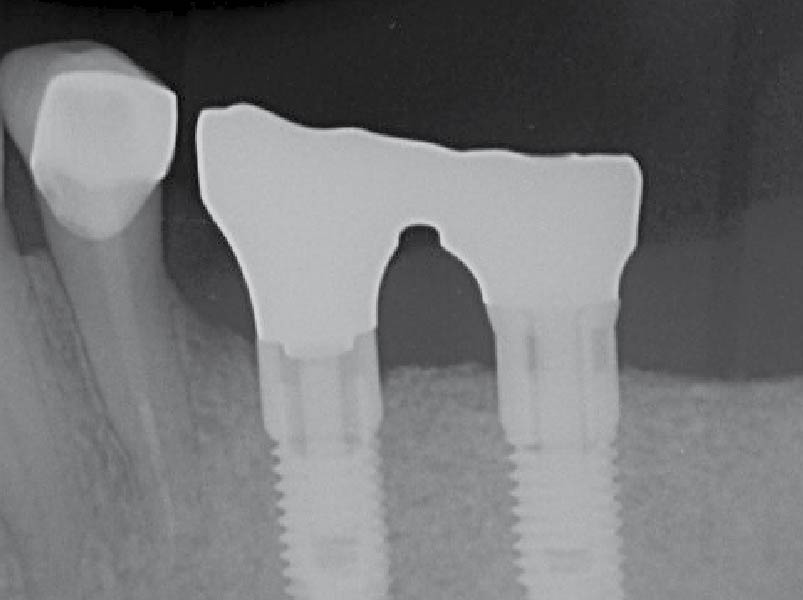
CLINICAL CASE





NEW EBOOK: How to Master Bone Regeneration with Digital Innovation. Download Today!
Mix & Match! Buy ANY 10 Biomaterial Products, Get 3 Free! Use code Q3BG10 Learn More
Buy 4 Geistlich Bio-Oss Collagen®, Get 1 Free! Use code GBOC25 Learn More
GEM 21S®, the first recombinant growth factor product for use in oral regenerative surgery. Learn More





















































CONCLUSIONS: