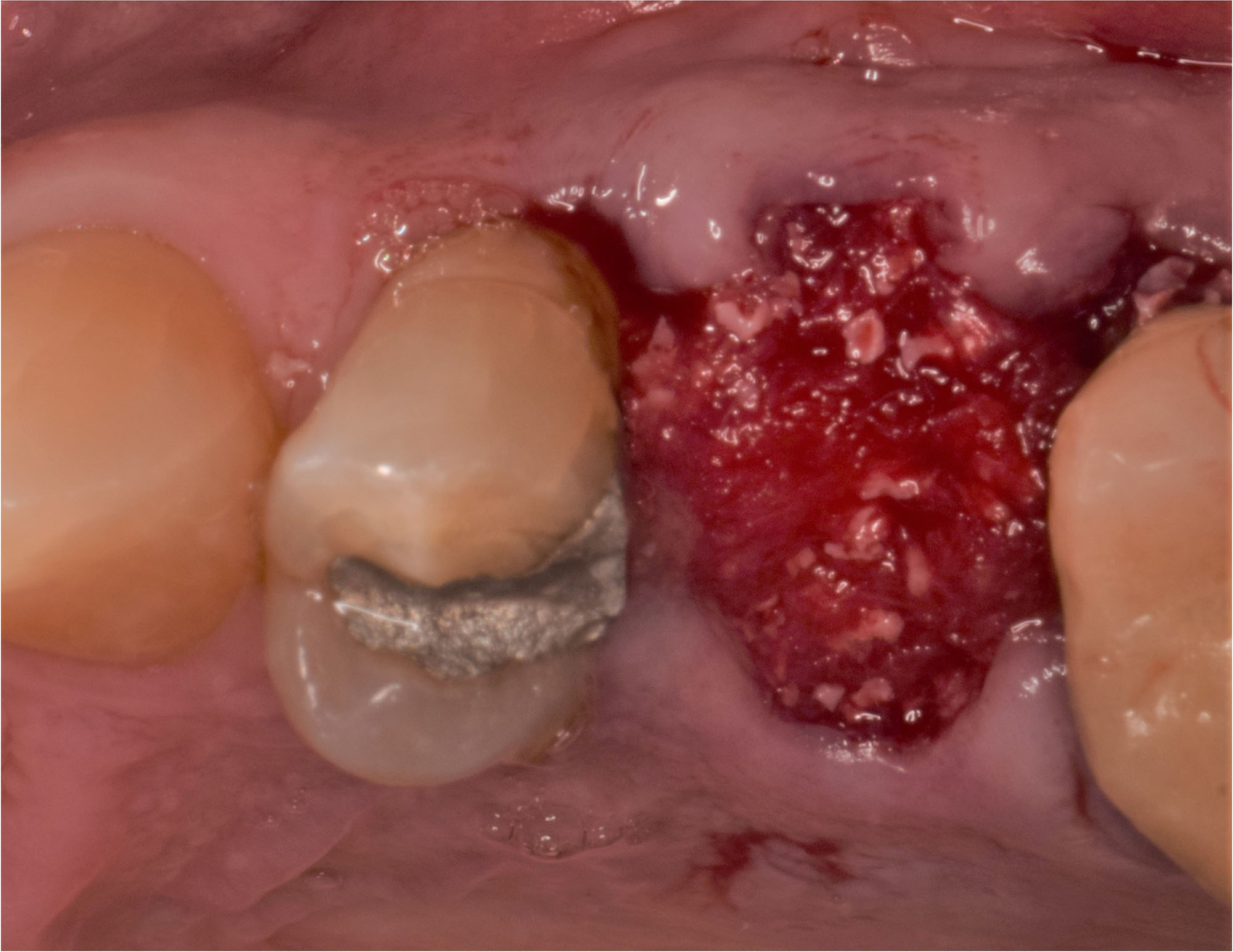
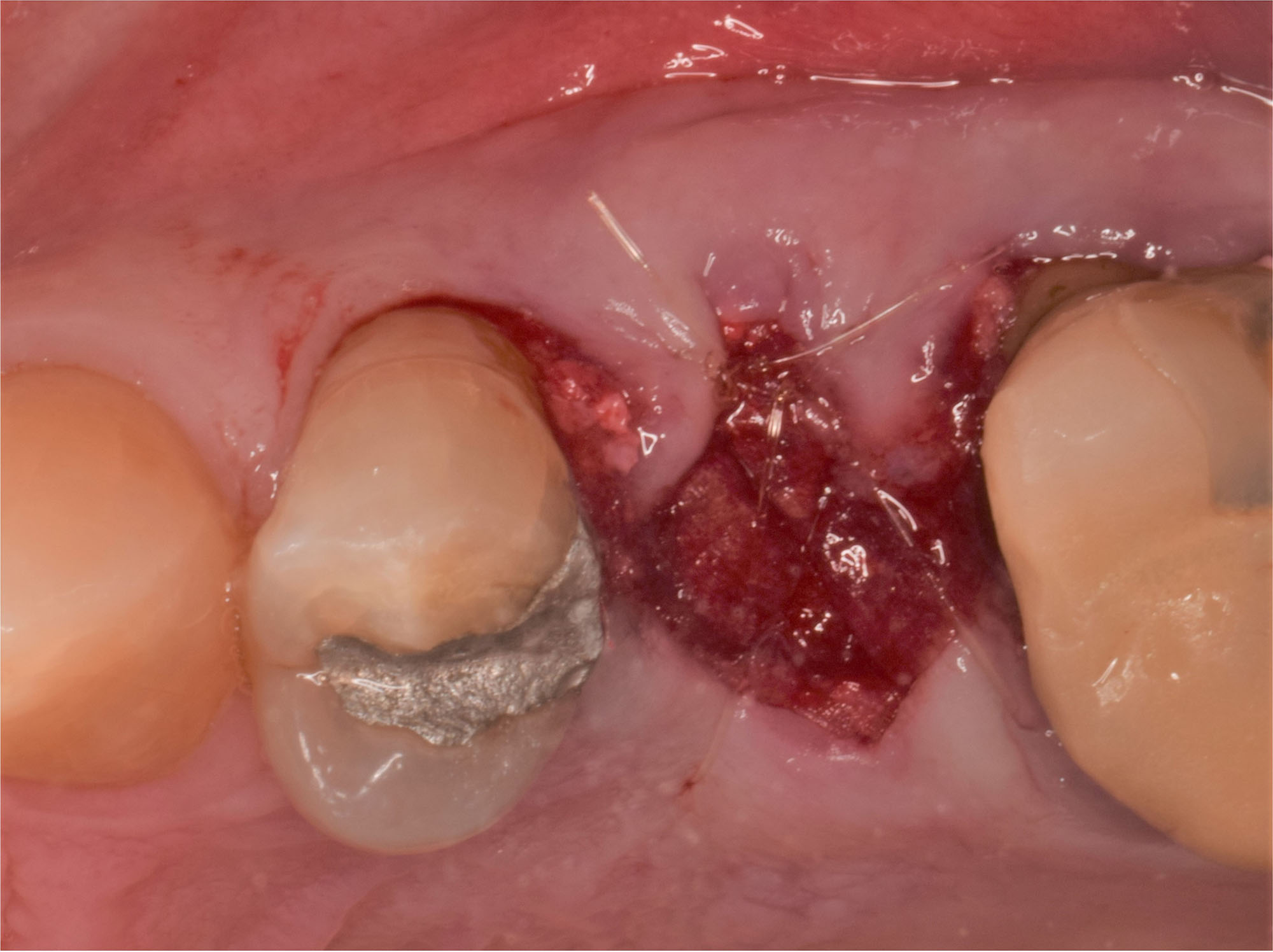
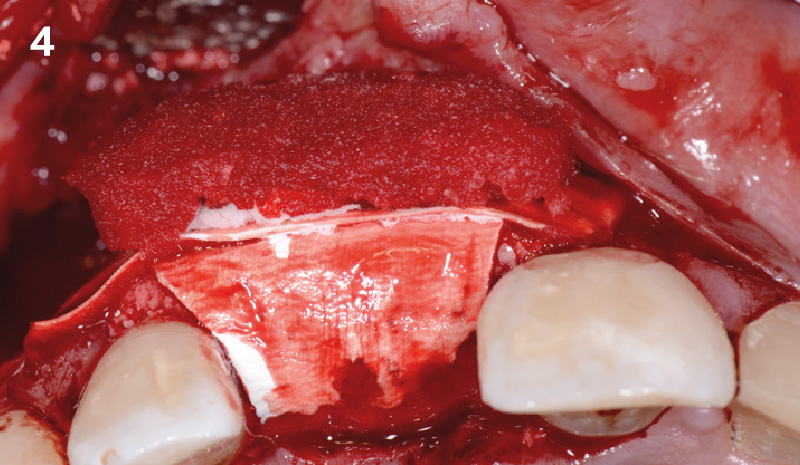
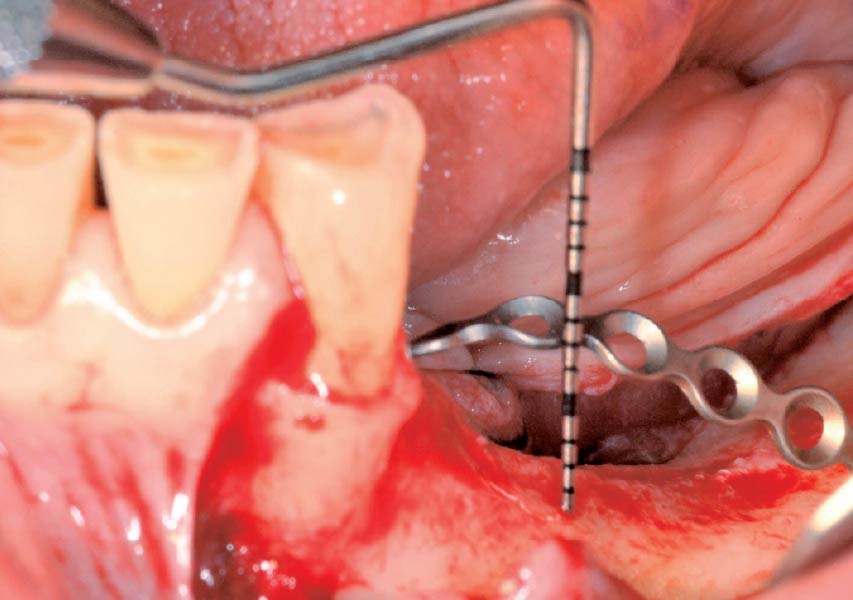
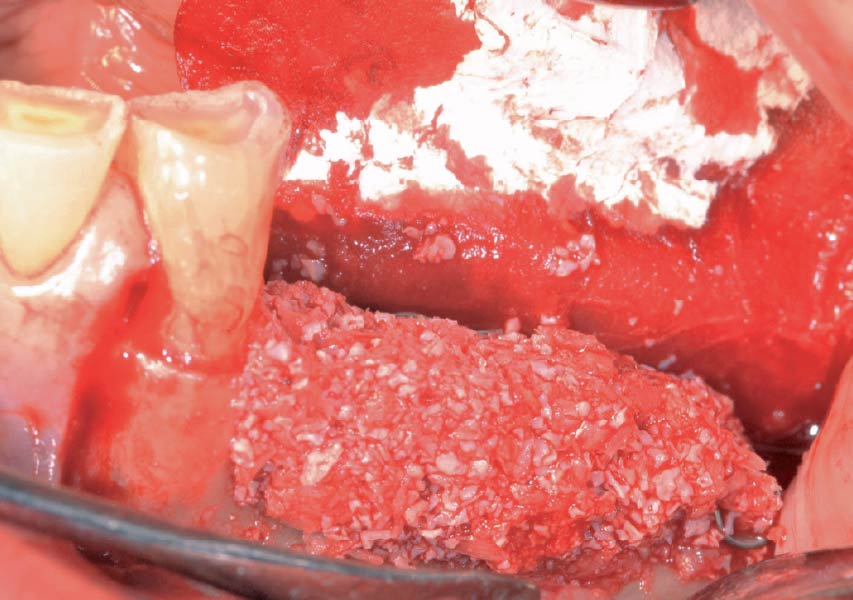
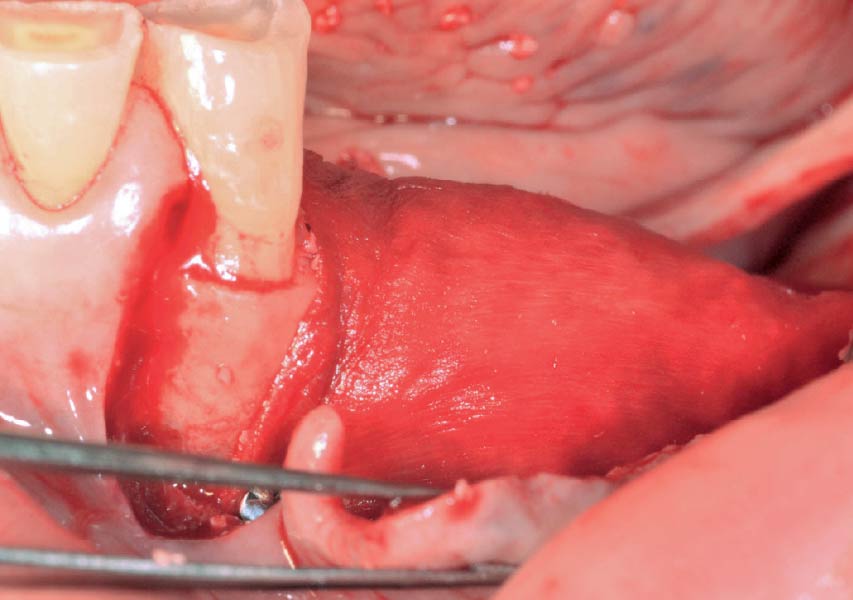
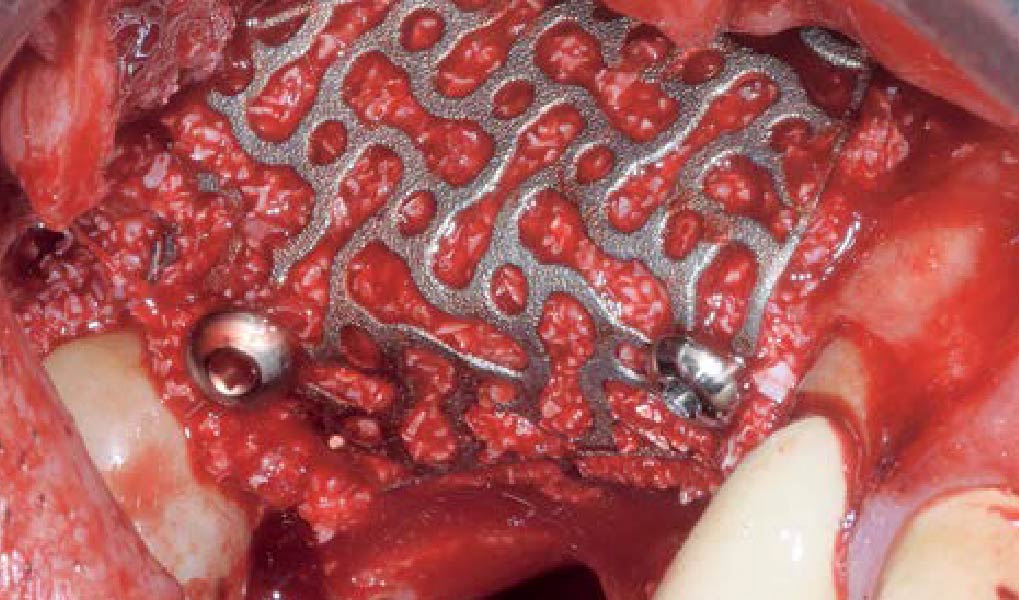
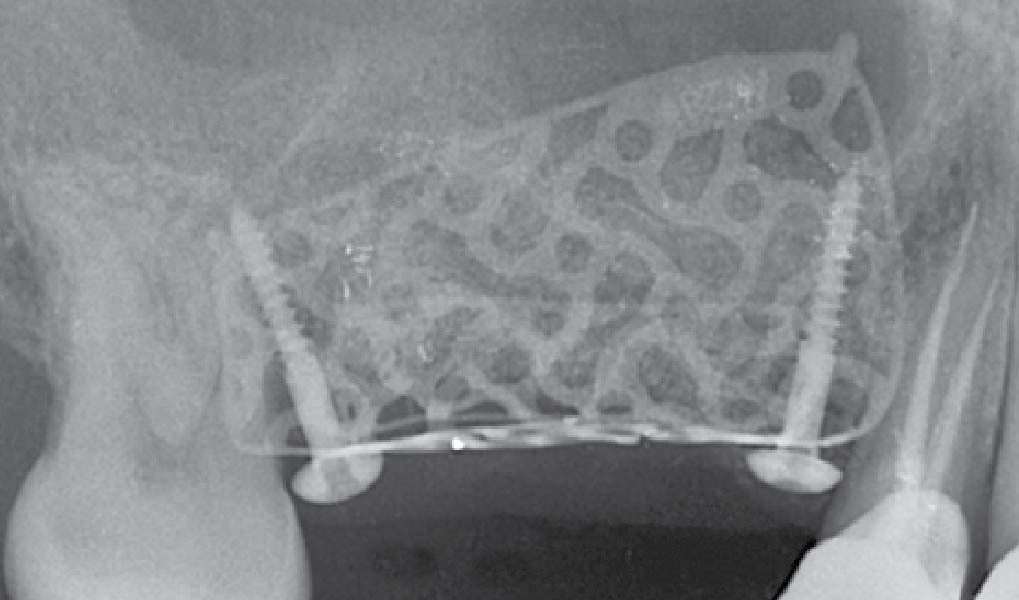
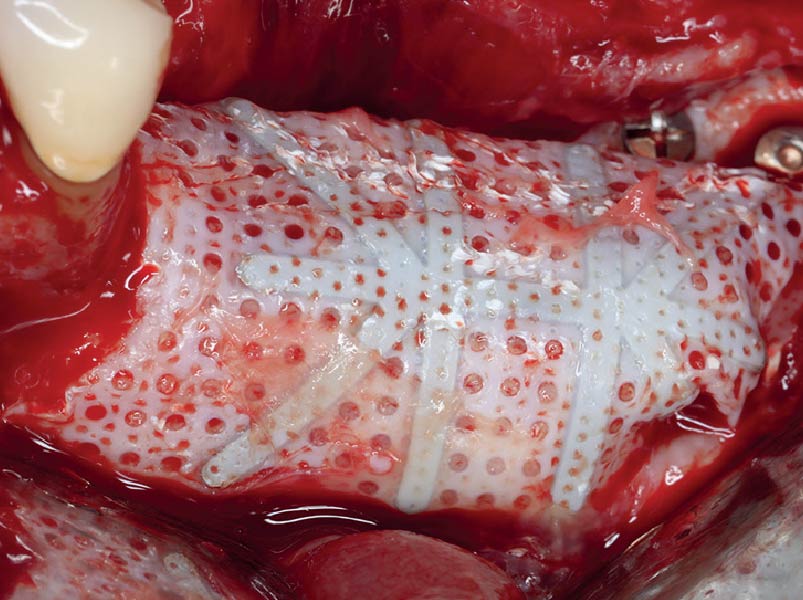
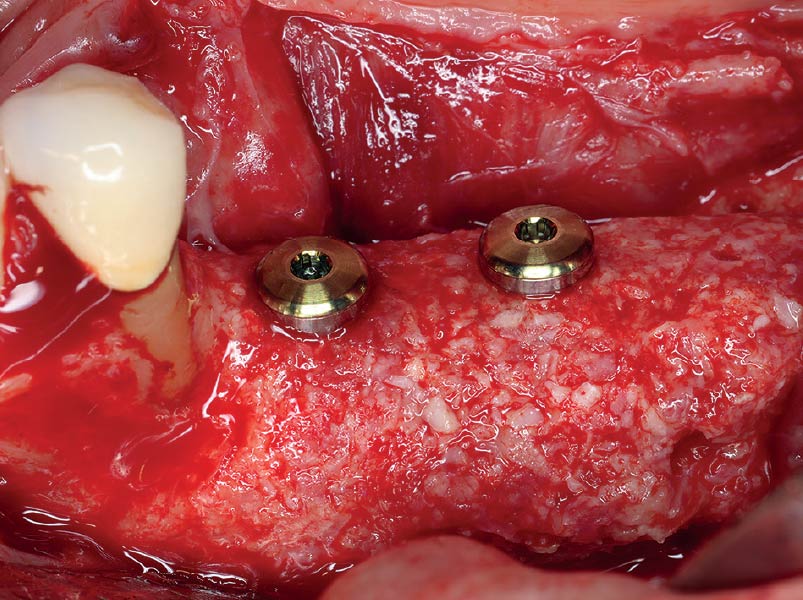
The goal of this procedure was to regenerate sufficient bone to place restoratively driven dental implants. Due to the horizontal and vertical ridge deficiency, we used a customized titanium mesh to predictably achieve this outcome.
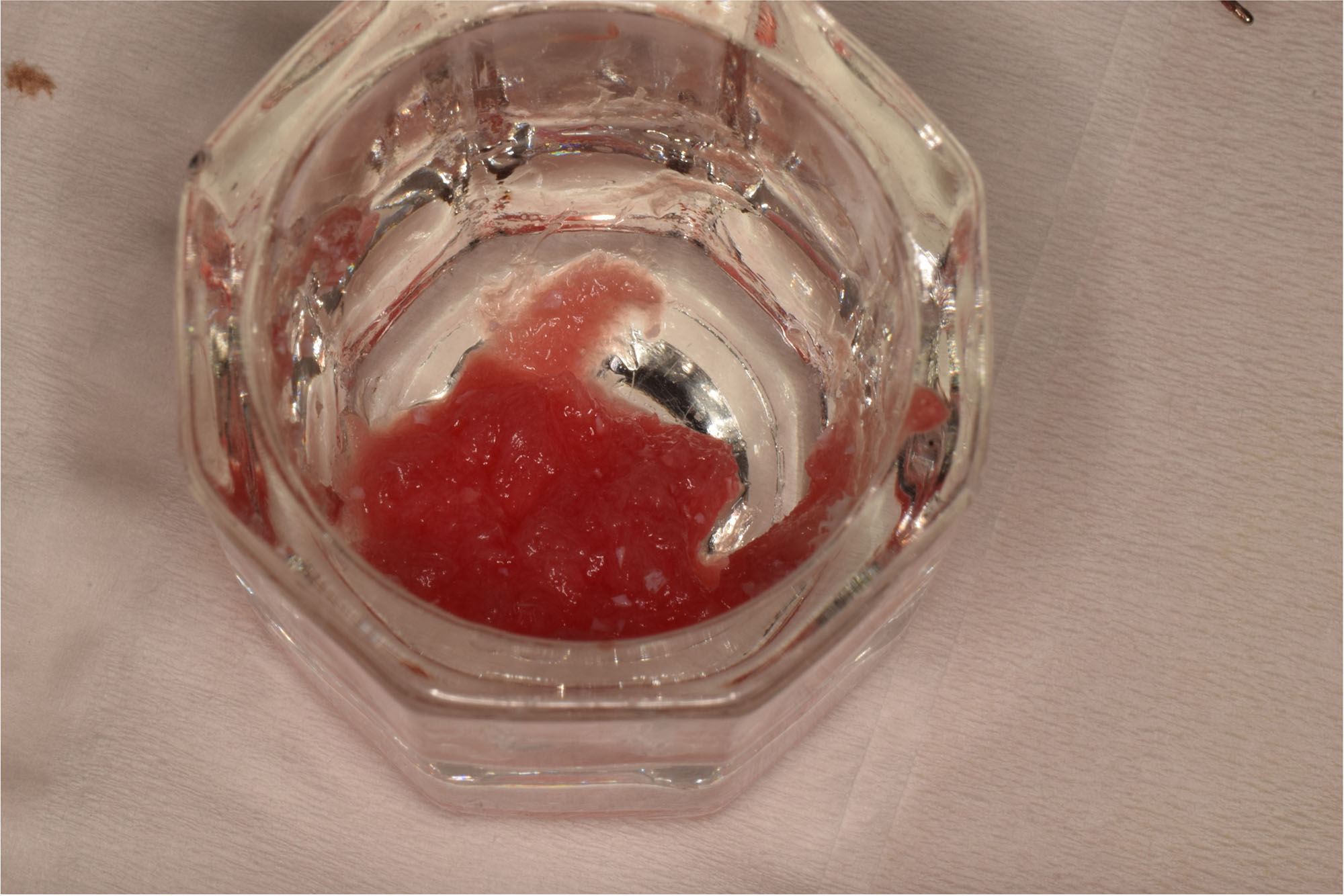
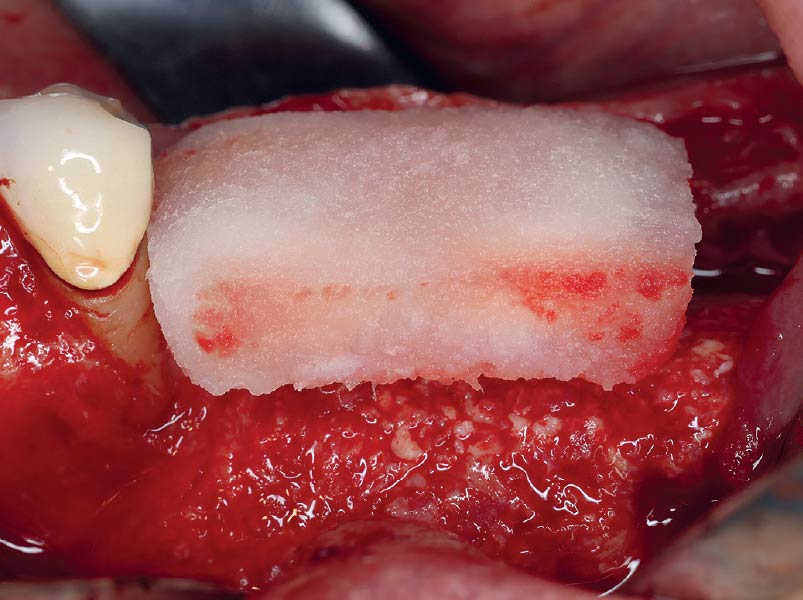
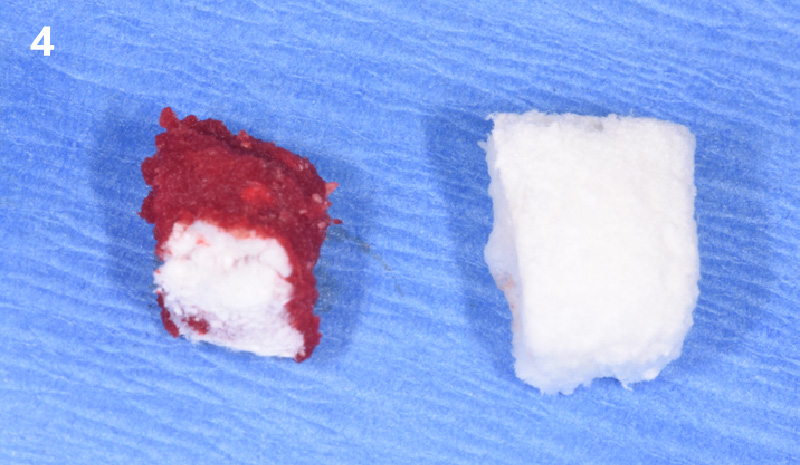
Autogenous bone collected with SafeScraper Twist and Geistlich Bio-Oss® filled the Yxoss CBR® Protect and a Geistlich Bio-Gide® collagen membrane covered the mesh.
.
“Success in these cases primarily depends on proper mesh design and careful handling of soft tissue to ensure zero-tension primary closure.”
— Shaun R. Young, DMD
THE OUTCOME
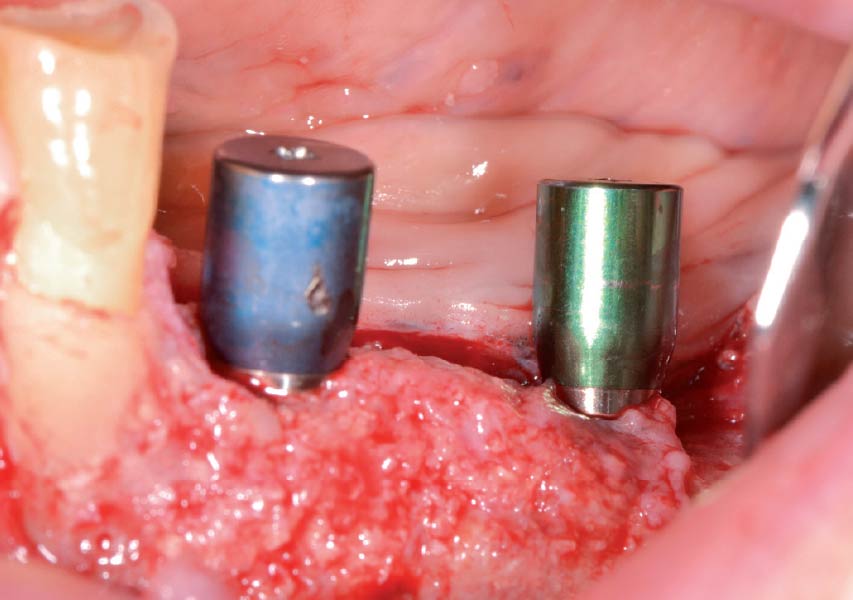
A left mandibular ridge deficiency was corrected using a Yxoss CBR® Protect Customized Bone Regeneration Titanium Mesh, designed from the patient’s CBCT scan.


Shaun R. Young, DMD
Dr. Shaun Young, an Oral and Maxillofacial Surgeon based in Tampa, Florida, specializes in complex ridge augmentation, immediate implants, and All-on-X full arch rehabilitation. He earned his Doctor of Dental Medicine degree from the University of Florida and completed his OMFS residency at Emory University in Atlanta, Georgia, where he served as Administrative Chief Resident. Dr. Young brings his expertise to a full-scope group practice, serving Tampa, Clearwater, and New Port Richey, Florida.
Sorry, you do not have permission to view this content.

BIOBRIEF
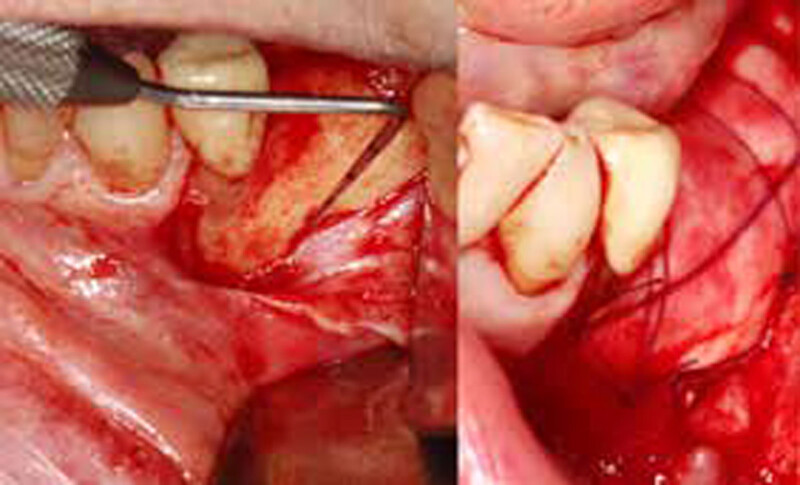
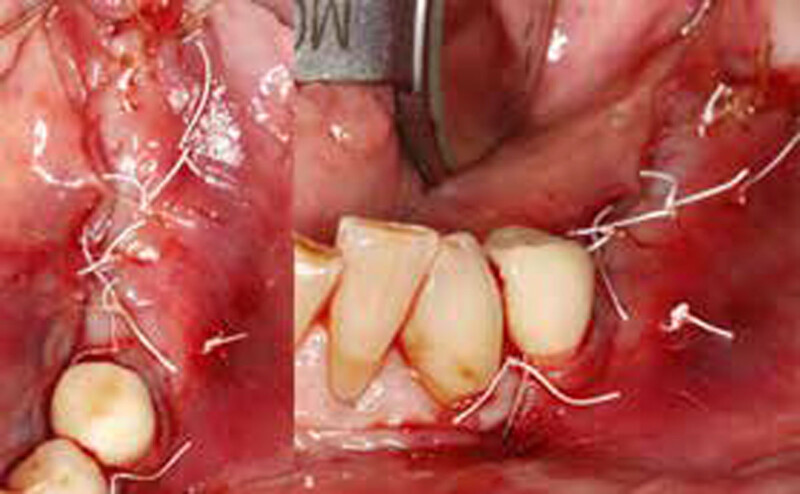
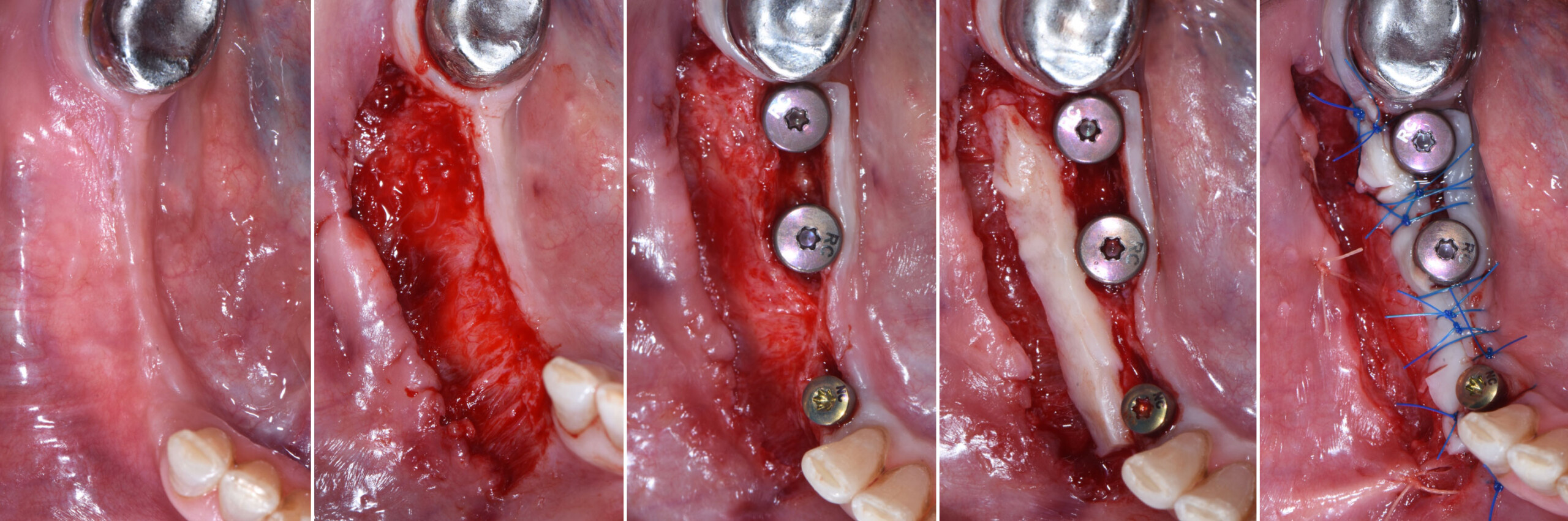
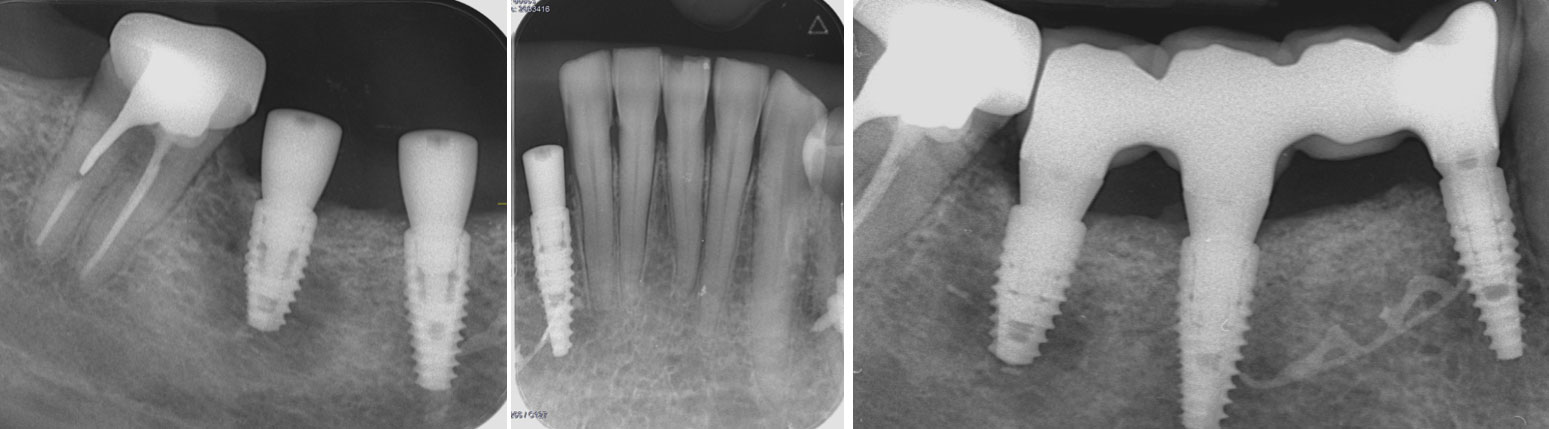
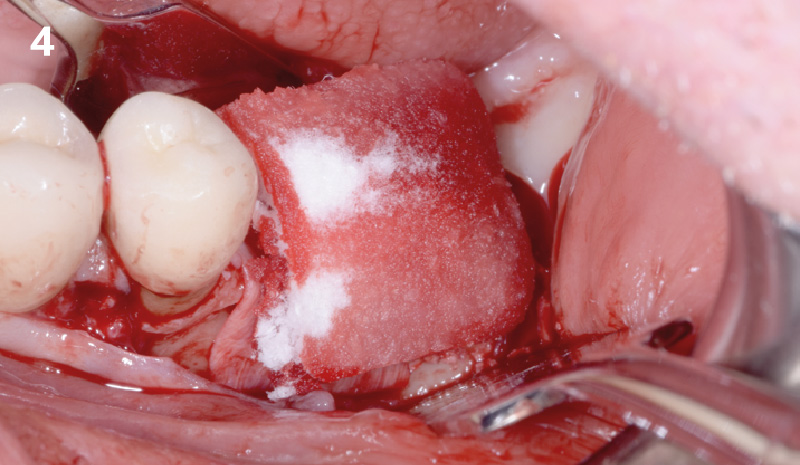
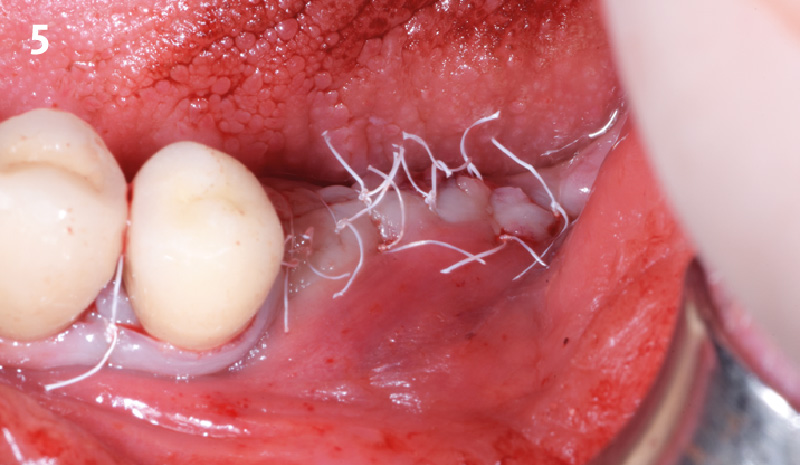
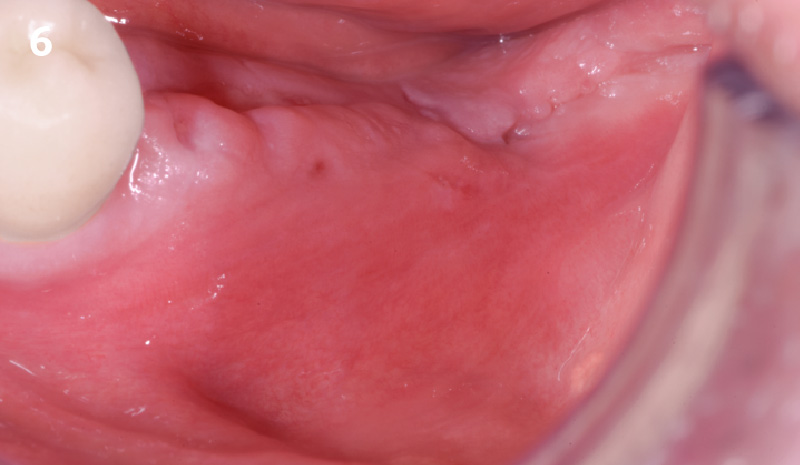
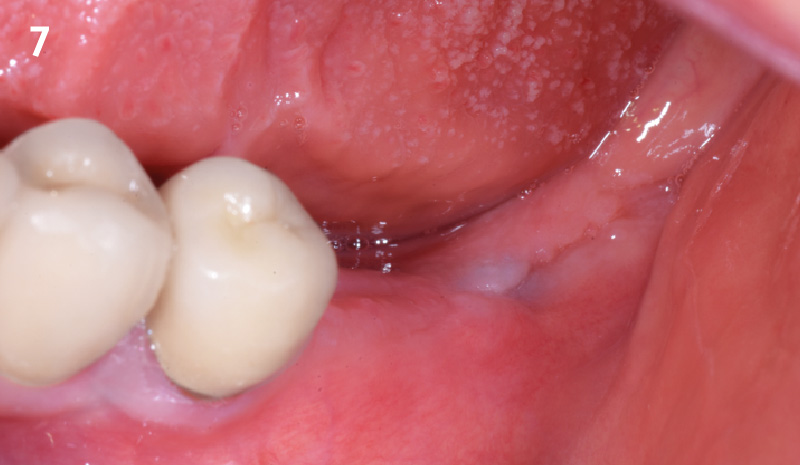
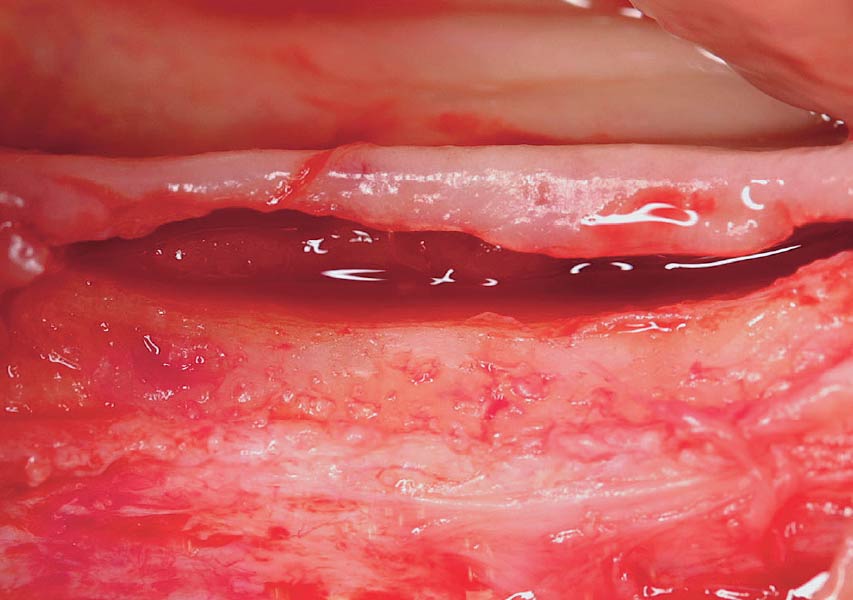
Mandibular Alveolar Ridge Split with Delayed Implant Placement


THE SITUATION
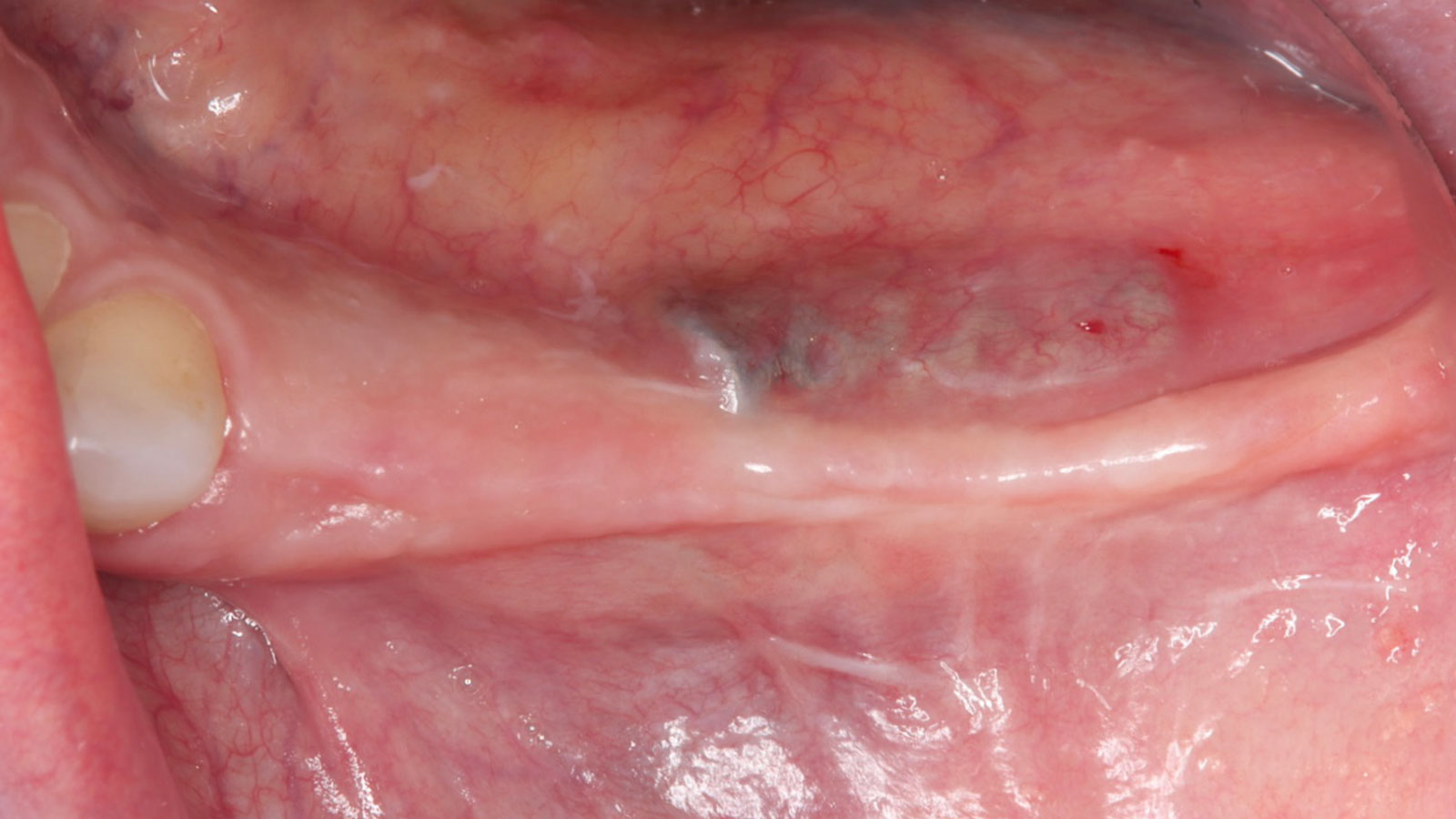
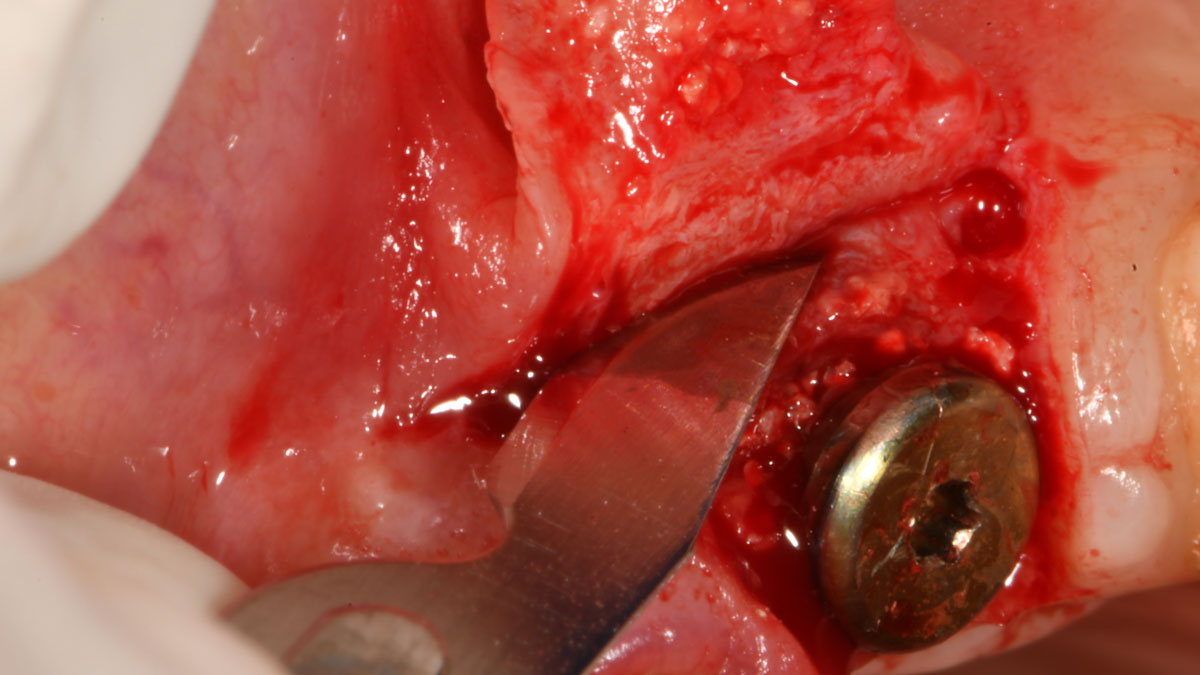
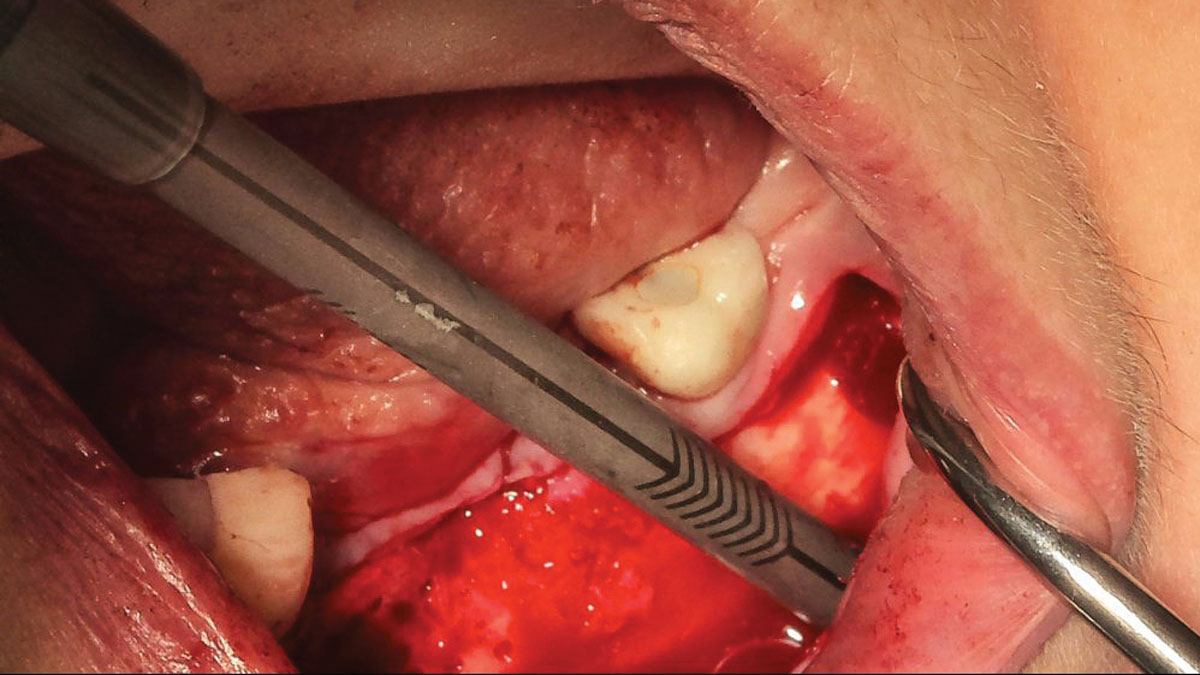
A healthy (ASA 1) non-smoker 63-year-old female presented to my office with Kennedy Class II partial edentulism in the mandibular right posterior quadrant for several years. She denied removable options and wanted dental implants to individually replace her missing teeth. The clinical and radiographic evaluation revealed atrophic mandibular bone height and width at site #’s 29, 30 & 31. The edentulous site required engineering prior to the placement of conventional dental implants and prosthetics.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system/Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
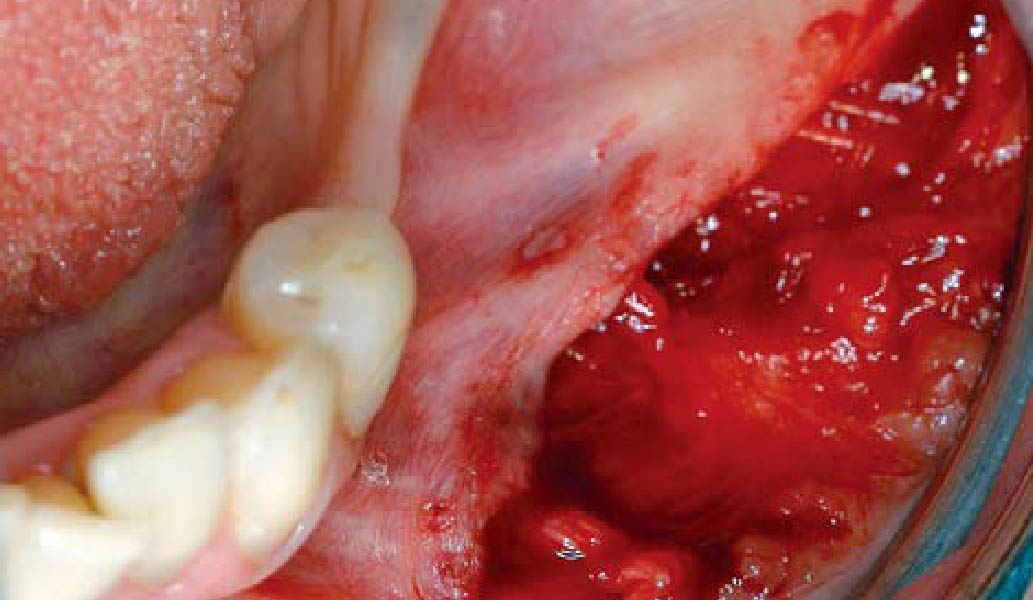
THE APPROACH
The goal is to provide adequate soft and hard tissue at edentulous site #’s 29, 30 & 31 in order to place dental implants and restore a stable balanced occlusion.
“The hard and soft tissue of the edentulous posterior mandible were inadequate to rehabilitate with dental implants.”
— Dr. Gregory Santarelli
THE OUTCOME
The patient summarized this challenging case very well – “I never imagined I would have fixed teeth again.” Geistlich Bio-Oss® and Geistlich Mucograft® allowed for retention of the hard and soft tissue volume to achieve our final result and for maintenance of the final prosthesis.


Gregory A. Santarelli, DDS
Dr. Santarelli earned his DDS degree in 1998 from the University School of Dentistry, Milwaukee, WI, after graduating with his B.S. in Biology from Arizona State University (Tempe, AZ). In 1999, he completed his General Practice Residency at the University of Iowa Hospital and Clinics, and went on to an Oral & Maxillofacial Surgery Internship at the Medical College of Virginia (Richmond, VA) as well as an Oral & Maxillofacial Surgery Residency Program, Christiana Care Health System (Wilmington, DE).
After completing his formal training in 2004, Dr. Santarelli’s work experience includes the Bankor Hospital for Children, Cambodia (2003), Adjunct Clinical Professor, University of Marquette, School of Dentistry, Department of Oral Sugery, Marquette, WI (2005), and Oral Surgery Associates of Milwaukee, Milwaukee, WI (2004-2005). He now maintains a private practice in Kenosha, WI with his partner Dr. Deno Tiboris.
Dr. Santarelli performs numerous hard/soft tissue regeneration surgeries in preparation for dental implants and is actively involved in clinical research with The McGuire Institute (iMc).

BIOBRIEF
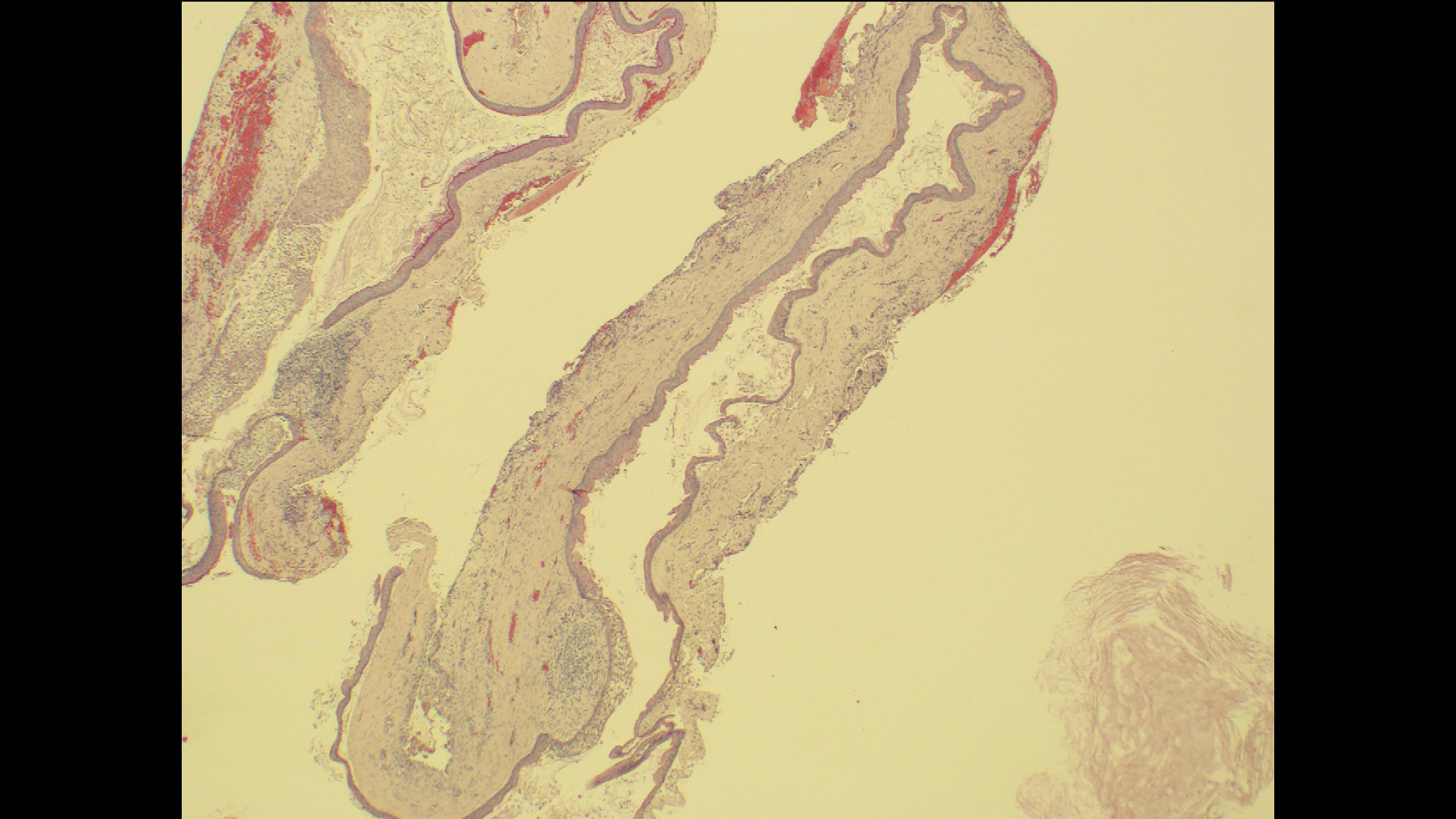
Odontogenic Keratocyst Management


THE SITUATION
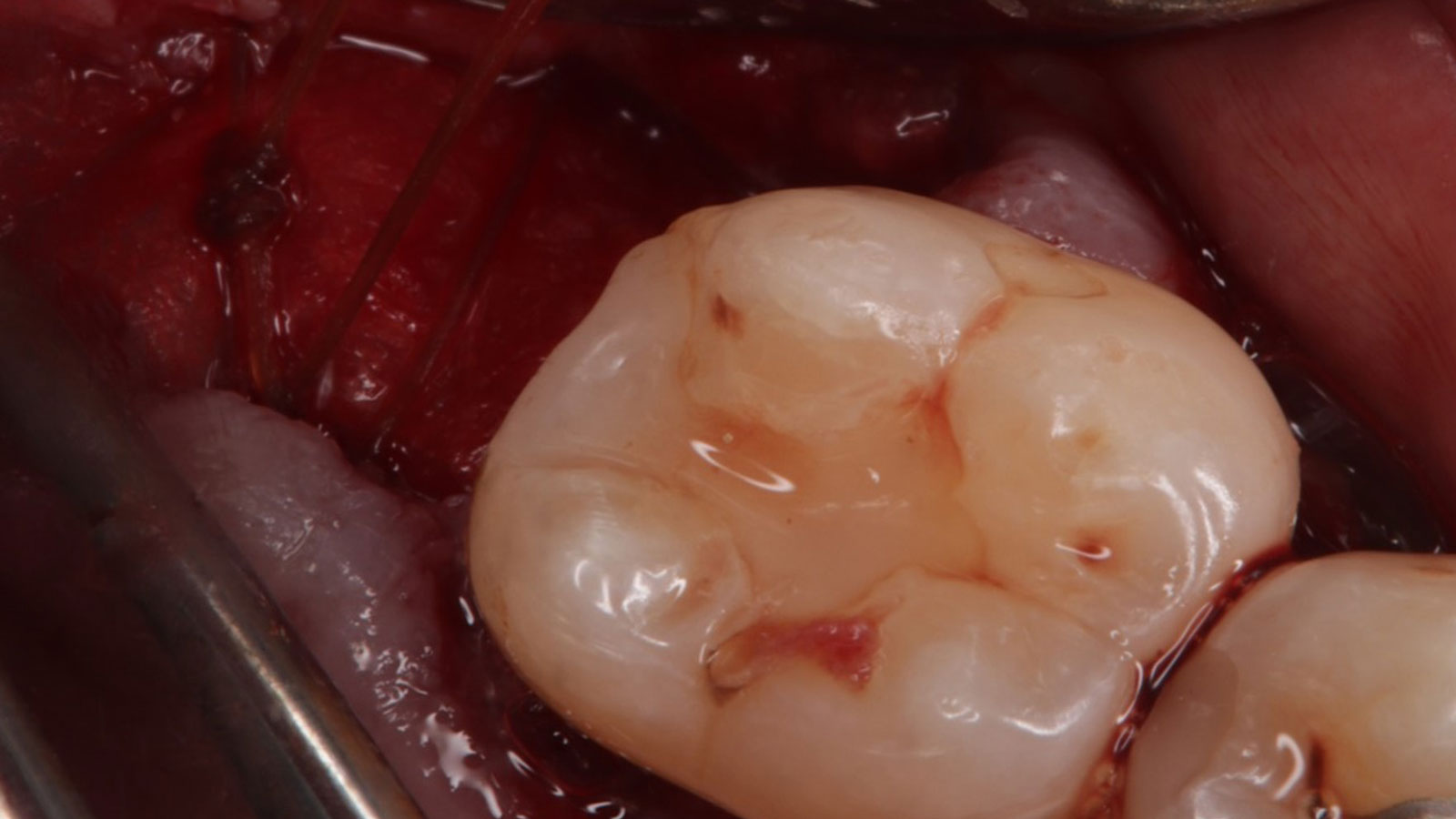
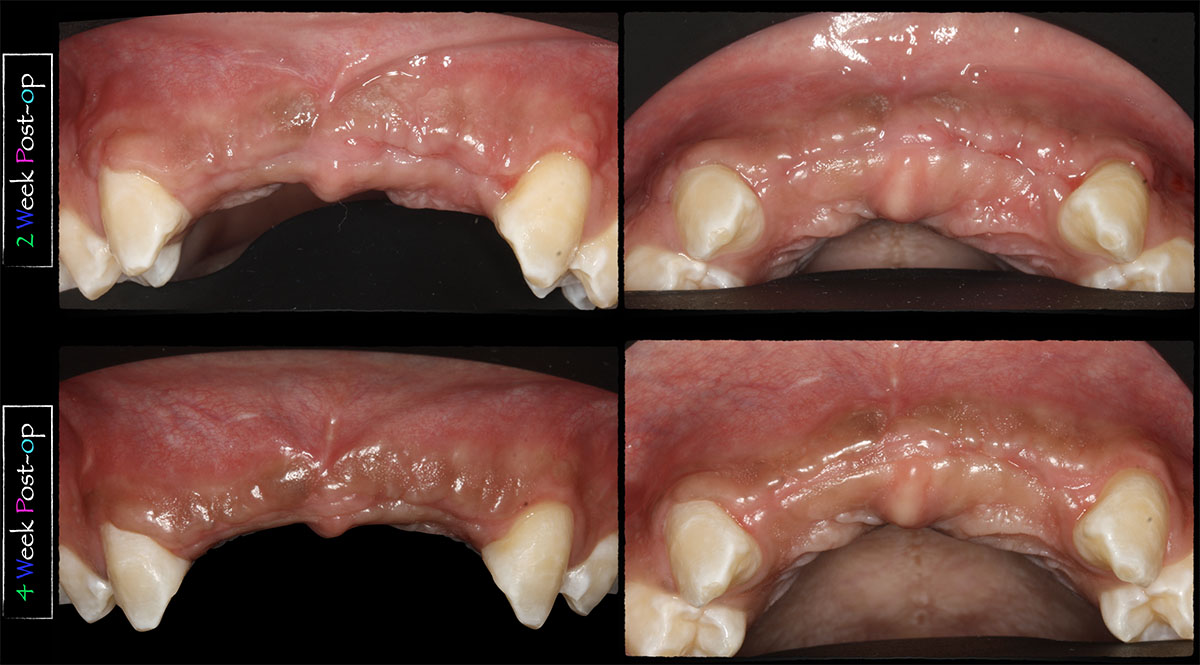
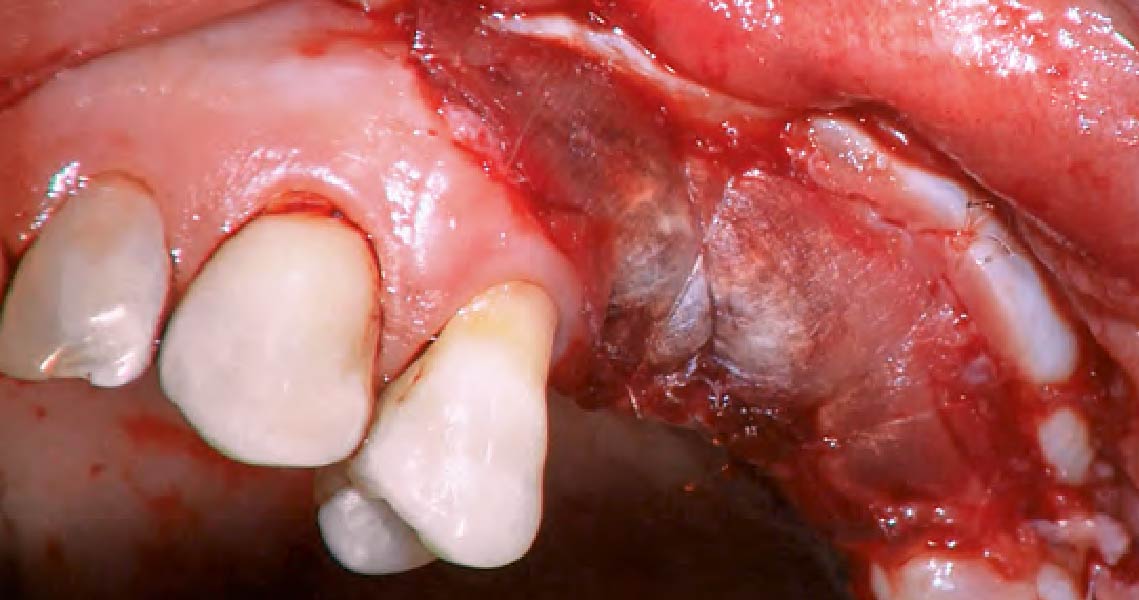
A 60-year-old-heathy Caucasian female presented with the chief complaint: “I noticed a bump on my lower left teeth since last year.” An examination revealed a stable periodontium except for enlarged gingival tissue between #21-22 measuring 10x8x5mm, well-defined borders, depressible, non-painful, and vital teeth without displacement. The treatment plan included flap surgery, excisional biopsy, GTR #21-22 (Diff Dx: Lateral periodontal cyst (LPC), Odontogenic Keratocyst (OKC), Benign Fibro-Osseous lesion (BFOL).
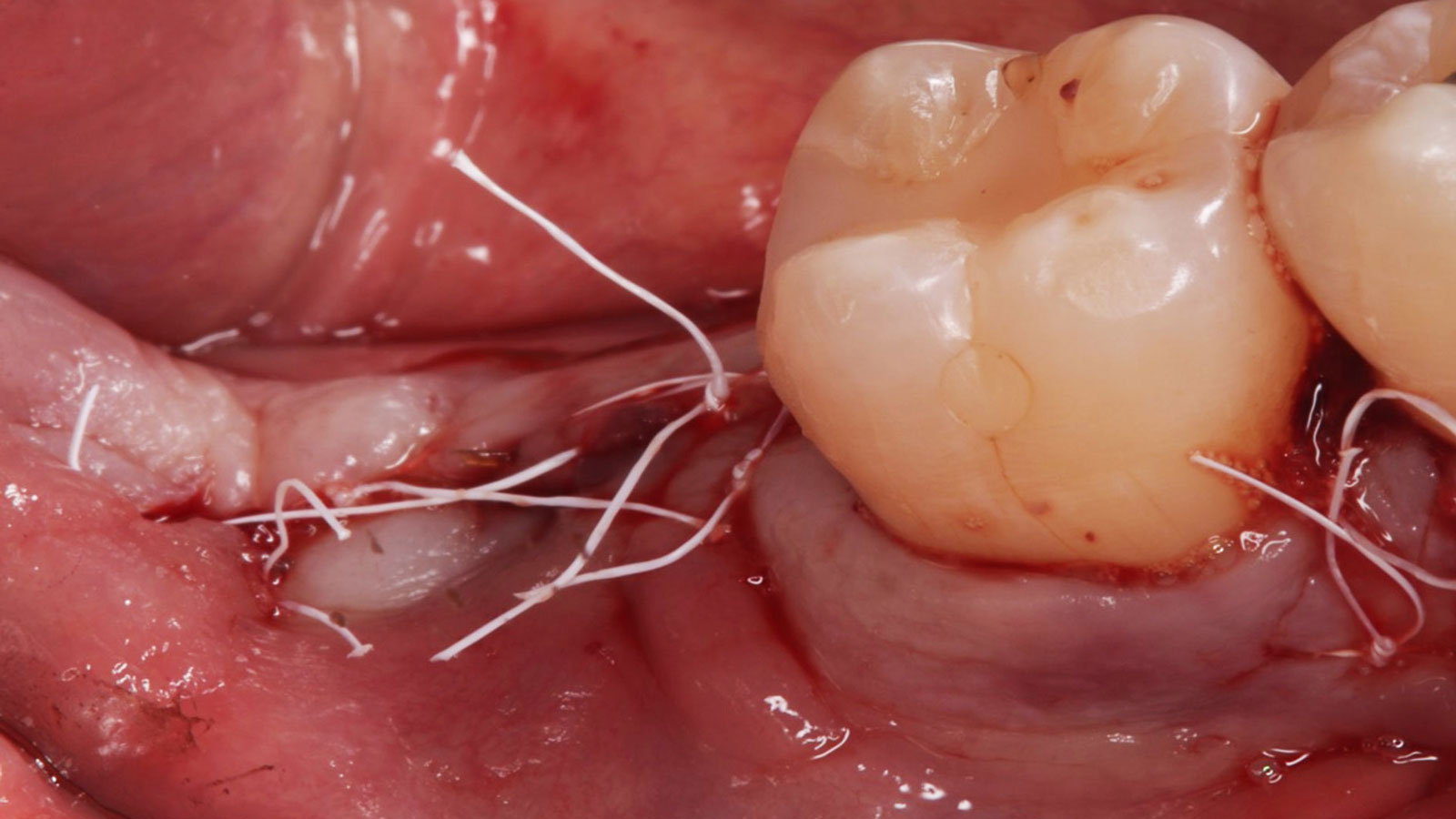
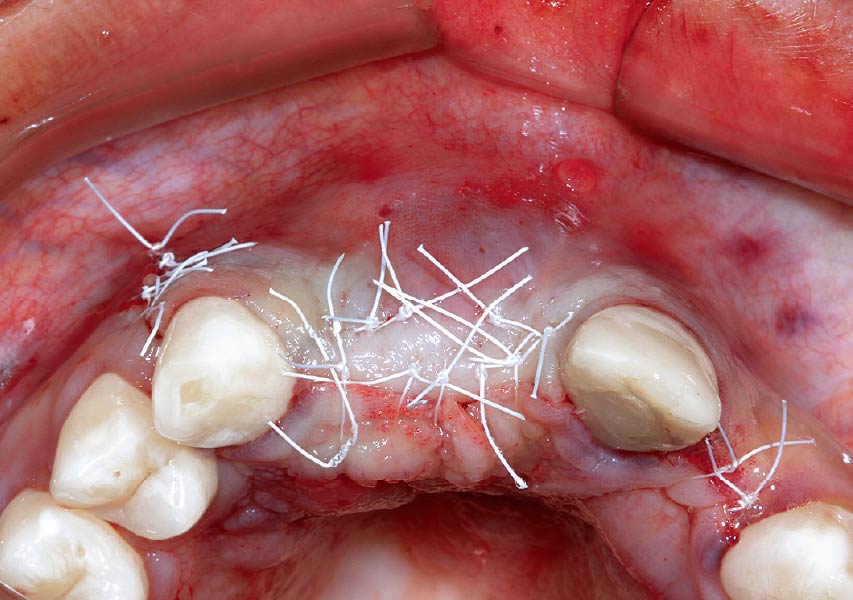
Guided Tissue Regeneration (GTR) using Geistlich Bio-Oss® and vallos®f was performed and covered with a resorbable collagen membrane (Geistlich Bio-Gide®).
Primary closure was completed using non-resorbable sutures. Follow-up at 2, 4 weeks, 3, 6 months showed stable periodontium without re-occurrence. The pathology report indicated OKC and the area is monitored annually.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The treatment goal was to excise the lesion around #21-22 and stabilize the periodontium. Sulcular incisions #20-22 with vertical incision #22 MF were performed. Upon full thickness flap reflection, the lesion was removed (excisional biopsy). The defect extended #21M-#22D with complete facial bone loss. It was a wide 1-2 bony wall defect measuring 10x8x5mm. GTR procedure using Geistlich Bio-Oss® and vallos®f and Geistlich Bio-Gide® for the collagen membrane were employed. Primary closure was obtained using 6-0 prolene suture.
“Excisional biopsy and guided tissue regeneration is indicated to treat the pathology (#21-22 area) and stabilize the periodontium.”
— Dr. Bassam Kinaia
THE OUTCOME
Complete excision of pathology and biopsy followed by GTR using vallos®f internally for maximum osteogenic/osteoinductive potential and Geistlich BioOss® externally for space maintenance showed excellent radiographic bone fill and stable periodontium.


Bassam Kinaia, DDS, MS, DICOI
Dr. Kinaia is the Associate Director of the Graduate Periodontology Program at the University of Detroit Mercy (UDM). He is also the former Director of the Periodontology Program at UDM in Michigan and Boston University Institute for Dental Research and Education in Dubai. He is a Diplomate of the American Academy of Periodontology (AAP) and International Congress of Oral Implantology (ICOI). He received a certificate of Excellence from the AAP in recognition of teaching-research fellowship.

BIOBRIEF
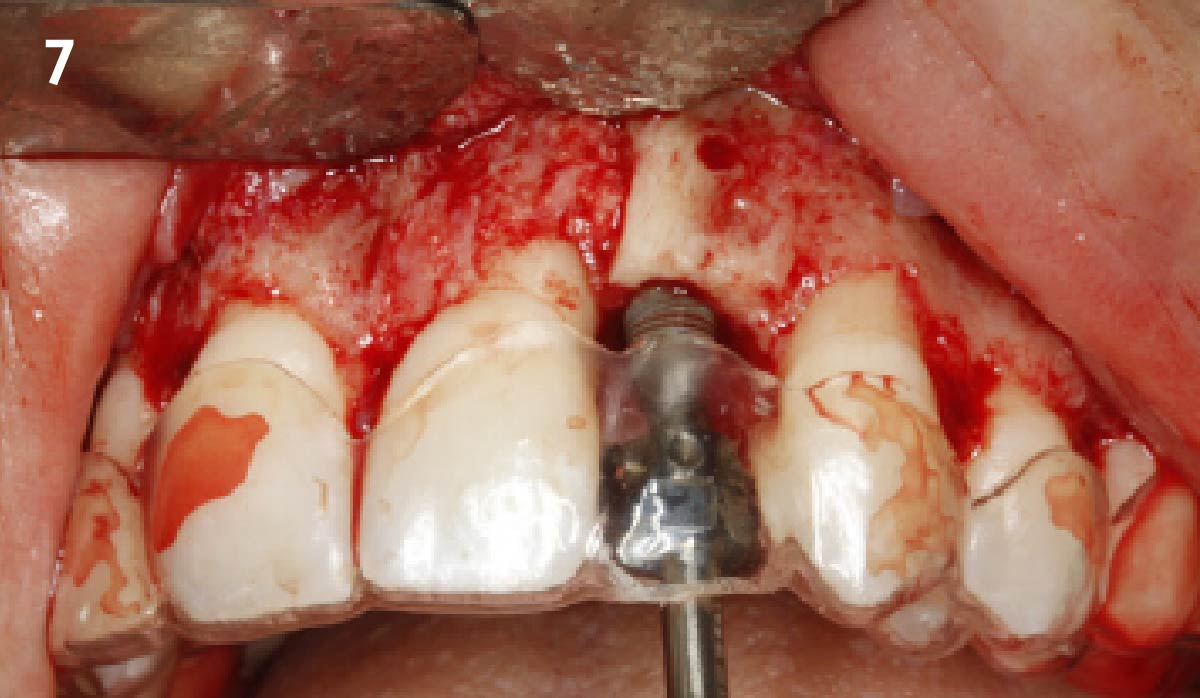
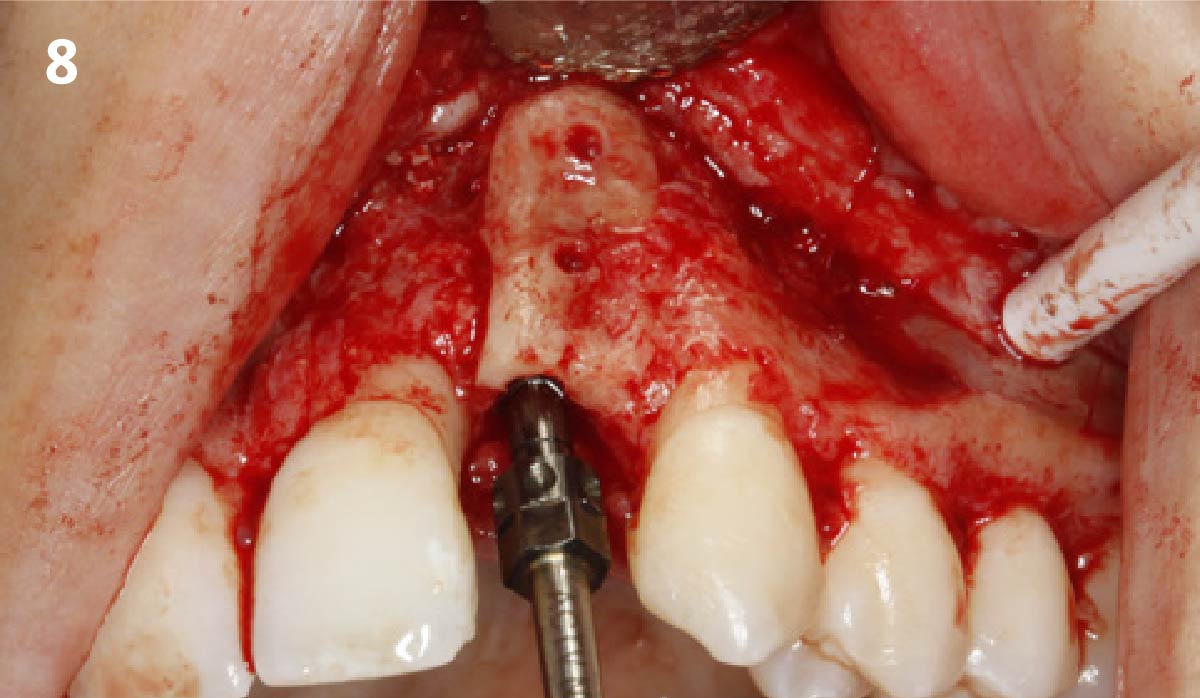
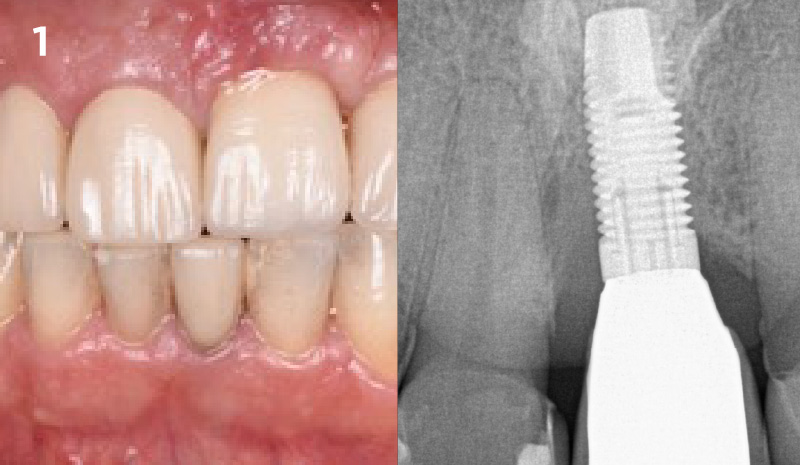
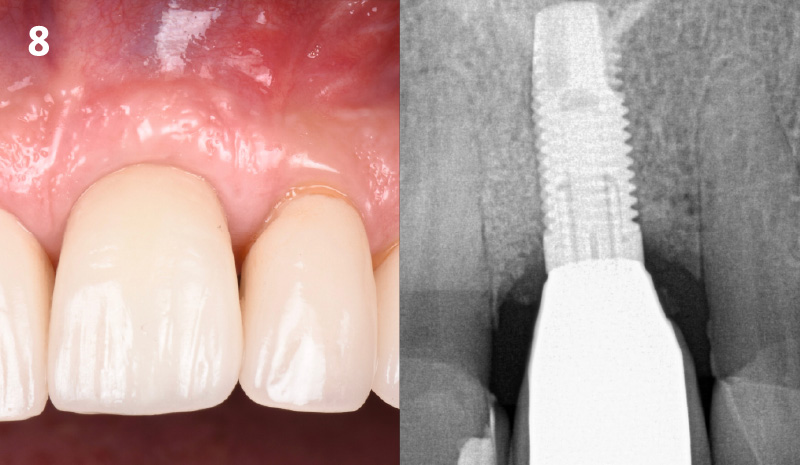
The Buccal Pedicle Flap for Peri-Implant Soft Tissue Volume


THE SITUATION
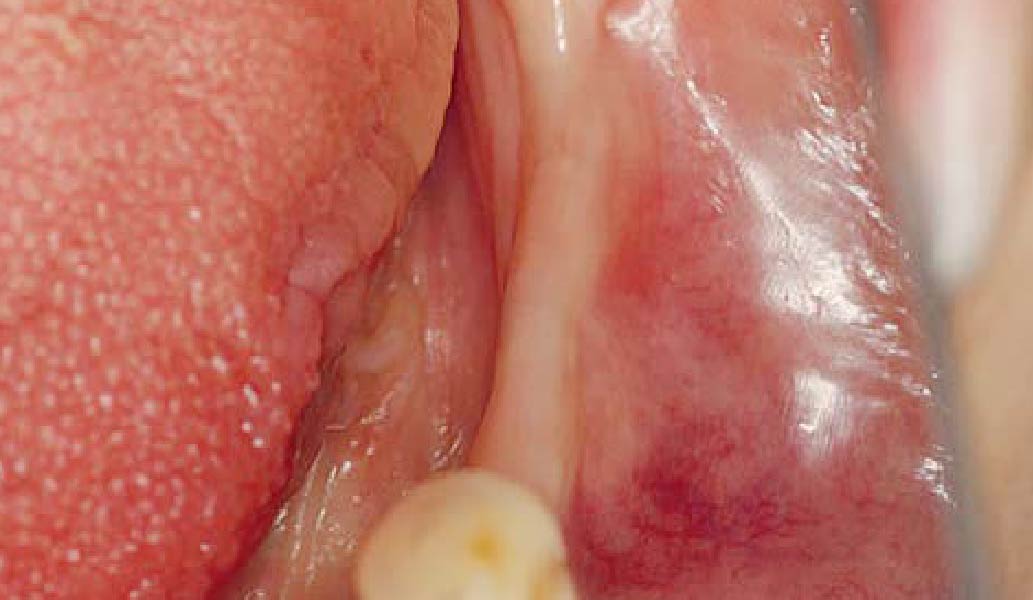
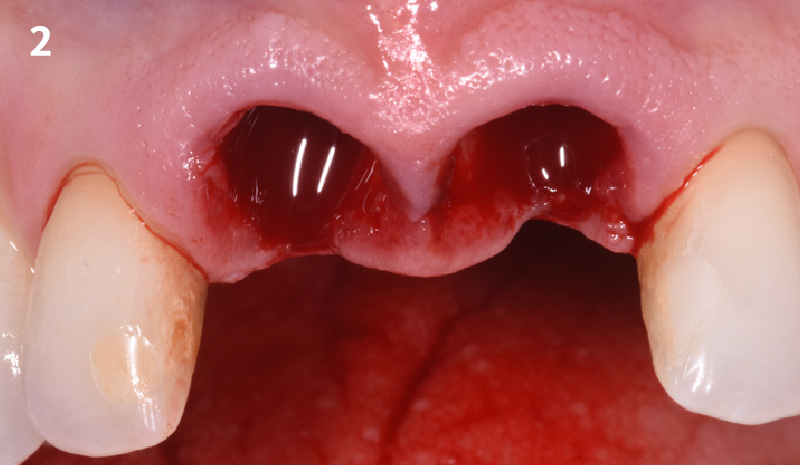
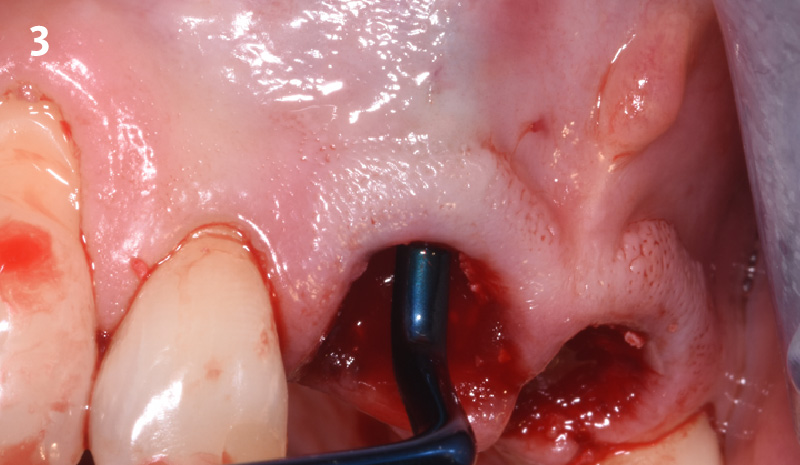
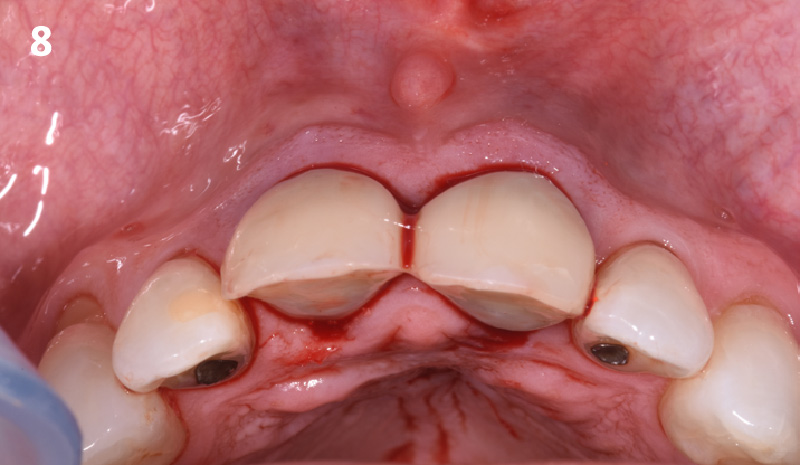
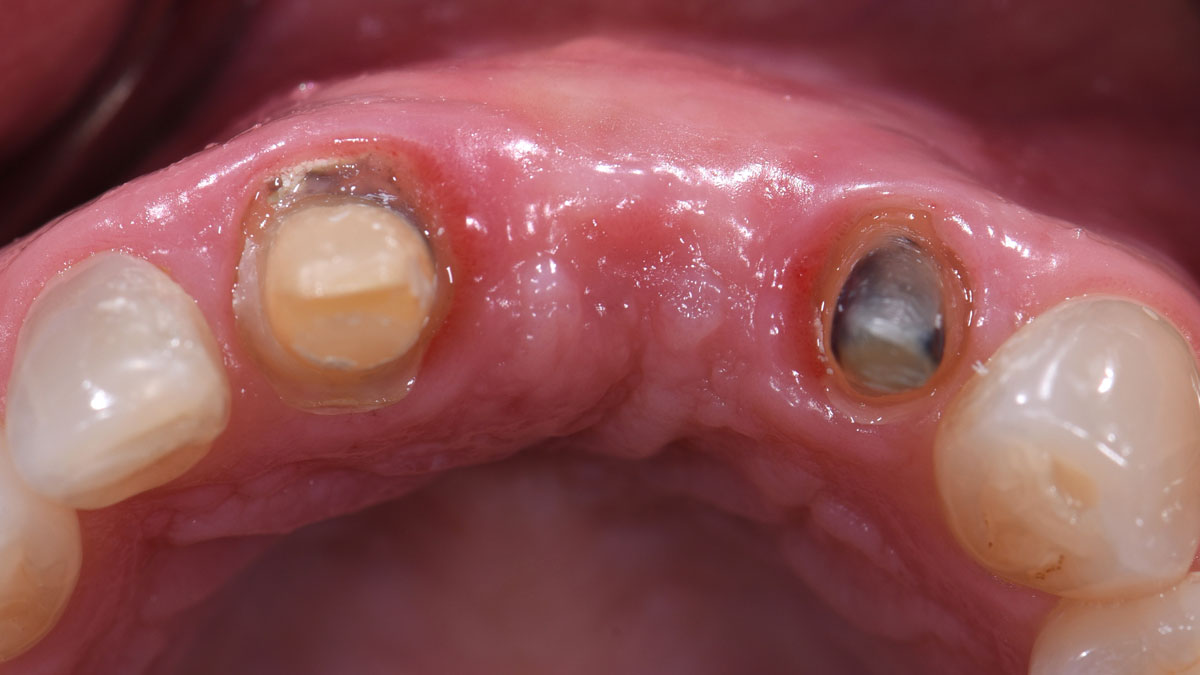
Patient presented with a fistula buccal on tooth #9 associated with a chronic peri-apical lesion and external root resorption. Also tooth #8 showed a chronic peri-apical lesion. Her chief complaint was the misalignment of her teeth. The clinical situation revealed the presence of bleeding upon probing and generalized moderate periodontal disease (Stage II, Grade I) as well as multiple endodontic failures.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The aim of the treatment is to eradicate periodontal disease and restore esthetics and function. Treatment planning: non-surgical and surgical periodontal treatment, orthodontic alignment, extraction of both central incisors, immediate implant placement and Guided Bone Regeneration with Geistlich Bio-Oss®, peri-implant soft tissue boosting with a buccal pedicle flap and full ceramic CAD-CAM restorations.
“Orthodontic treatment must be postponed because of the presence of periodontal disease. A thin biotype and a high smile line needs to be taken into consideration.”
THE OUTCOME
The final outcome at 8 weeks is showing pink esthetics as well as biomimetics and function. The use of the buccal pedicle flap allowed the increased volume of the peri-implant mucosa with a minimally invasive approach. The combination of Geistlich Fibro-Gide® and a buccal pedicle flap had the main advantage of reducing the morbidity generally associated with CT harvesting.


Dr. Giorgio Tabanella
Dr. Tabanella is a Diplomate of the American Board of Periodontology, an Active Member of the Italian Academy of Esthetic Dentistry and author of the book “Retreatment of Failures in Dental Medicine”. He graduated from the University of Southern California, Los Angeles, USA where he obtained his Certificate in Periodontics as well as a Master of Science in Craniofacial Biology. He is Director of O.R.E.C. – Oral Reconstruction and Education Center (www.tabanellaorec.com), reviewer and author of original articles.

BIOBRIEF
Successful Implant Placement and Horizontal Augmentation for Bilateral Congenitally Missing Maxillary Incisors


THE SITUATION
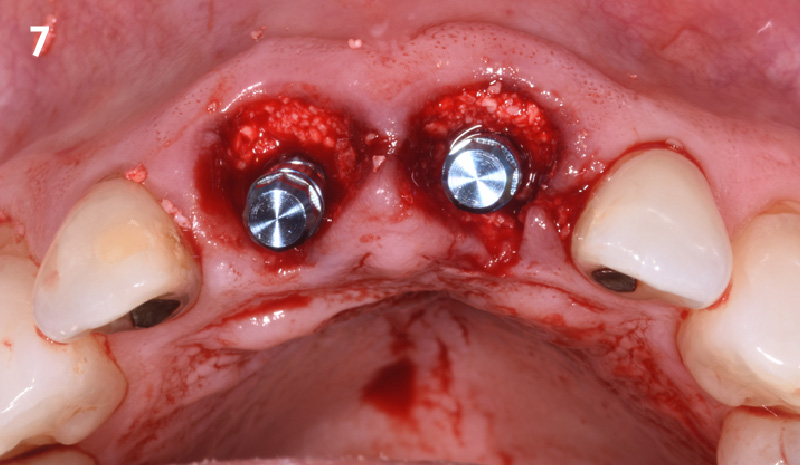
A 30-year-old male patient was referred to me with bilateral congenitally missing lateral incisors in the maxilla. The referring general dentist had previously made a resin-bonded bridge which was successful for a few years but had frequent debondings. Clinical examination revealed lack of ridge contour but the CBCT revealed existence of adequate width for placement of narrow-diameter implants with additional bone grafting and contour augmentation. The existing bone anatomy precluded placement of implants for screw-retained restorations without a pre-surgical lateral ridge augmentation procedure. The patient accepted a treatment plan for placement of two narrow-diameter implants and simultaneous bone grafting and contour augmentation followed by restoration with zirconia cement-retained crowns.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Compromised | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
My treatment goals were to preserve the existing soft-tissue architecture, especially the interdental papilla, mesial and distal to the lateral incisors, improve the facial contour at the lateral incisor sites by bone grafting with a low substitution biomaterial, and harmonize esthetics and function with optimal implant-supported restorations.
“The patient had failed resin-bonded bridges with deficient contours for bilateral congenitally missing lateral incisors.”
THE OUTCOME
Single-stage implant placement with bilateral papilla-sparing incision design and simultaneous contour augmentation using a mixture of Geistlich Bio-Oss® autologous bone chips and Geistlich Bio-Gide®.


Dr. Avinash Bidra
Dr. Bidra is a Board Certified Maxillofacial Prosthodontist and Director of the Prosthodontics Residency Program at UCONN School of Dental Medicine. He has extensive surgical experience and maintains a part-time private practice restricted to Implant Surgery and Prosthodontics in Meriden, CT. He has lectured at national and international meetings, as well as published extensively in international scientific journals. He has invented prosthetic components and is a co-inventor of a new implant design.

BIOBRIEF
Horizontal Ridge Augmentation in the Posterior Mandible of a 90-Year-Old Female

THE SITUATION
A 90-year-old female presented requesting dental implants be placed in the left mandibular posterior region. Her chief complaint was increased drooling and difficulty chewing on only one side. She lost her bridge one year prior to her visit and firmly stated that she did not want to wear a partial denture. The clinical exam and CBCT showed that there was a horizontal alveolar ridge deficiency that precluded the implants from being placed in a restoratively desirably position. Therefore, a horizontal ridge augmentation was done using multiple layers of Geistlich Bio-Gide® Compressed over a 1:1 ratio of autogenous bone and Geistlich Bio-Oss® xenograft.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The treatment goal was to gain adequate horizontal bone dimension to allow for prosthetically-driven implant placement. Guided bone regeneration was performed in which autogenous bone was mixed with Geistlich Bio-Oss® xenograft in a 1:1 ratio. PRF was used to create “sticky bone” and was covered by multiple layers of Geistlich Bio-Gide® Compressed. The membrane was stabilized with periosteal biting stabilizing sutures. Tension-free primary closure was achieved and the grafted site was allowed to heal for 8 months prior to the implant surgery for #19 and #20.
“A predictable ridge augmentation procedure was needed to help our 90-year-old patient avoid having nutritional deficiencies due to lack of proper chewing ability and also to improve her quality of life.”
THE OUTCOME
The horizontal ridge augmentation procedure resulted in adequate bone for implant therapy as evidenced by the CBCT scan and re-entry surgery. With a sufficient quantity of good quality regenerated bone, implants for #19 and #20 were placed using a surgical guide based on a diagnostic wax up. Our 90-year-old patient is very happy to be able to chew efficiently again.

Dr. John Kim
Dr. Kim, originally from Fairfax, VA, received his DMD from Harvard School of Dental Medicine. He completed his residency and received his M.S. in Periodontics at UNC School of Dentistry at Chapel Hill. Dr. Kim is a Diplomate of the American Board of Periodontology and actively speaks as an expert on guided bone regeneration, implant therapy, soft tissue grafting, and managing complications domestically and internationally. He is also an adjunct faculty at UNC Adams School of Dentistry.

BIOBRIEF
Horizontal Ridge Augmentation in the Esthetic Zone


THE SITUATION
An adult female patient presented with a long history of edentulism at site #9. Patient was interested in replacing her missing tooth with a dental implant, and was wearing a Nesbit appliance. The irritation from the ill-fitting Nesbit appliance resulted in irregular and friable soft-tissue at site #9.
Pre-operative CBCT demonstrated a hard-tissue concavity apical to the crest of the bone. The primary goal of therapy was to regain horizontal dimension of hard and soft-tissue to achieve prosthetically-driven placement of a dental implant to replace the patient‘s left central incisor.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The treatment goal was to regain the horizontal dimension of hard and soft-tissue through guided bone regeneration. In coordination with the restoring dentist, a diagnostic wax up was completed to determine the ideal tooth position and to regain mutually protected occlusion on the patient’s left side. The combination of Geistlich Bio-Oss® and autologous bone chips was used along with Geistlich Bio-Gide® to regenerate the horizontal dimension for prosthetically-driven implant placement.
“Patient with a long history of partial edentulism was seeking a long-term, predictable restorative option to replace her missing left central incisor.”
THE OUTCOME
Adequate hard and soft-tissue architecture was restored with the use of Geistlich Bio-Oss® and Geistlich Bio-Gide® for predictable, prosthetically-driven implant placement. The combination of Geistlich Bio-Oss® and autologous bone chips provides the best chance for regeneration while maintaining the hard and soft-tissue contours.

Dr. Justin Kang
Dr. Justin Kang received his Doctor of Dental Medicine degree from University of Pennsylvania School of Dental Medicine. He completed his residency and received his Masters of Science in Periodontics at Columbia University College of Dental Medicine. Dr. Kang is a Diplomate of the American Board of Periodontology and a member of numerous professional associations including the Academy of Osseointegration, American Dental Association and the New Jersey Dental Association.

BIOBRIEF
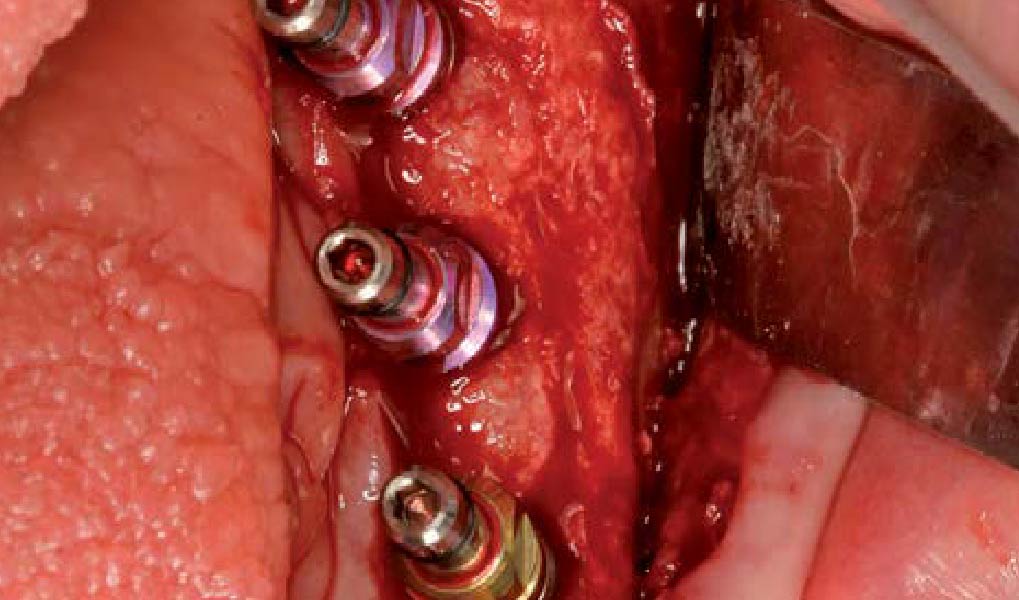
Lateral Ridge Augmentation in the Posterior Mandible

THE SITUATION
A 70-year-old female in good health presented with a fracture of tooth #19 which is the distal abutment for a four-unit bridge tooth #19-22, with pontics in the #20 and #21 positions. With the loss of the bridge, the patient desired a fixed prosthetic replacement. A bridge from tooth #22 to an implant placed at the #18 position was not deemed mechanically sound. She opted for implant placement at positions #19, #20 and #21 following lateral ridge augmentation with autogenous bone and Geistlich Bio-Oss® contained with a Geistlich Bio-Gide® membrane.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Compromised | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
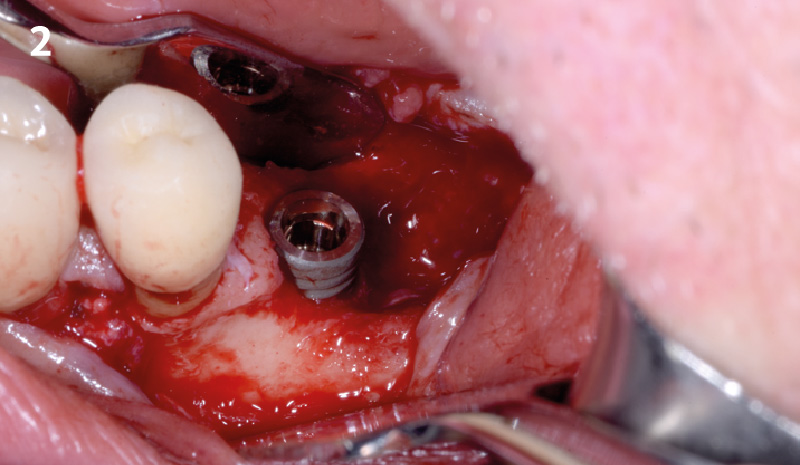
A subperiosteal flap with a mid-ridge incision was performed with anterior and posterior releasing incisions which were placed the distance of one tooth mesial and one tooth distal from the graft site. The posterior releasing incision allowed for exposure of the ramus for harvesting of the autologous bone. The grafted site was allowed to heal for a period of 8 months at which time the implants were placed. Abutment connection occurred 4 months following implant placement.
“A bone graft was required to augment the ridge, a CBCT scan was performed prior to surgery to determine bone volume and the amount of bone required to graft.”
THE OUTCOME
Following 8 months of healing, the augmented site showed sufficient bone width that was assessed with a CT scan. After examination, it was determined that the bone width was adequate for implant placement in the desired position to allow an esthetically pleasing and functional outcome for the patient.

Dr. John M. Sisto
Dr. John M. Sisto received his Doctorate in Dental Surgery degree from Loyola University and completed his residency and certification in Oral and Maxilofacial Surgery at the Cook County Hospital in Chicago. Dr. Sisto was the Director of Residency Education at Cook County Hospital from 1985 to 2010 and started the residency program in oral and maxillofacial surgery in 1990. He held teaching positions at both Northwestern and University of Illinois Dental schools as a clinical assistant professor, and also at Northwestern Medical School. He was the Division Chief of Oral and Maxillofacial Surgery at Cook County Hospital and Chairman of Dentistry at Resurrection Medical Center. Dr. Sisto has published papers on dental implant surgery, trauma surgery, orthognathic surgery and maxillofacial infections. He has lectured both locally and nationally at various educational forums.

BIOBRIEF
Combined Horizontal and Vertical Regeneration Using a CAD-CAM Titanium Scaffold


THE SITUATION
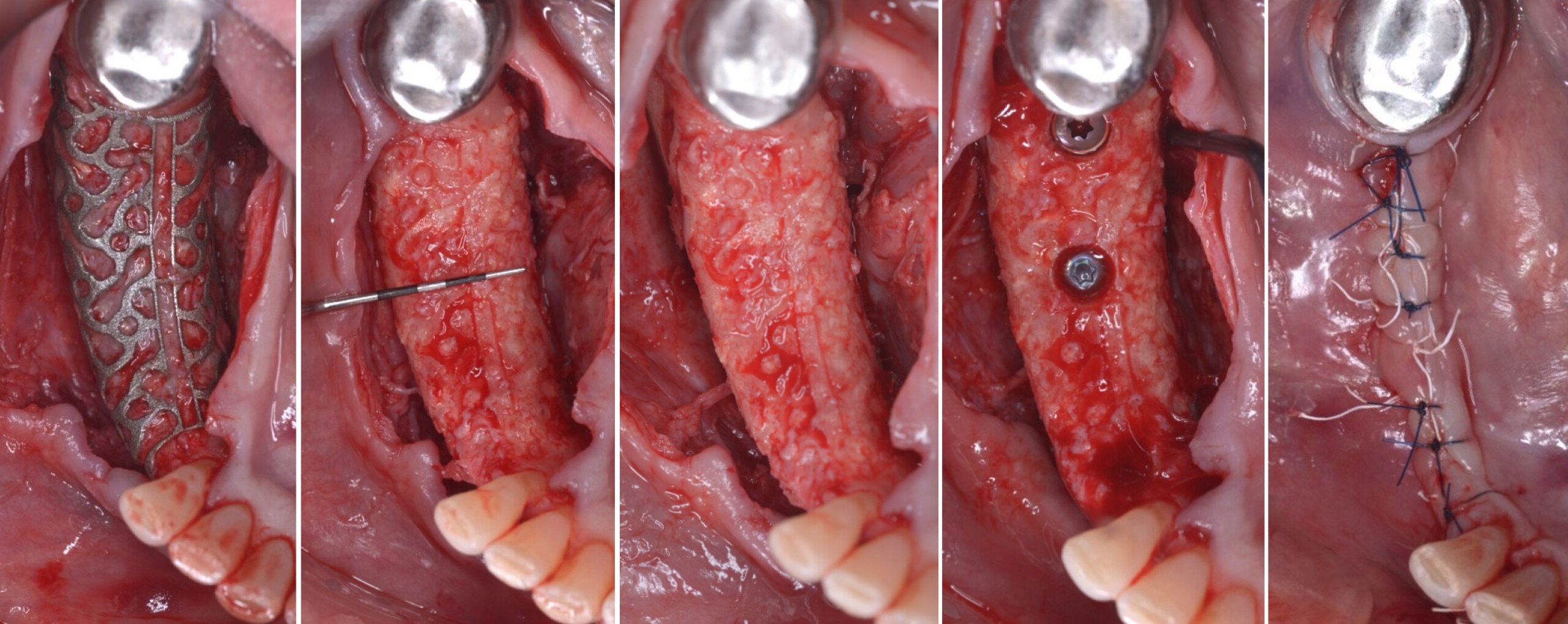
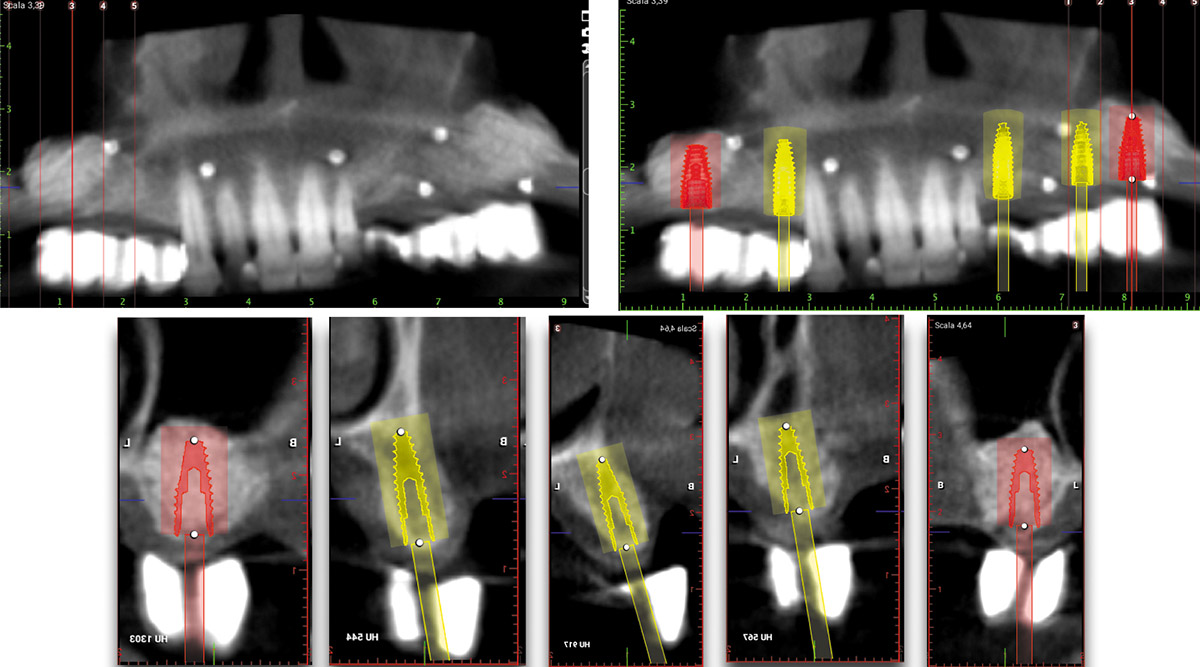
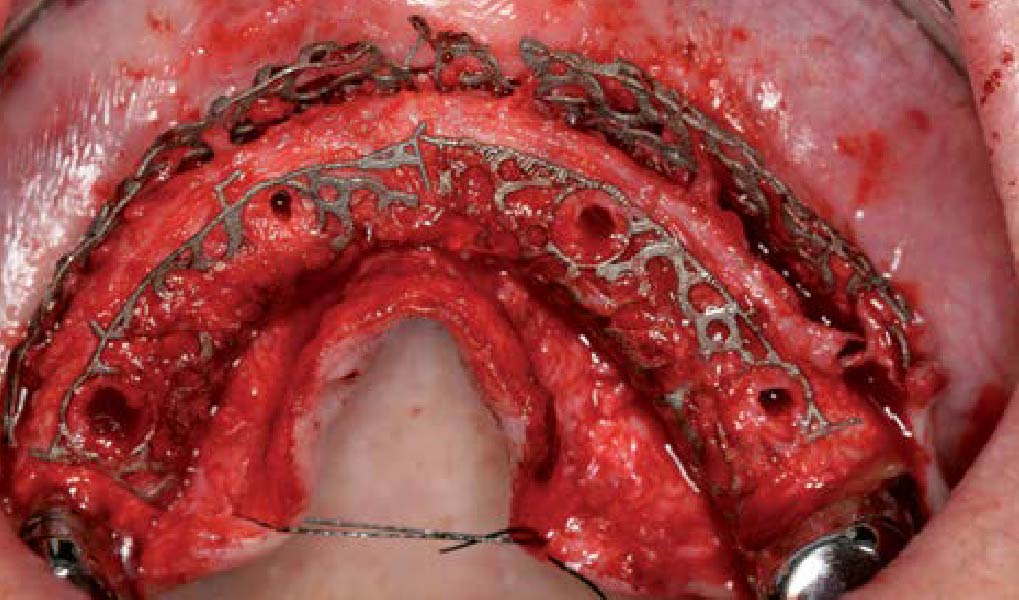
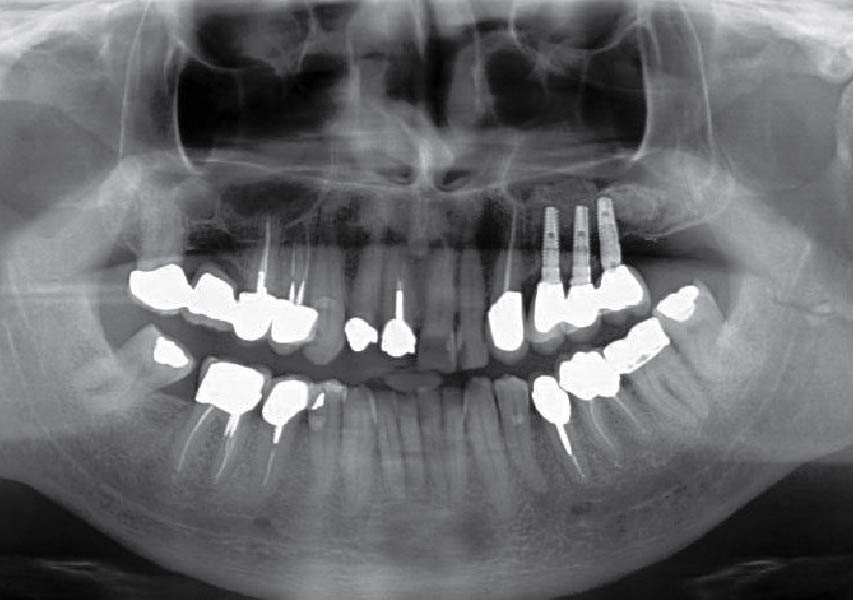
A 54-year-old, systematically healthy male patient (*ASA) came to our attention presenting with partial edentulism in the lower jaw and requiring a fixed and esthetic rehabilitation, refusing any removable solution. The clinical and radiographic evaluation resulted in significant bone atrophy both in the vertical and horizontal components; which makes it impossible to place both conventional implants and short or narrow implants.
*American Society of Anesthesiologists Physical Status Classification System
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
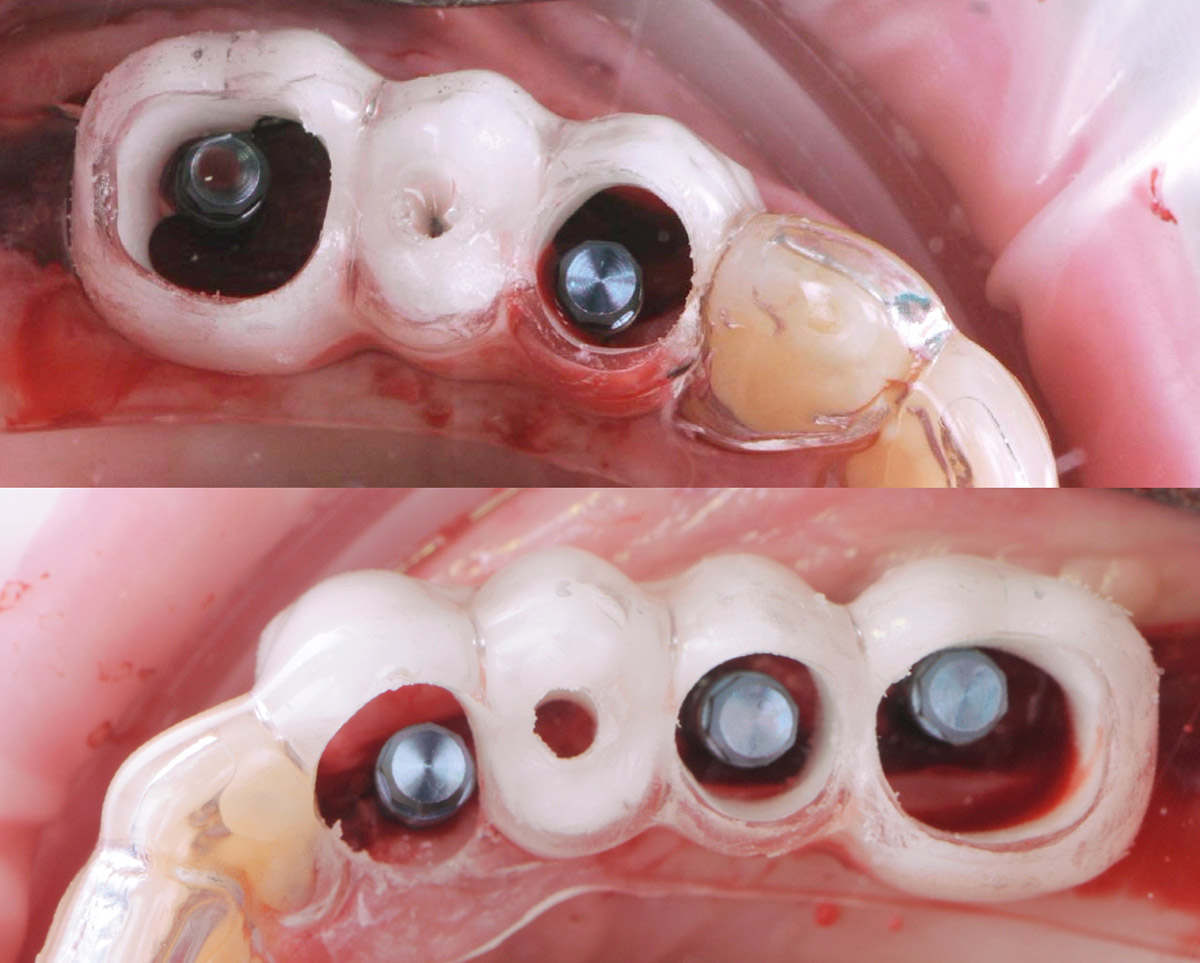
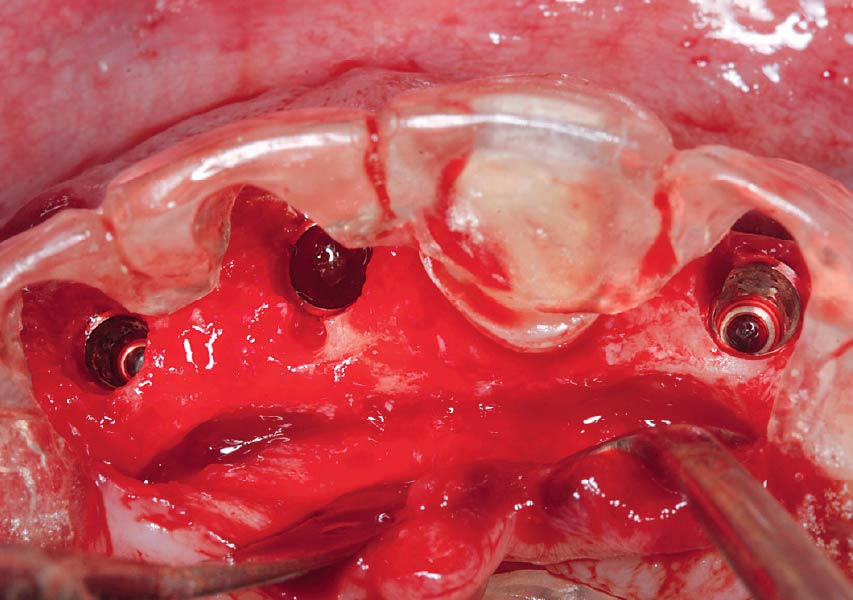
Solving the case was developed in two steps: first bone reconstruction to restore the ideal anatomy, second positioning of the prosthetically guided implants. An individualized regeneration technique was chosen using a CAD-CAM titanium scaffold (Yxoss CBR®) in conjunction with a mix of 60% autogenous bone and 40% Geistlich Bio-Oss®, covered by Geistlich Bio-Gide®. At 9 months, the titanium scaffold was easily removed and 3 prosthetically guided implants were placed, completely surrounded by bone. At 12 months, a free gingival graft was performed to re-establish the missing amount of keratinized mucosa. Finally, at 16 months, the final rehabilitation was carried out with a fixed prosthesis on implants.
“Combined horizontal and vertical bone augmentation utilizing a CAD CAM titanium scaffold can be achieved with less surgical time and less complications.”
THE OUTCOME
The final resolution of the case was very satisfactory. There were no complications during all the procedures performed. The Yxoss CBR® allowed for easier reconstructive surgery and a significant reduction in surgical times, thanks to the precise dimensions of the scaffold. This resulted in a favorable post- operative situation for the patient and complications were prevented.


Dr. Gian Maria Ragucci
Universitat Internacional de Catalunya (UIC), Barcelona Dental degree at Universidad Europea de Madrid 2015
International Master in oral surgery at UIC, Barcelona 2018
PhD student at UIC, Barcelona 2018
EAO Certification program in implant dentistry 2018
EAO European prize in implant dentistry 2019

Prof. Federico Hernández-Alfaro
Full professor & Chairman, Department of Oral and Maxillofacial Surgery, UIC, Barcelona
Institute of Maxillofacial Surgery, Teknon Medical Center, Barcelona

BIOBRIEF
Ramal Bone Graft for Congenitally Missing Maxillary Lateral Incisor

THE SITUATION
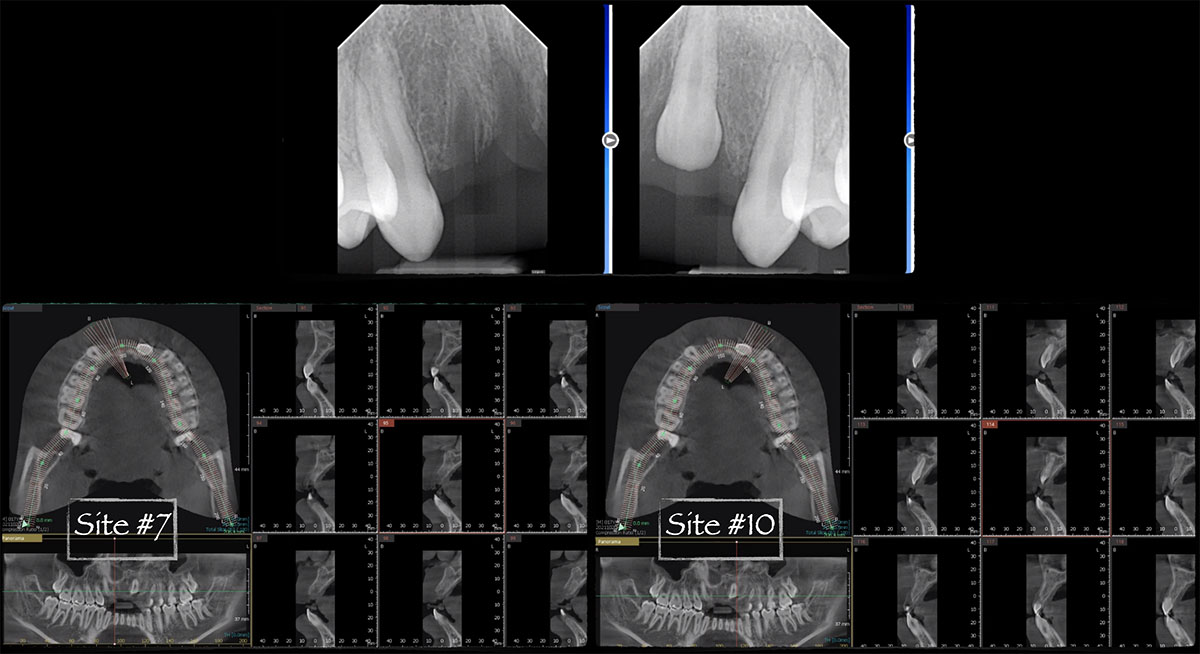
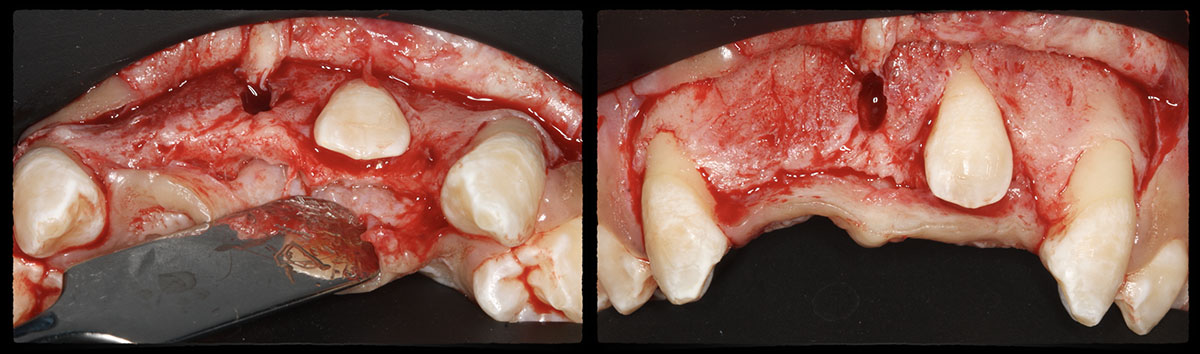
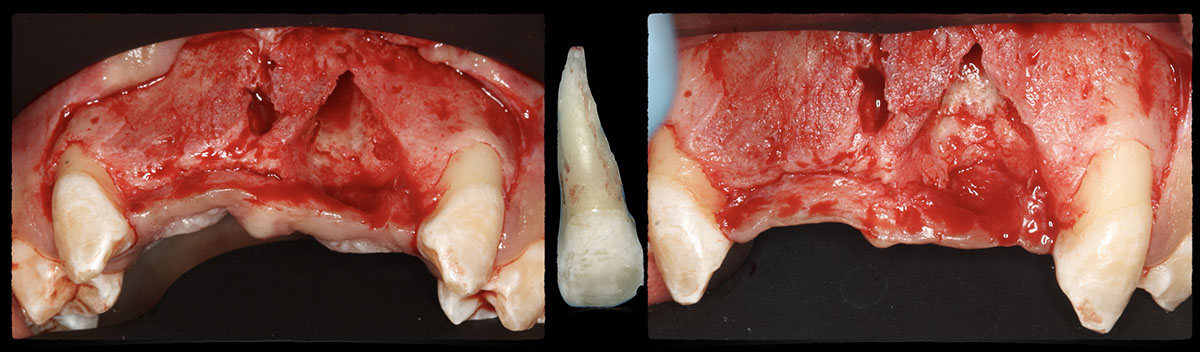
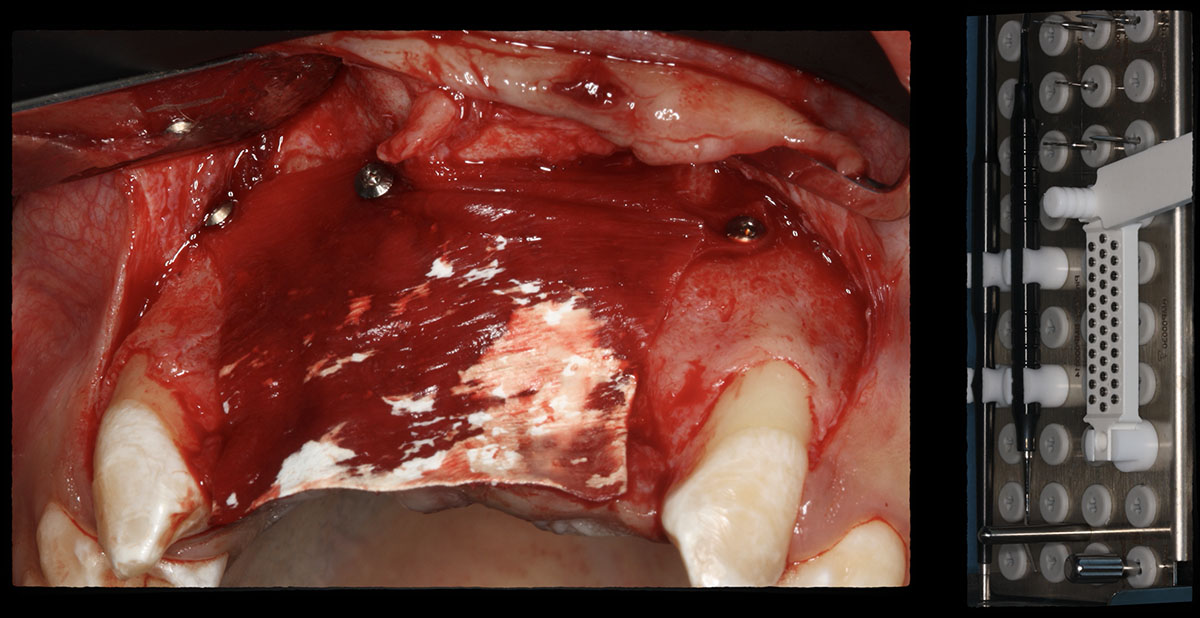
An 18-year-old female presented with a congenitally missing tooth #10. The patient previously sought care by another provider and had undergone guided bone regeneration with allograft and subsequent implant placement with additional grafting at the time of implant placement. The implant ultimately failed and was removed prior to my initial consultation. An examination revealed maximal incisal opening, within normal limits, missing #10 with 6 mm ridge width. In addition there was a significant palpable cleft-like depression on the facial aspect of the ridge, adequate attached tissue but reduced vertical height in relation to adjacent dentition and attached tissue. Previous surgeries resulted in extensive fibrous tissue with scarring at site #10. Plan: A ramal bone graft is indicated at the congenitally missing site #10 with Geistlich Bio-Oss® and Geistlich Mucograft® matrix utilized for ridge augmentation prior to secondary implant placement.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The goals for this patient are to reconstruct the osseous foundation and provide a matrix for improvement with the overlying soft tissue. Specifically, a coordinated multidisciplinary plan was established with the restoring dentist, periodontist and oral surgeon. A plan for idealized anterior cosmetic prosthetic restoration was established. Sequencing of treatment was established. Surgical phase one included a ramal bone graft to site #10 and Essix type temporary prosthesis for immediate post-operative phase followed by a temporary Maryland bridge. Surgical phase two included implant placement and simultaneous crown lengthening and osteoplasty. This stage was done with immediate provisionalization.
“This is a young patient with a congenitally missing incisor that has high esthetic concerns and has had multiple failed surgical attempts that is now presenting for definitive management.”
THE OUTCOME
This case was dependent upon adequate hard-tissue reconstruction combined with soft-tissue manipulation to eliminate scar tissue and provide esthetic recontouring. Obtaining an adequate autogenous graft combined with Geistlich Bio-Oss® at the periphery of the onlay graft is essential for anterior-posterior and vertical augmentation. Utilizing a Geistlich Mucograft® matrix at the ridge crest to help contain the particulate graft and improve the soft-tissue profile for subsequent immediate provisionalization and re-contouring of the surrounding soft tissue played a significant role in the esthetic success.


Dr. Richard E. Bauer, III
Oral and Maxillofacial Surgeon – University of Pittsburgh
Richard E. Bauer, III, DMD, MD is a graduate of the University of Pittsburgh Schools of Dental Medicine and Medicine. Dr. Bauer completed his residency training in Oral and Maxillofacial Surgery at the University of Pittsburgh Medical Center. Dr. Bauer has served on multiple committees for the American Association of Oral and Maxillofacial Surgery (AAOMS). He is a full-time faculty member and Residency Program Director at the University of Pittsburgh in the department of Oral and Maxillofacial Surgery and his practice is focused on dental implants and corrective jaw surgery. He has been active in research with focus on bone regeneration and virtual applications for computer assisted planning and surgery.

BIOBRIEF
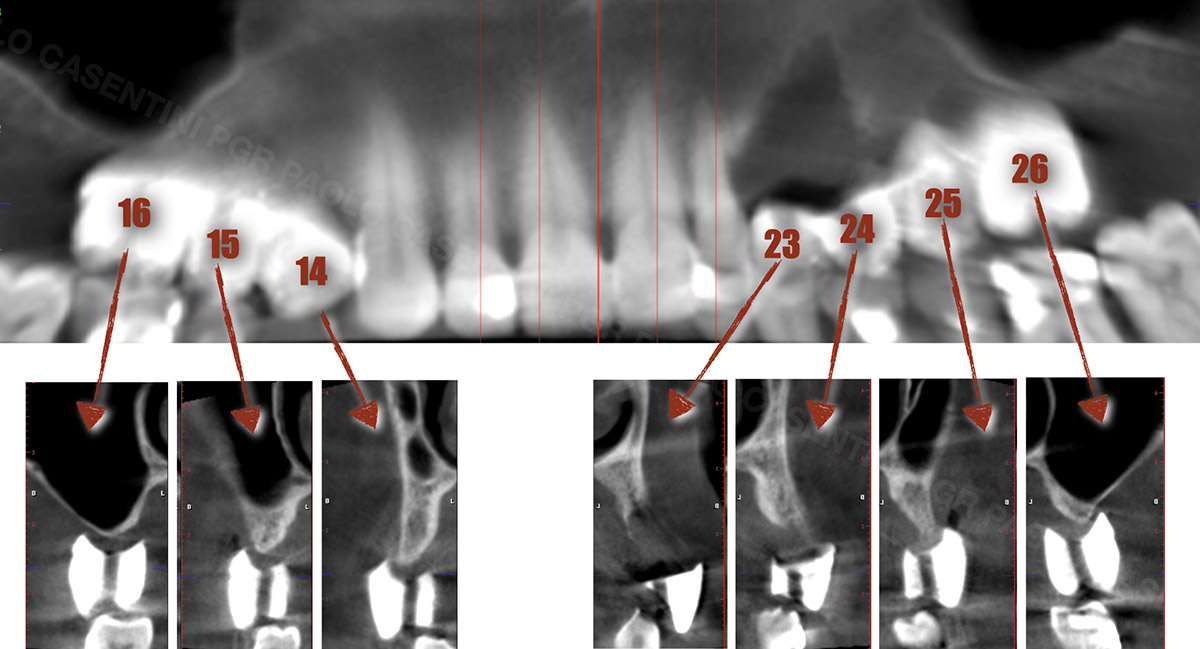
Prosthetically Guided Regeneration (PGR) in the Posterior Maxilla


THE SITUATION
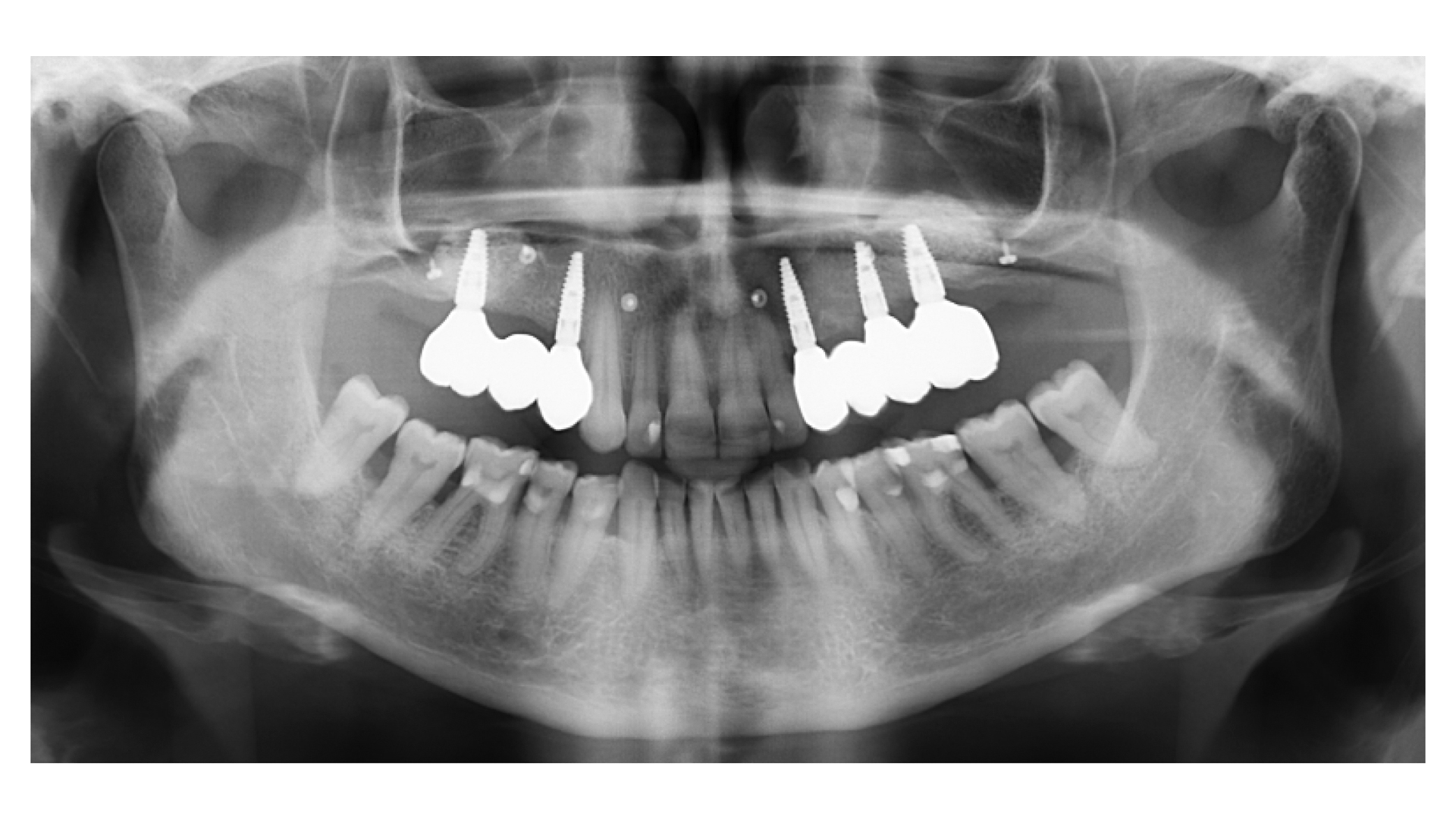
The 60-year-old female patient’s chief complaint was represented by unsatisfactory esthetics and function, related to loss of multiple maxillary teeth. Her request focused on improving esthetics and function by means of a fixed reconstruction.
The patient presented five residual anterior maxillary teeth (from 6 to 10) that could be maintained. After preliminary periodontal diagnosis and treatment, specific diagnostic steps for implant treatment demonstrated inadequate bone volume for implant placement.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
Bi-lateral sinus lift with Geistlich Bio-Oss Pen® and horizontal bone augmentation with a 1:1 mix of autogenous bone and Geistlich Bio-Oss® were performed six months prior to implant placement, following a Prosthetically Guided Regenerative (PGR) approach. The augmented sites were protected with Geistlich Bio-Gide® stabilized with titanium pins. The template utilized for radiographic diagnosis and GBR was then used to guide the implants’ placement.
Using a diagnostic template during the GBR procedure helps to highlight the presence of bone defects in relationship to the restorative plan and future position of implants.
THE OUTCOME
After a healing period of six months, adequate bone volume was achieved for the placement of five implants. Geistlich Fibro-Gide® was also used to optimize soft tissue volume at the buccal aspect of implants.
Implants were early loaded with a temporary screw-retained fixed prostheses six weeks after placement. The final prosthetic reconstruction included ceramic veneers of the frontal residual teeth and zirconium-ceramic screw-retained fixed prostheses on implants.


Paolo Casentini, DDS
Graduated in Dentistry at the University of Milan, Fellow and Past Chairman of the Italian section of ITI, Active member Italian Academy of Osseointegration. Co-author of 10 textbooks including ITI Treatment Guide volume 4, translated in eight languages, and “Pink Esthetic and Soft Tissues in Implant Dentistry” translated in five languages. His field of interest is advanced implantology in complex and esthetically demanding cases. He has extensively lectured in more than 40 countries.

BIOBRIEF
A Regenerative Approach to Peri-implantitis

THE SITUATION
A 55-year-old man was referred to me by his general dentist. Upon initial clinical and radiographic findings, failing implant #9 showed signs of peri-implantitis that included BoP, Suppuration, 9+mm PD and radiographic bone loss affecting both the implant and the natural adjacent tooth. Patient stated that although his gums bleed, he does not have any pain. Gingival erythema was also found.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
Note: Peri-implantitis on implant #9 migrating to the mesial portion of root #8
THE APPROACH
The clinical goals were to eliminate the peri-implant infection, restore hard and soft-tissues and have long-term success. The technique utilized was a systematic regenerative approach to eliminate the underlying cause of the peri-implantitis infection and restore hard and soft-tissues to prior health.
Geistlich Fibro-Gide® has the capacity to enhance the soft-tissue during a bone regenerative approach.
THE OUTCOME
My observation at the 1.5 year follow-up shows the elimination of peri-implantitis and complete peri-implant health was achieved showing a reduction in BOP, PD and most importantly soft tissue thickness stability. Radiographically, crestal bone shows no signs of progressive pathological loss and has maintained adequate volume.

Hector L. Sarmiento, D.M.D., MSc.
Dr. Hector Sarmiento was awarded his D.M.D. degree by the University of Rochester. He is uniquely trained in both maxillofacial surgery and periodontics. He is a professor in the maxillofacial surgery department of trauma and reconstructive unit at the Regional Hospital in Mexico and is an Assistant Clinical Professor in periodontics at the University of Pennsylvania. Along with his periodontal degree, he also received his masters in oral biology from the University of Pennsylvania. Dr. Sarmiento is an international and national lecturer and has published numerous articles in peer reviewed journals and textbooks. His research focus includes infected dental implants such as peri-implantitis, sinus complications as well as bone biology. Dr. Sarmiento maintains his private practice in the upper east side of Manhattan in NYC.

BIOBRIEF
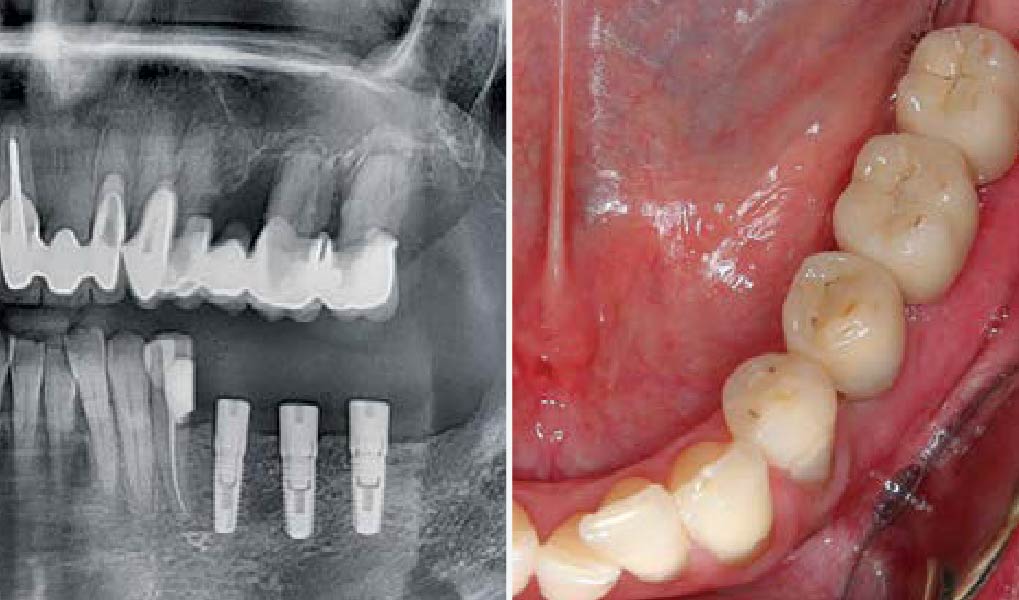
3D Bone Augmentation Using Customized Titanium Mesh in Conjunction with Autogenous Bone and Bovine Bone Material Granules


THE SITUATION
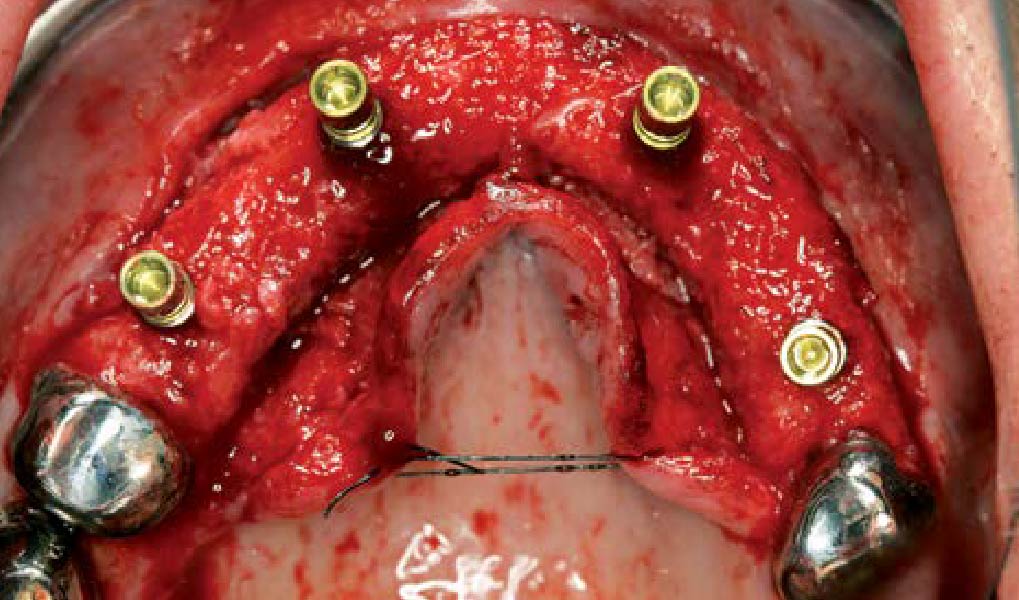
A 75-year-old systemically healthy female came to our attention presenting with absent mandibular second bicuspids and molars and requiring a fixed rehabilitation supported by implants as she refused a removable solution. The clinical and radiographic evaluation showed a relevant vertical and horizontal bone atrophy of such an extent that short or narrow implants were not considered a reliable option. The patient smoked <10 cigarettes per day.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
The main goal was to obtain a horizontal and vertical reconstruction of the deficient alveolar bone in order to allow safe and prosthetically-guided implant placement. Reconstruction was obtained by means of a customized titanium mesh, Yxoss CBR®, in combination with a mixture of autologous bone chips harvested from the mandibular ramus and bovine bone mineral, Geistlich Bio-Oss®.
The 3-dimensional reproduction of the left edentulous area permits the production of a precise and customized Ti-mesh.
THE OUTCOME
Post-operative recovery of this patient was uneventful, no complications such as dehiscence or late exposure of the customized mesh, with complete correction of the initial defect. The Yxoss CBR® allowed an easy and faster reconstruction thanks to the precision of the prefabricated mesh filled with autologous chips, Geistlich Bio-Oss® and Geistlich Bio-Gide®.


Matteo Chiapasco, D.D.S., M.D.
Graduated in Medicine and specialized in Maxillofacial Surgery at the University of Milan, Italy. Professor, Unit of Oral Surgery, University of Milan; Associate Professor, Loma Linda University, Los Angeles, California, USA.

Grazia Tommasato, D.D.S., M.S.C.
Graduated in Dentistry in 2013, specialized in Oral Surgery at the University of Milan magna cum laude. PhD student and a medical consultant of the Clinical Unit of Oral Surgery (“G. Vogel” Clinic, Milan).

WEBINAR

WEBINAR

WEBINAR

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE
CLINICAL CHALLENGE:
- The planning of the patient’s case takes local and general patient-specific risk factors into consideration according to the principles of backward planning for implant positioning.
AIM/APPROACH:
- Highlights step-by-step the important procedures to regenerate the bone (horizontal and vertical) with the 3-D printing technology, Yxoss CBR®.

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE
CLINICAL CHALLENGE:
- Severely atrophied alveolar ridge with insufficient bone volume for implant placement
- High complication rates and patient discomfort associated with large augmentations when using autologous bone grafts
AIM/APPROACH:
- 3-dimensional augmentation of alveolar ridge by the fence technique for implant placement
- At the same time reducing complication rates and patient discomfort

CLINICAL CASE
CLINICAL CHALLENGE:
- Insufficient alveolar ridge width for implant placement
- Autologous bone is subject to resorption and may lead to loss of volume
AIM/APPROACH:
- Ridge Split procedure in combination with Geistlich Bio-Oss® and Geistlich Bio-Gide® for horizontal augmentation
- Preservation of the alveolar ridge volume

CLINICAL CASE
CLINICAL CHALLENGE:
- Insufficient alveolar ridge width for implant placement
- Donor site morbidity after autologous bone block harvesting and resorption of autologous bone
AIM/APPROACH:
- Horizontal alveolar ridge augmentation with Geistlich Bio-Oss® and Geistlich Bio-Gide®
- Minimizing autologous bone harvesting and resorption protection

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE

CLINICAL CASE
CONCLUSIONS:
- Geistlich Mucograft® with a keratinized tissue strip was utilized to increase vestibular depth and gain additional keratinized tissue.
- Augmentation of severely atrophied alveolar ridge provided sufficient bone for implant placement 8 months following augmentation.