BIOBRIEF
Bone Augmentation L-Shape Technique with Early Implant Placement


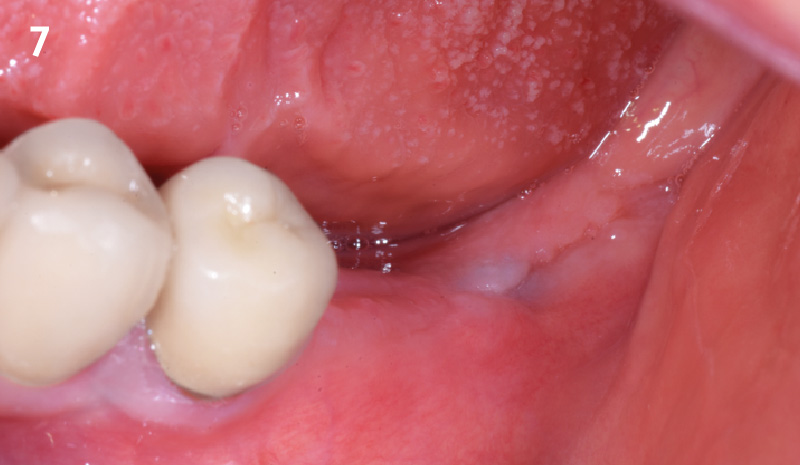
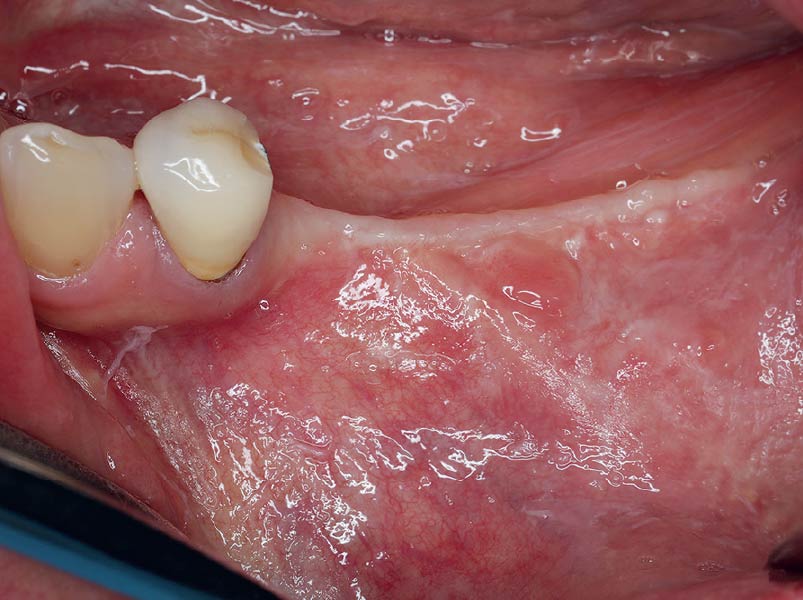
THE SITUATION
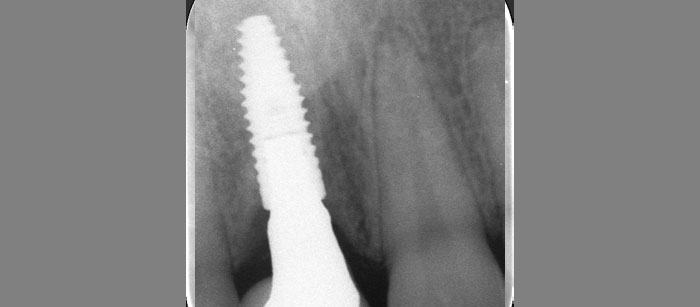
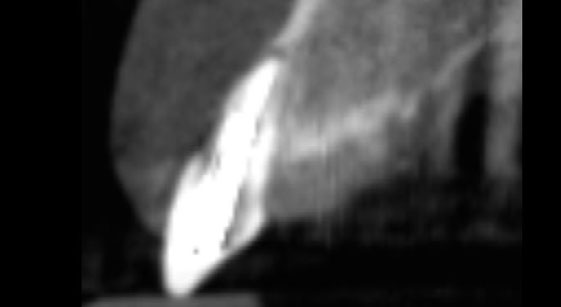
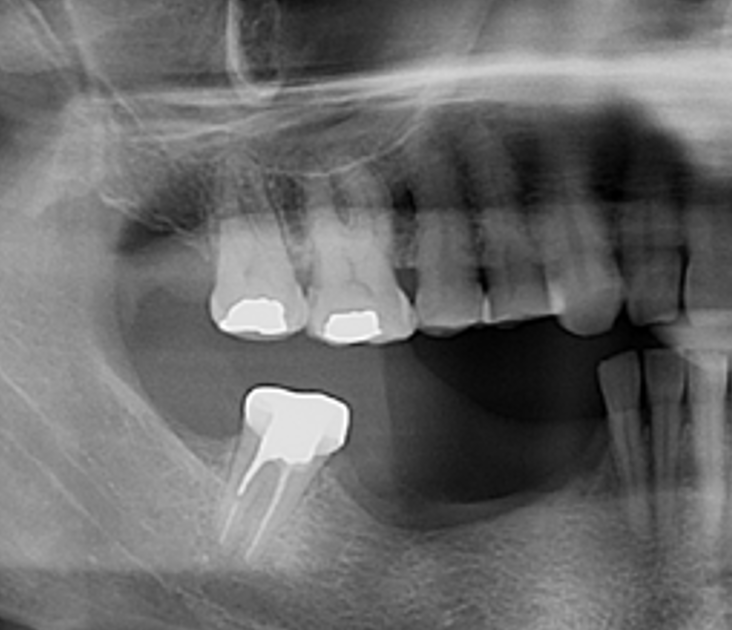
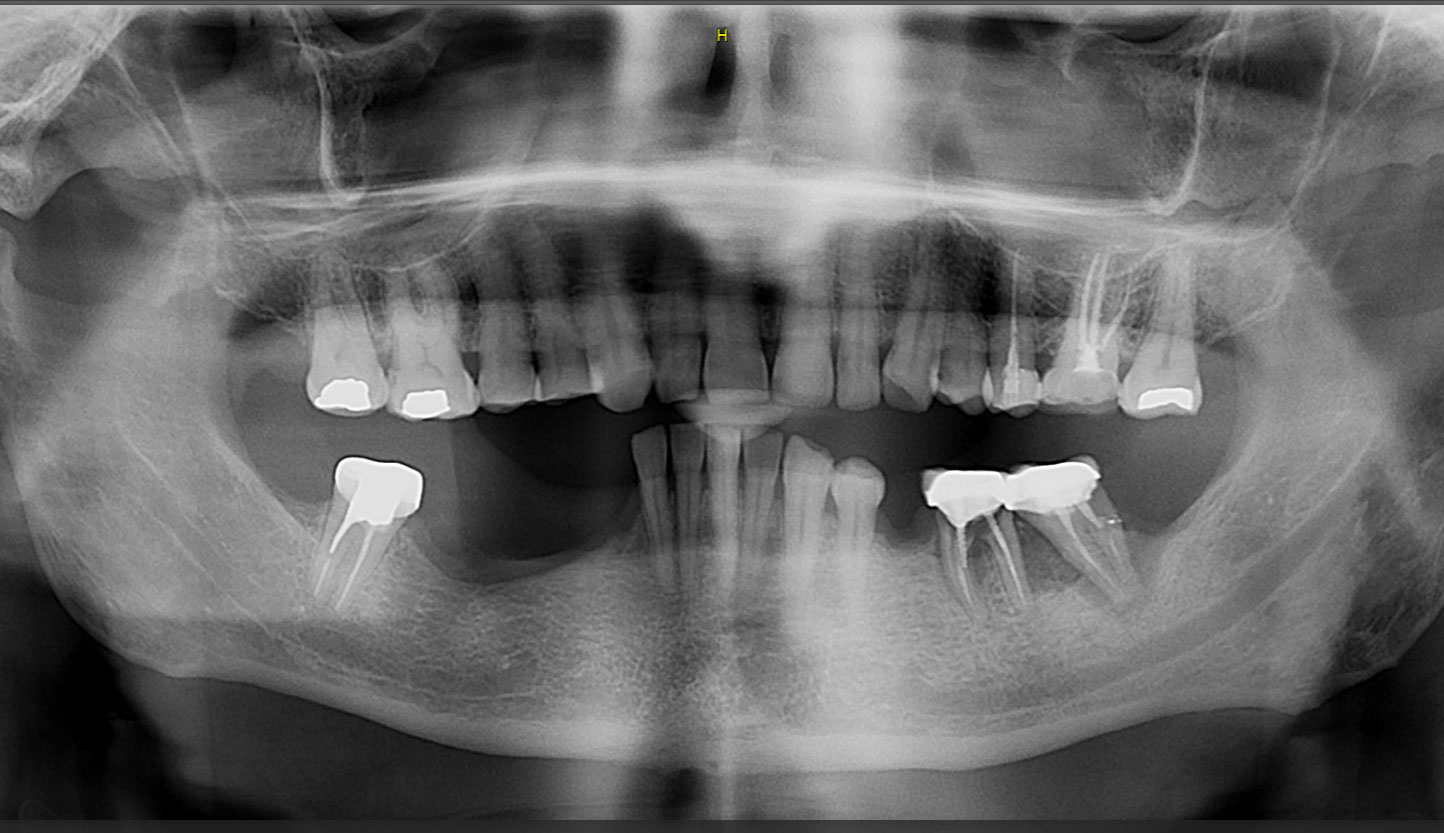
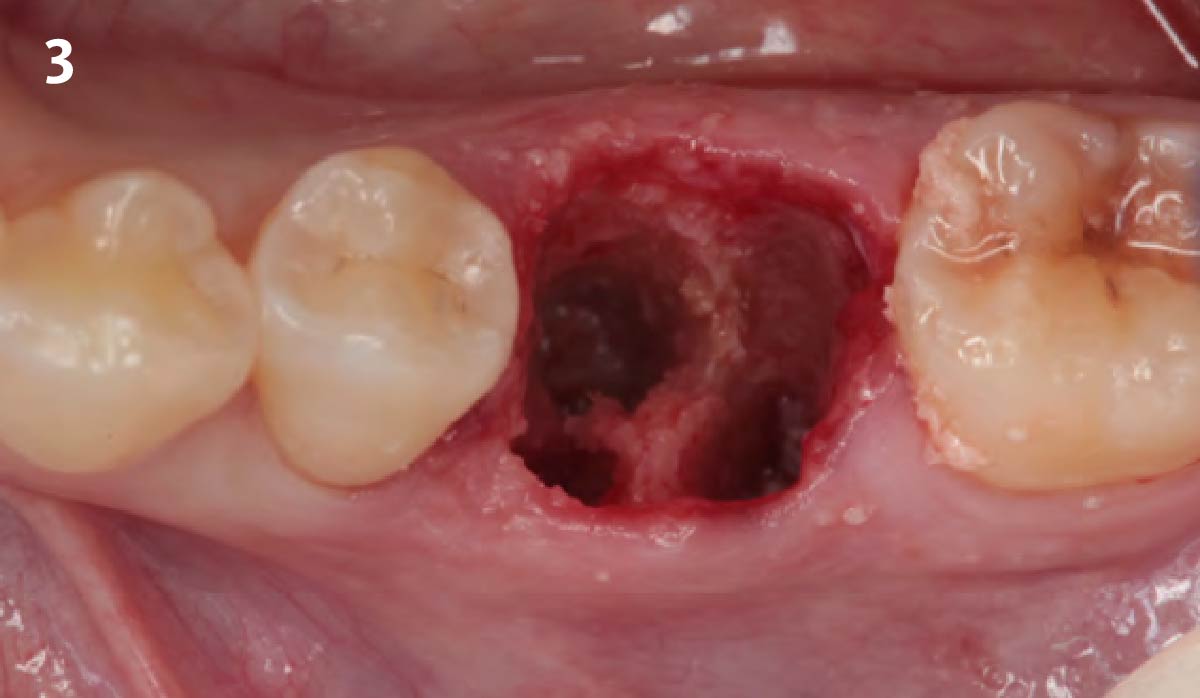
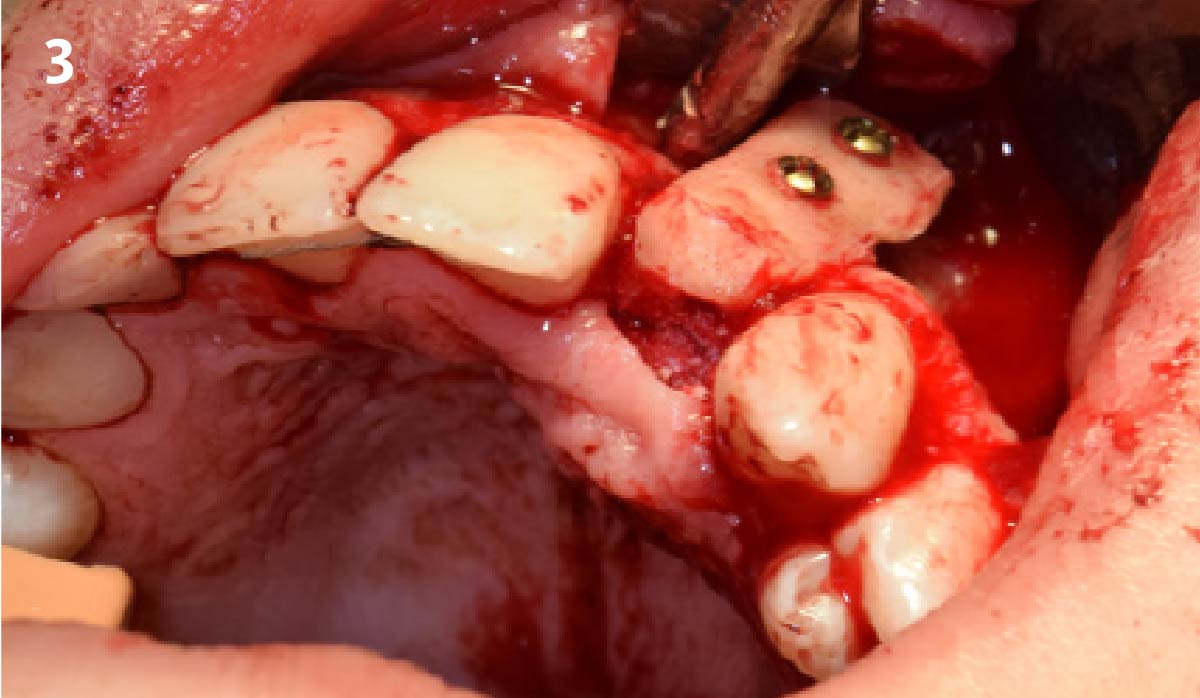
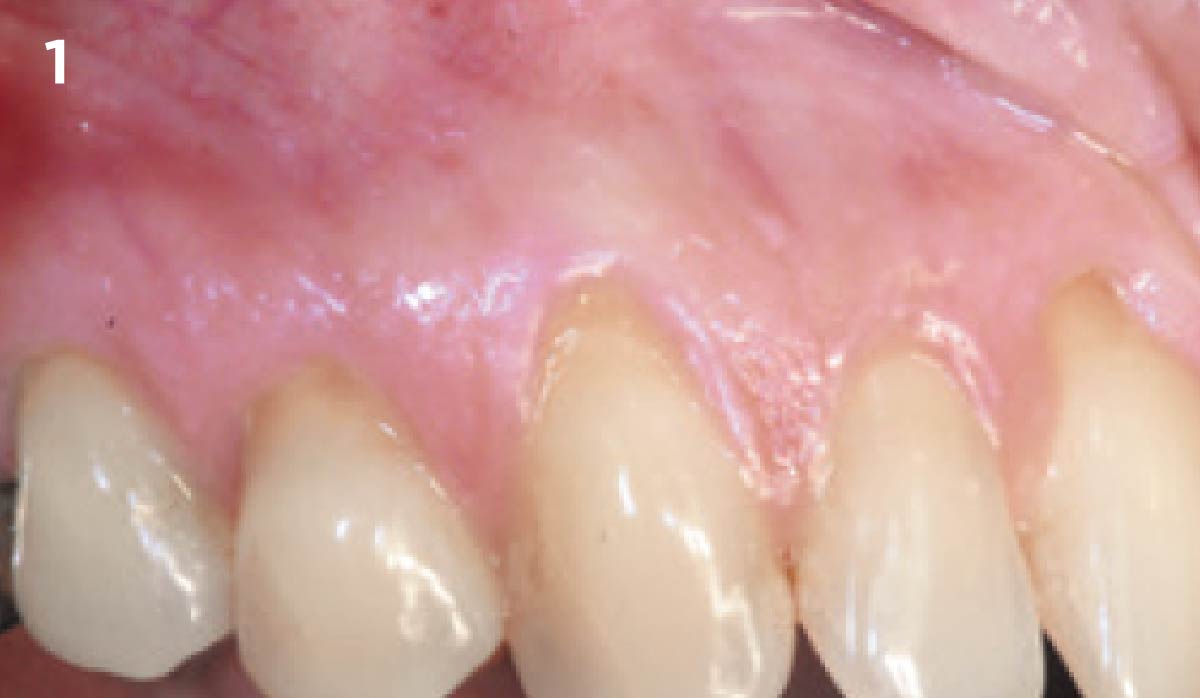
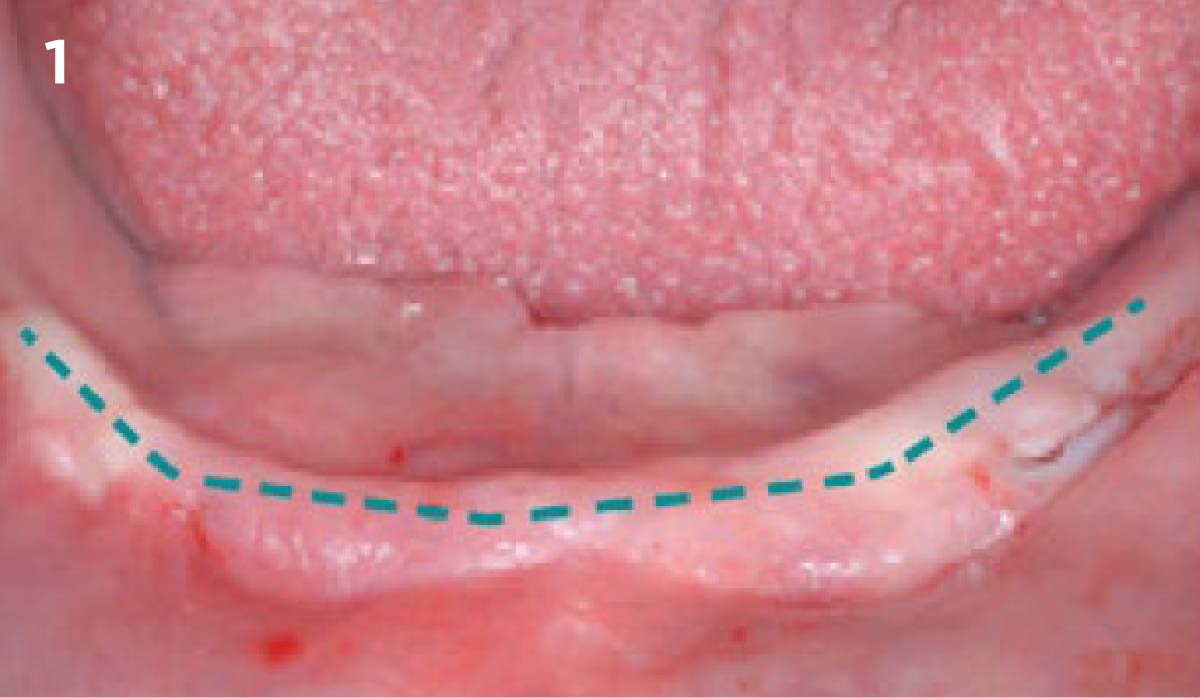
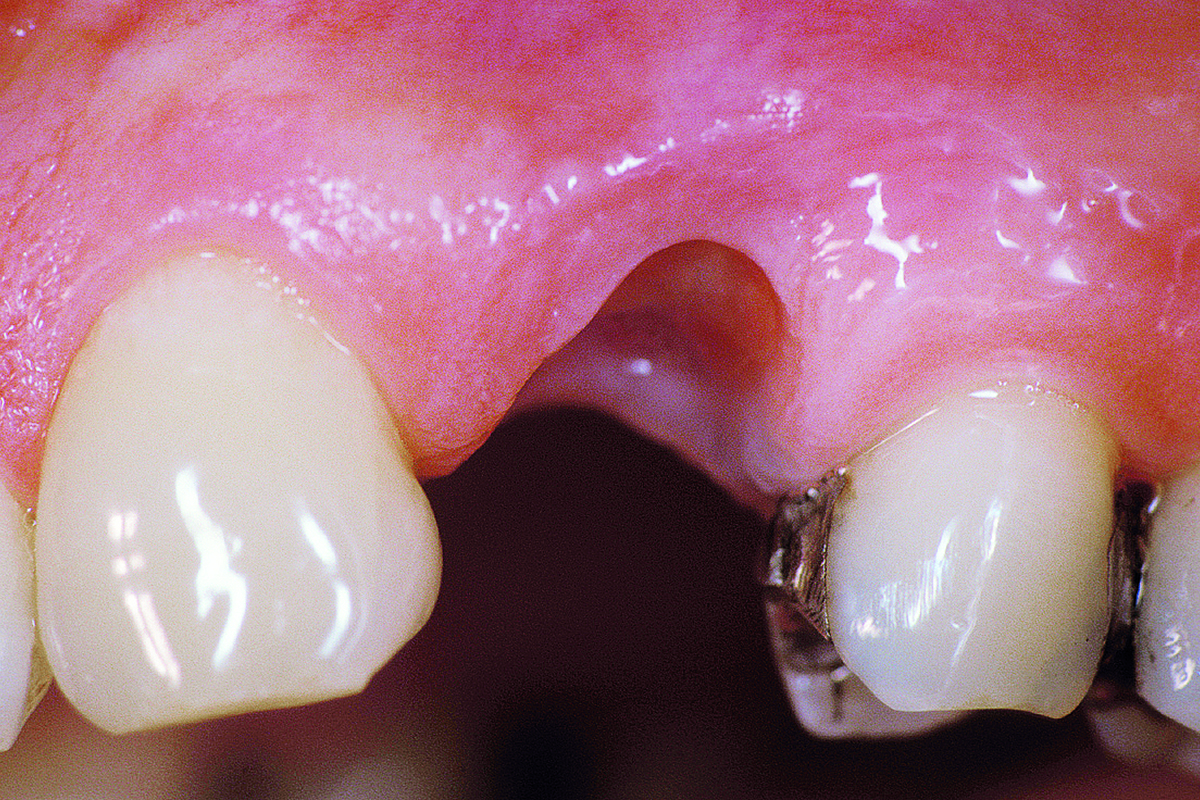
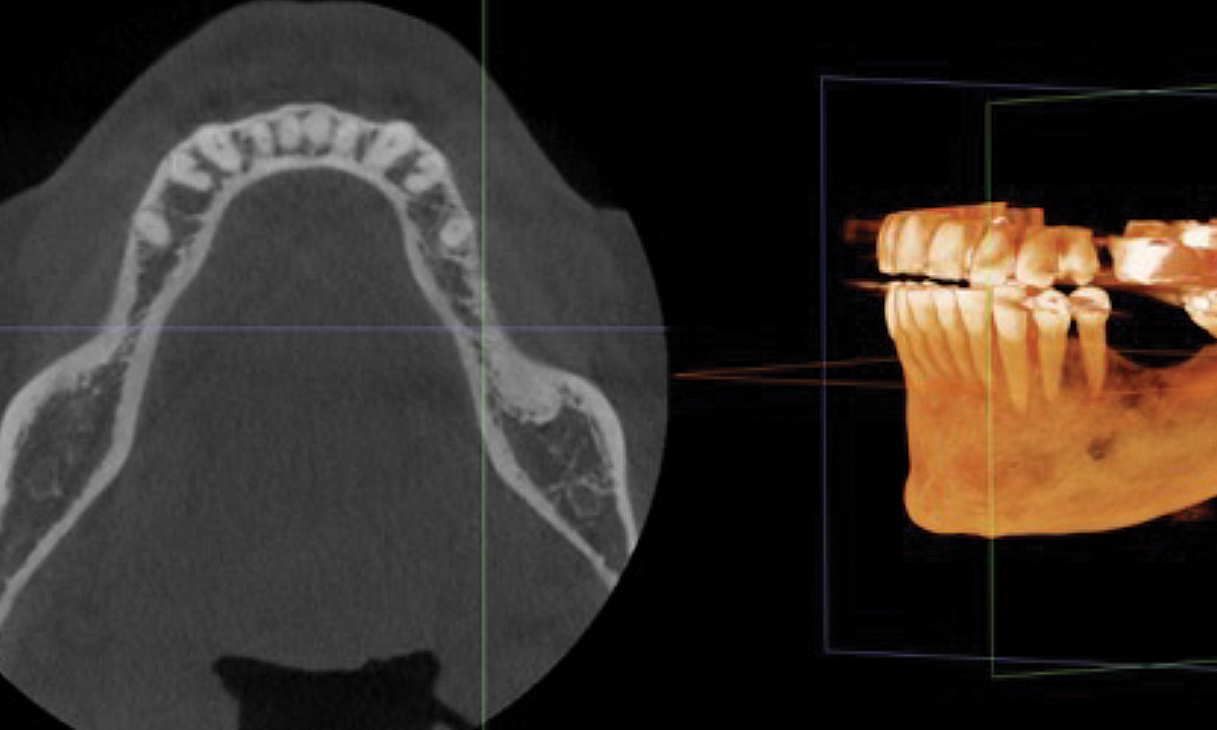
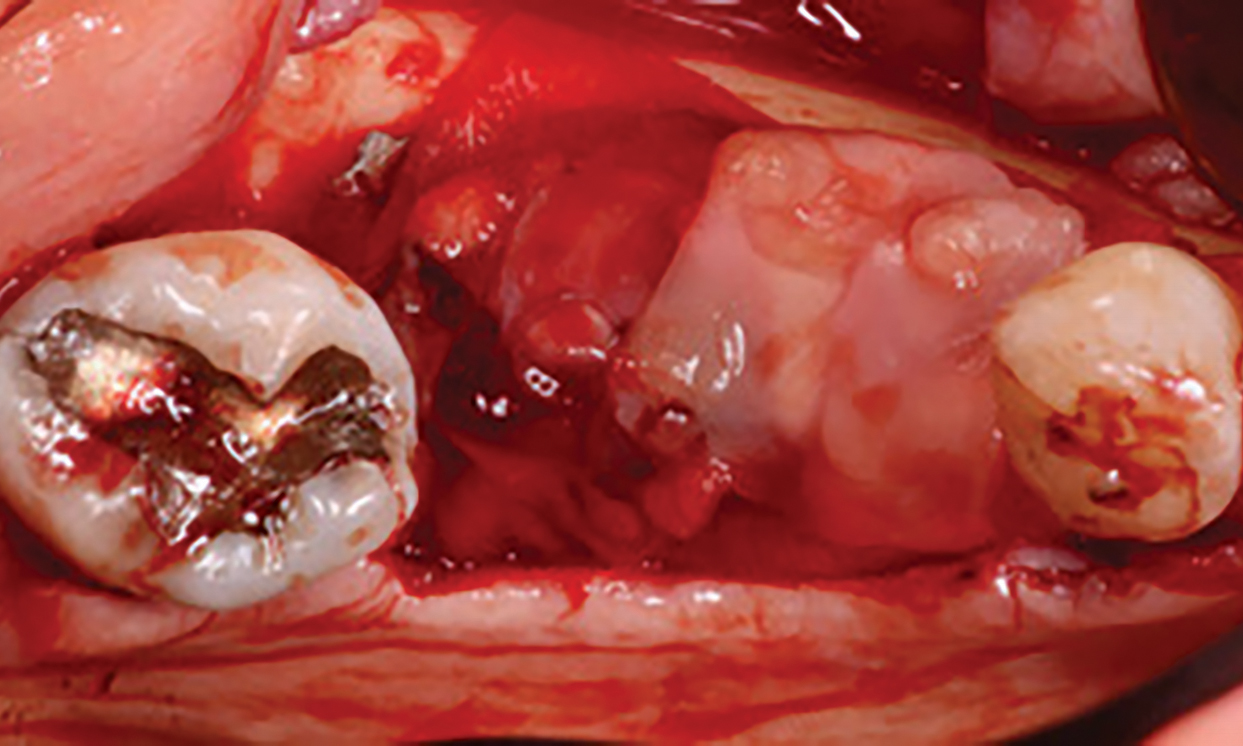
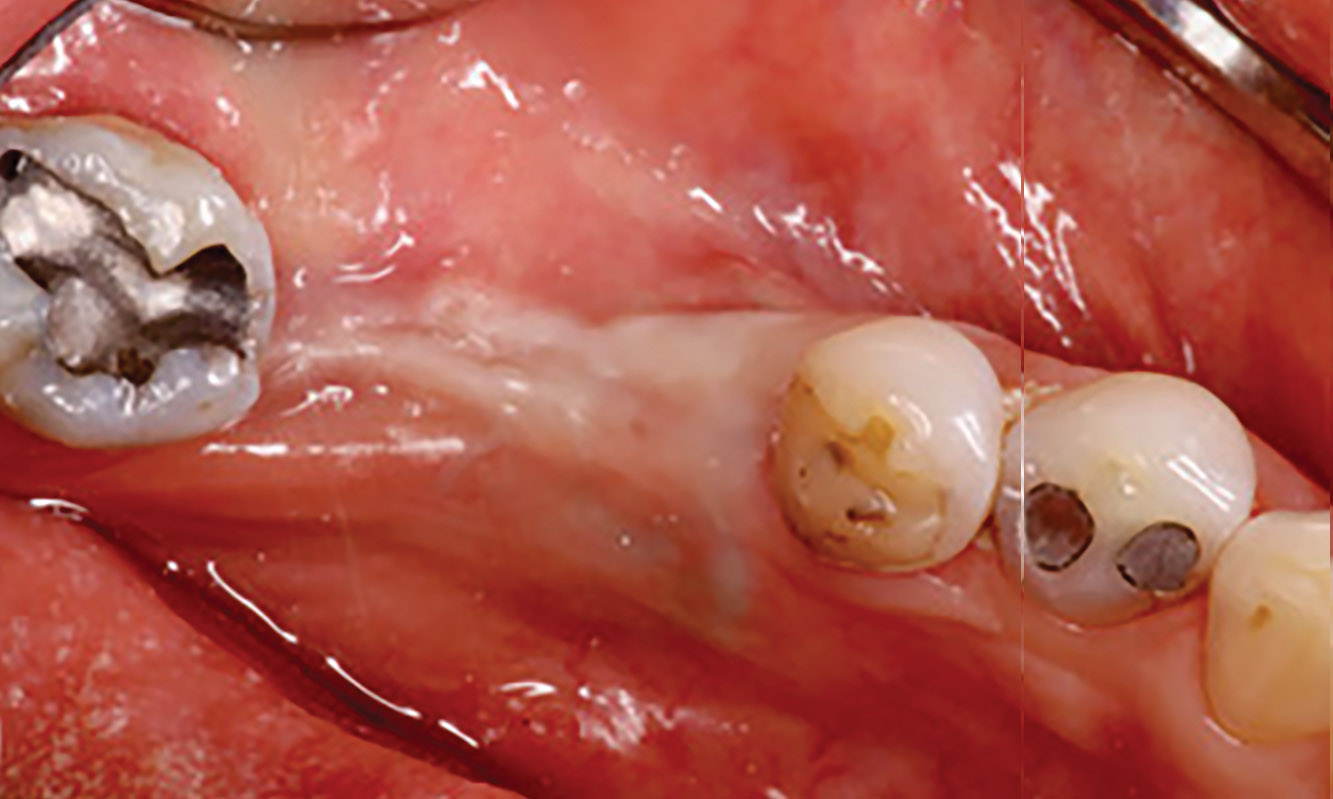
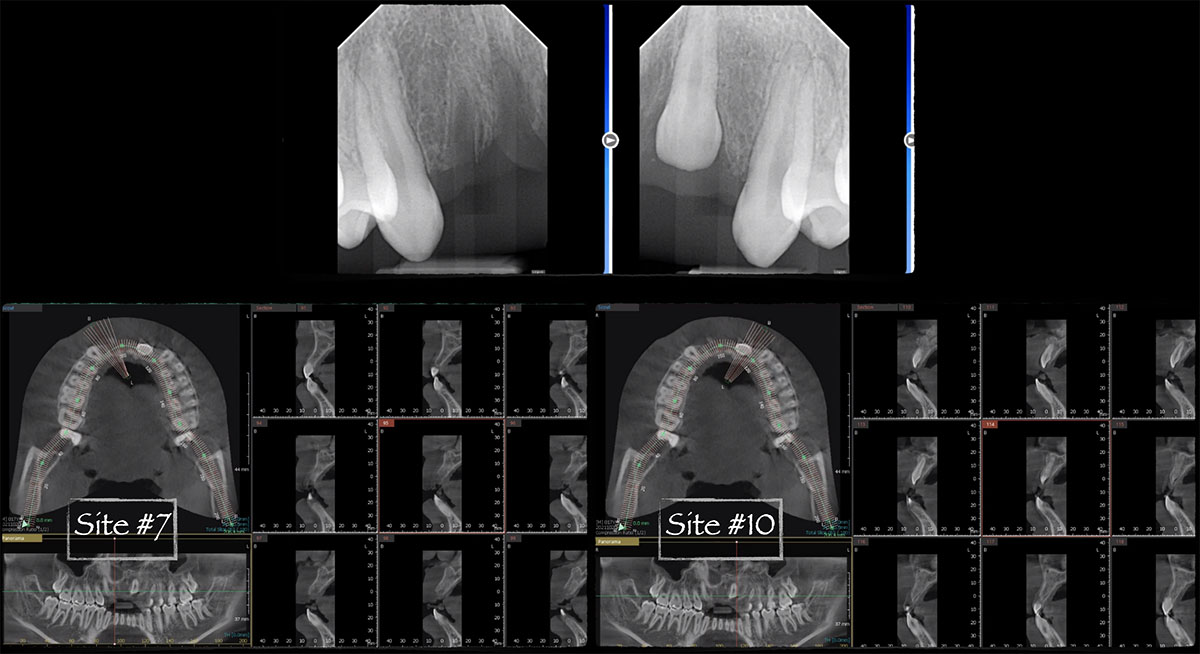
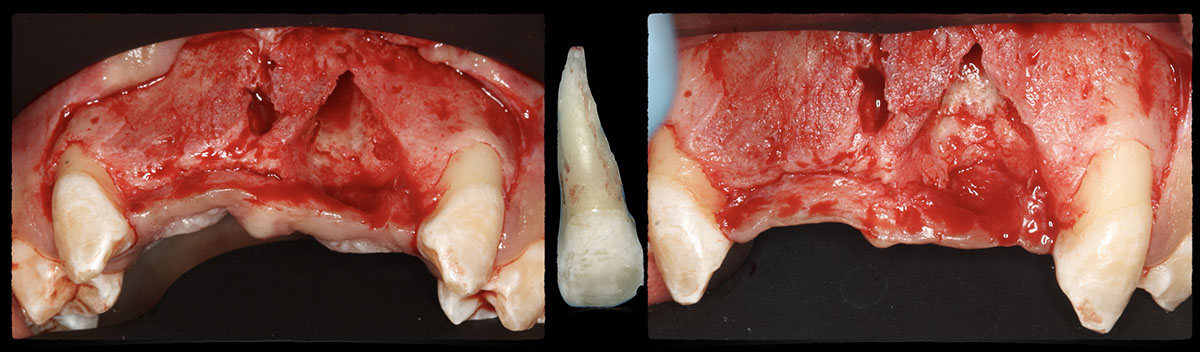
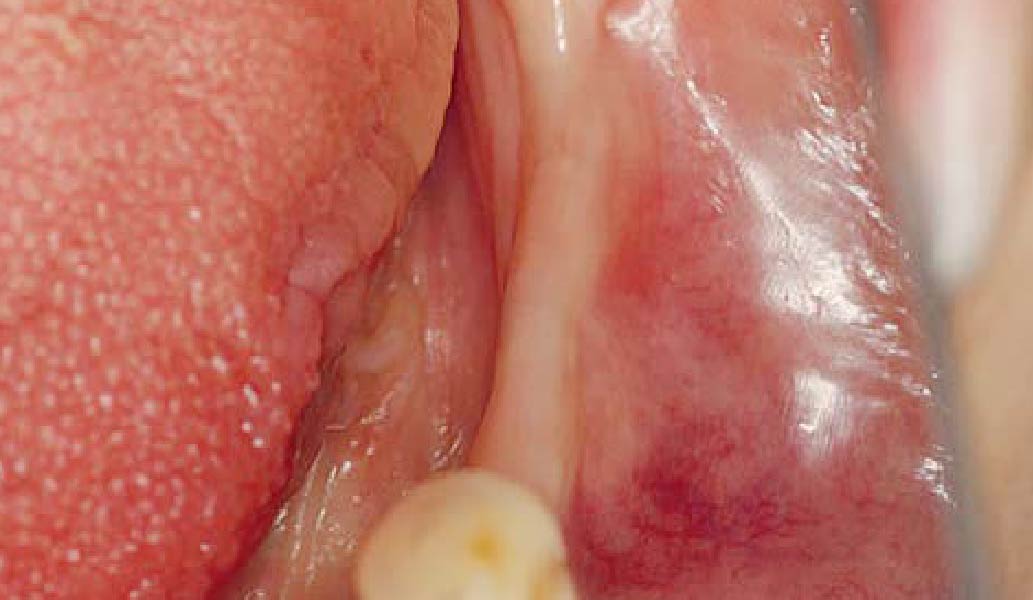
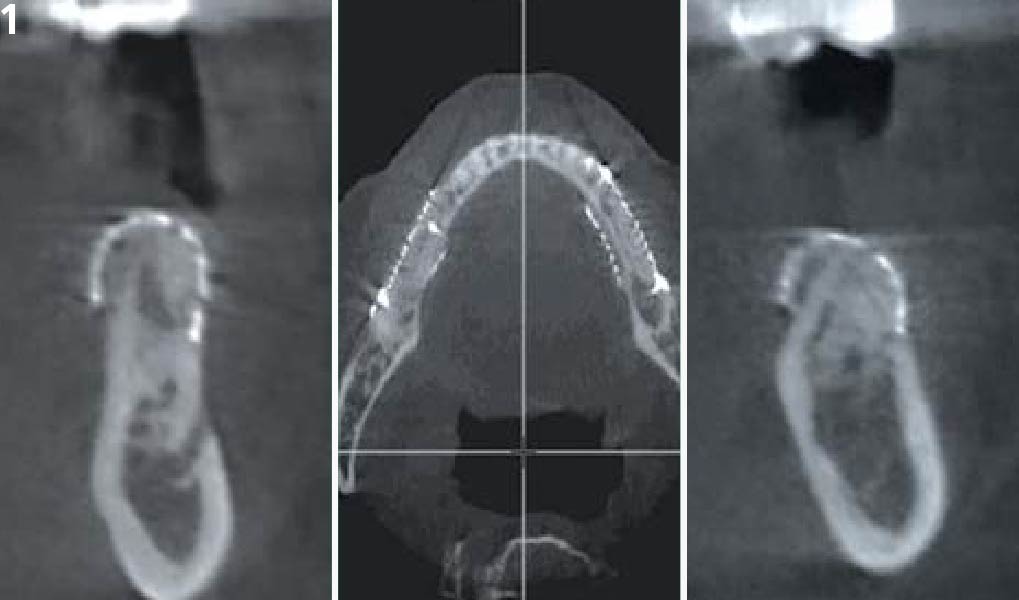
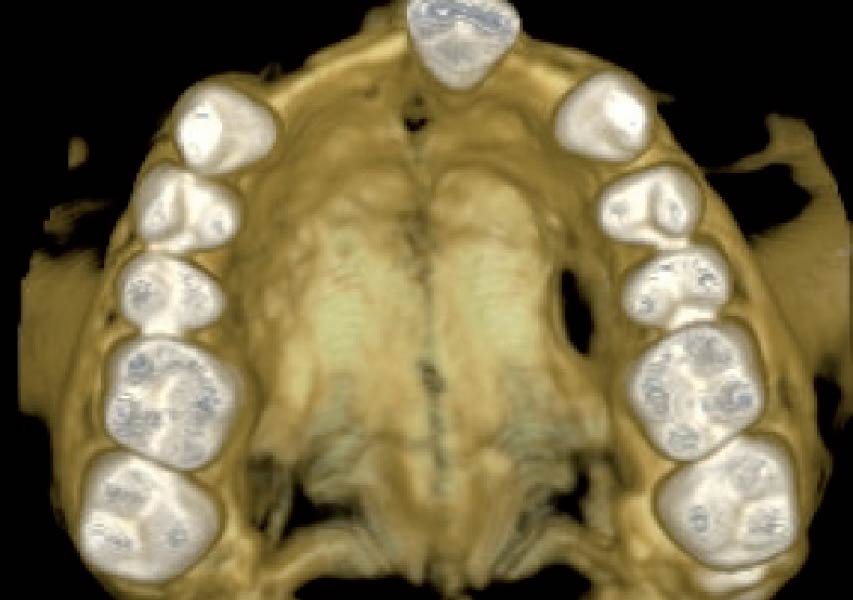
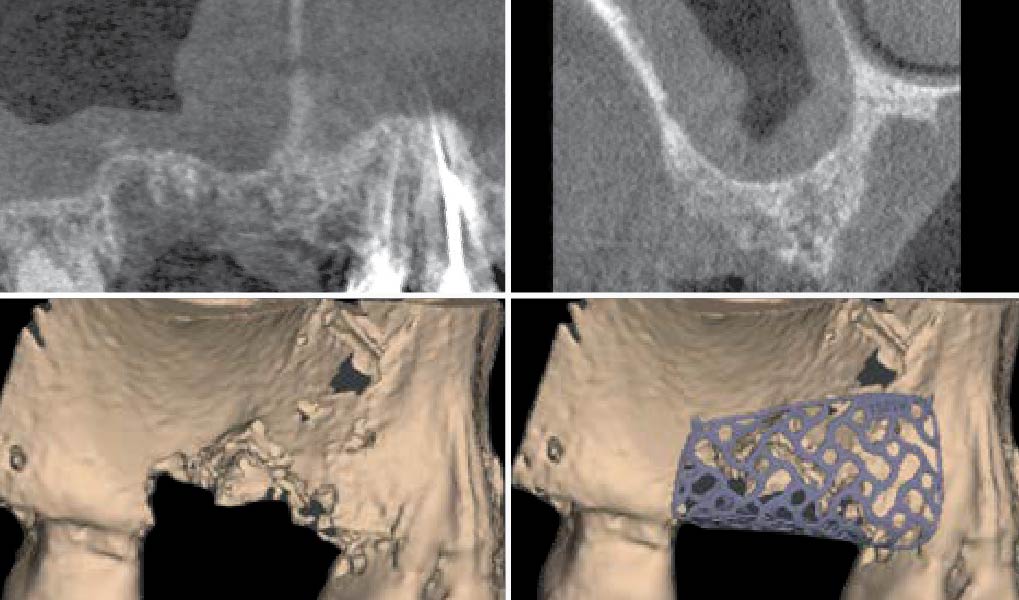
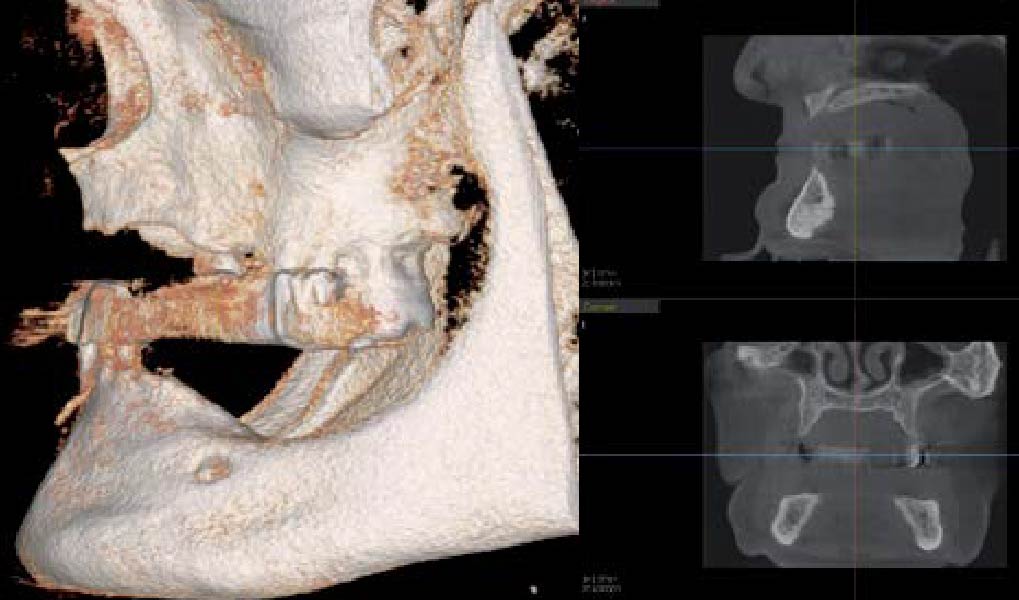
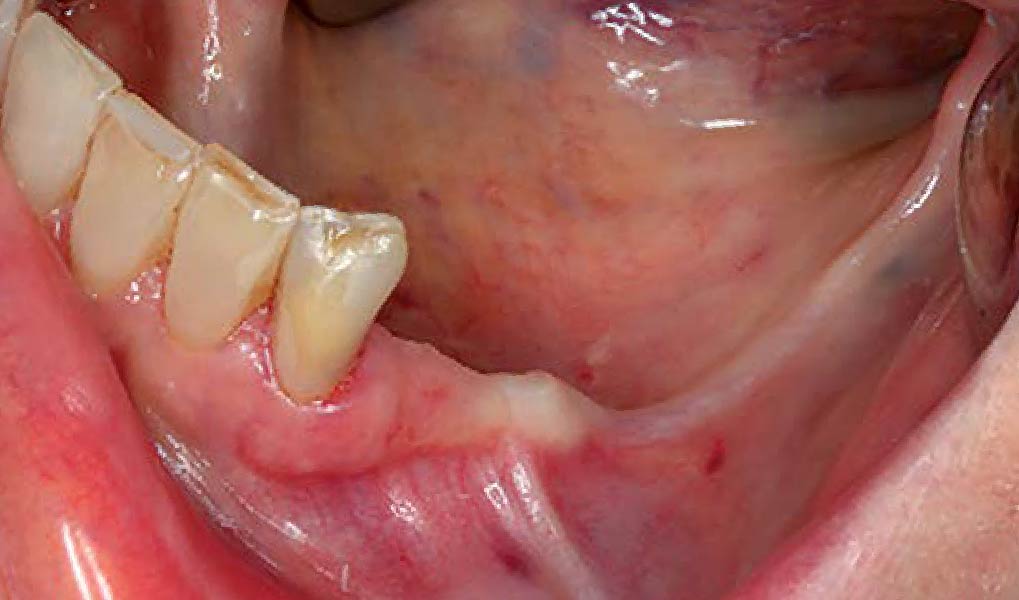
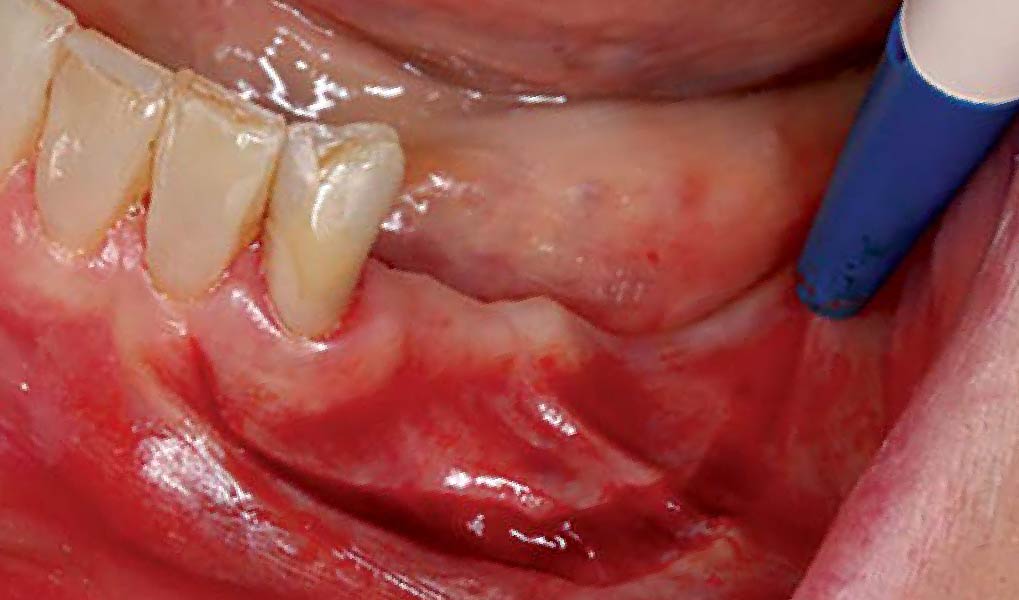
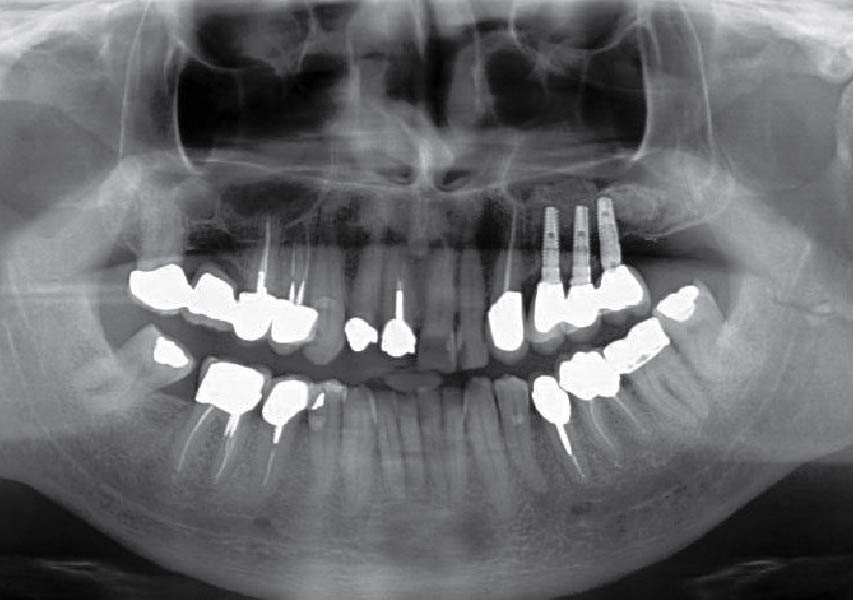
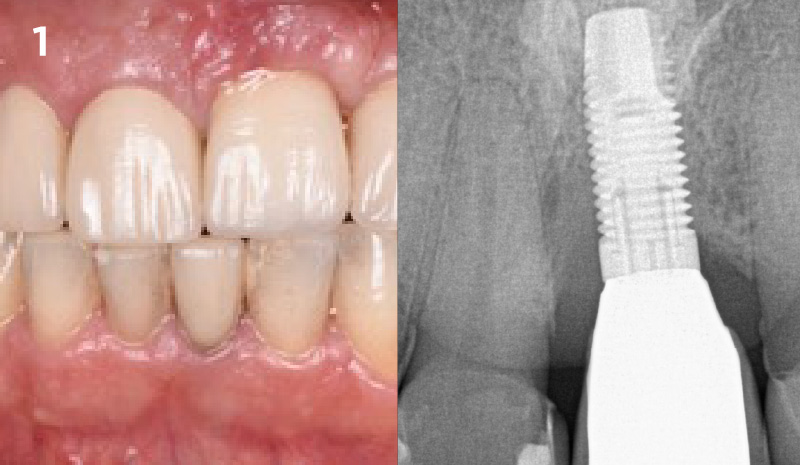
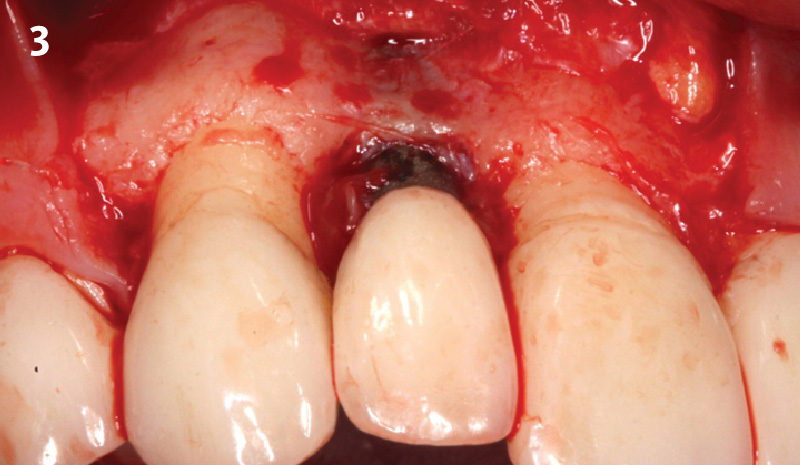
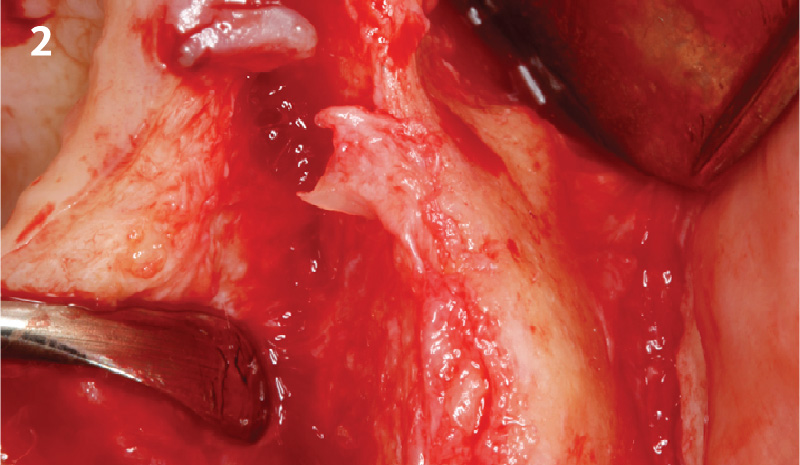
The patient presented to the clinic with a discolored tooth #8, with mobility and a history of trauma. The tooth has a horizontal fracture in the apical third of the root and has recurrent infection after the root canal treatment. The patient feels discomfort and dislikes his esthetic appearance. He would like the fractured tooth #8 removed and replaced with a fixed solution.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
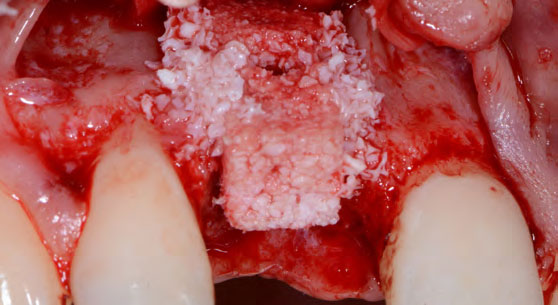
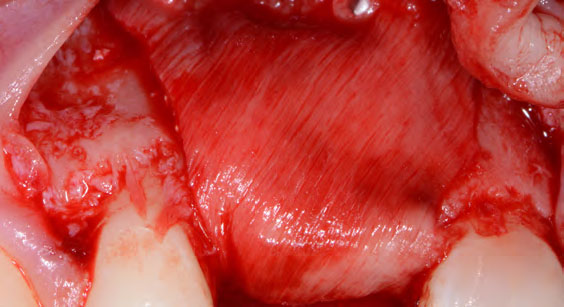
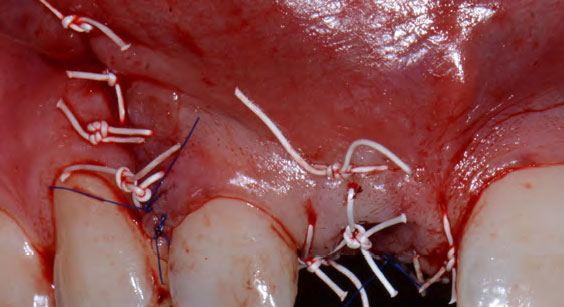
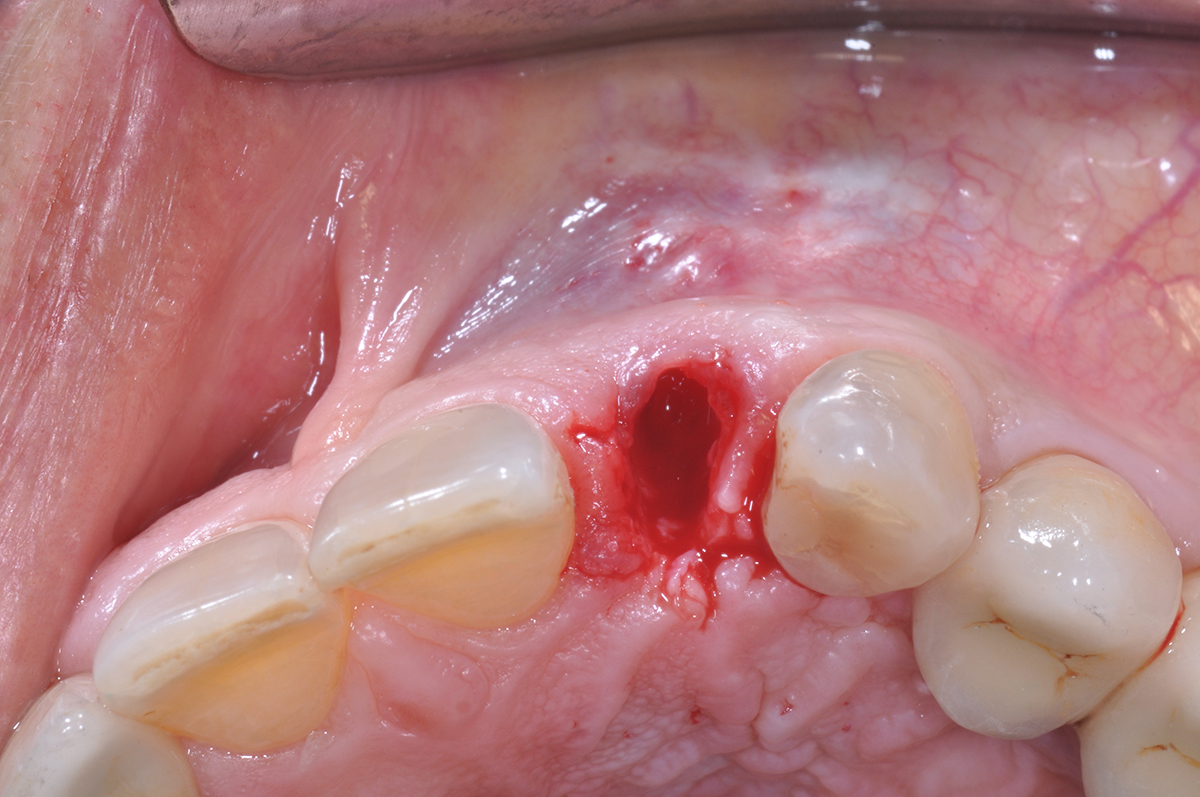
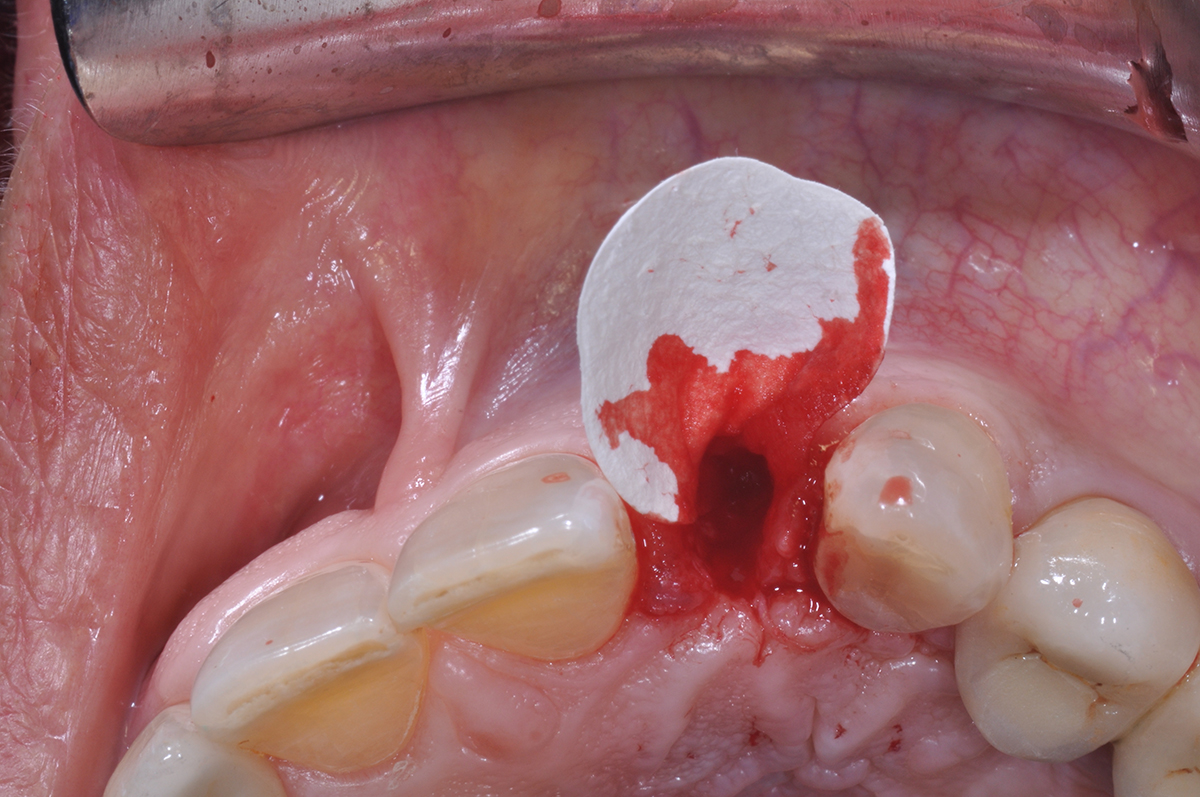
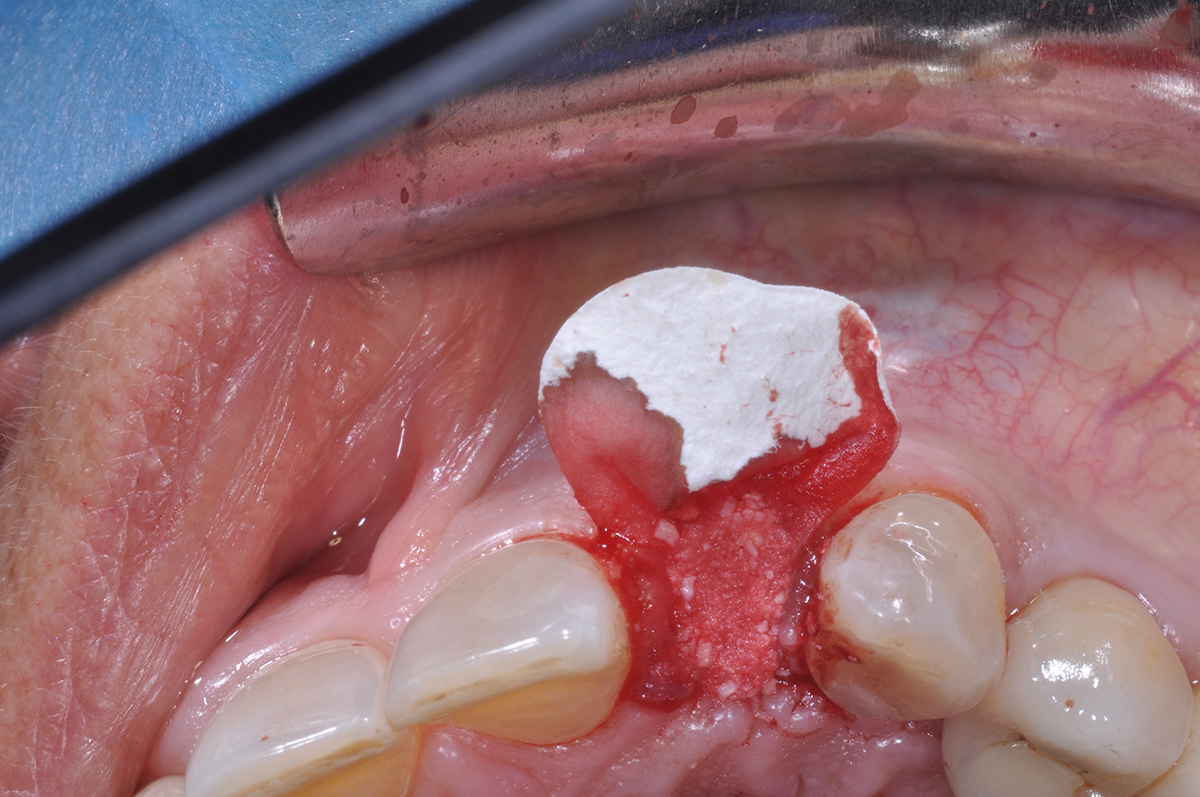
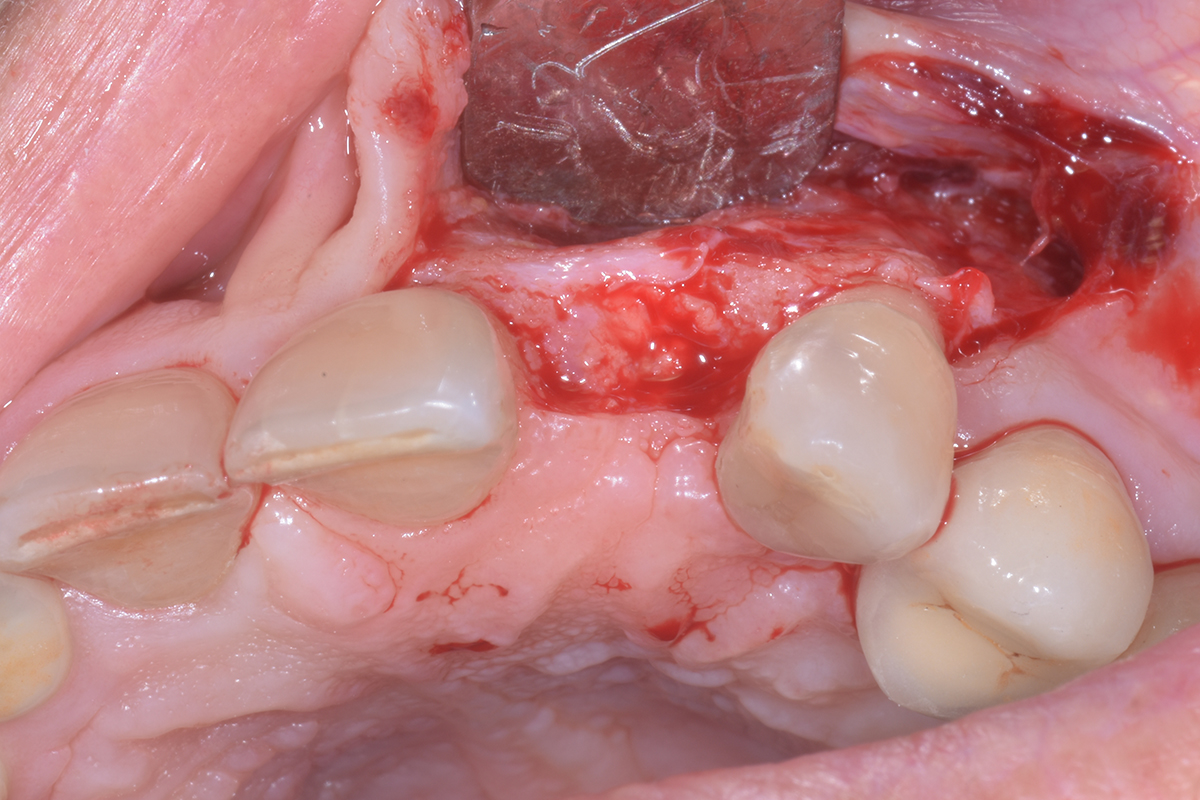
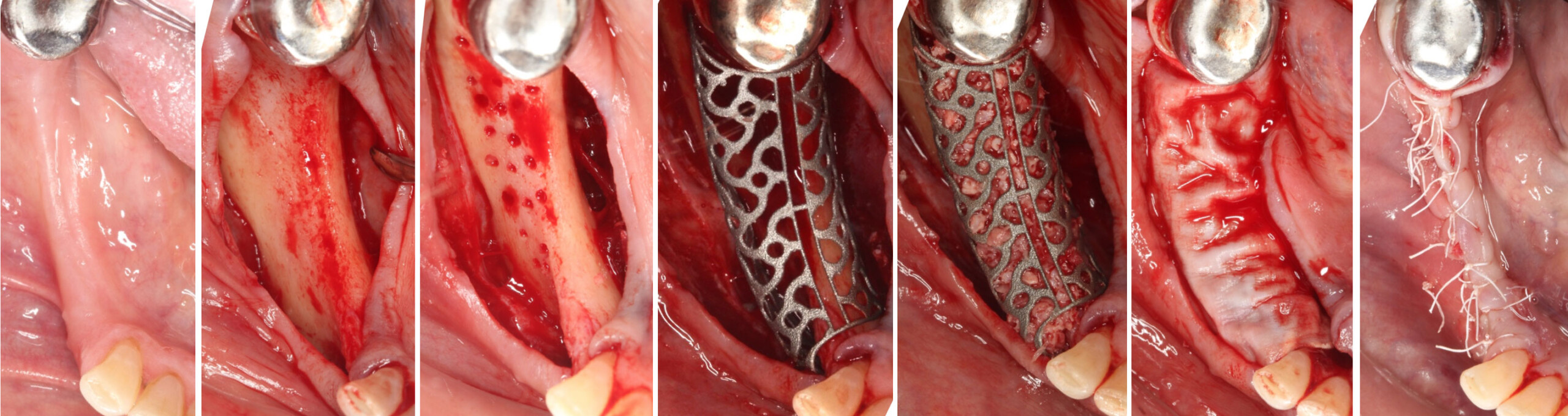
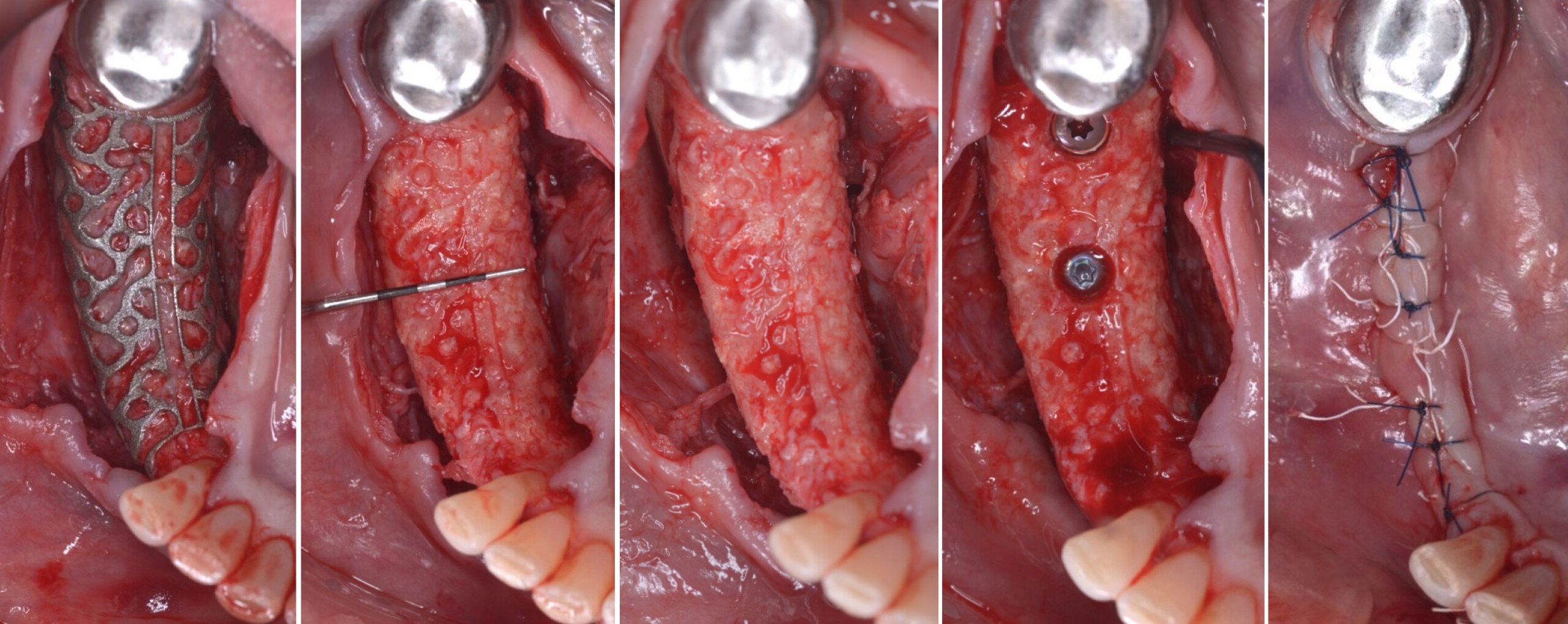
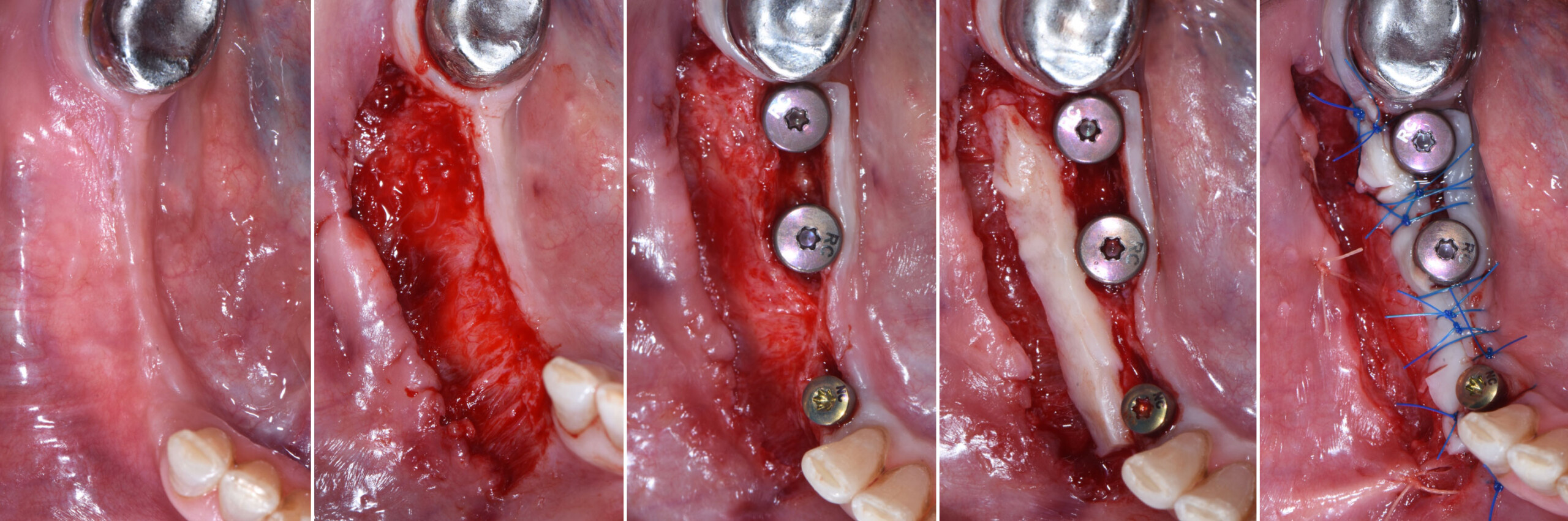
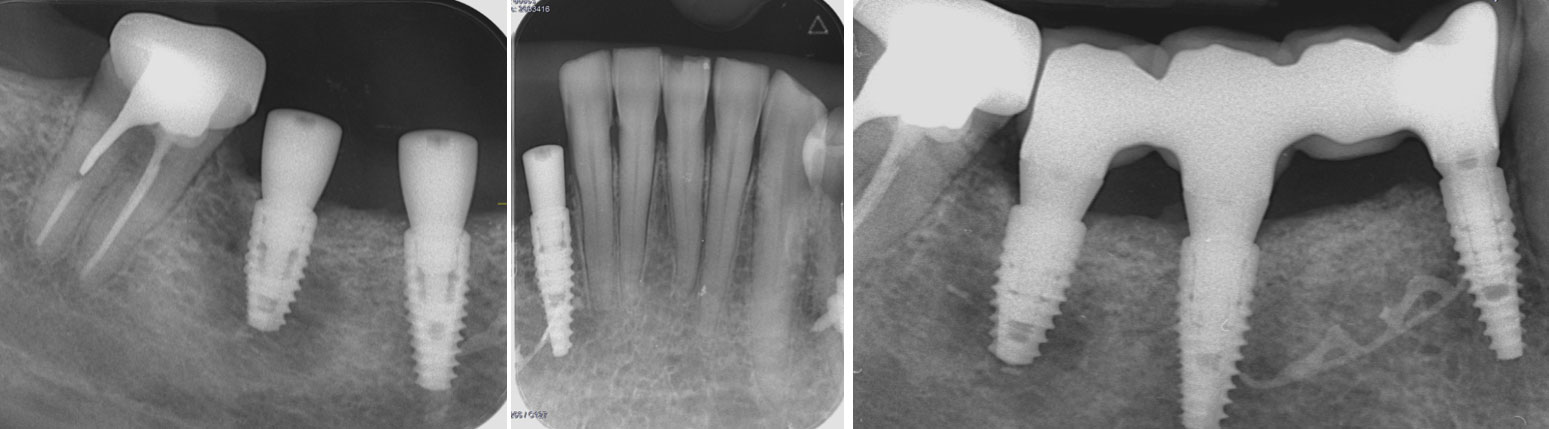
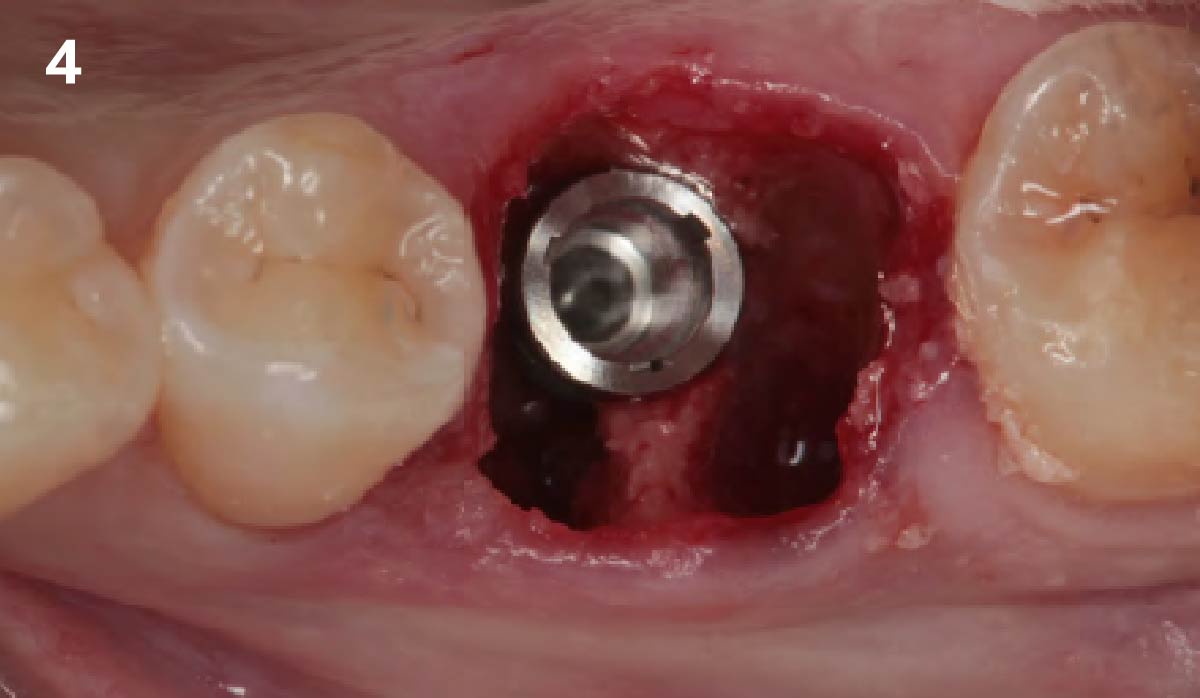
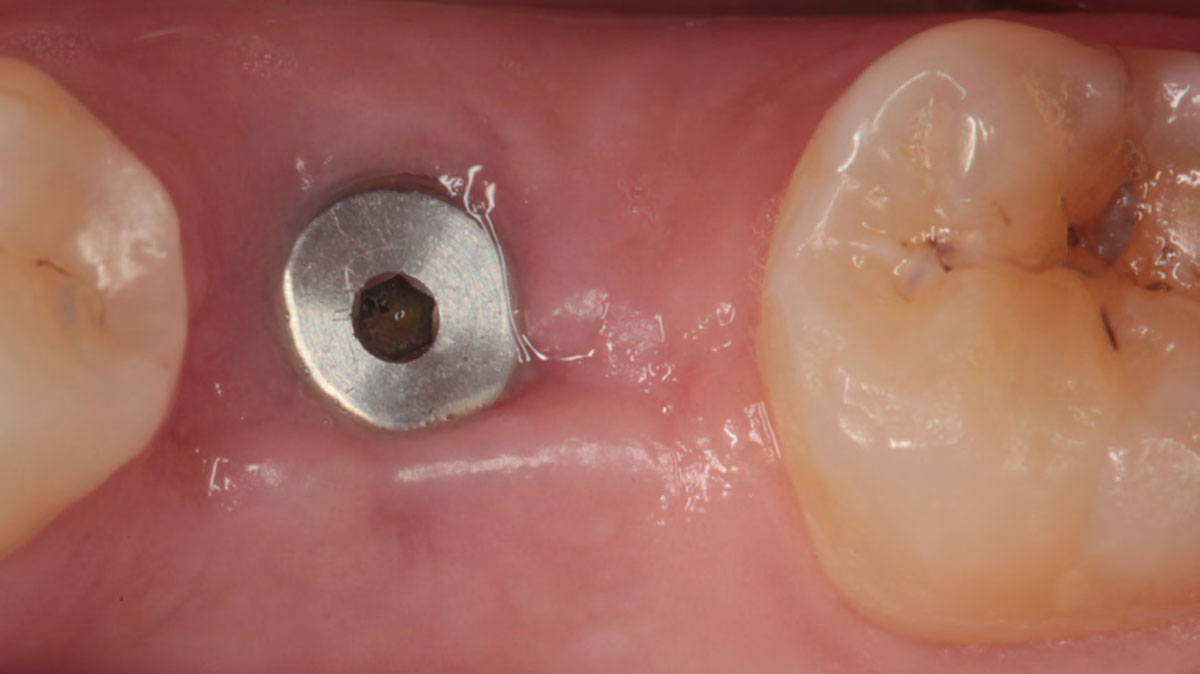
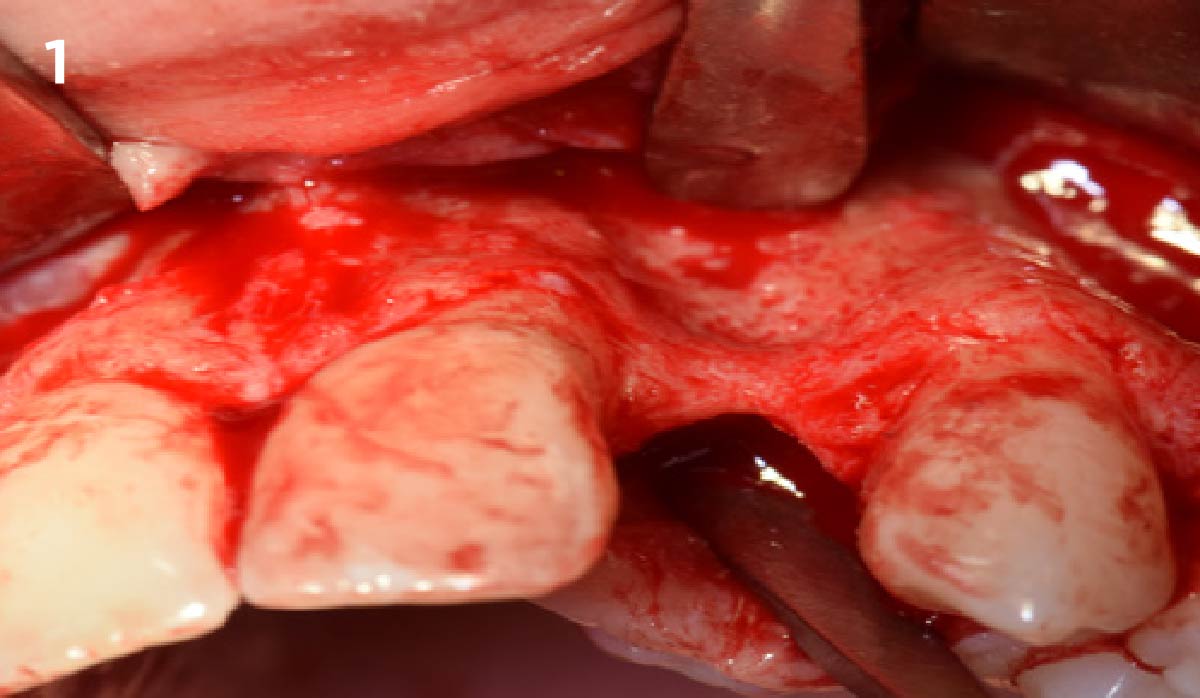
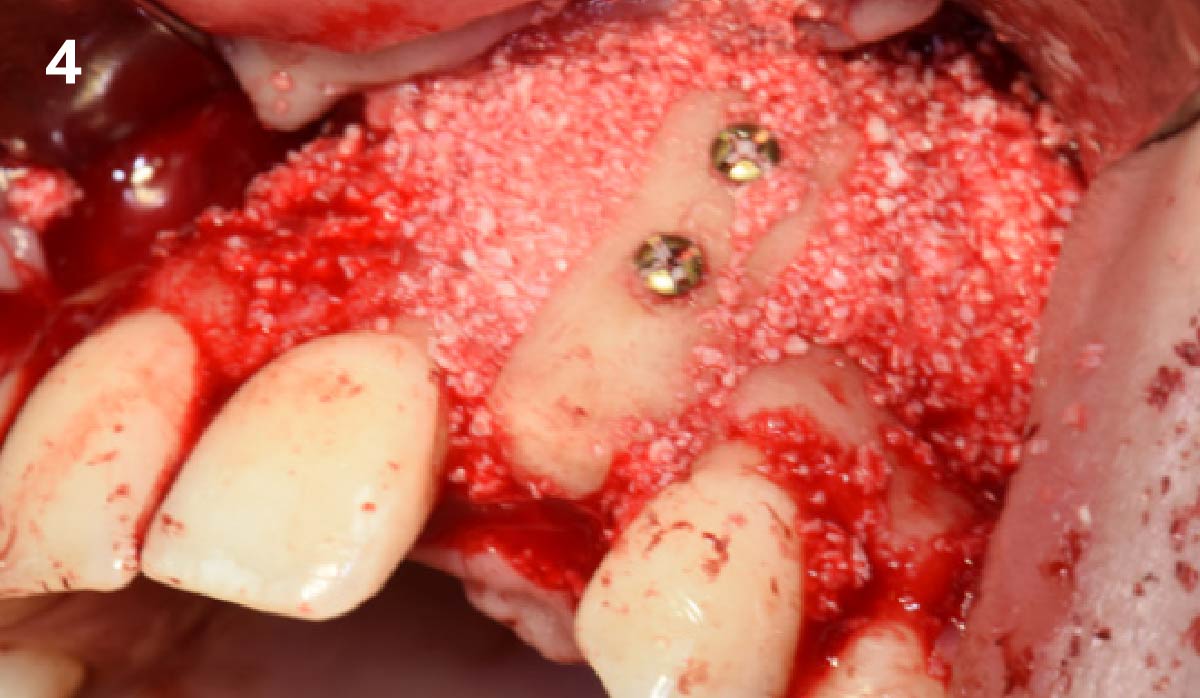
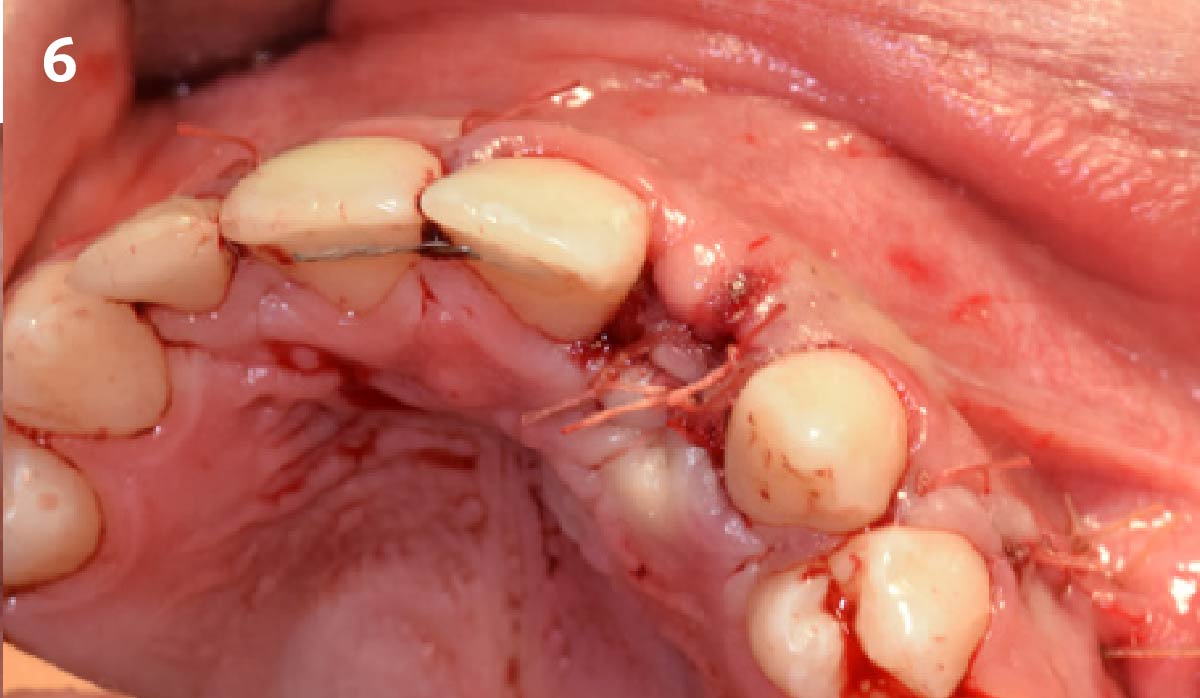
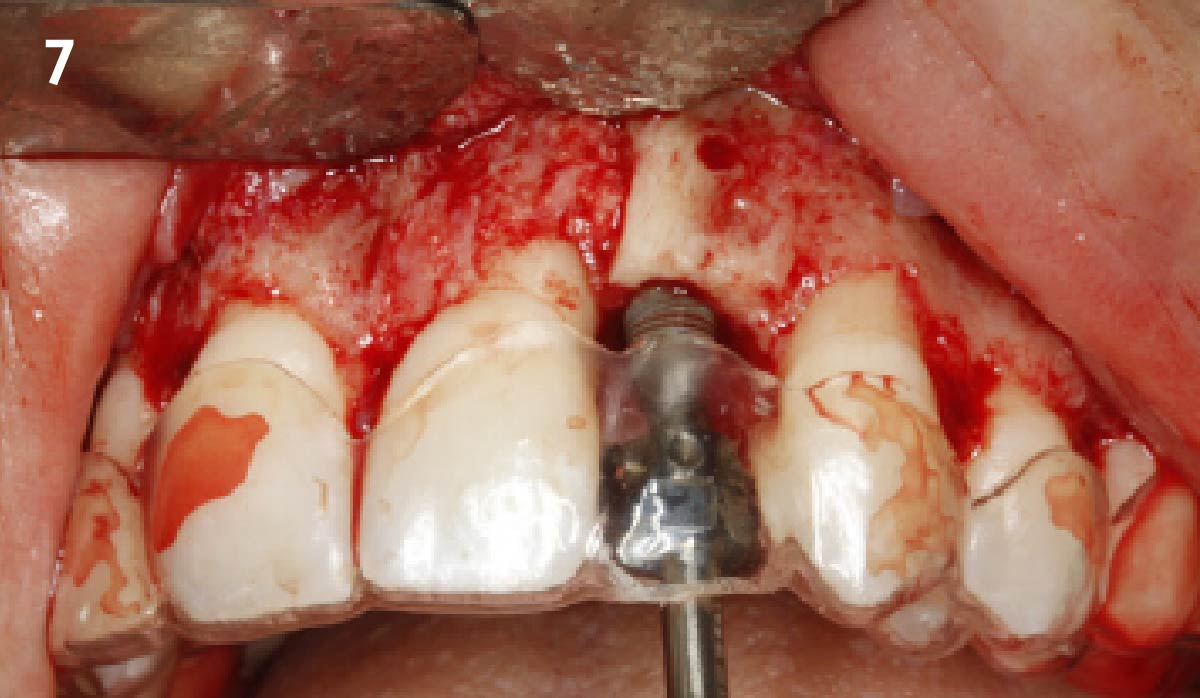
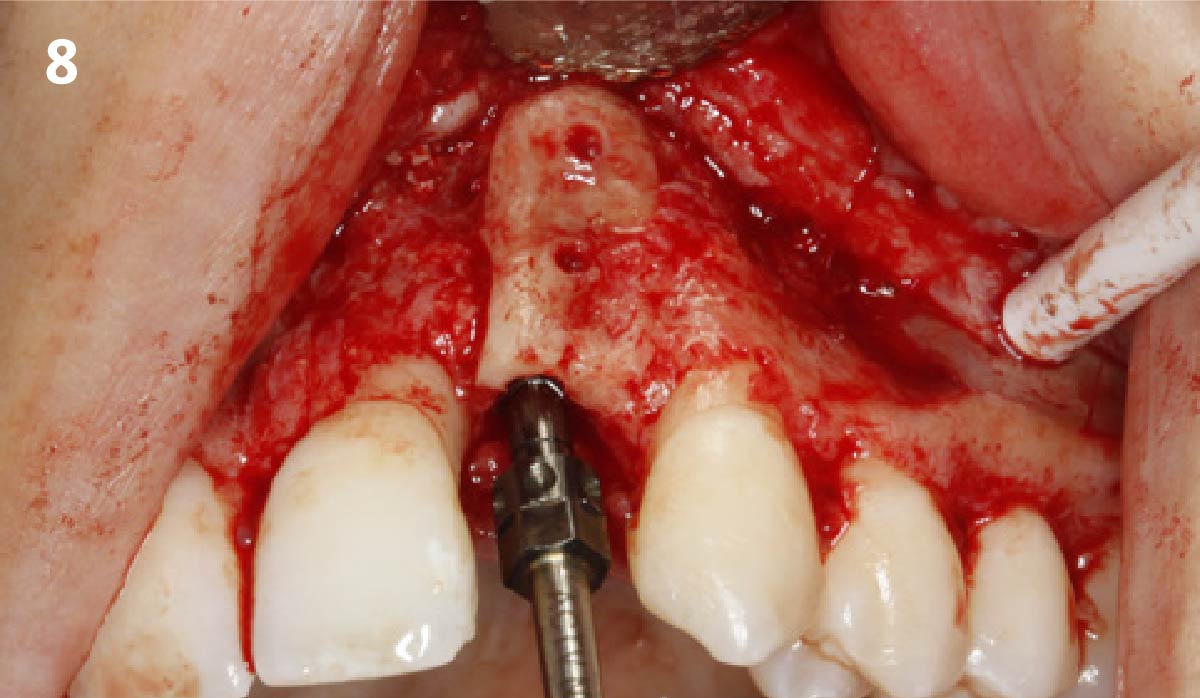
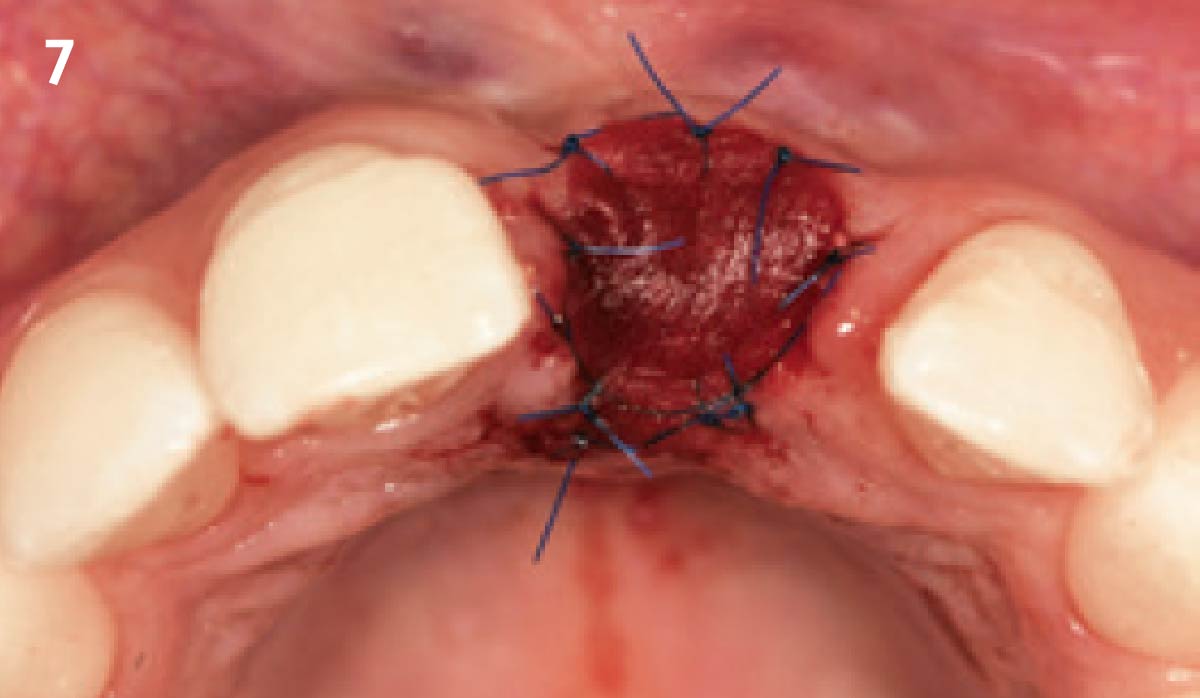
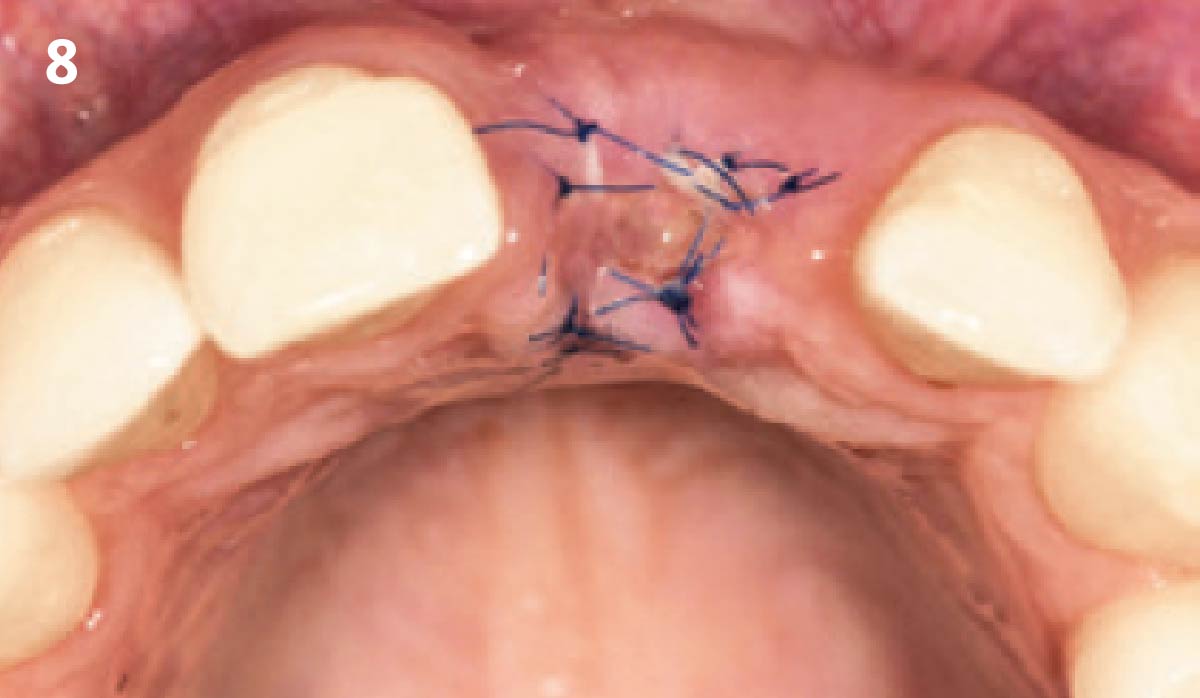
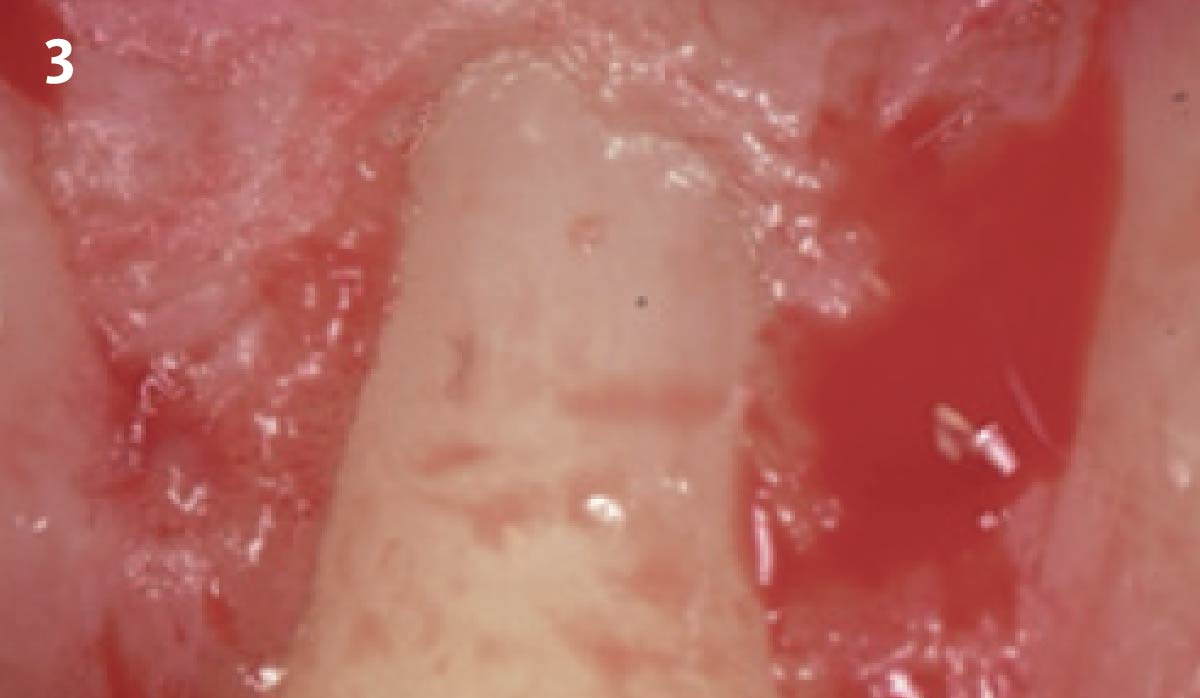
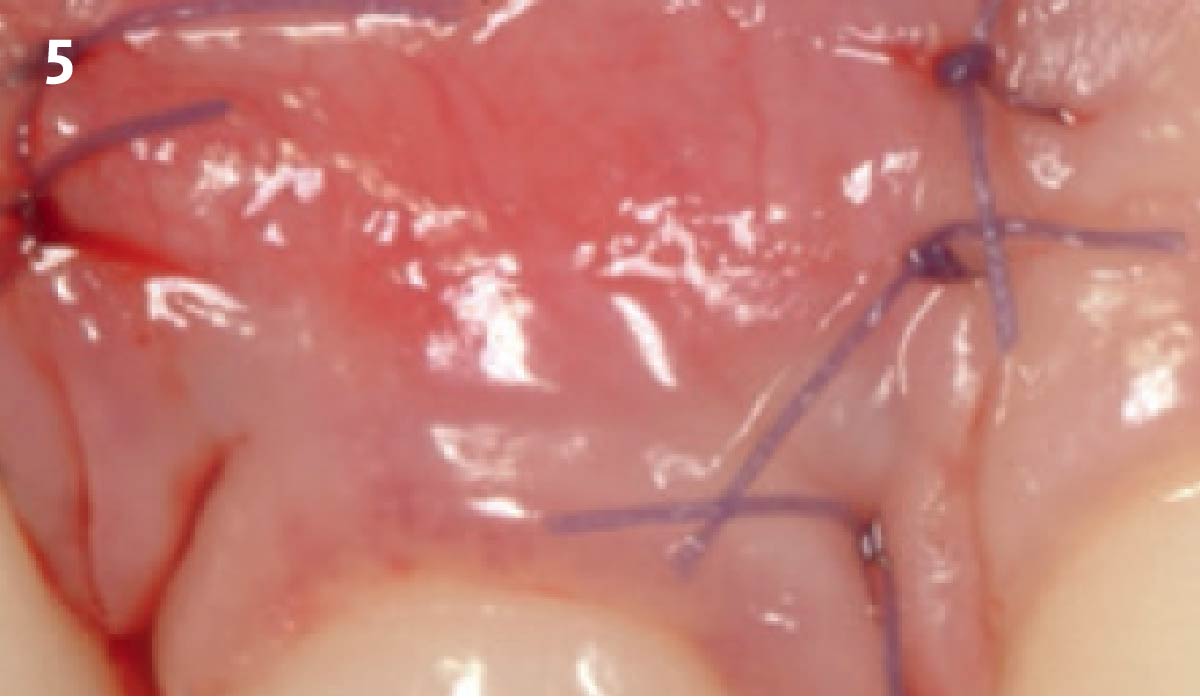
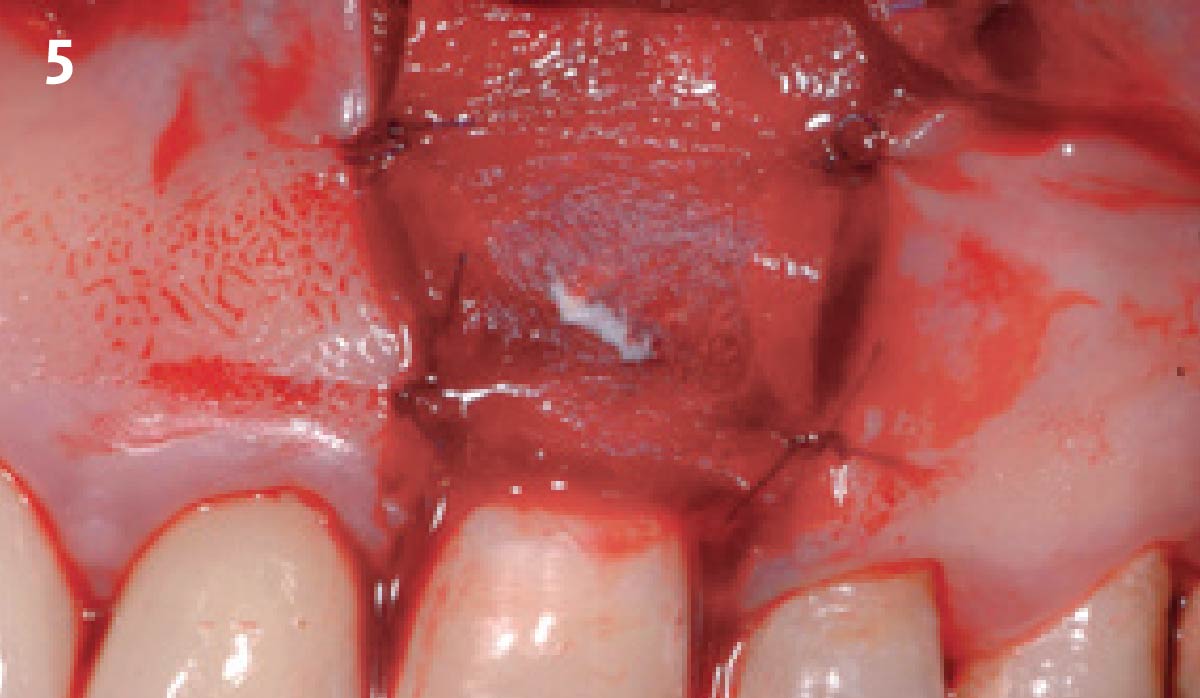
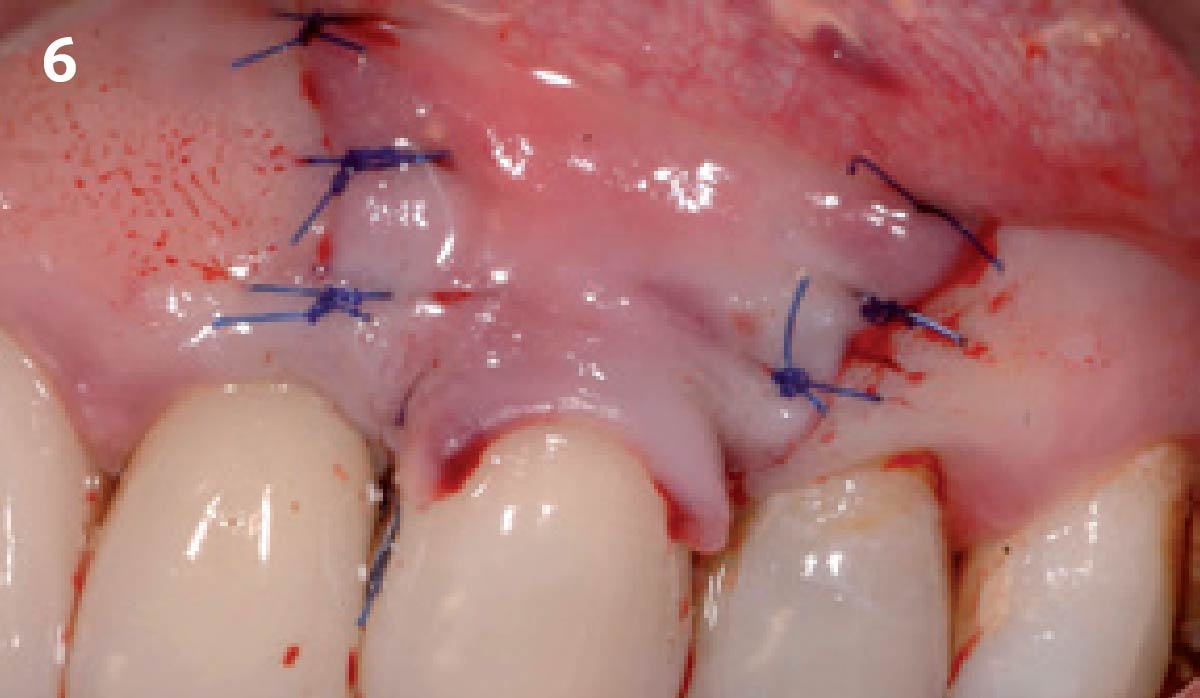
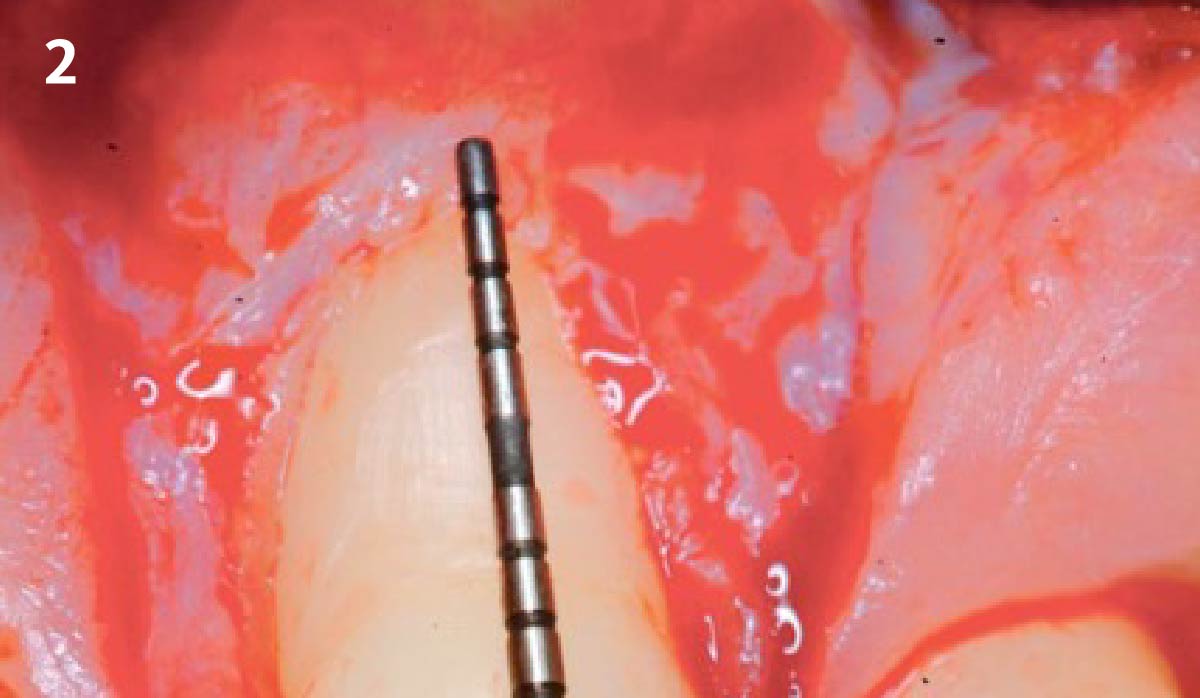
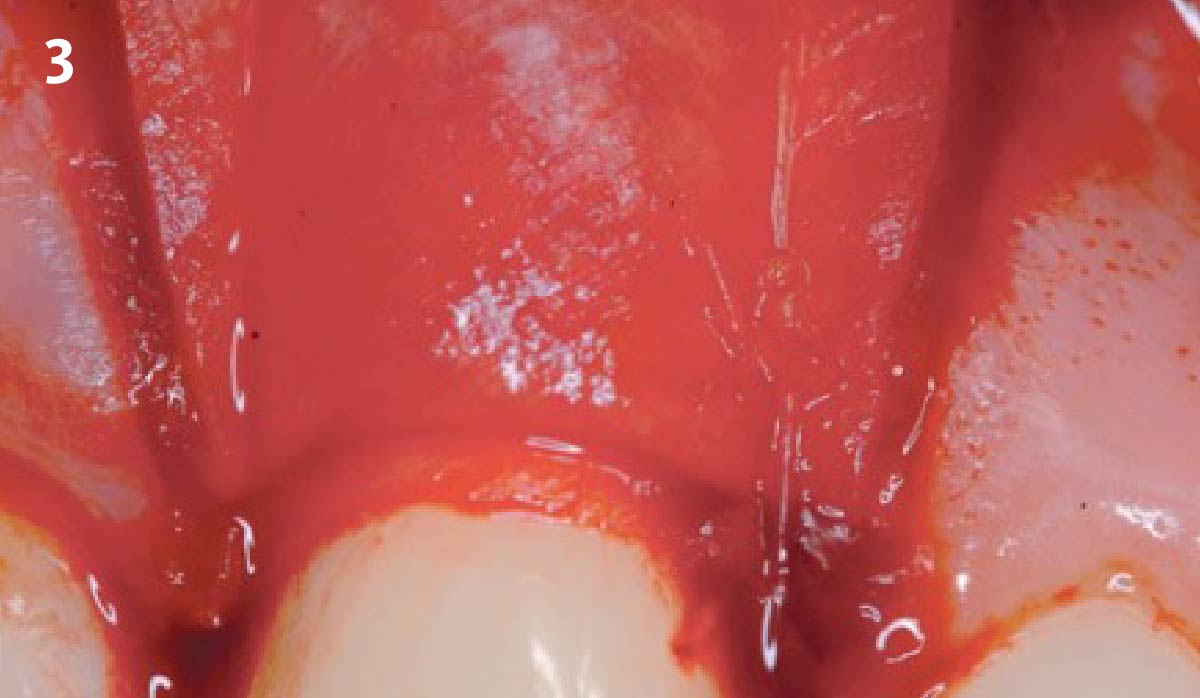
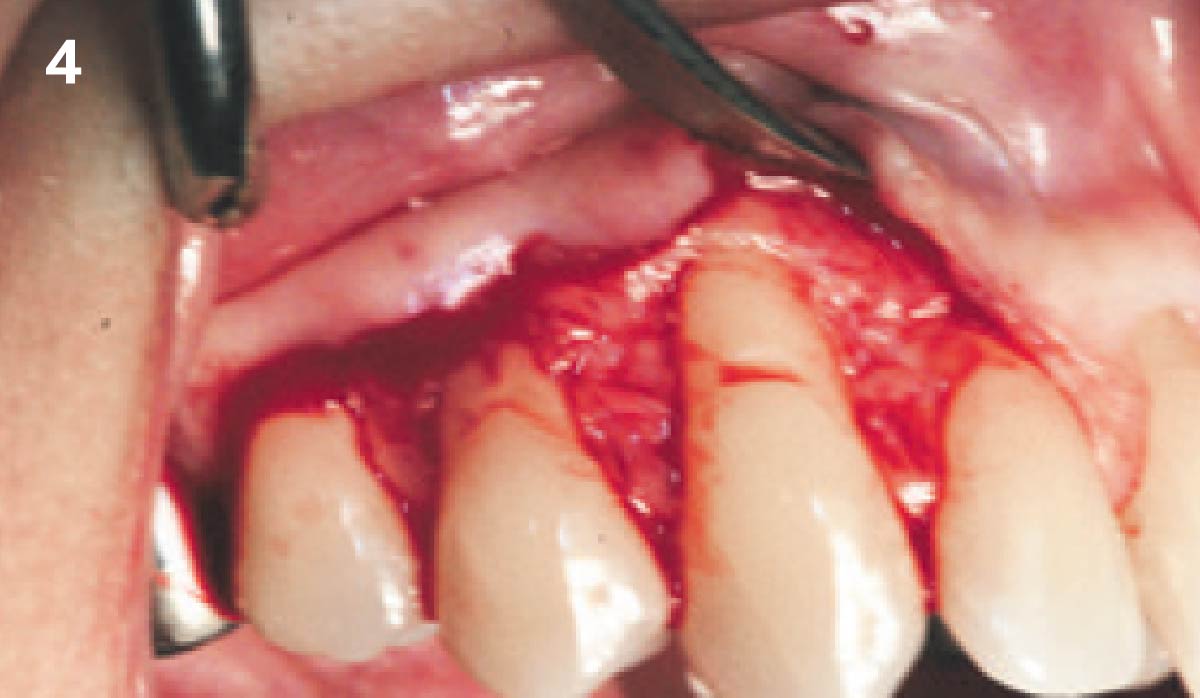
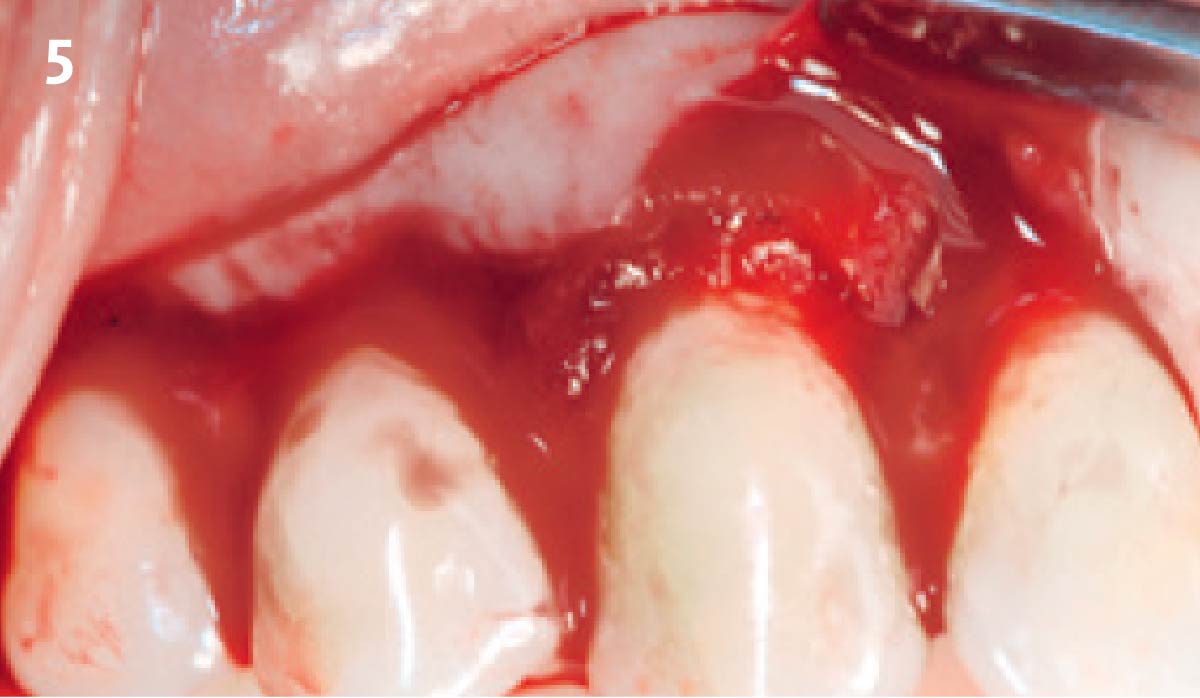
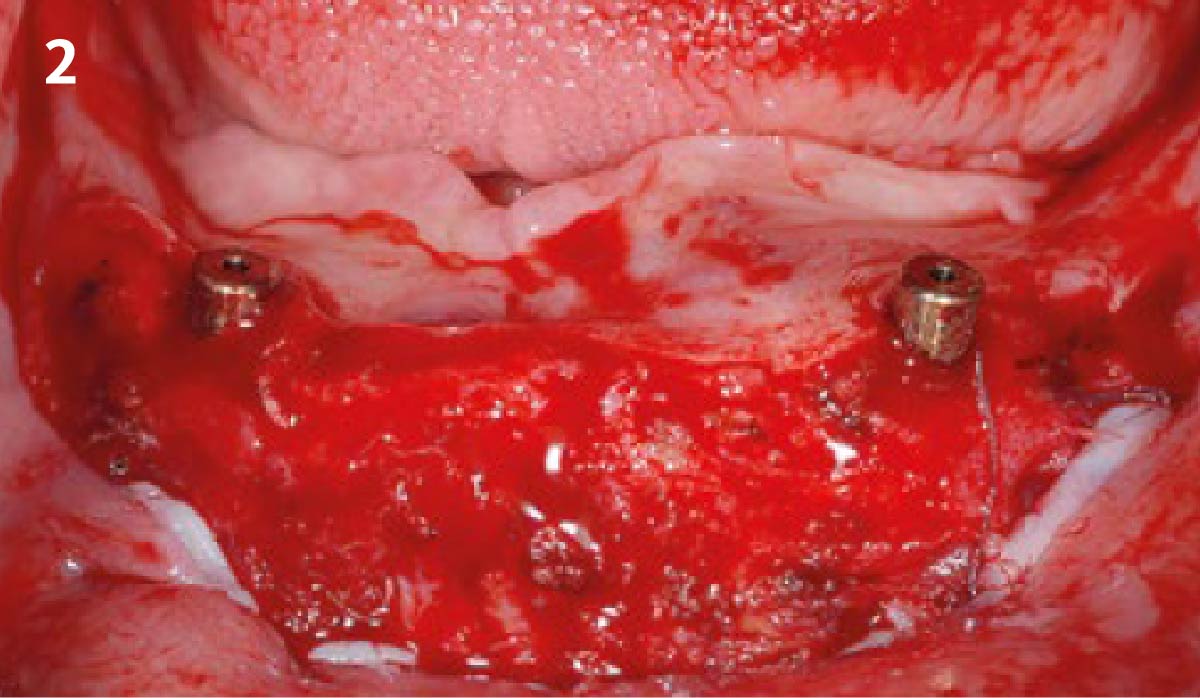
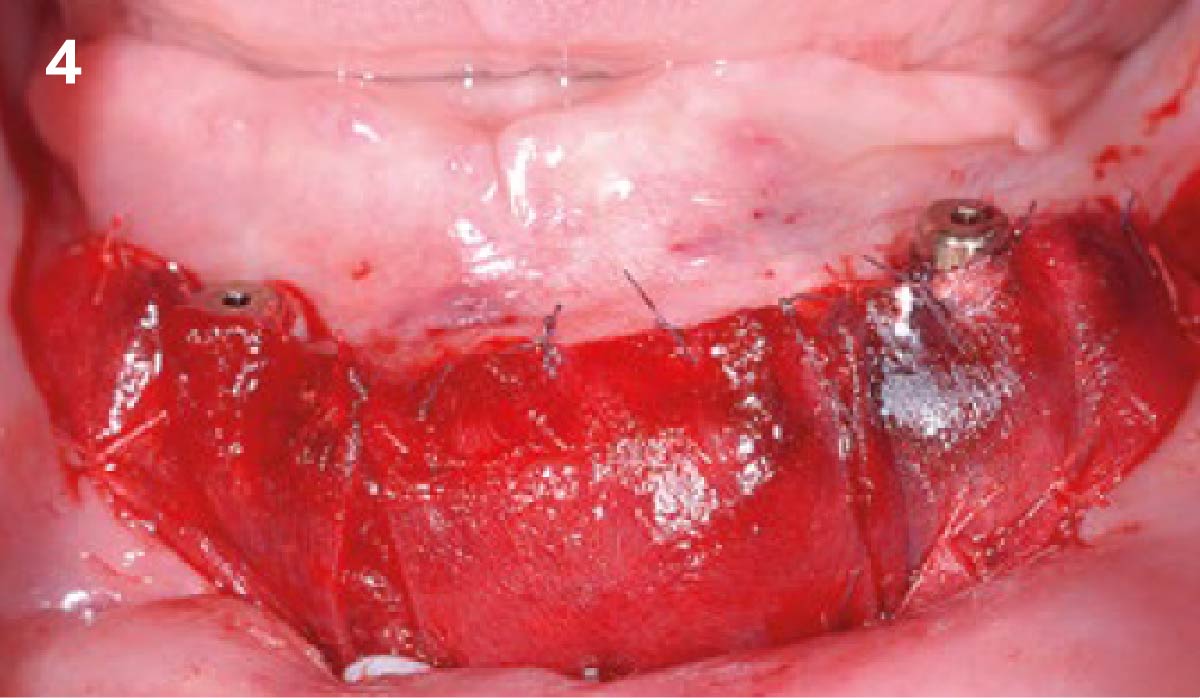
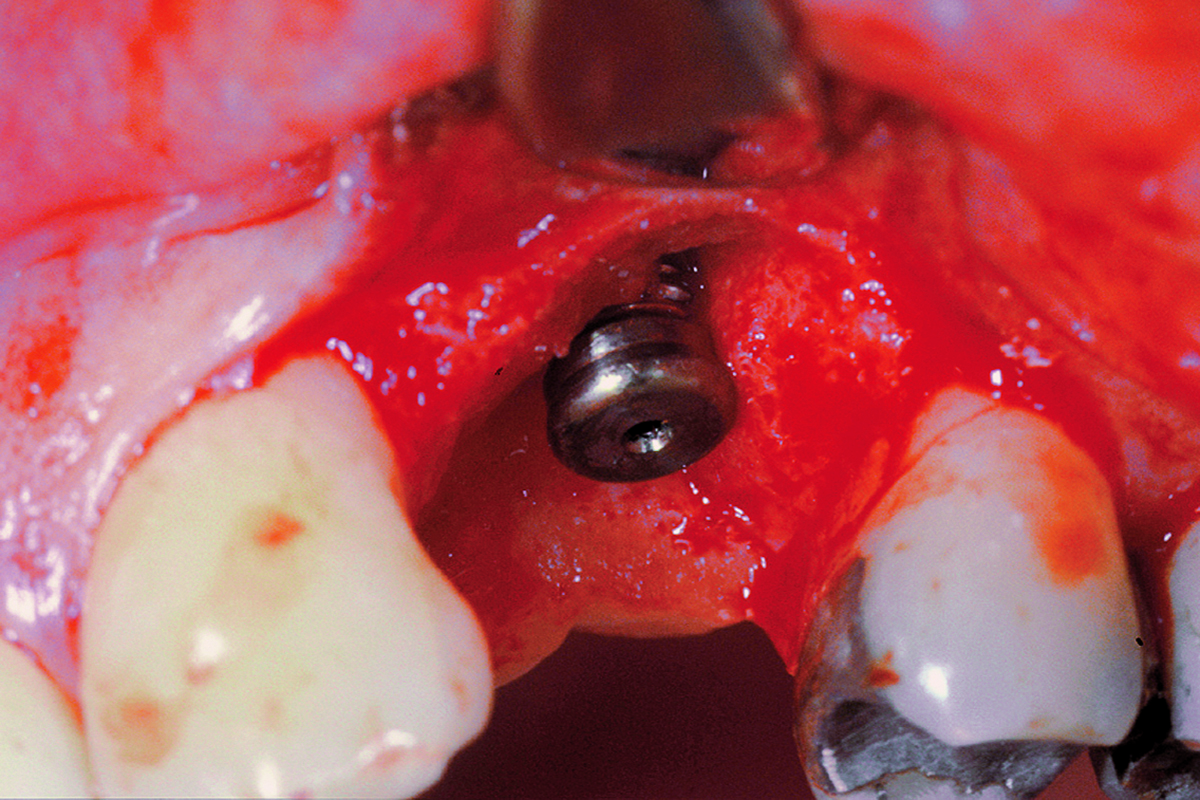
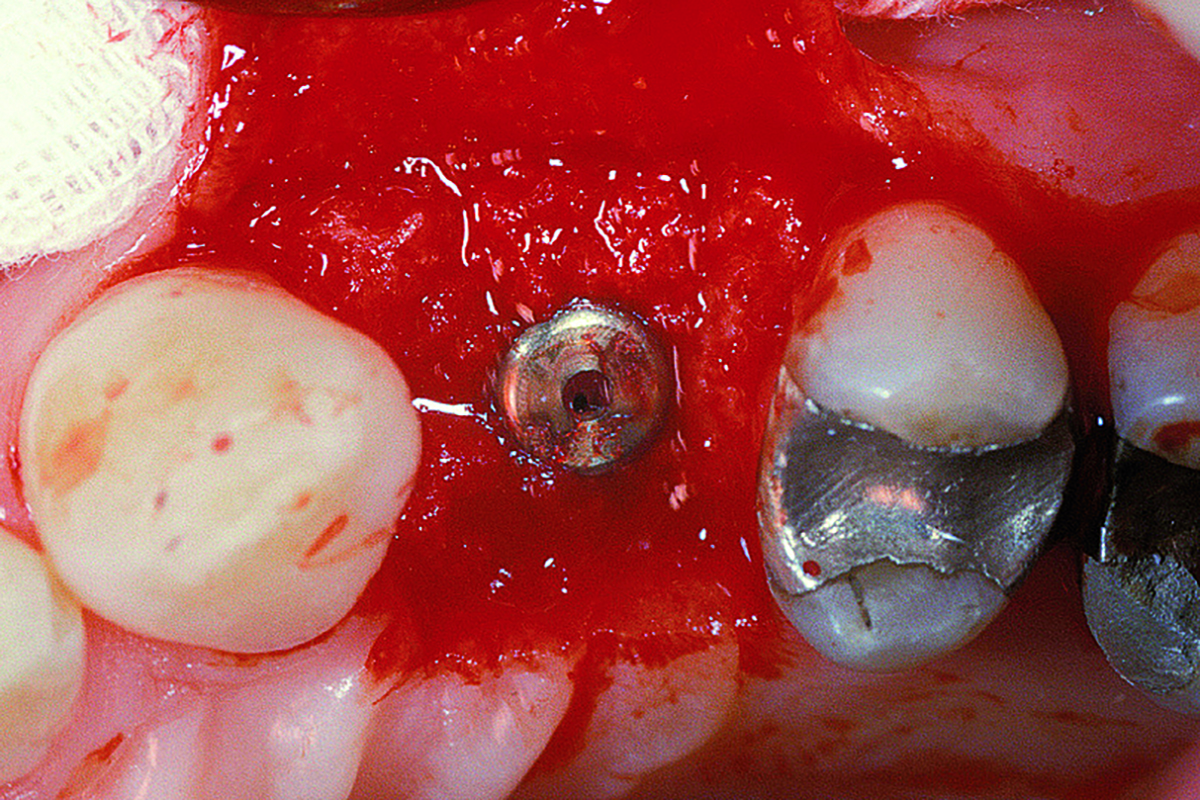
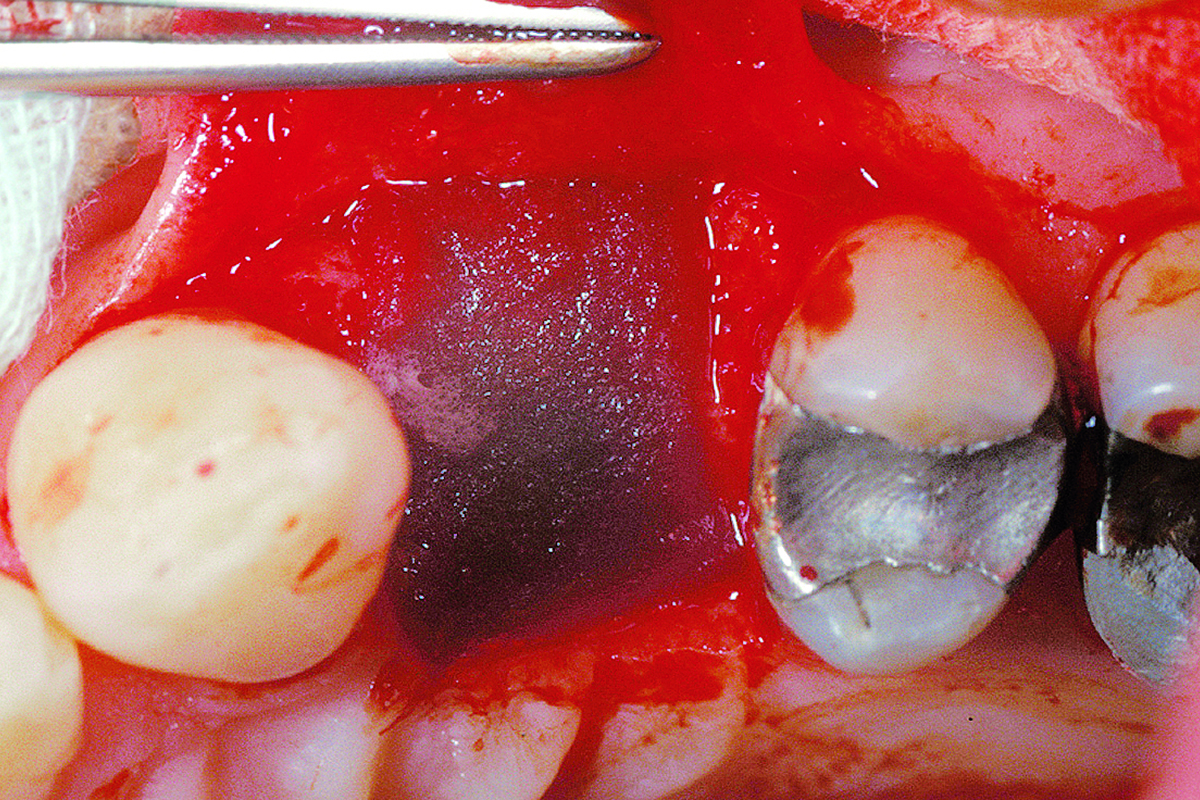
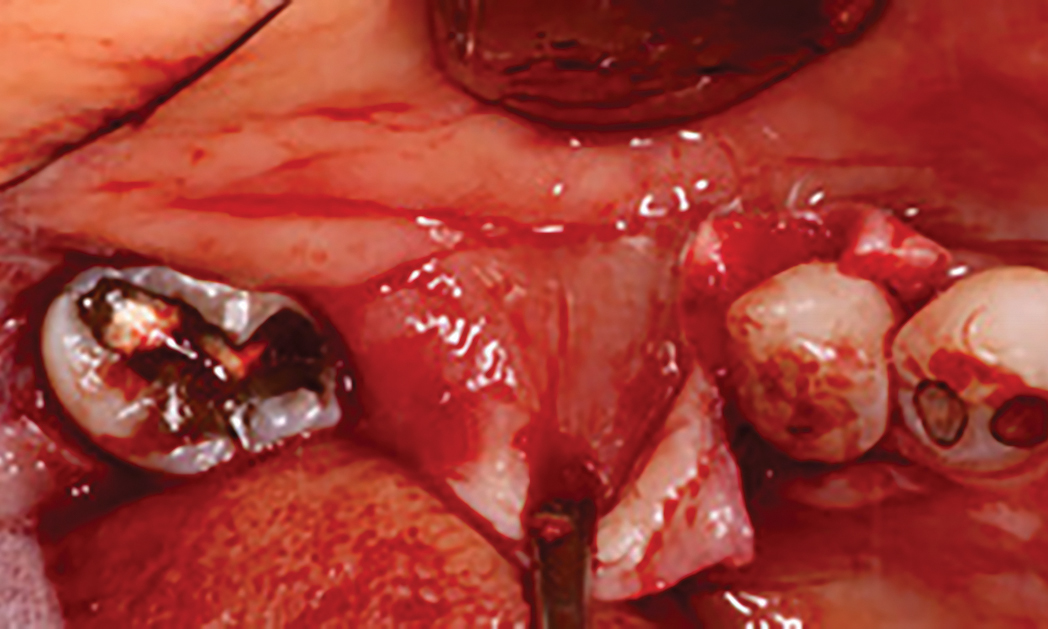
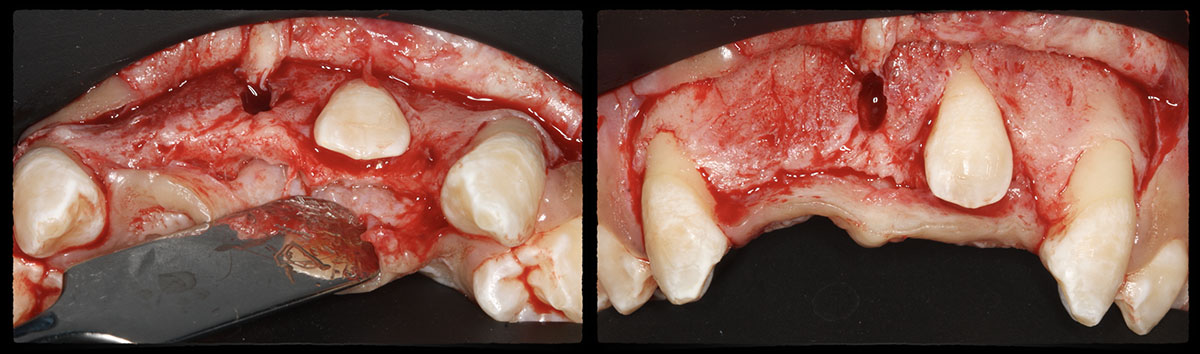
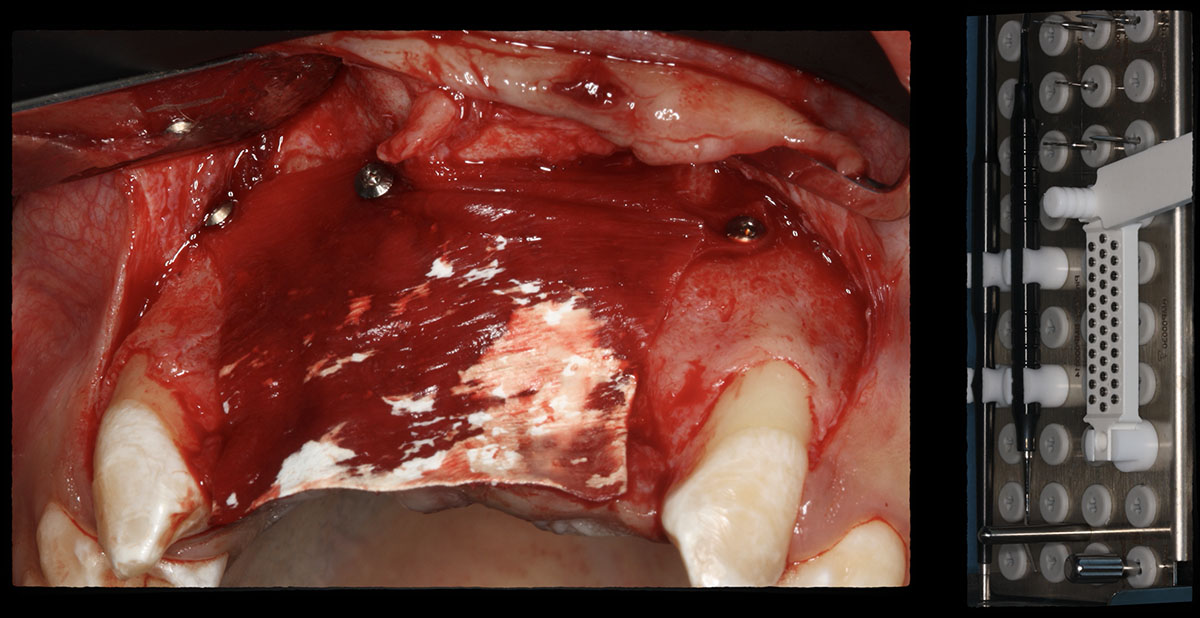
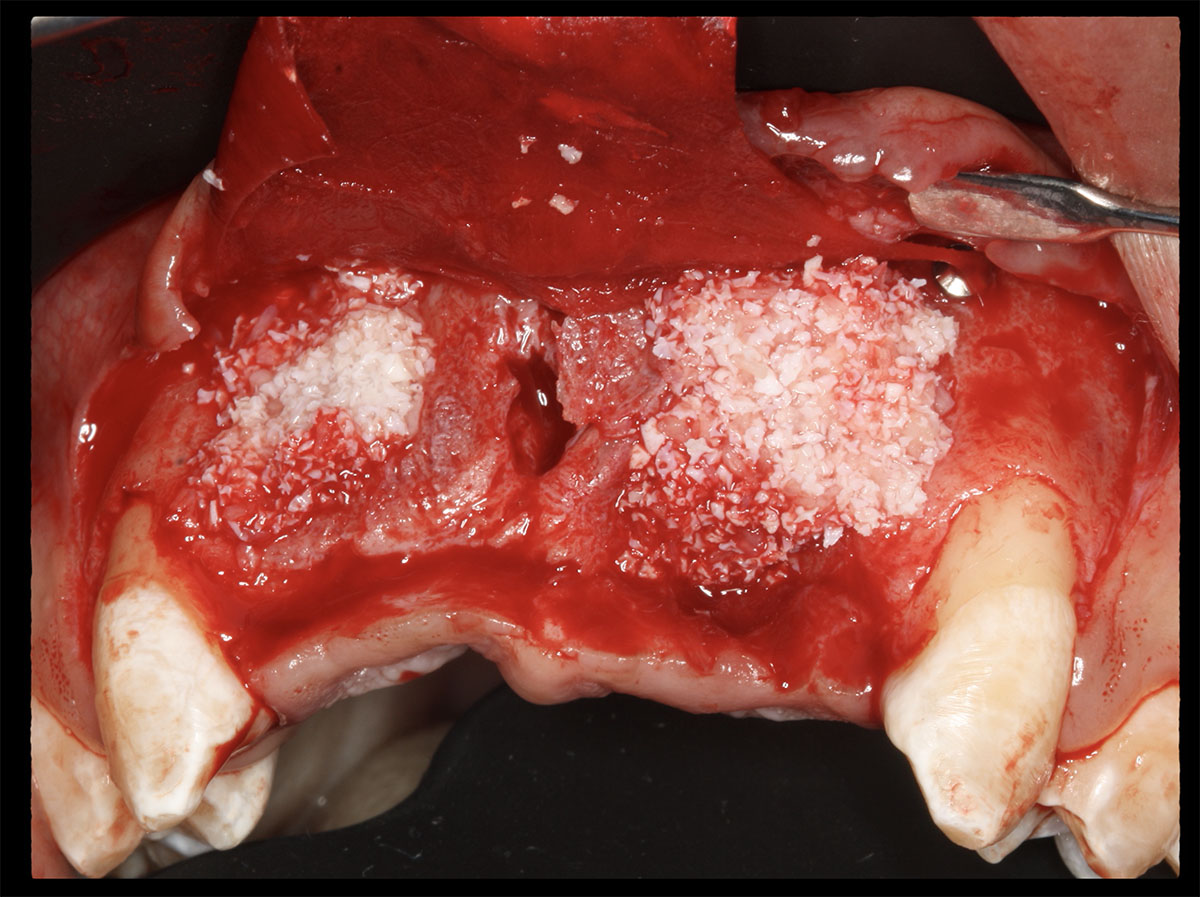
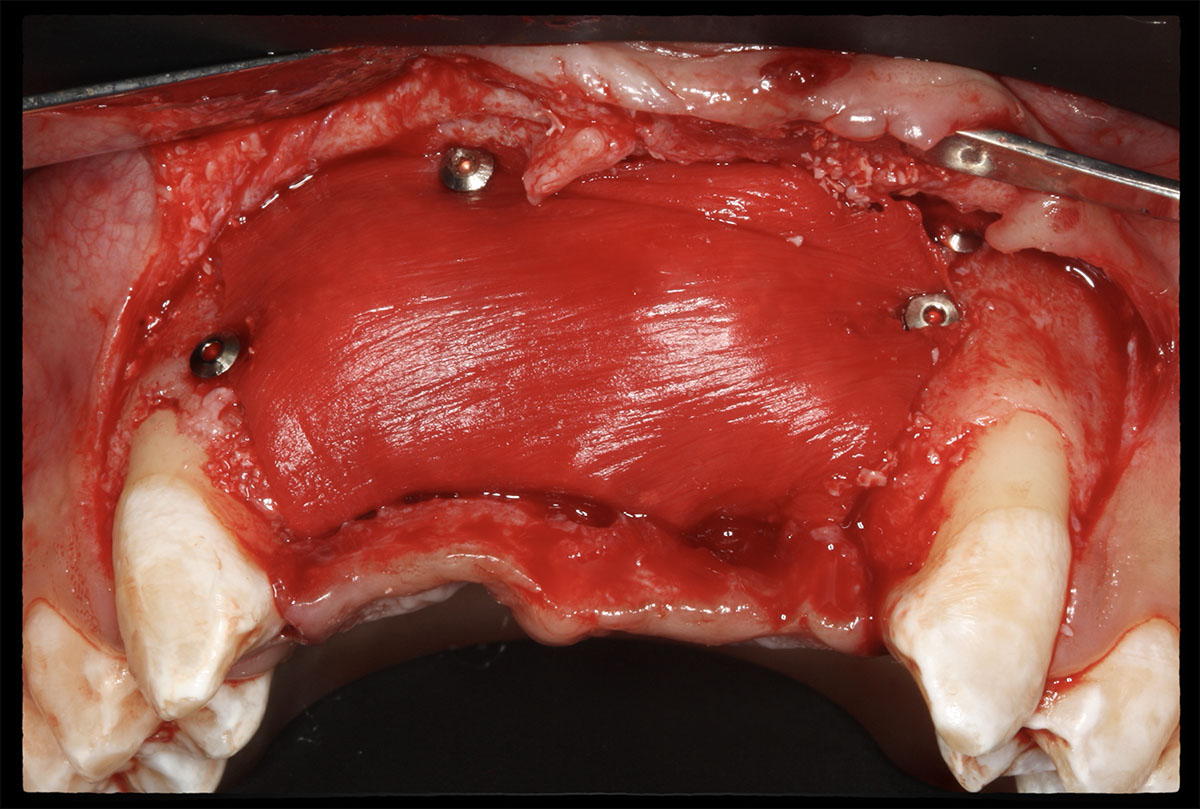
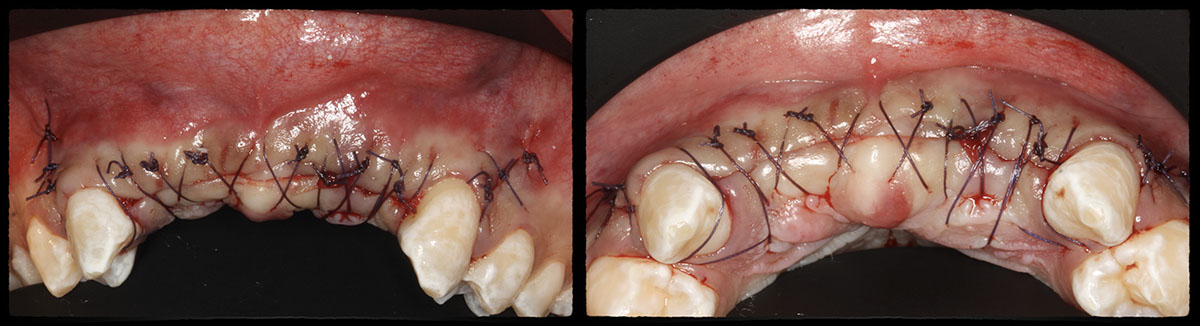
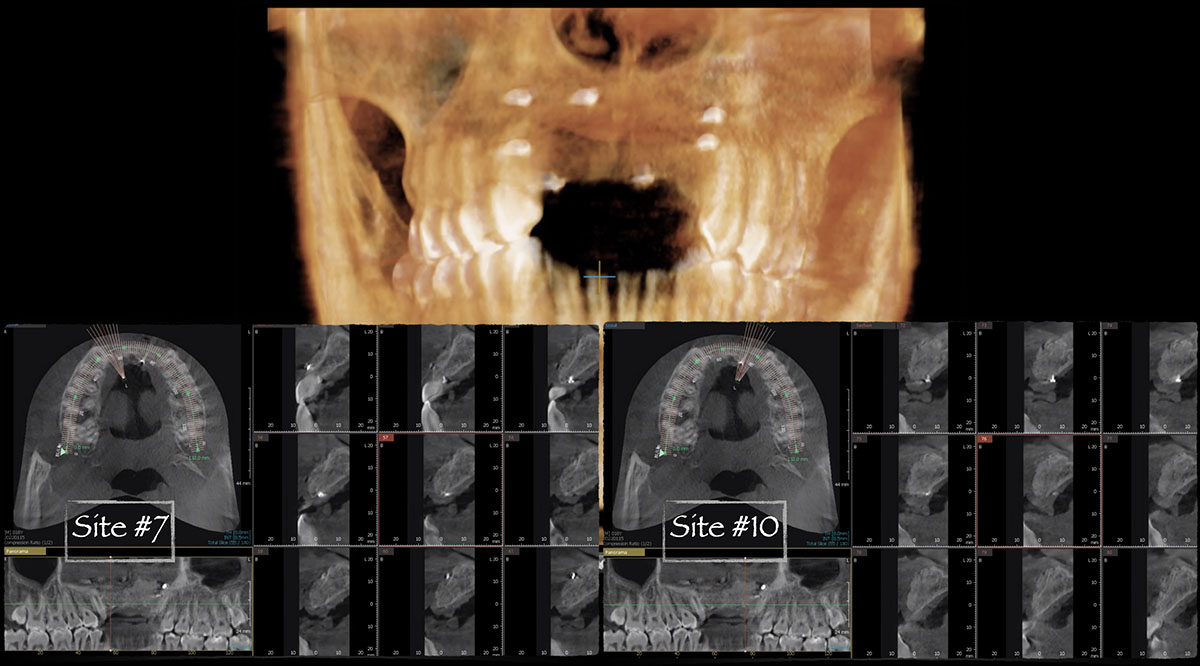
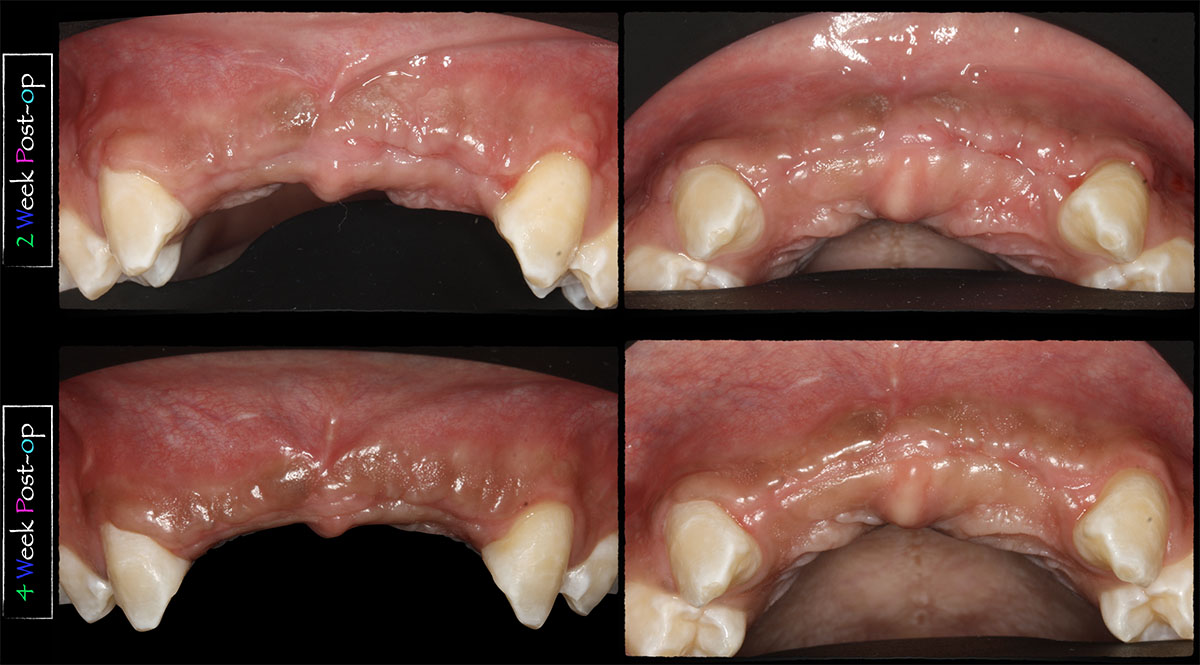
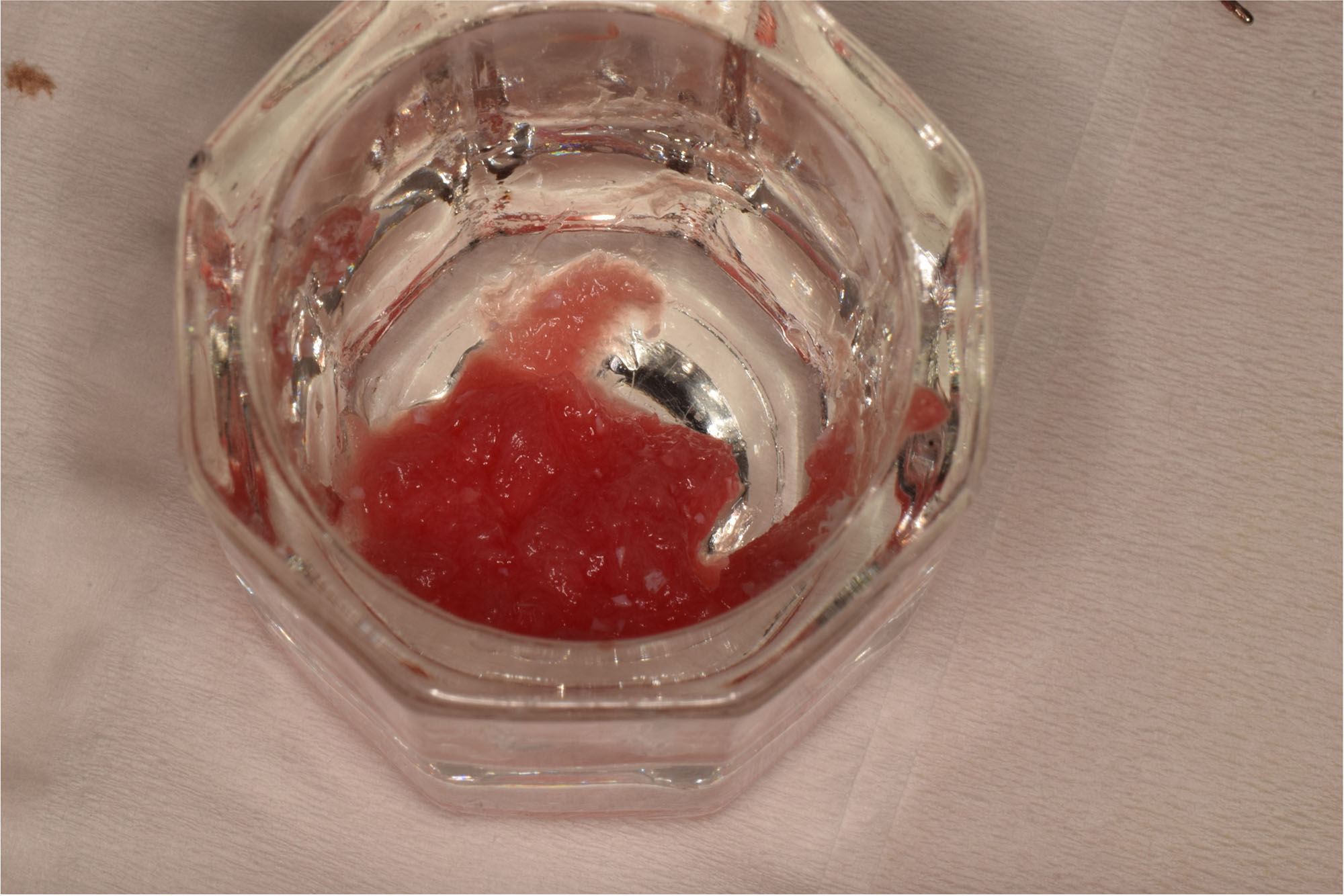
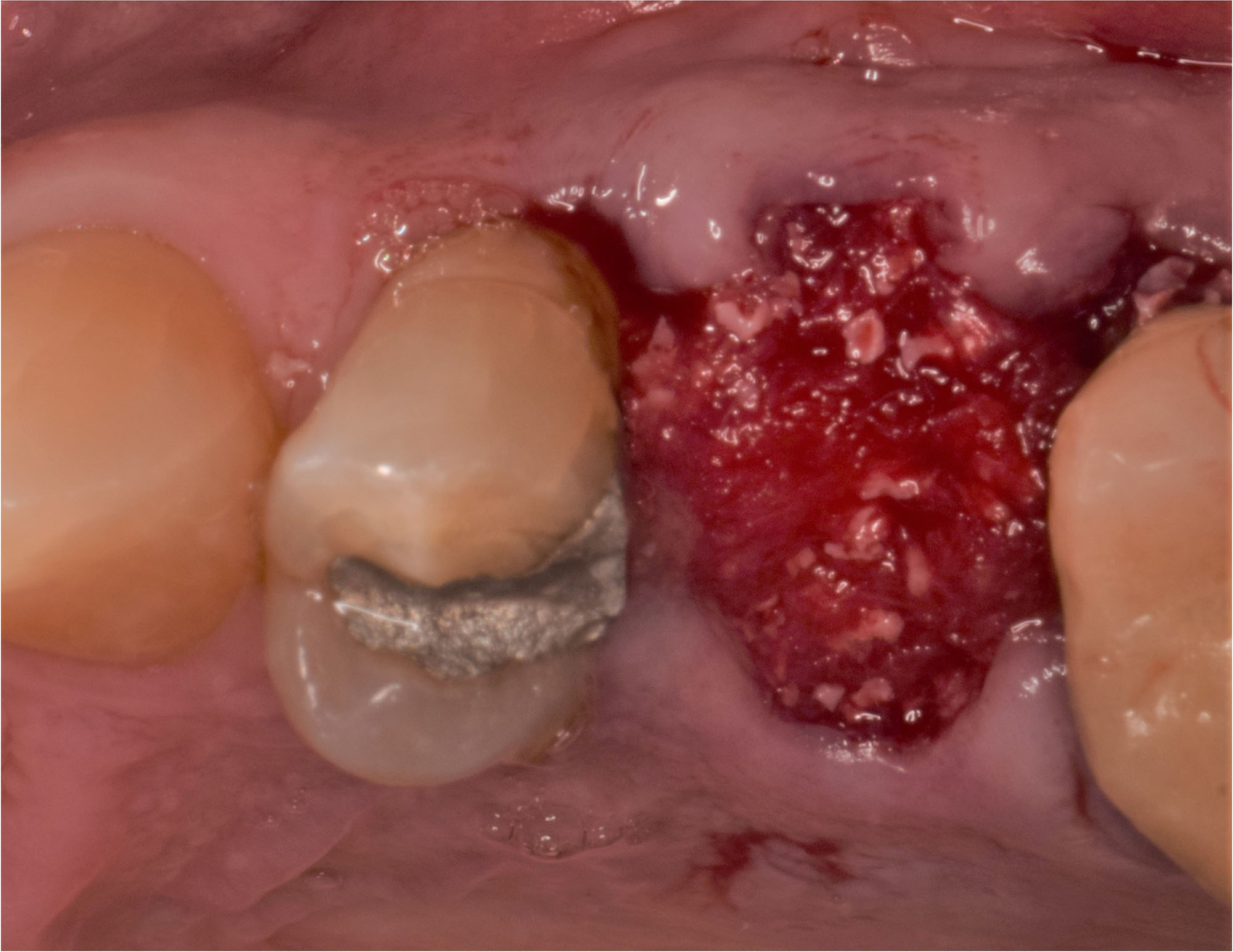
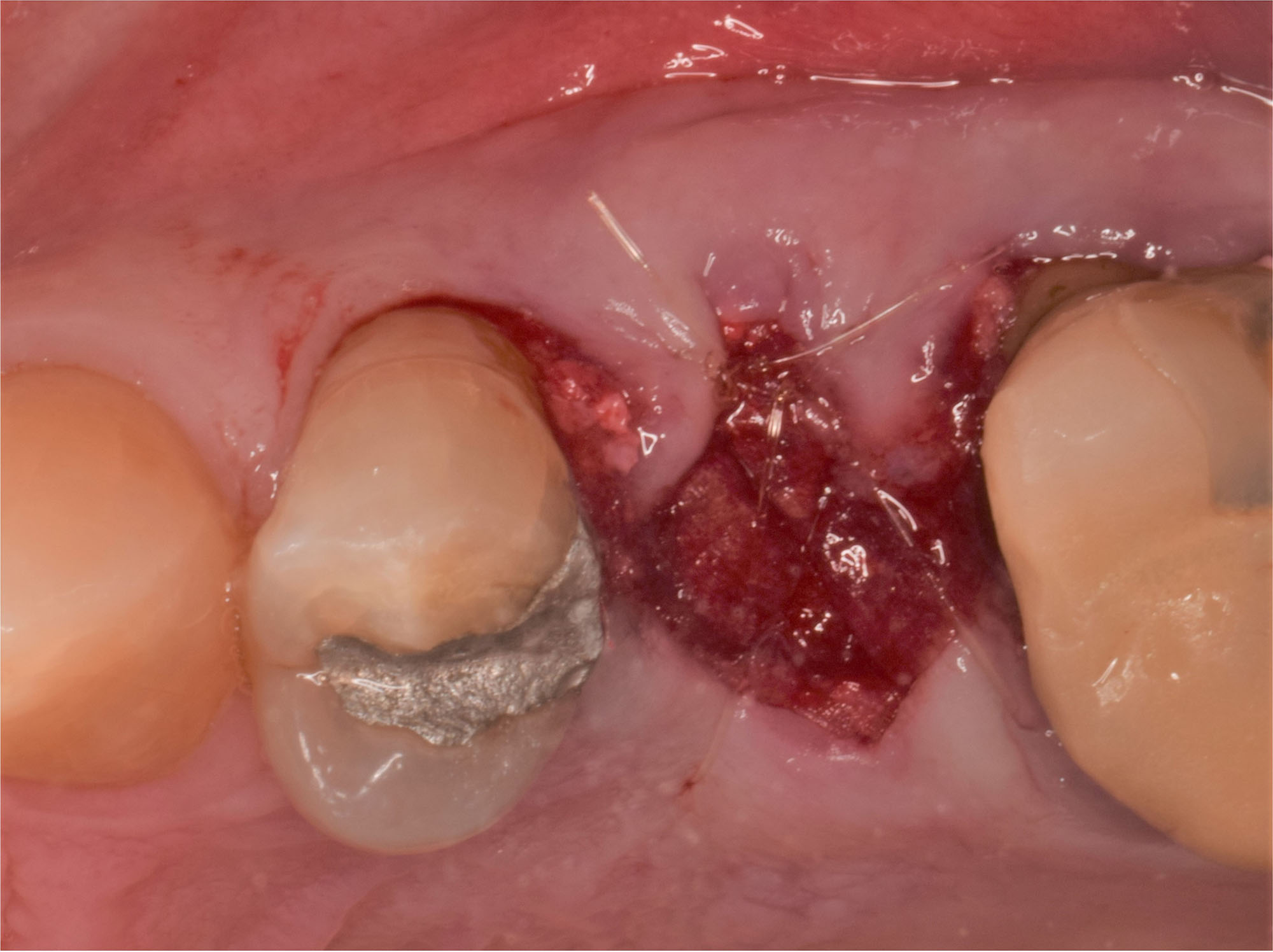
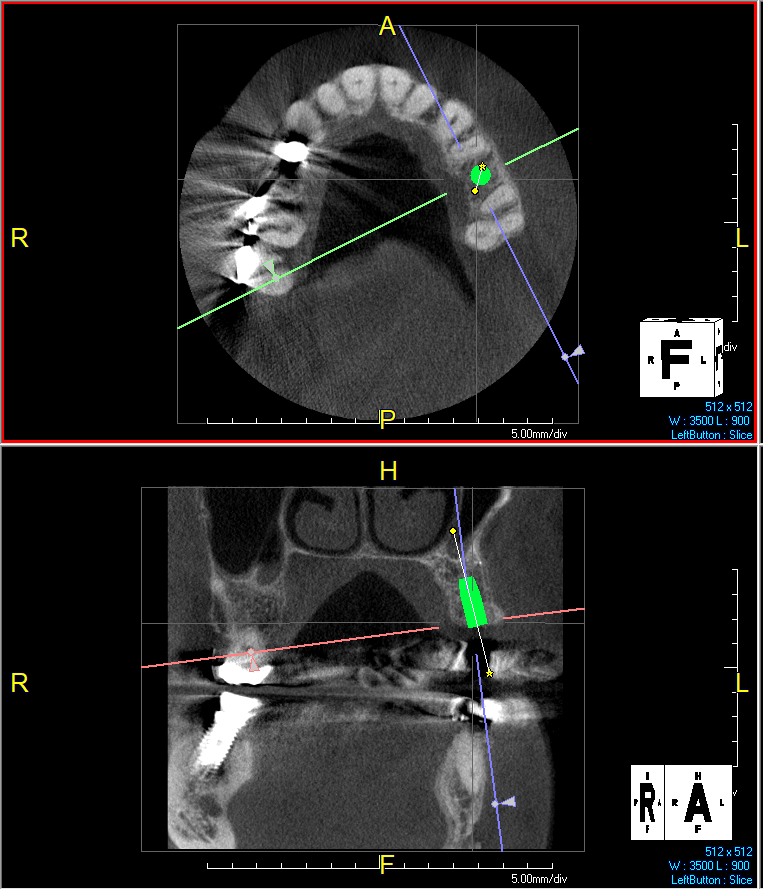
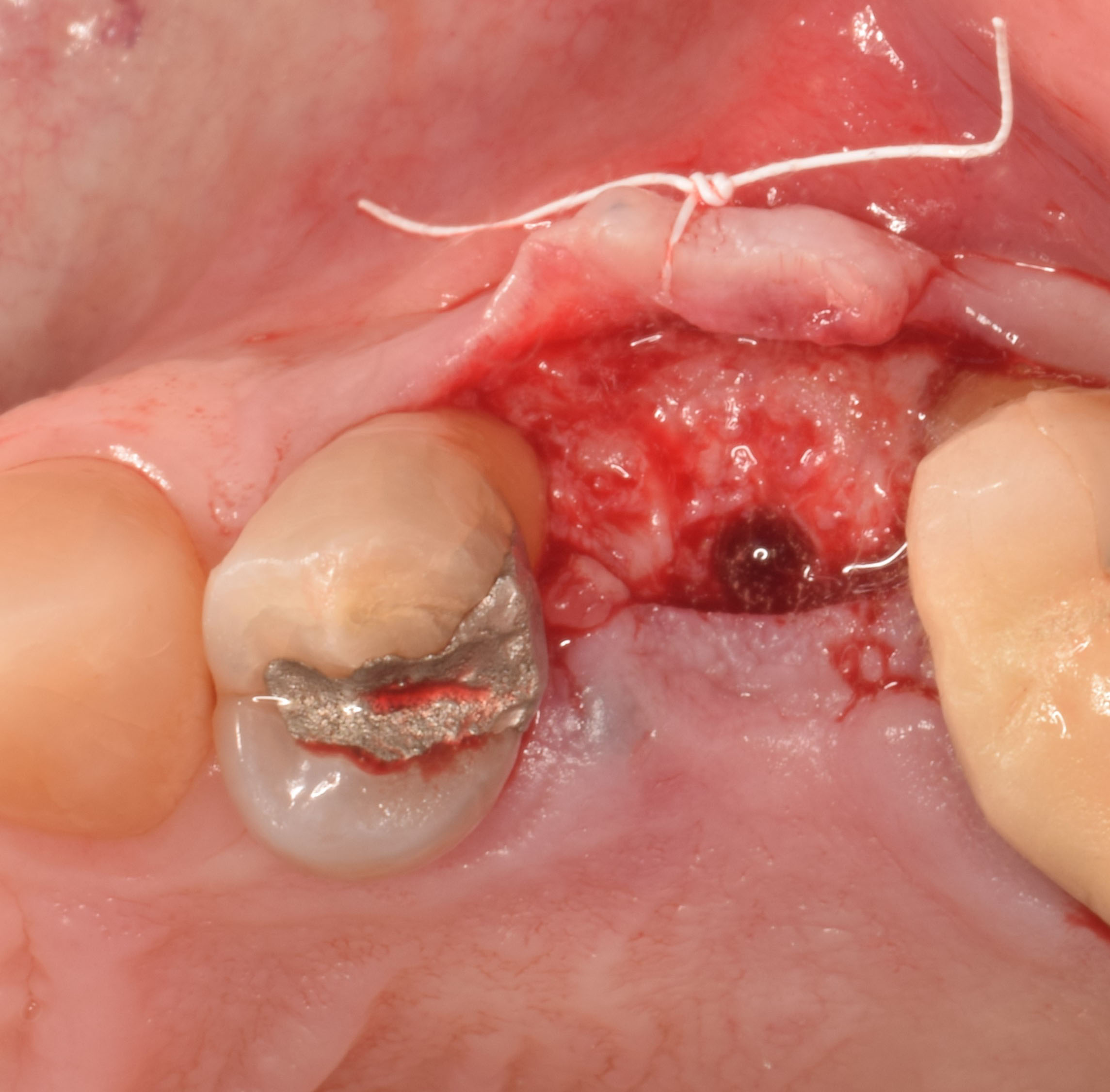
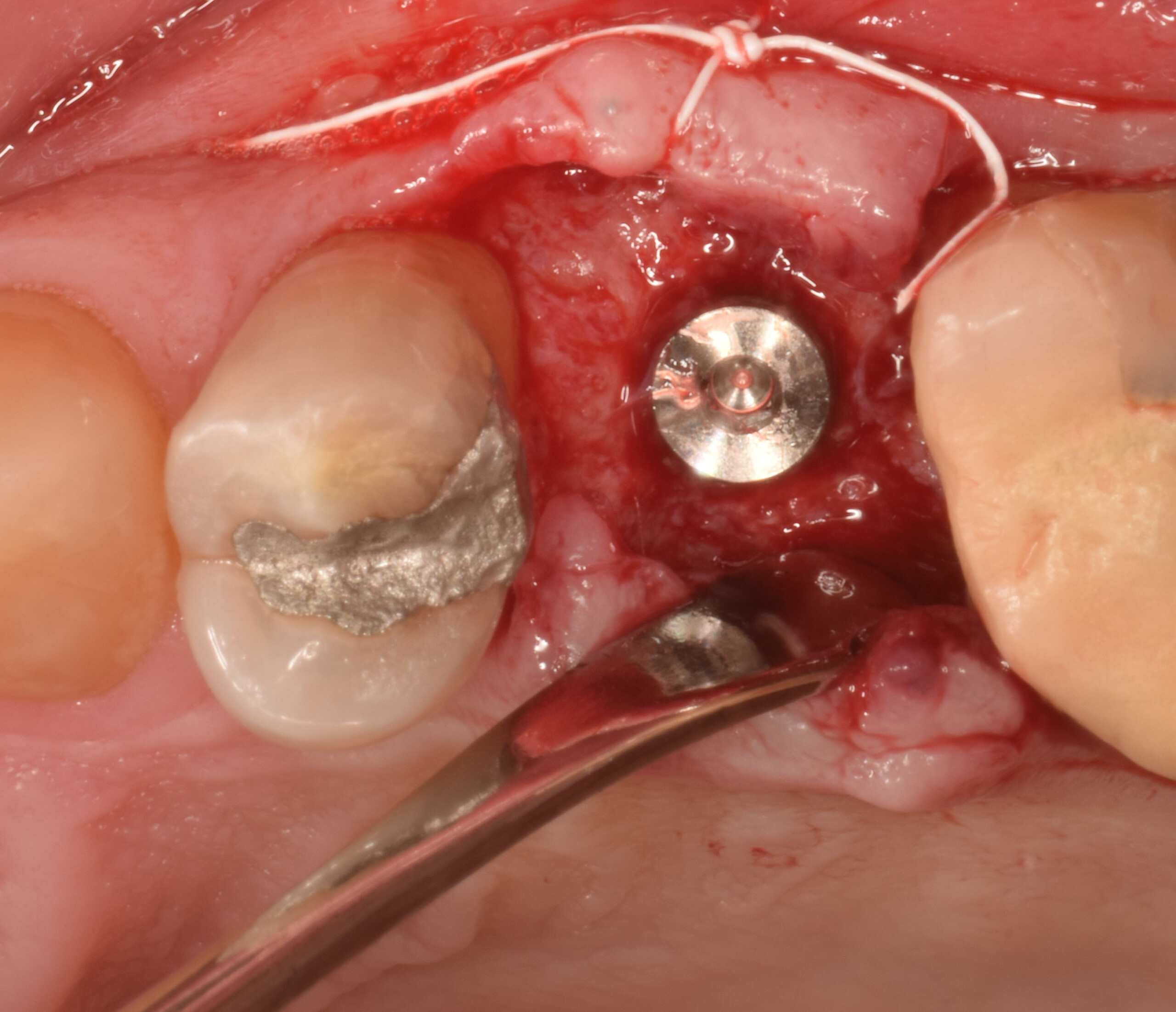
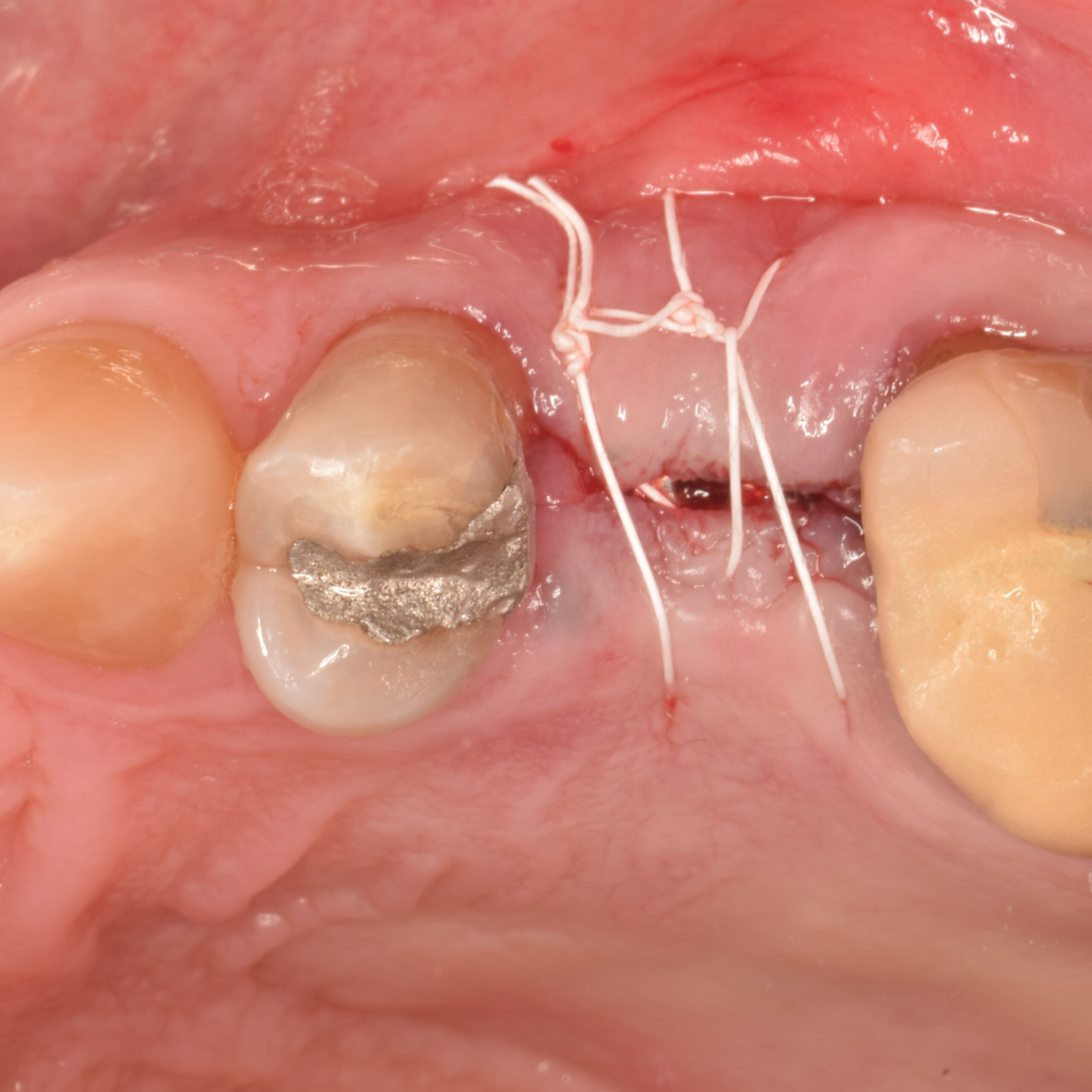
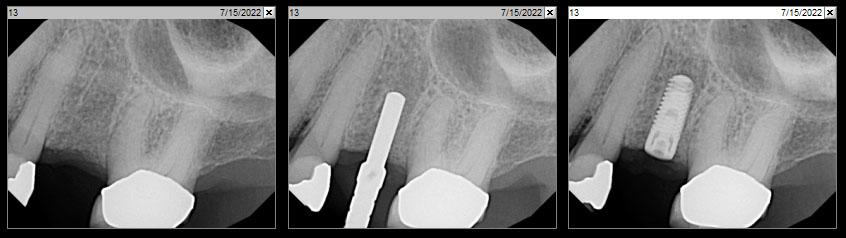
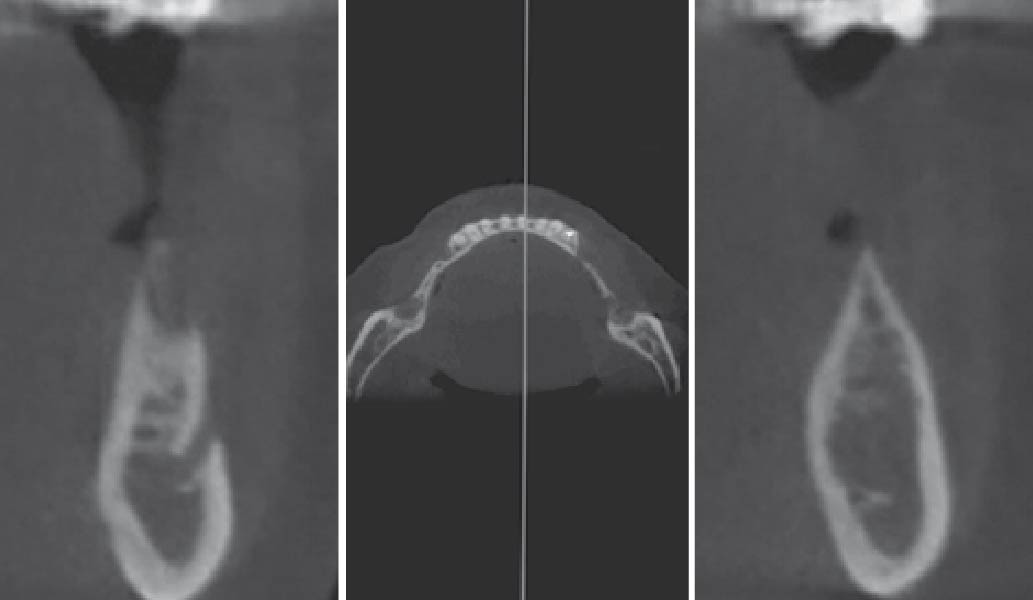
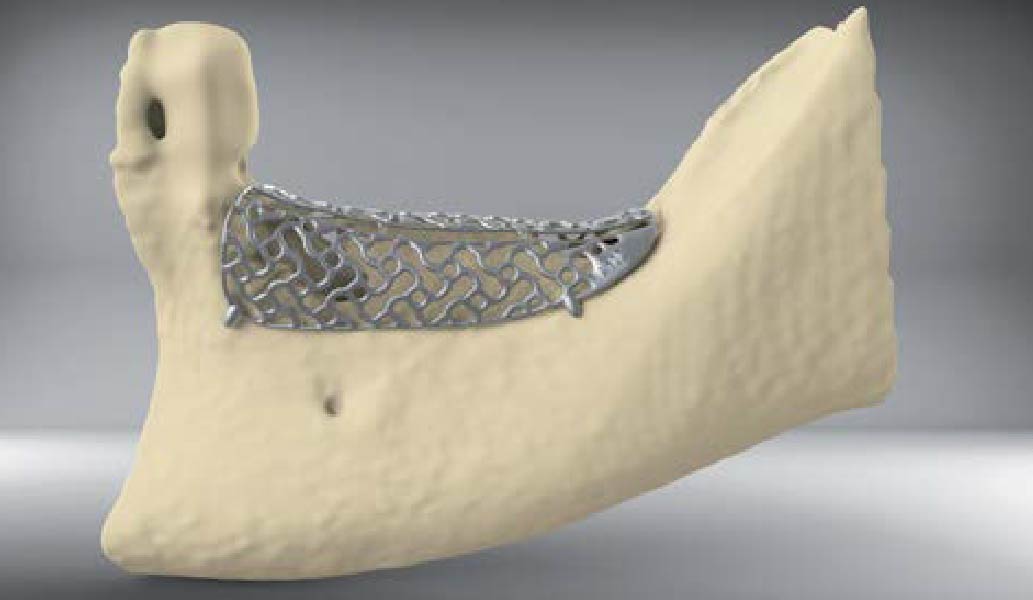
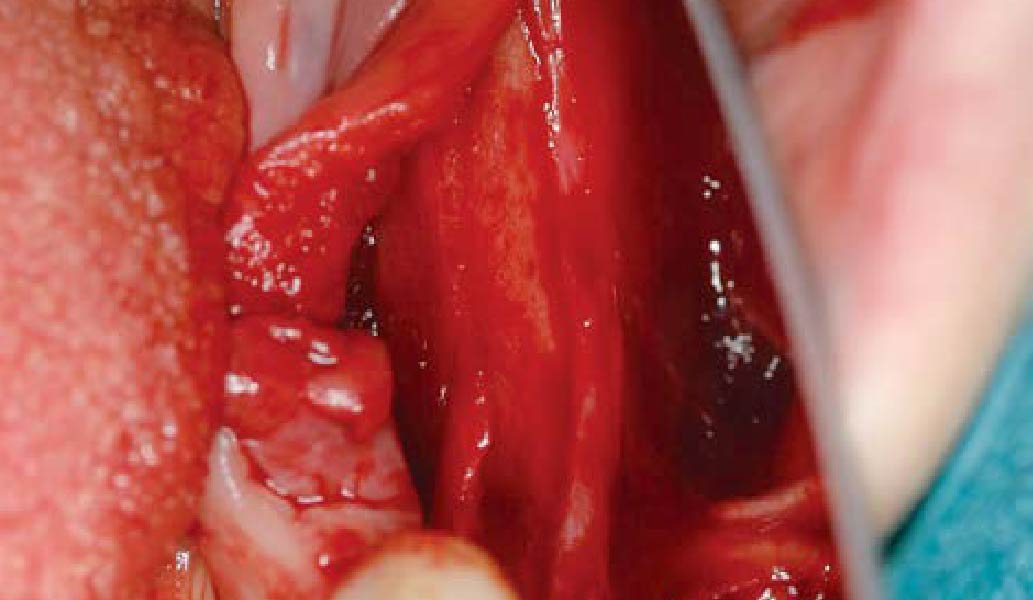
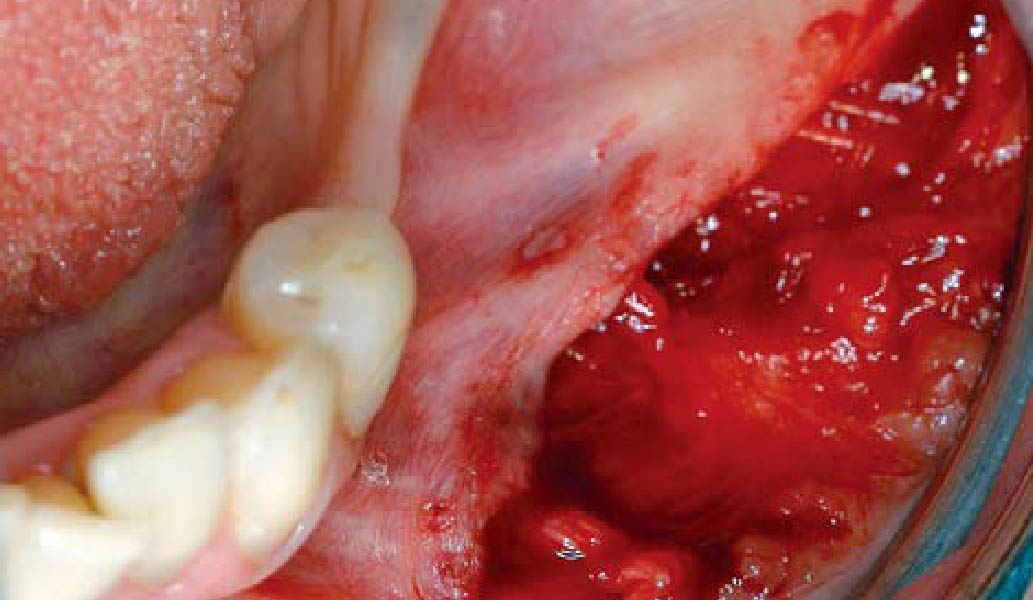
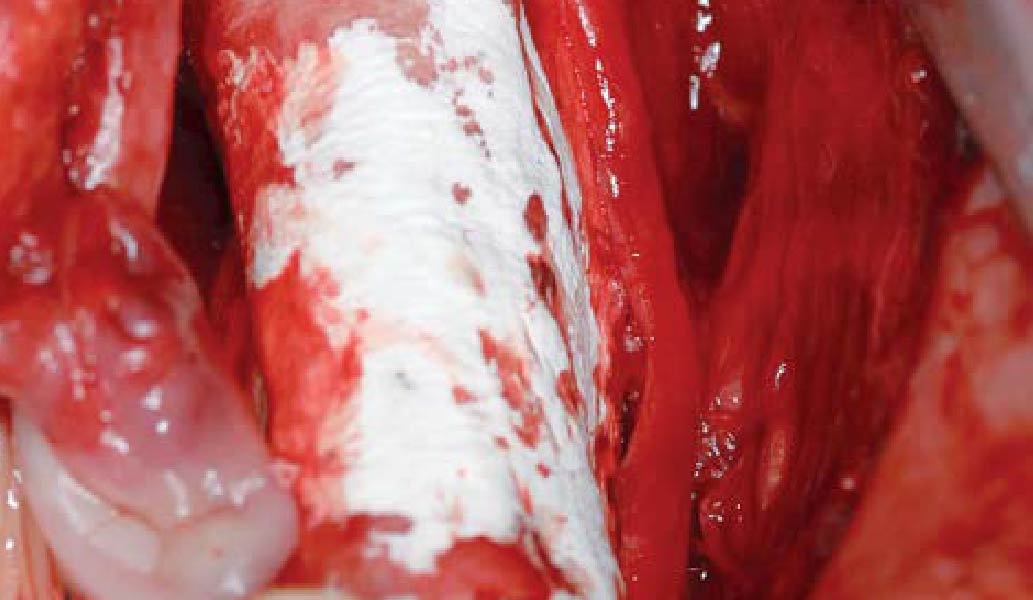
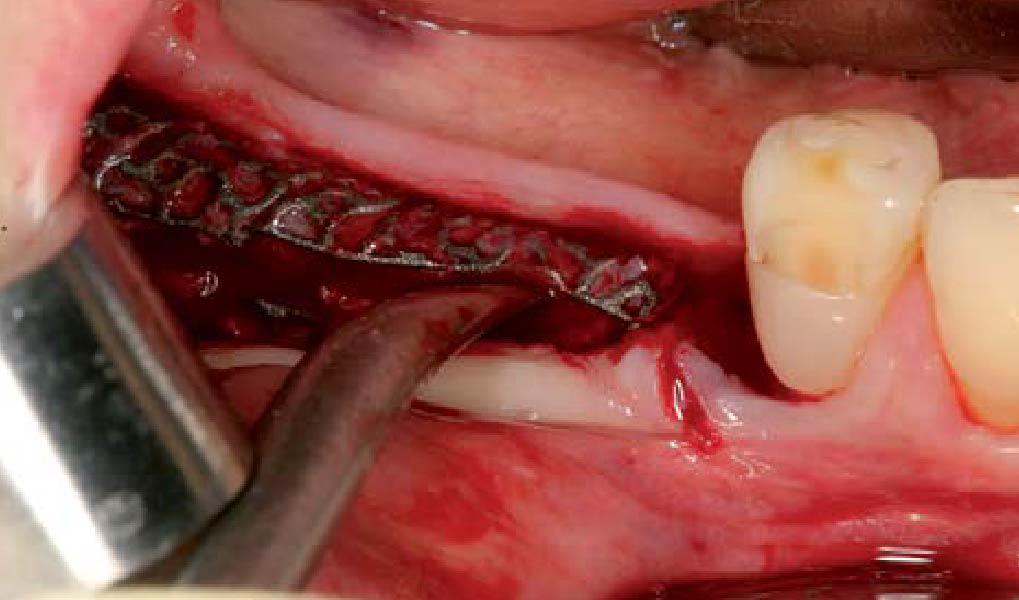
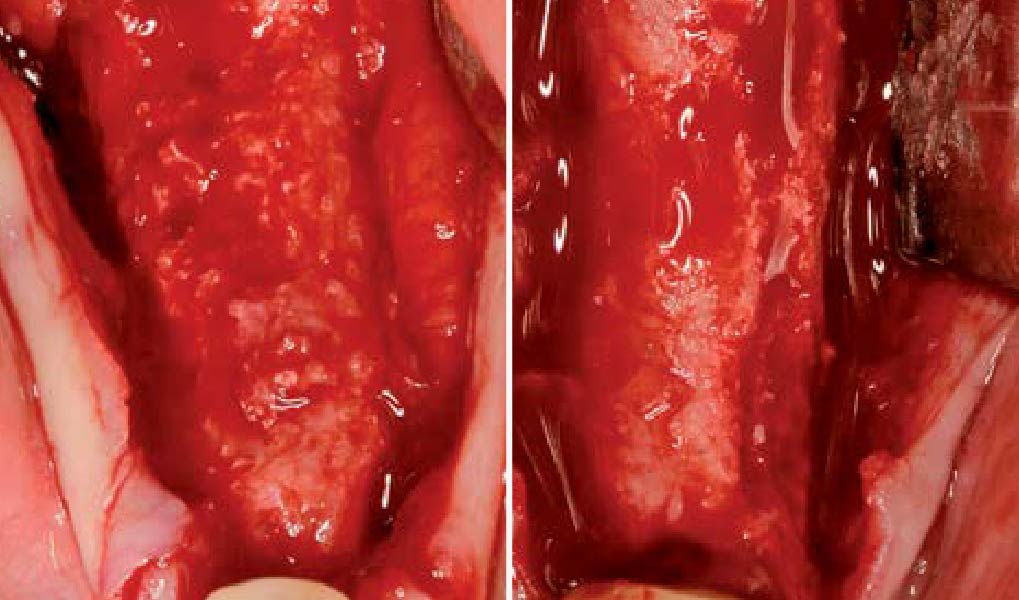
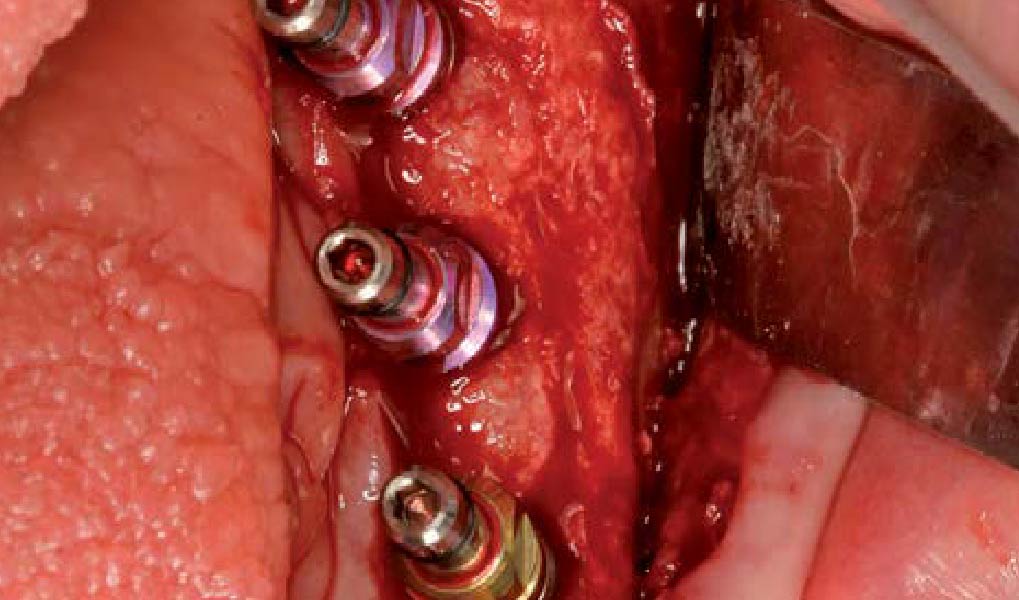
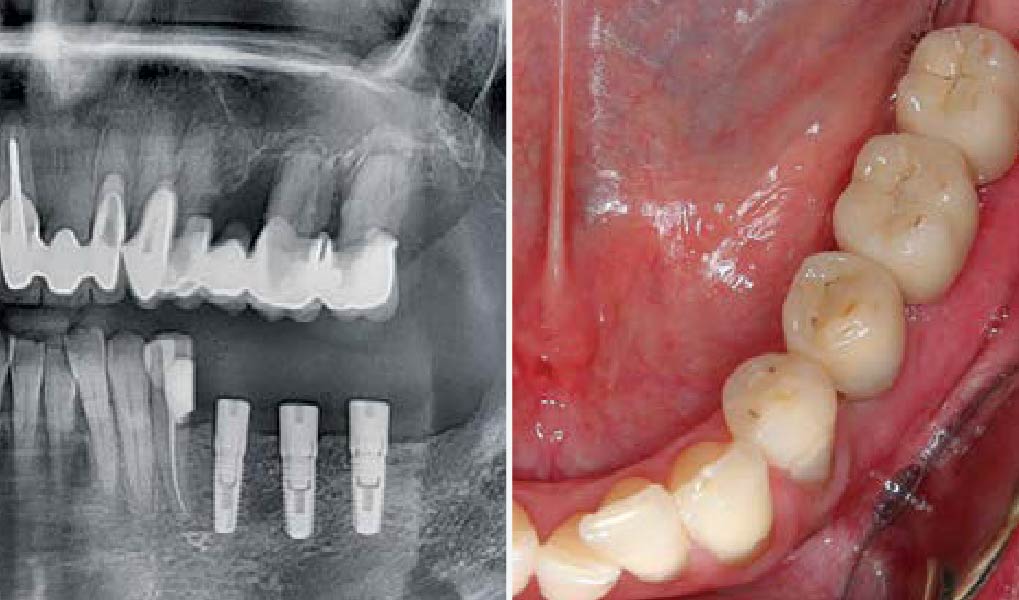
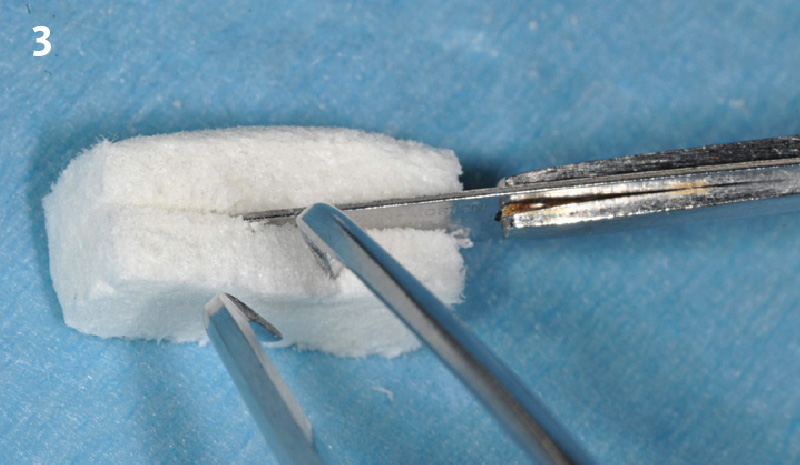
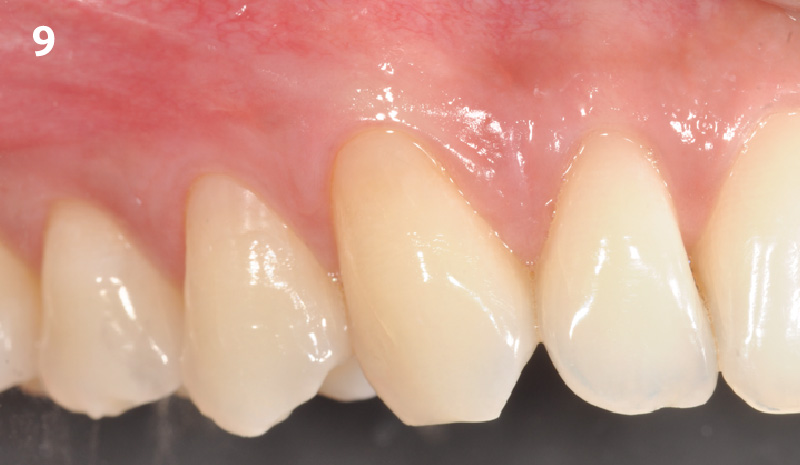
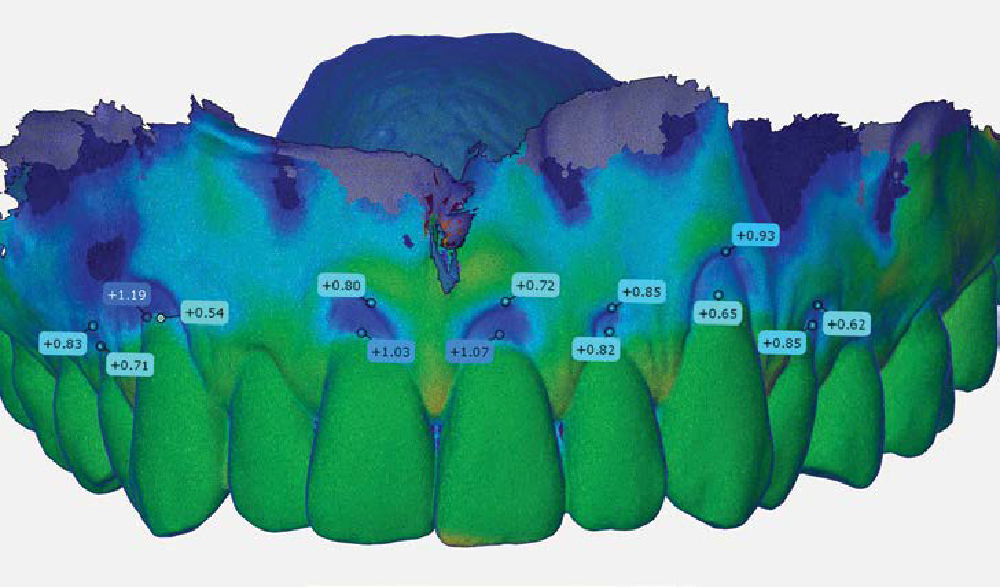
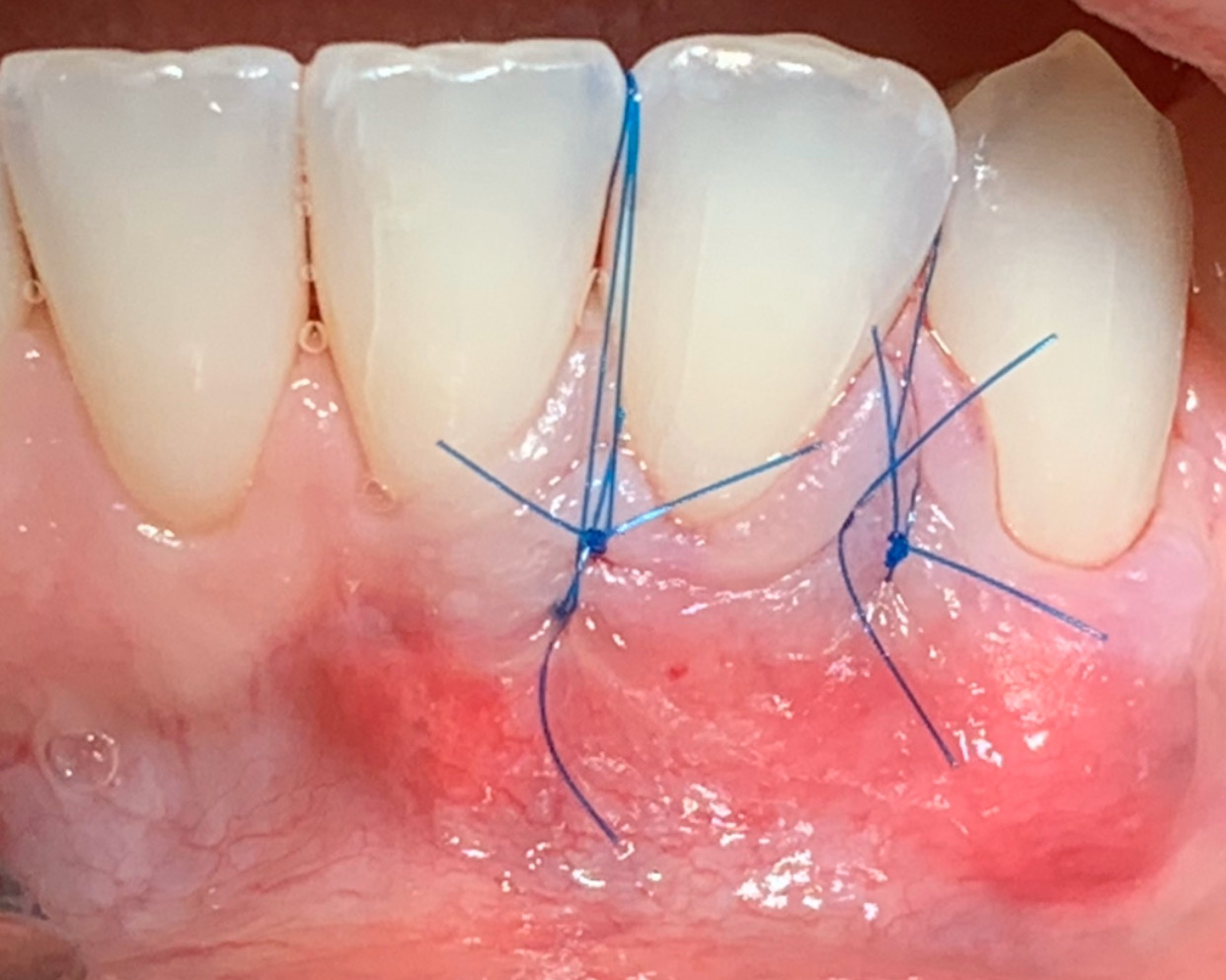
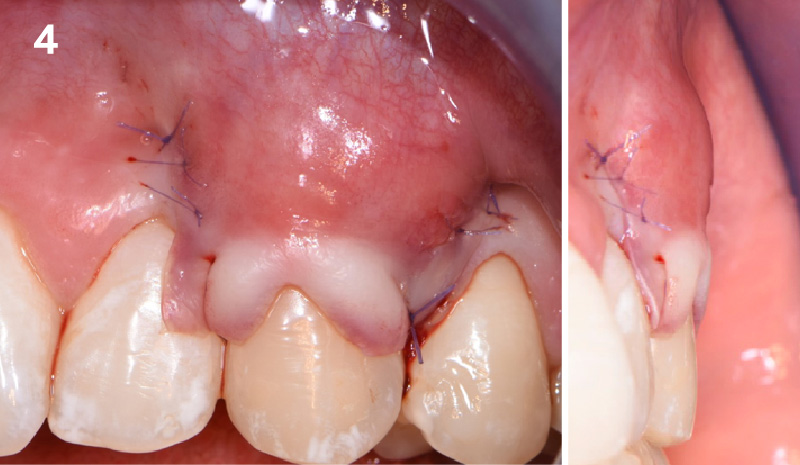
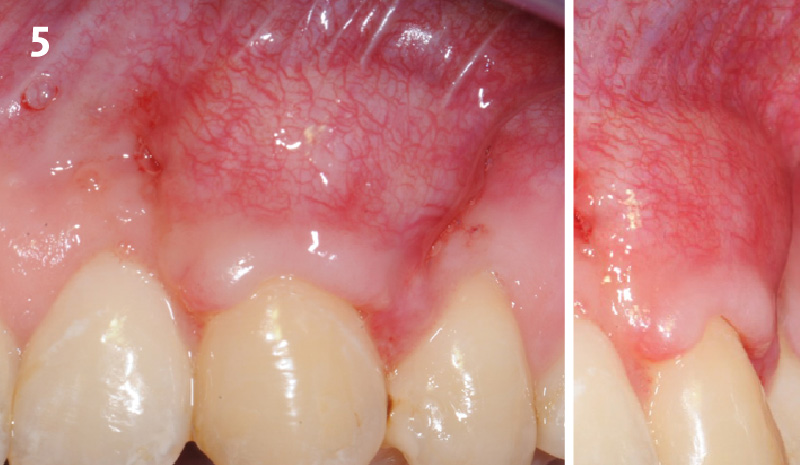
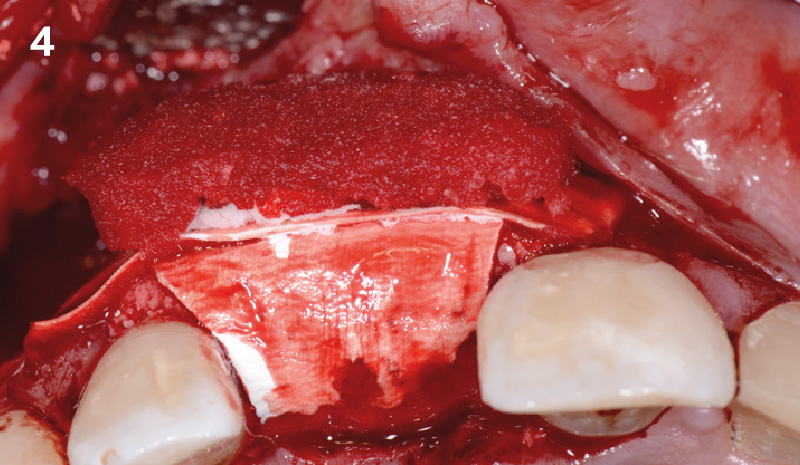
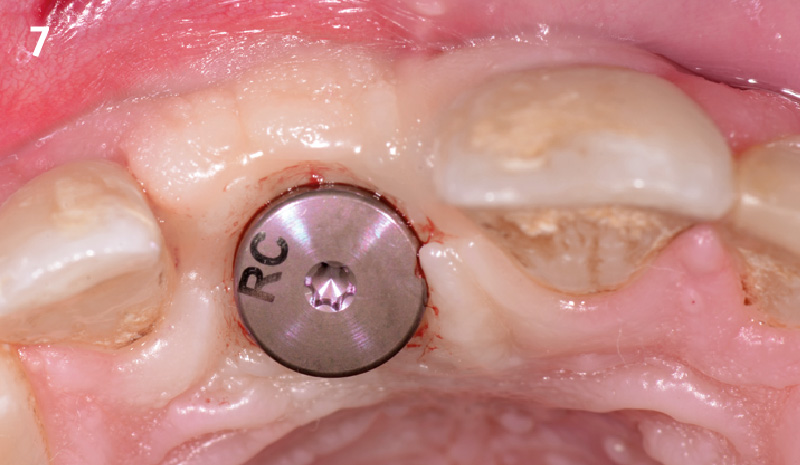
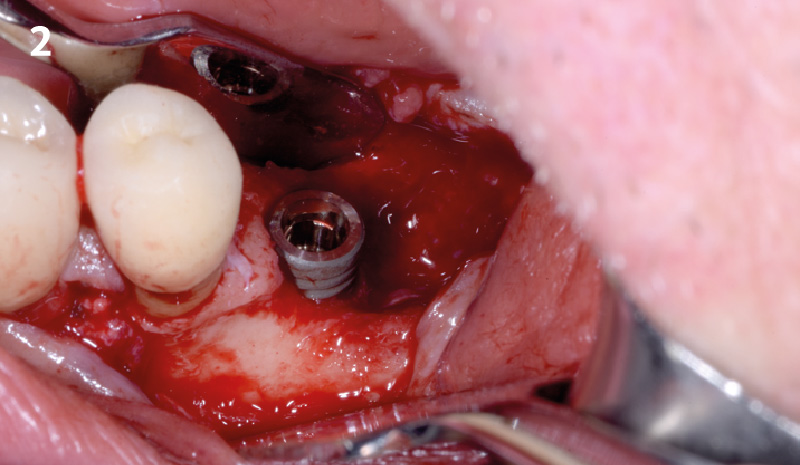
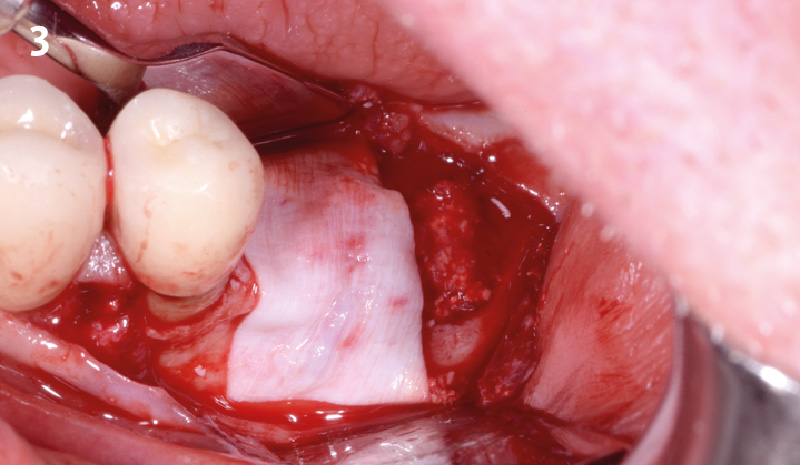
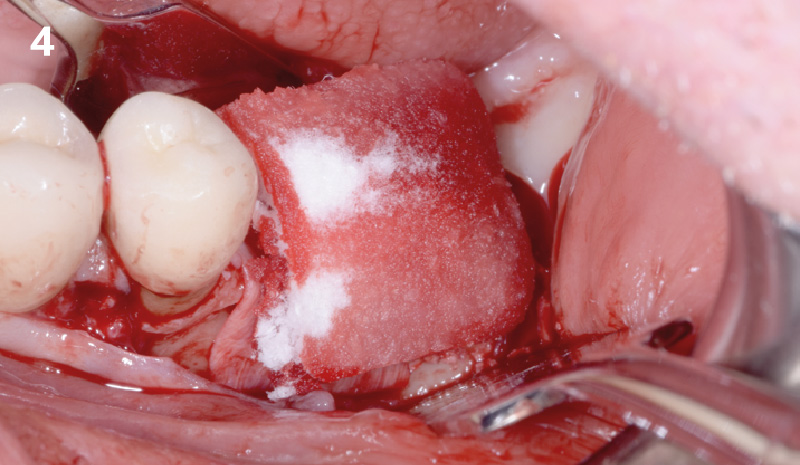
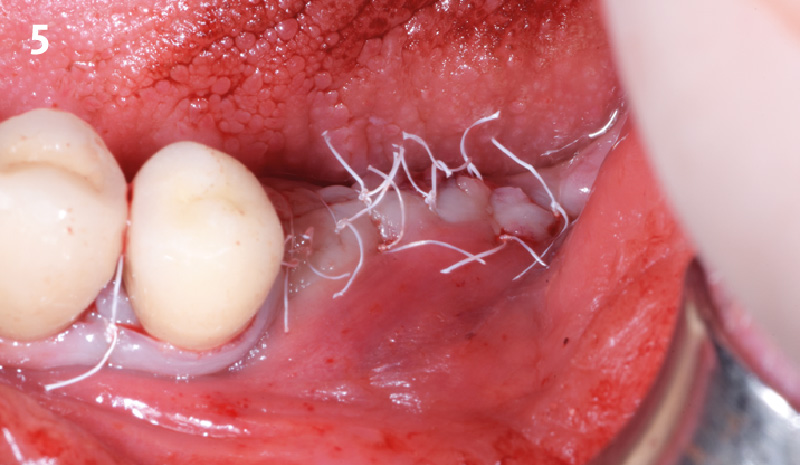
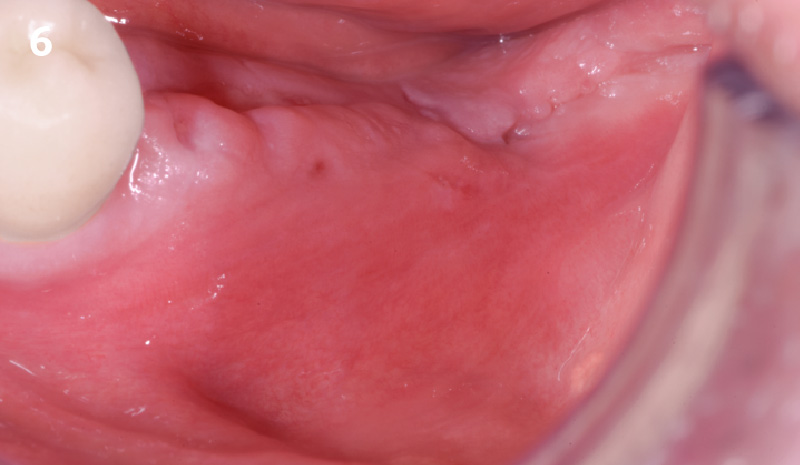
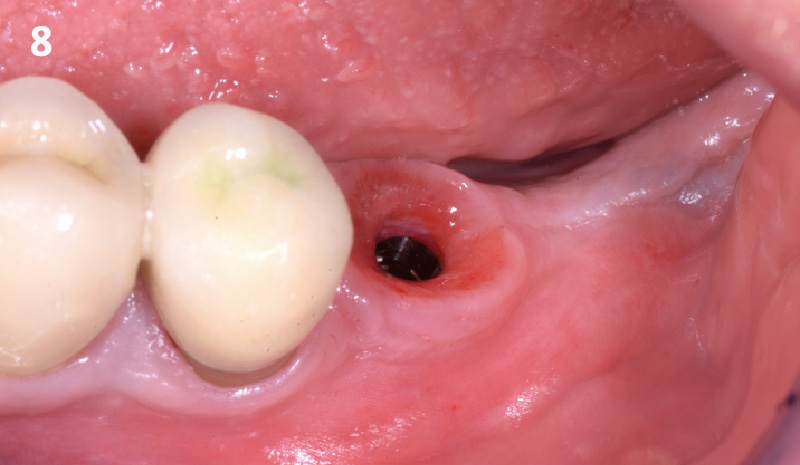
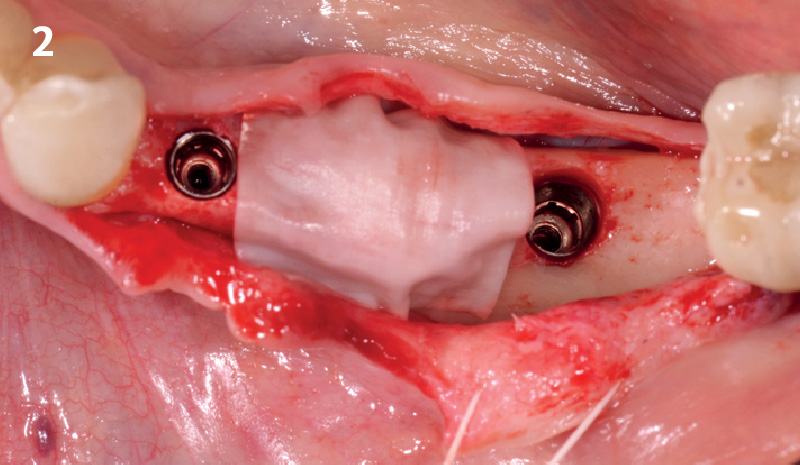
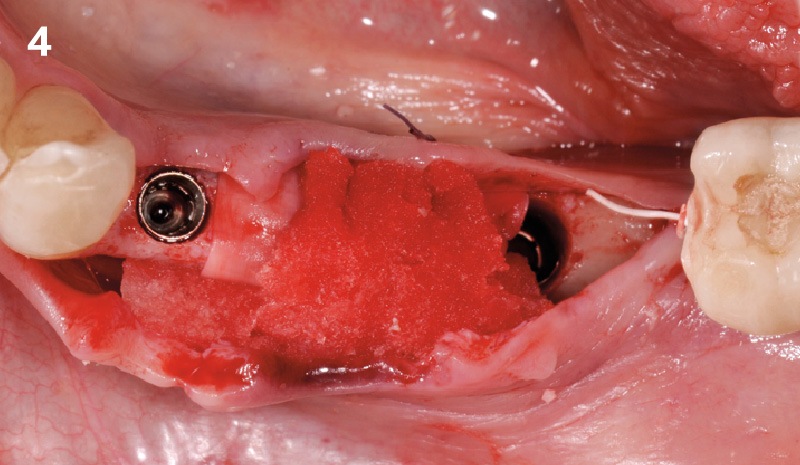
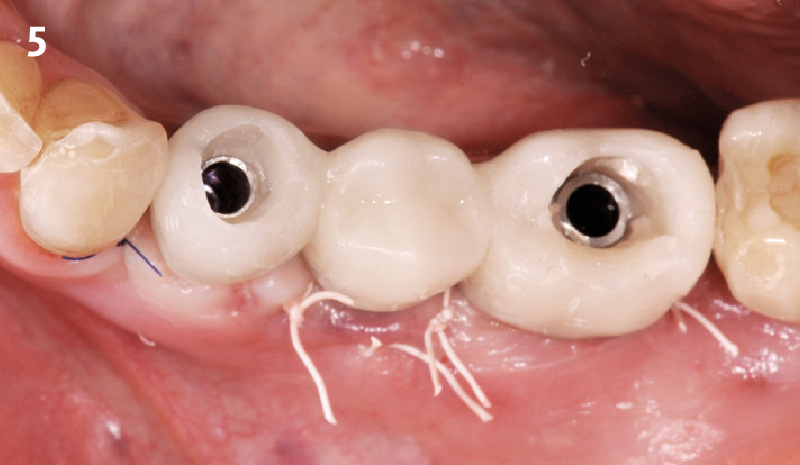
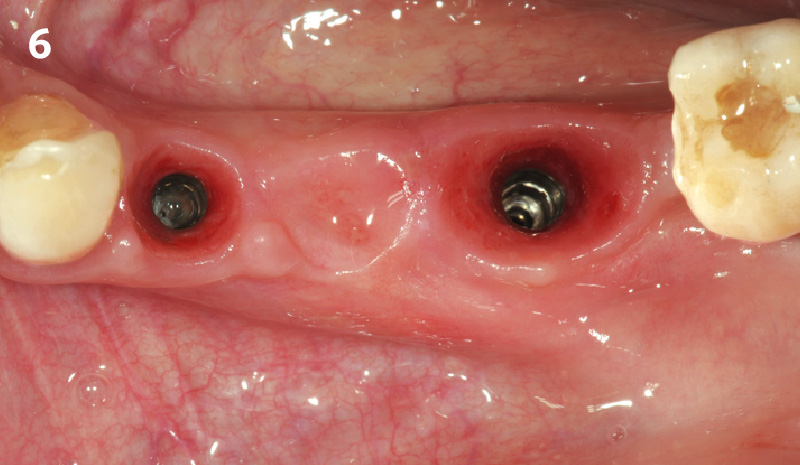
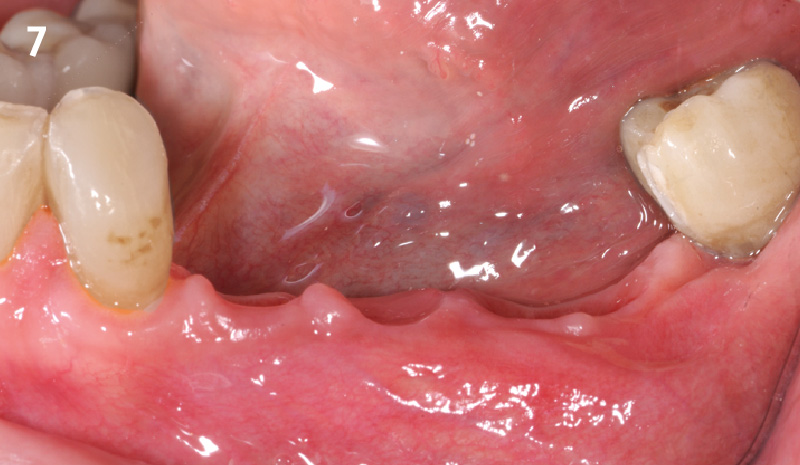
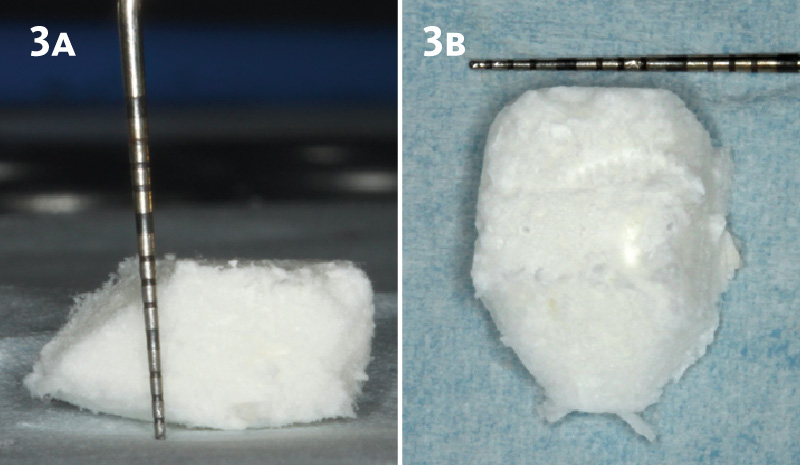
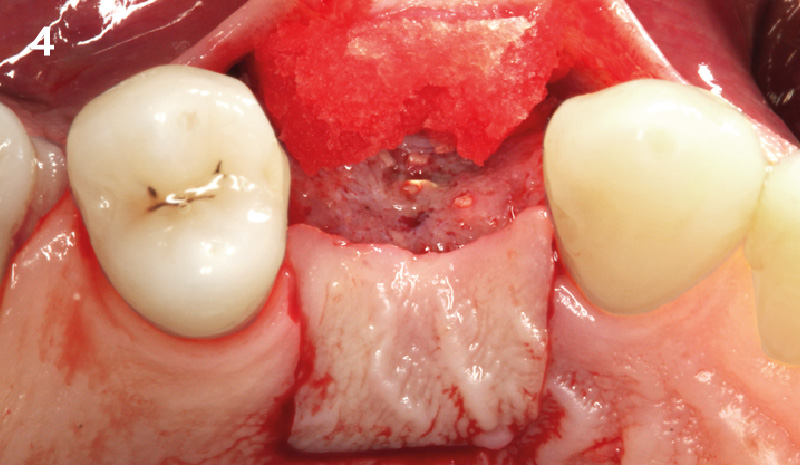
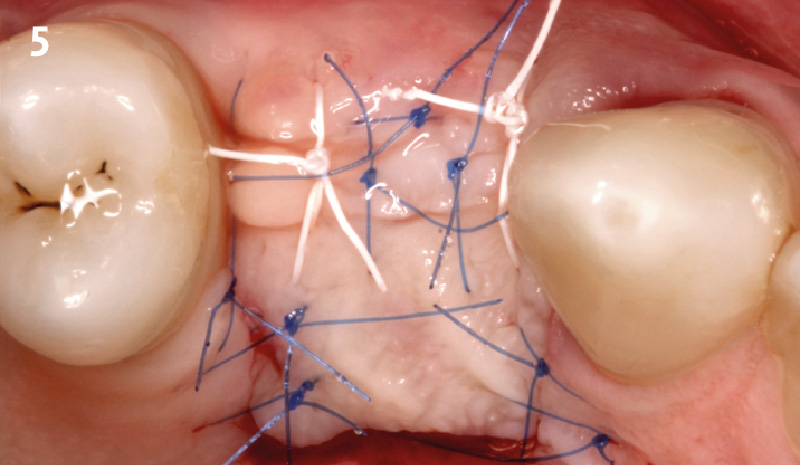
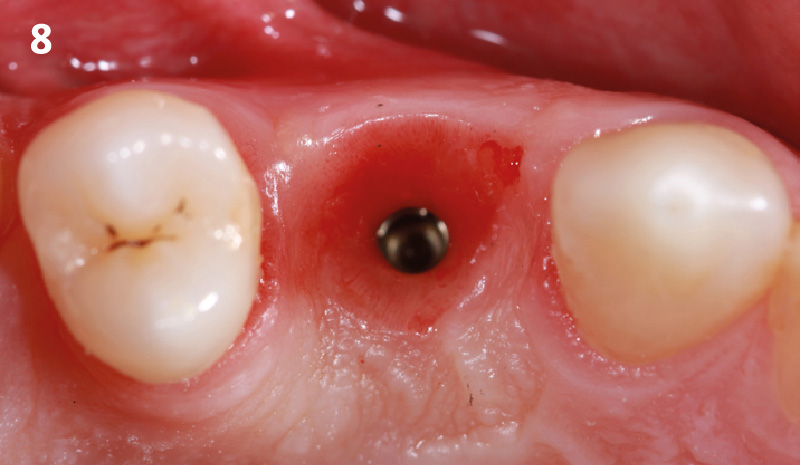
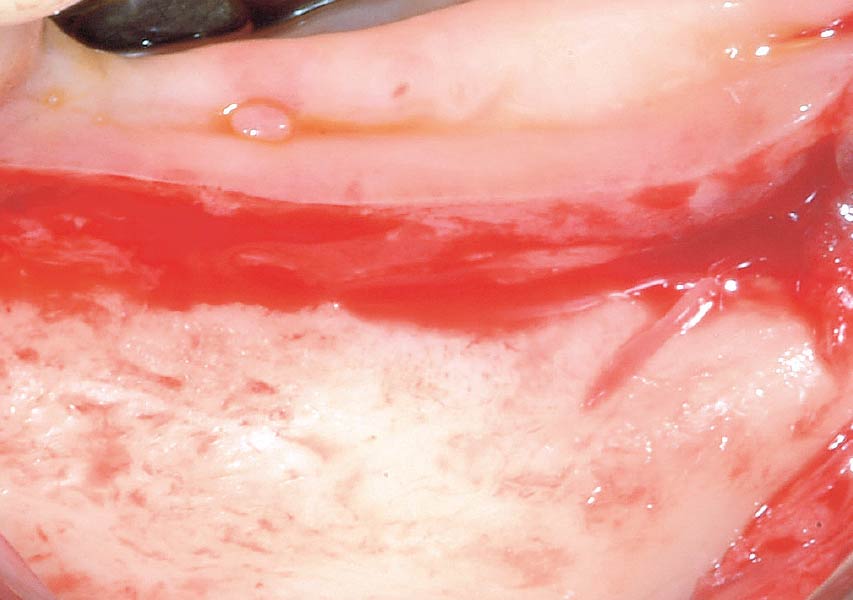
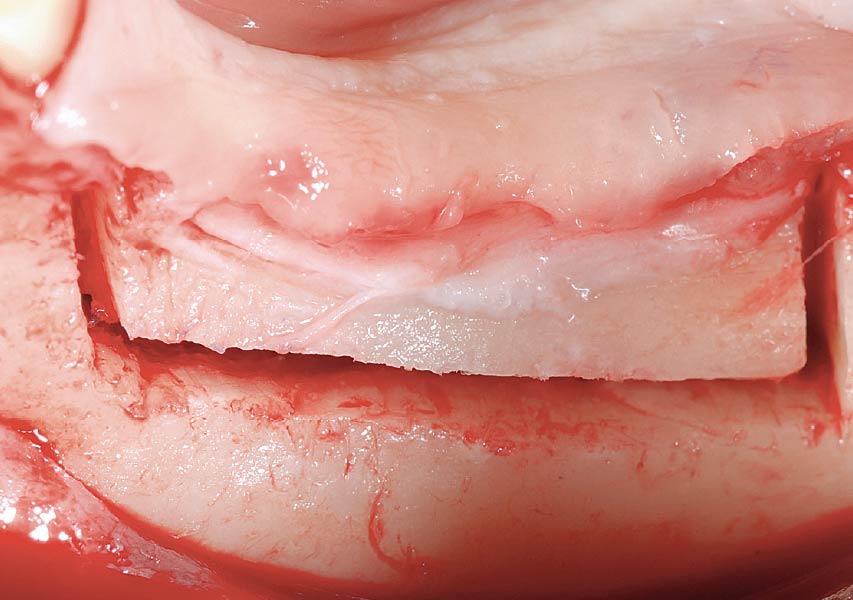
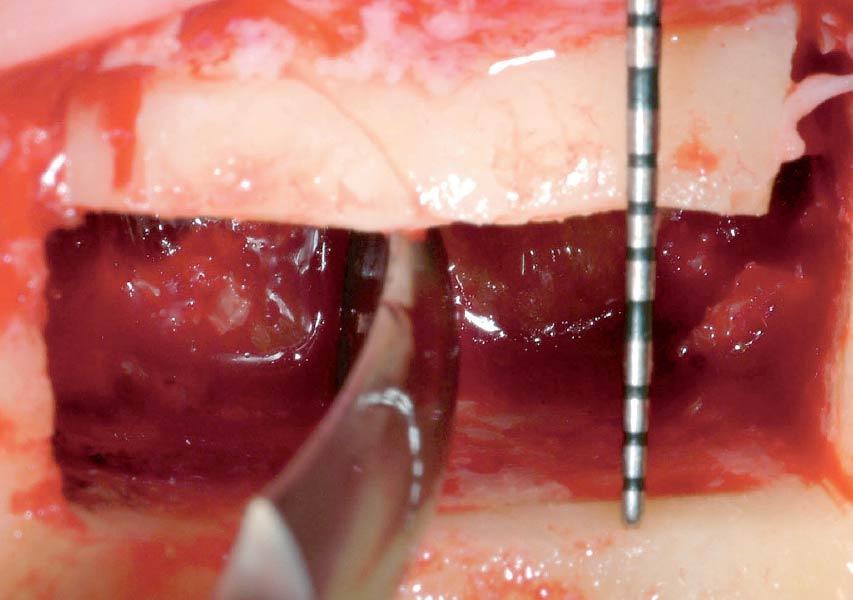
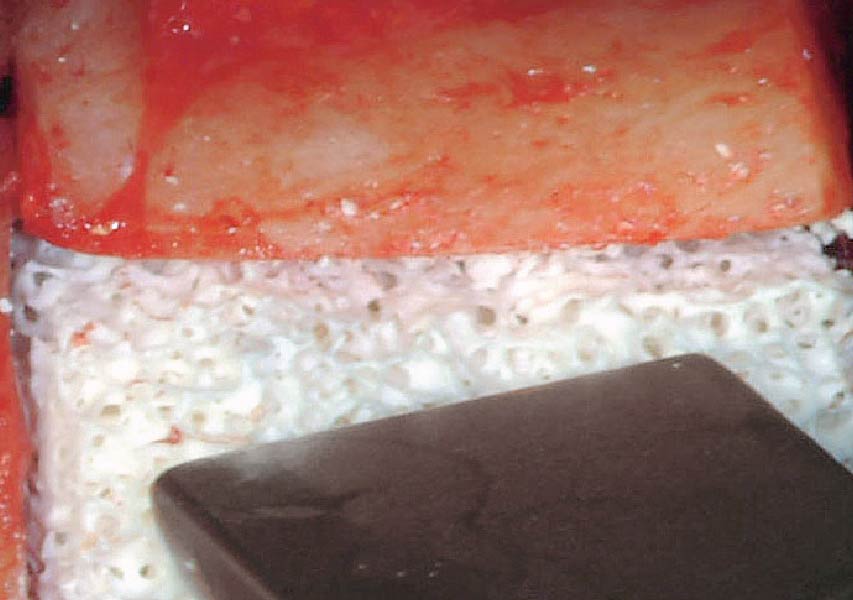
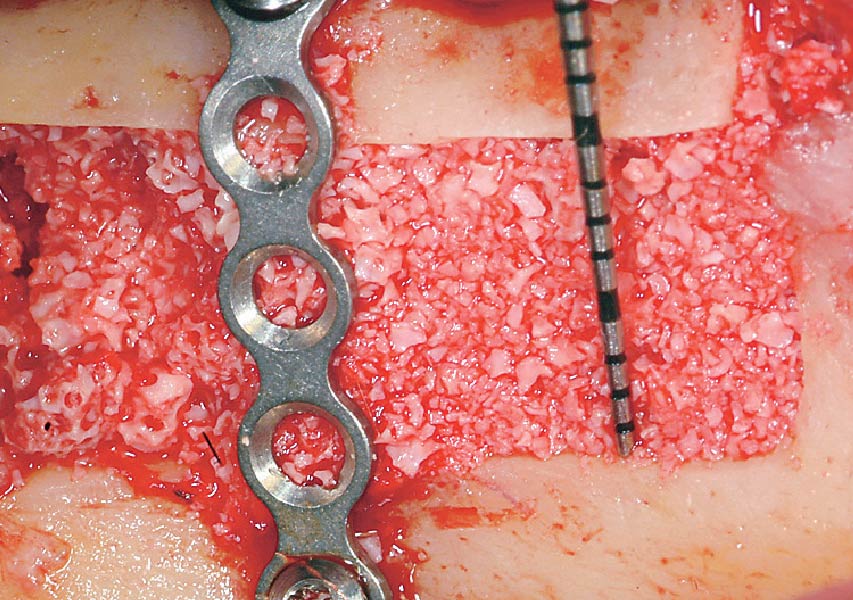
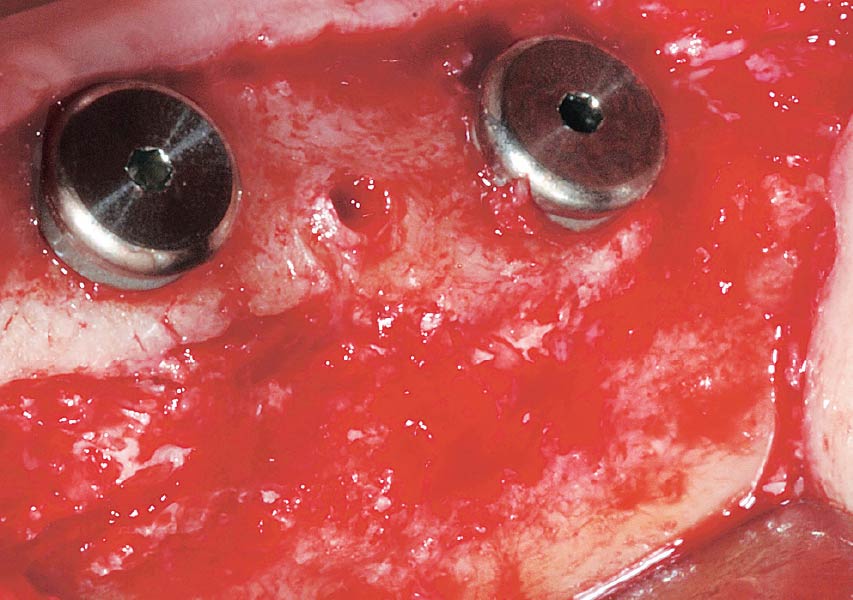
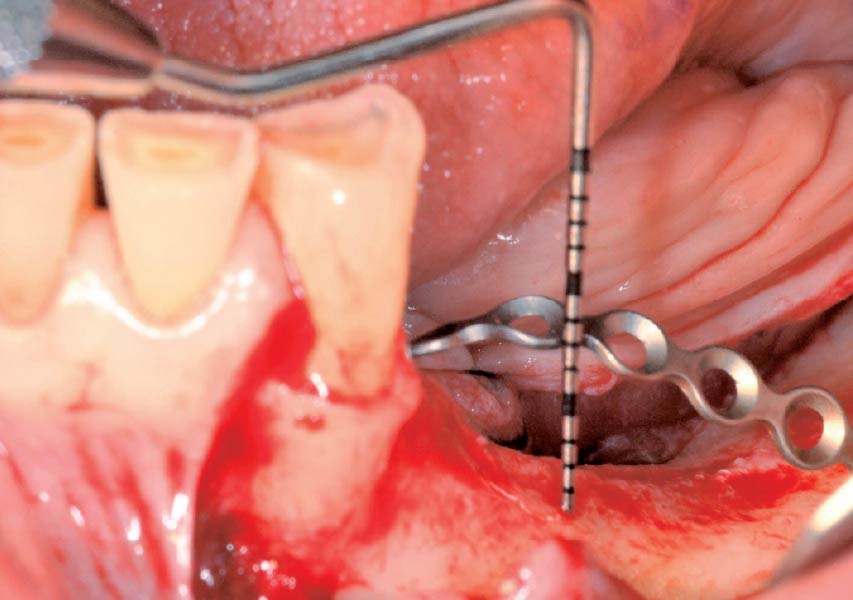
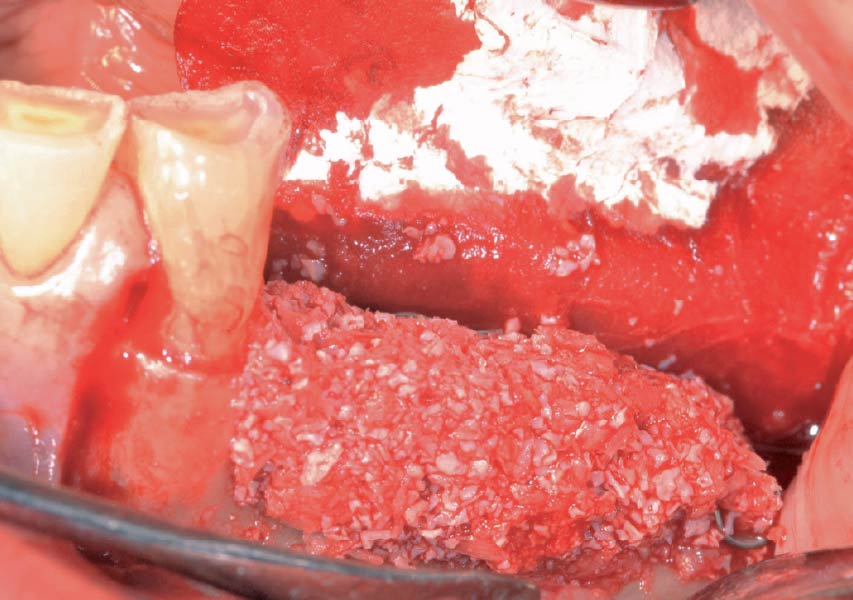
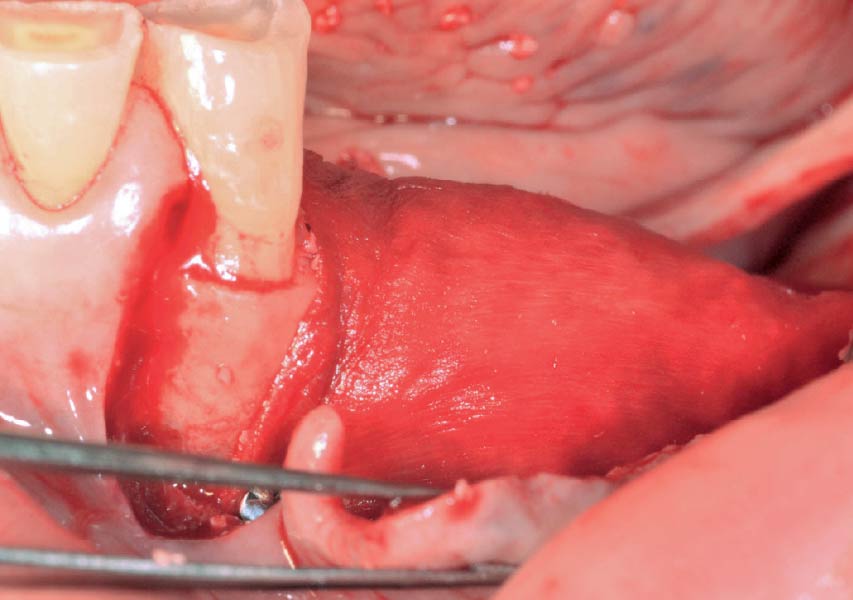
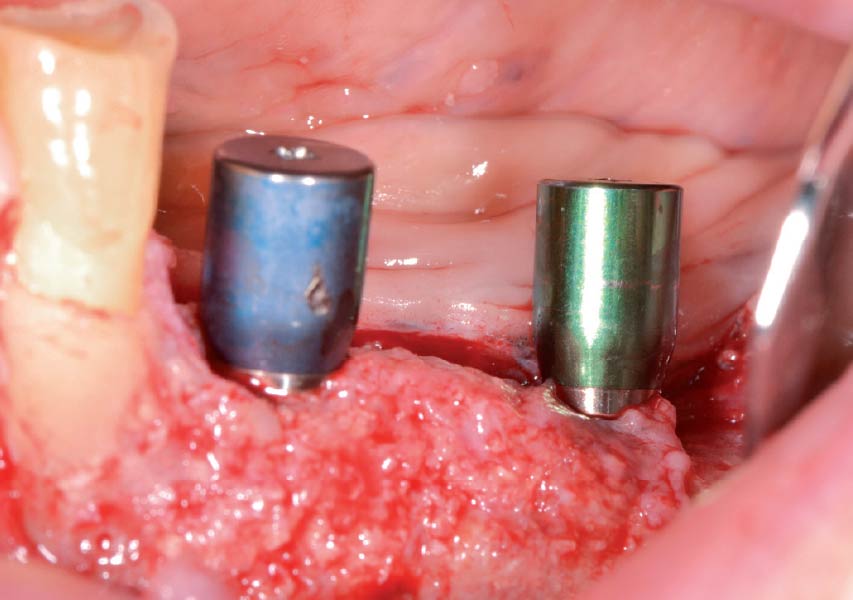
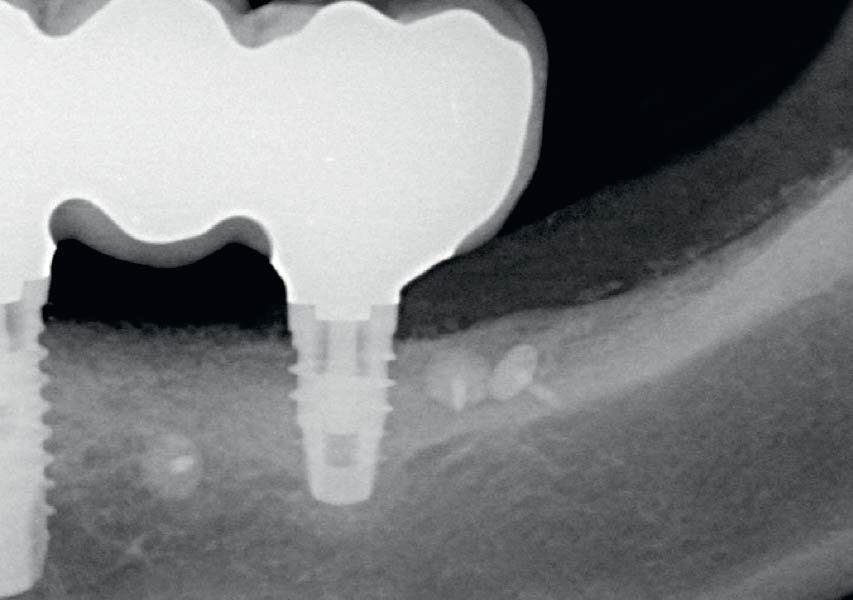
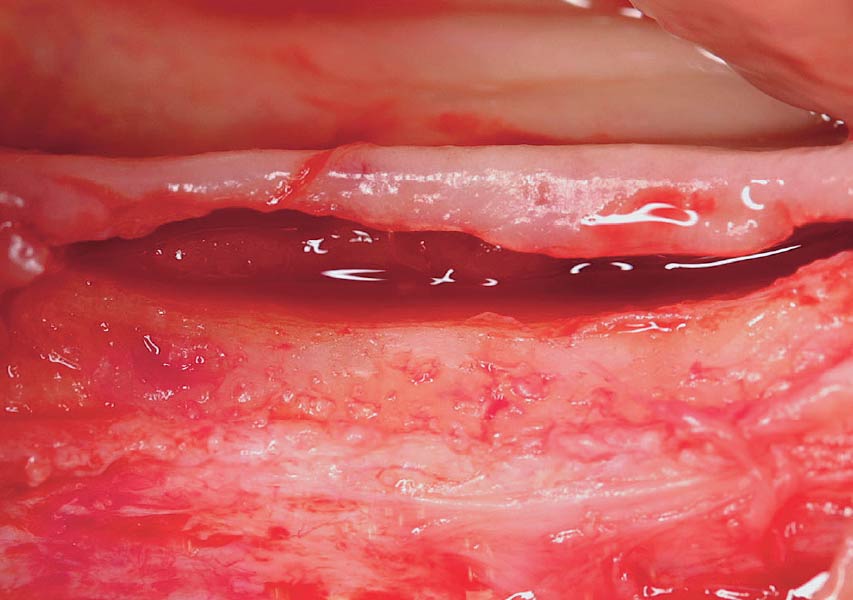
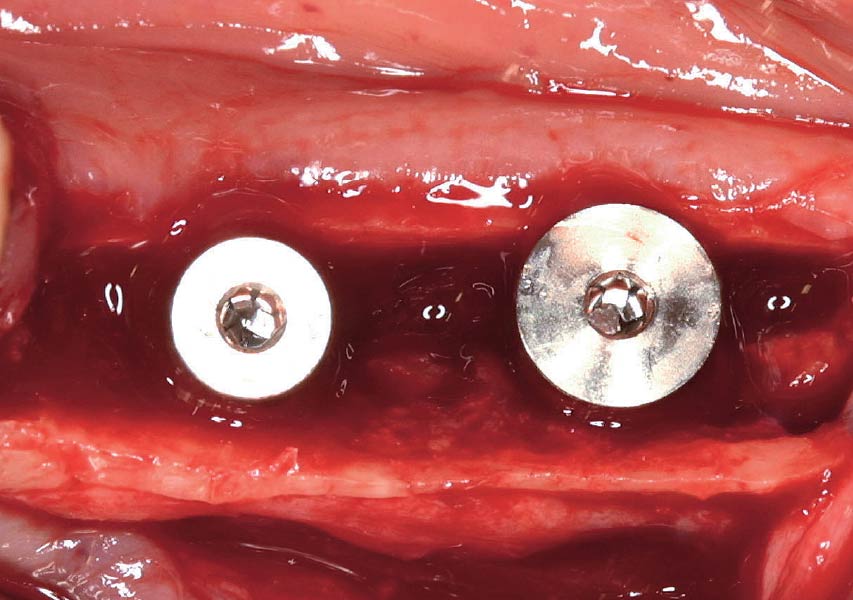
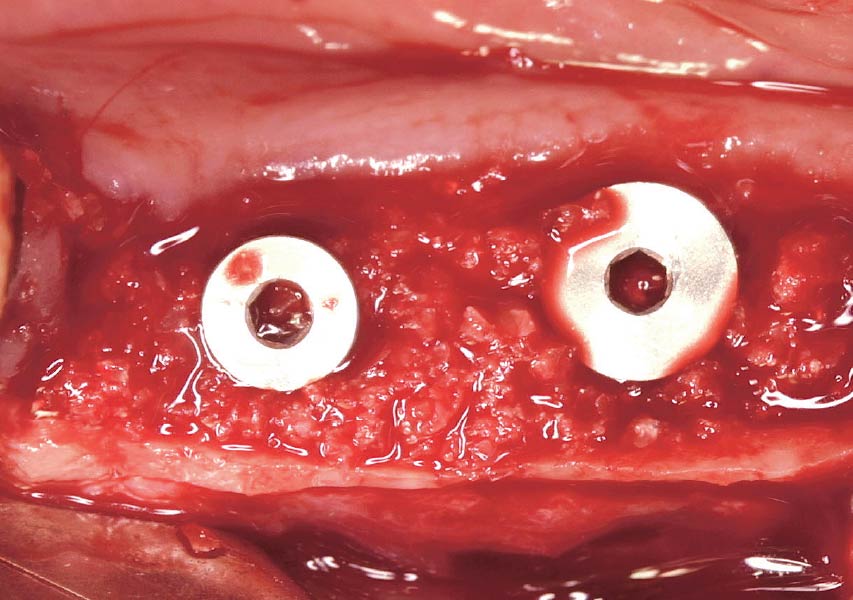
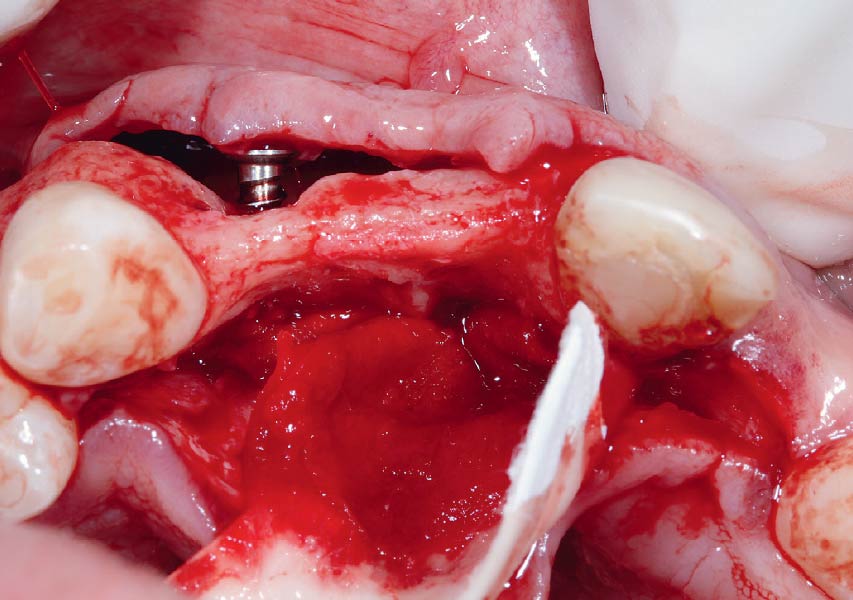
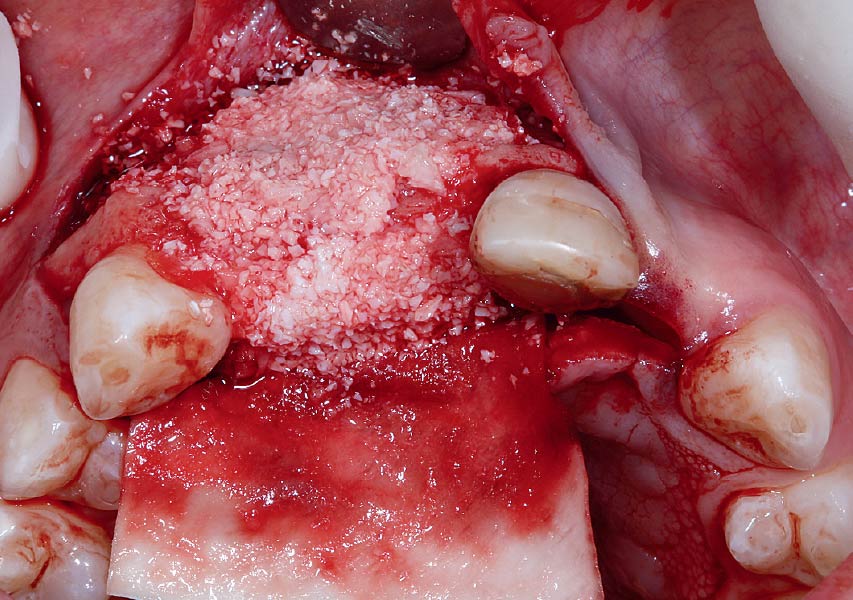
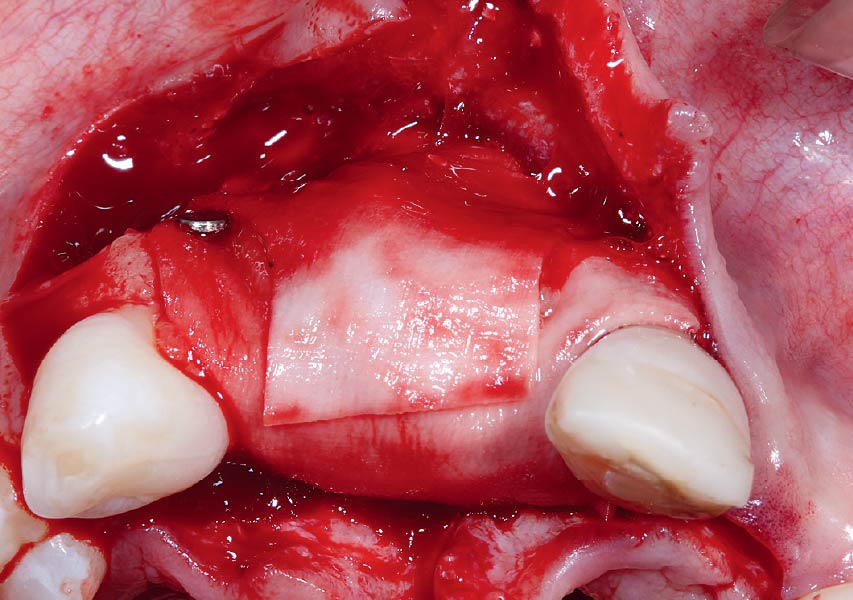
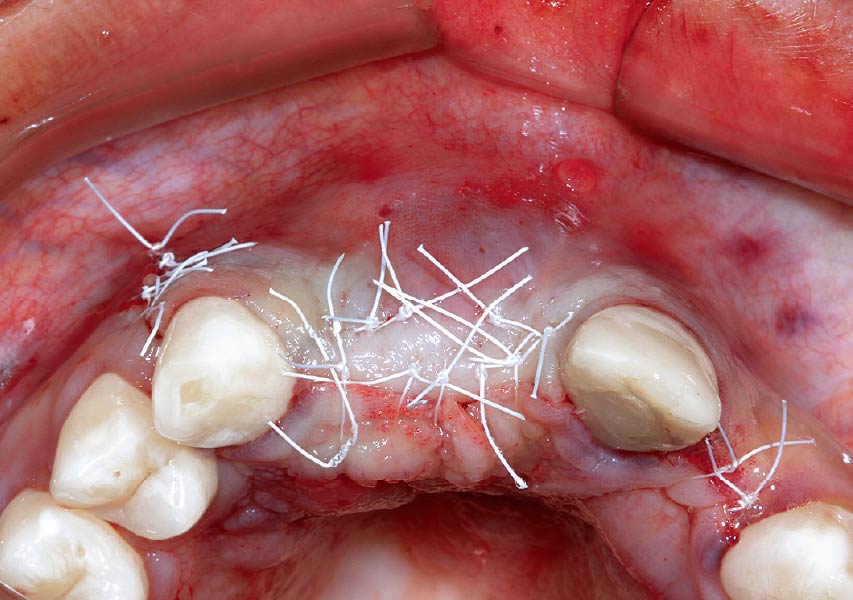
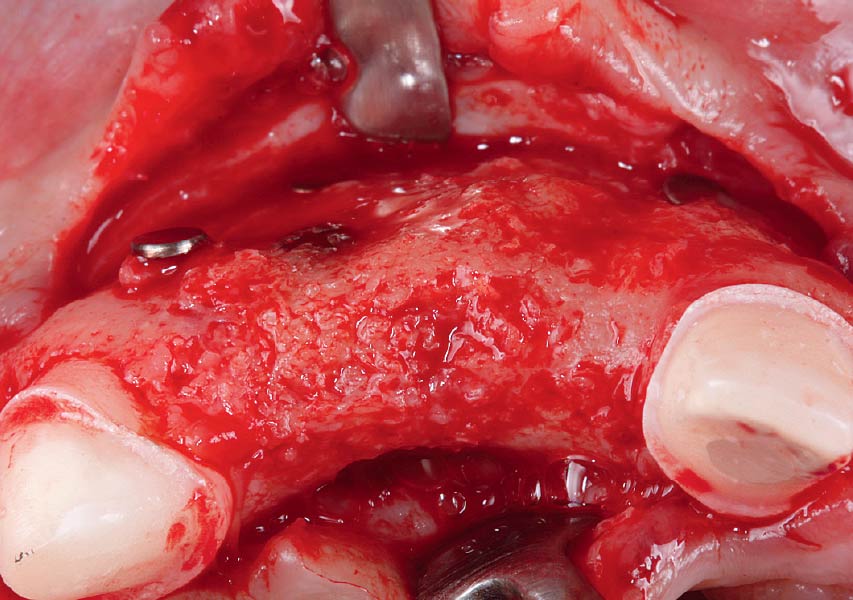
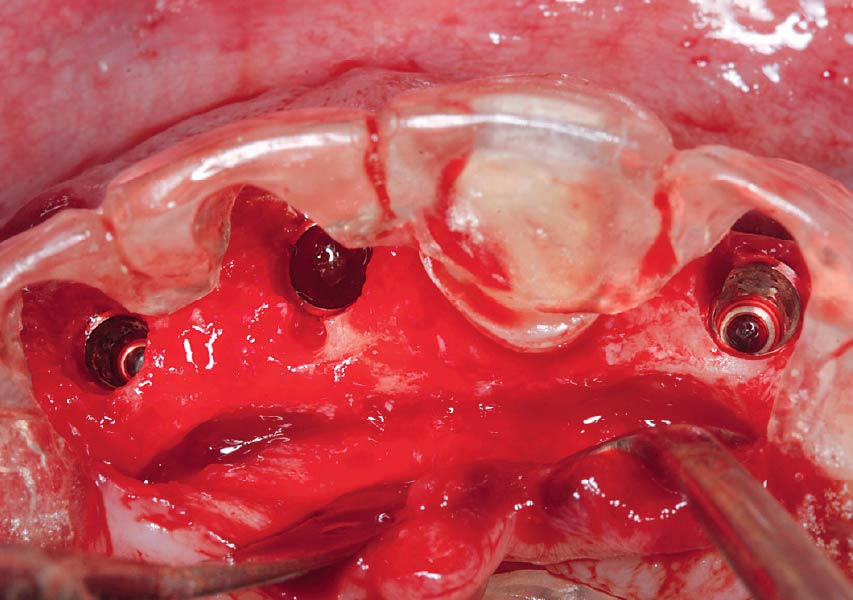
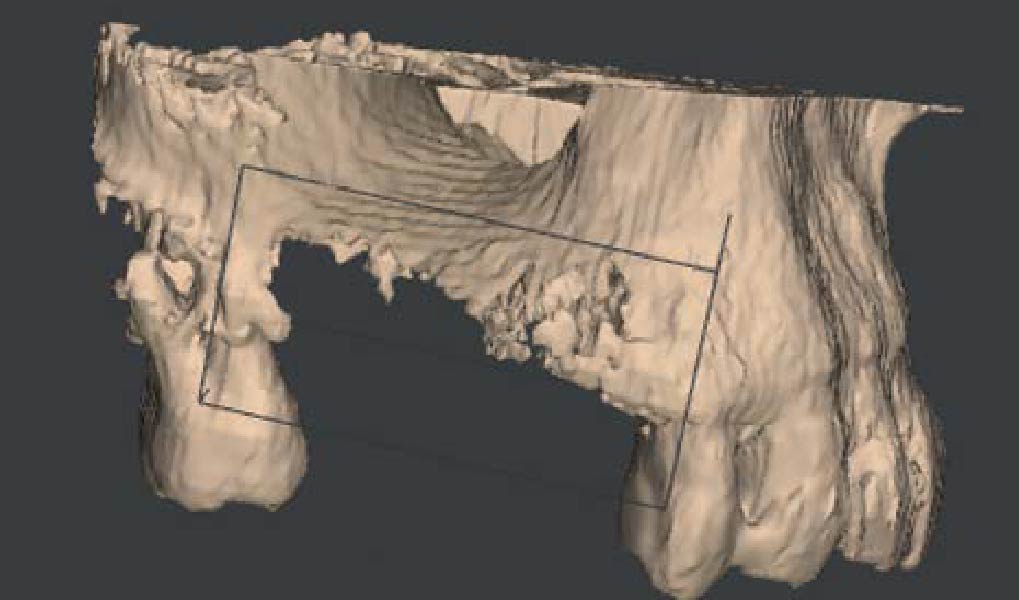
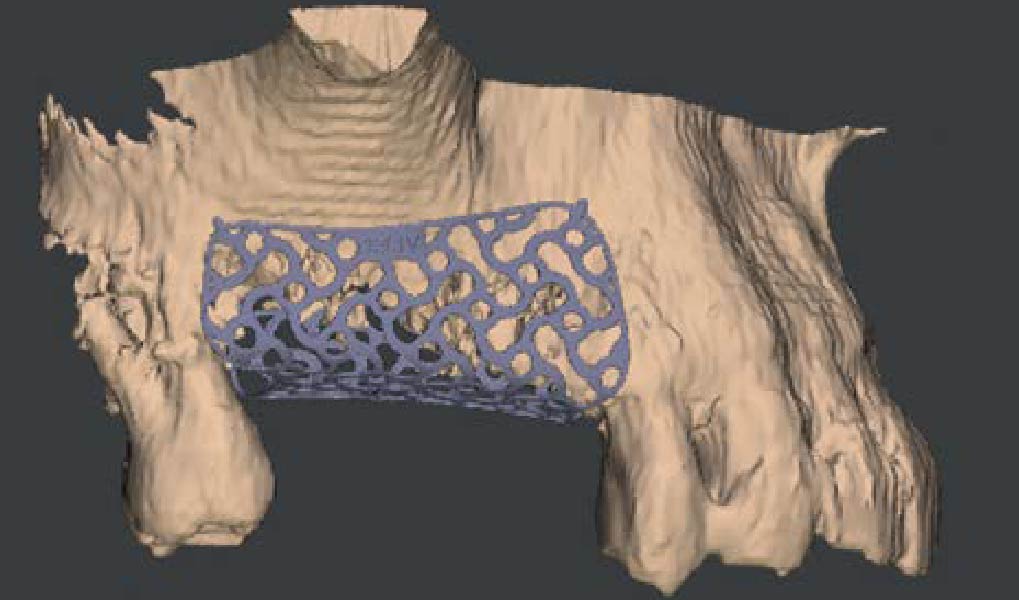
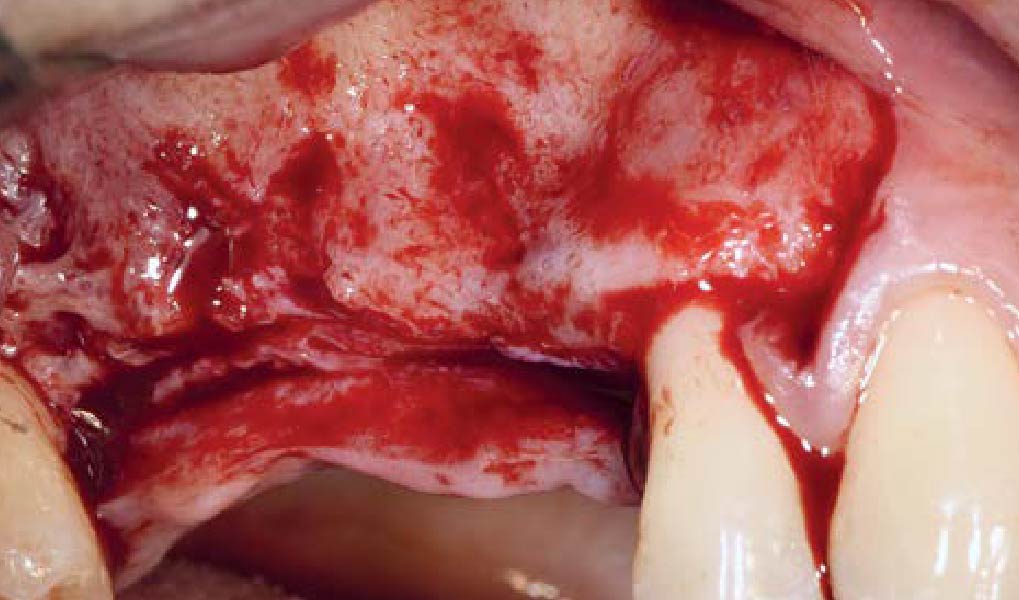
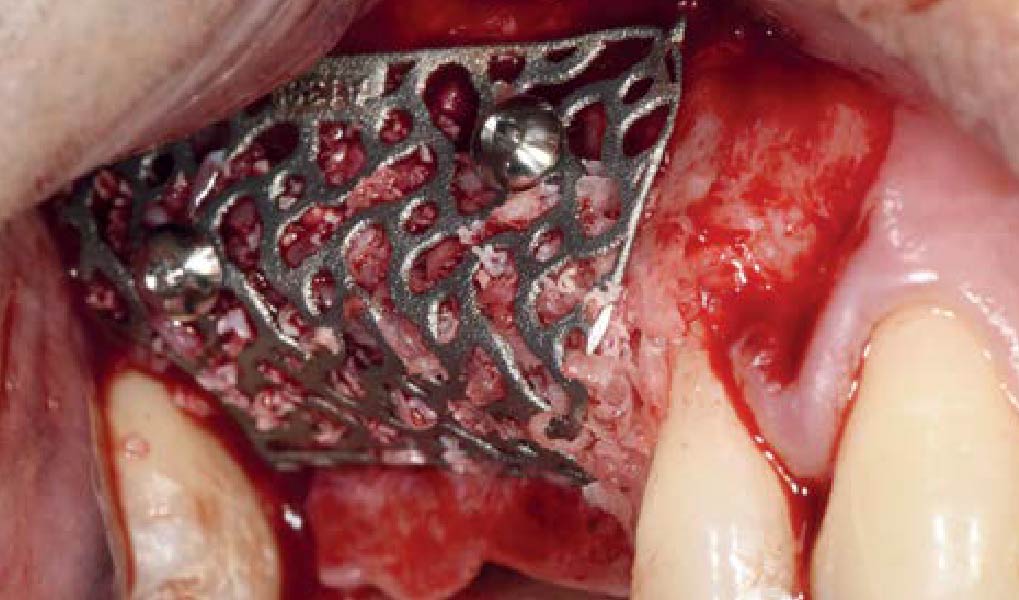
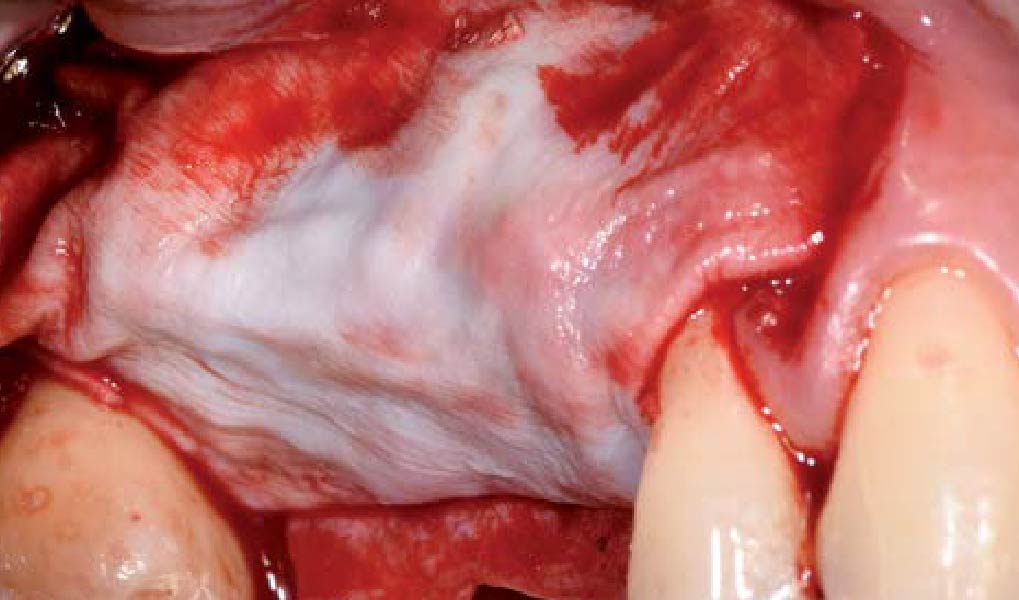
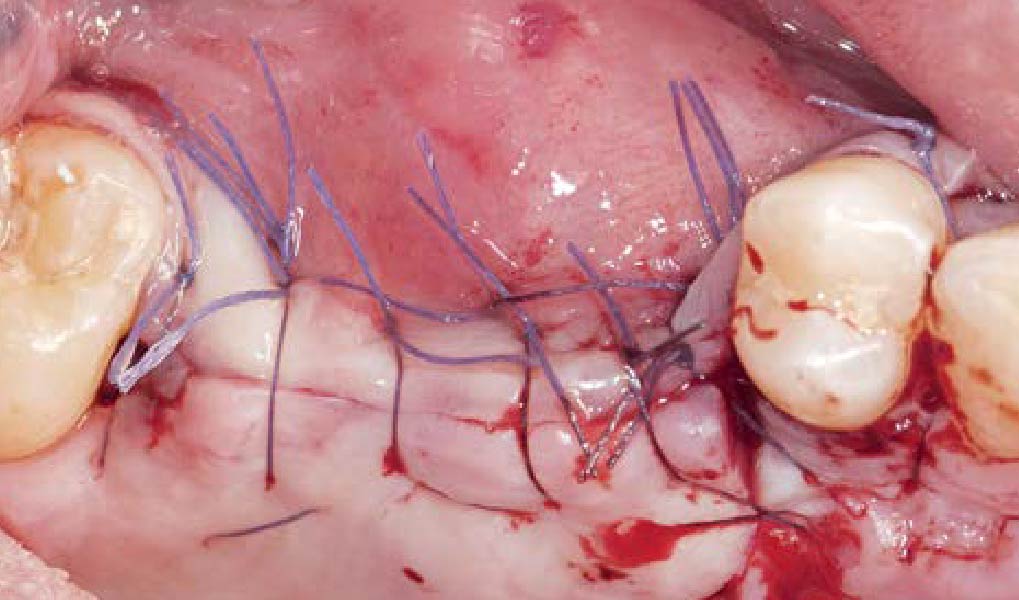
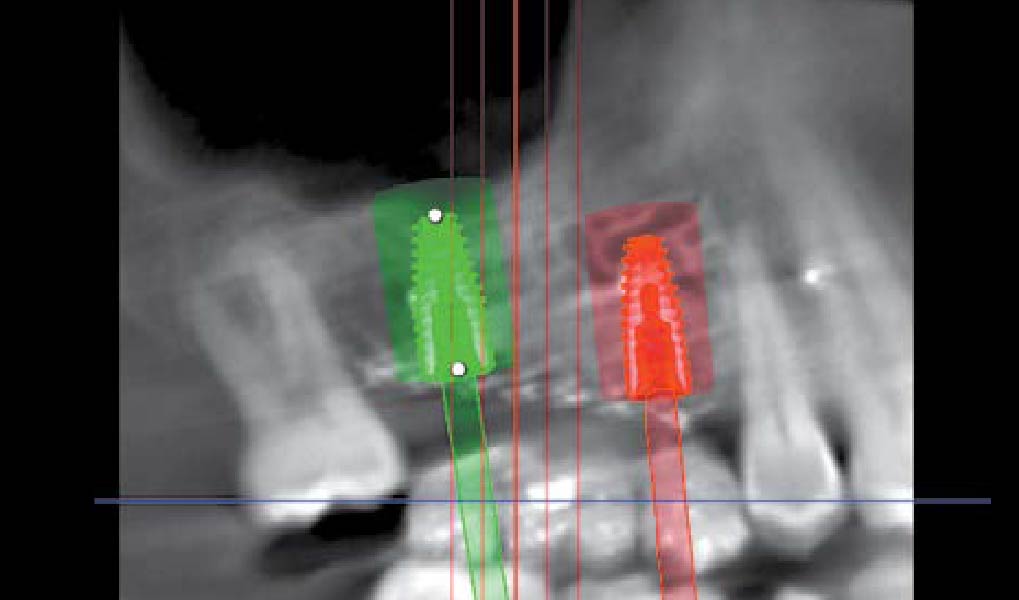
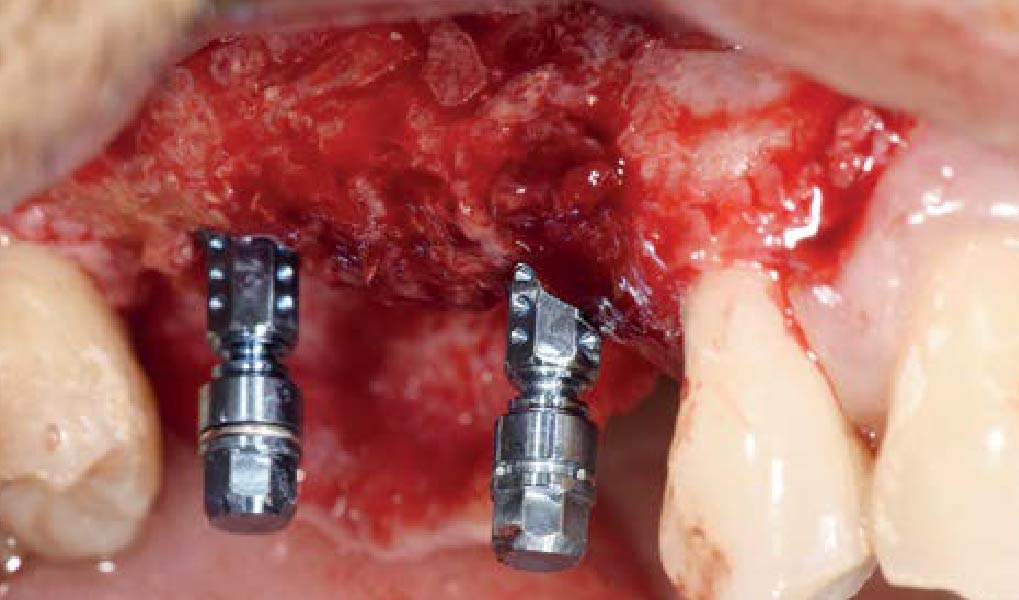
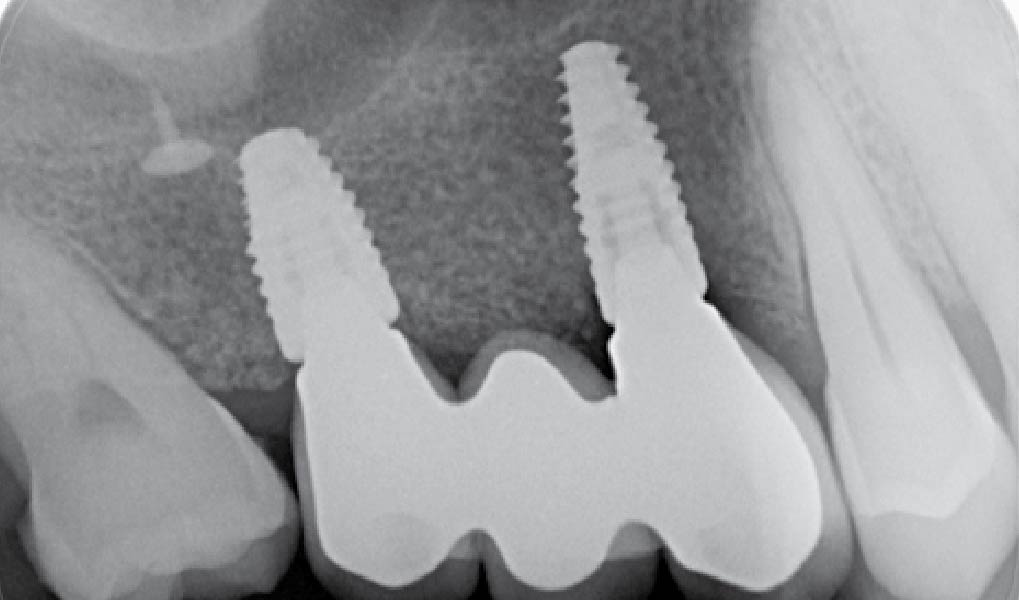
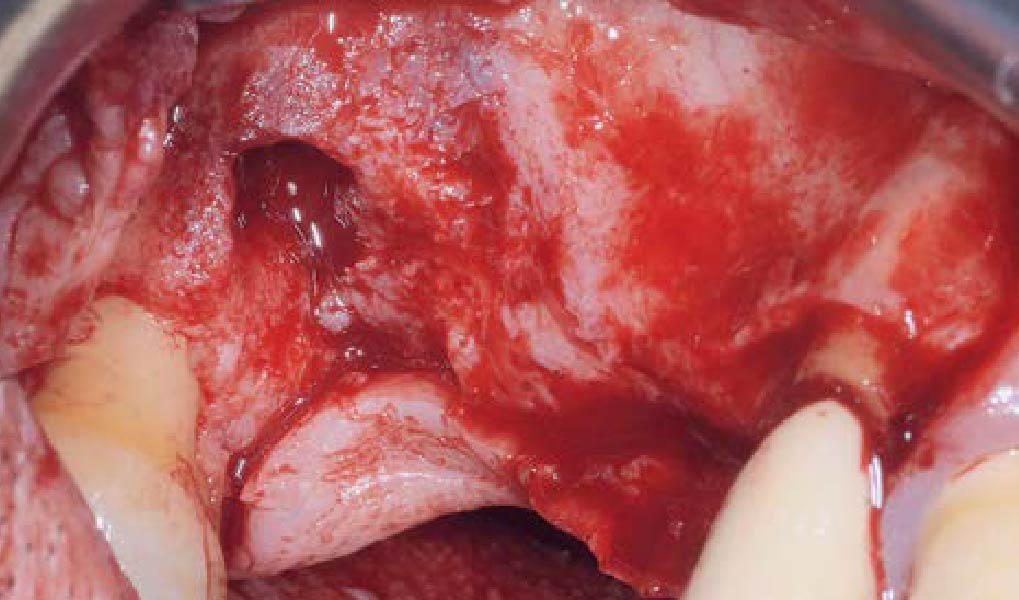
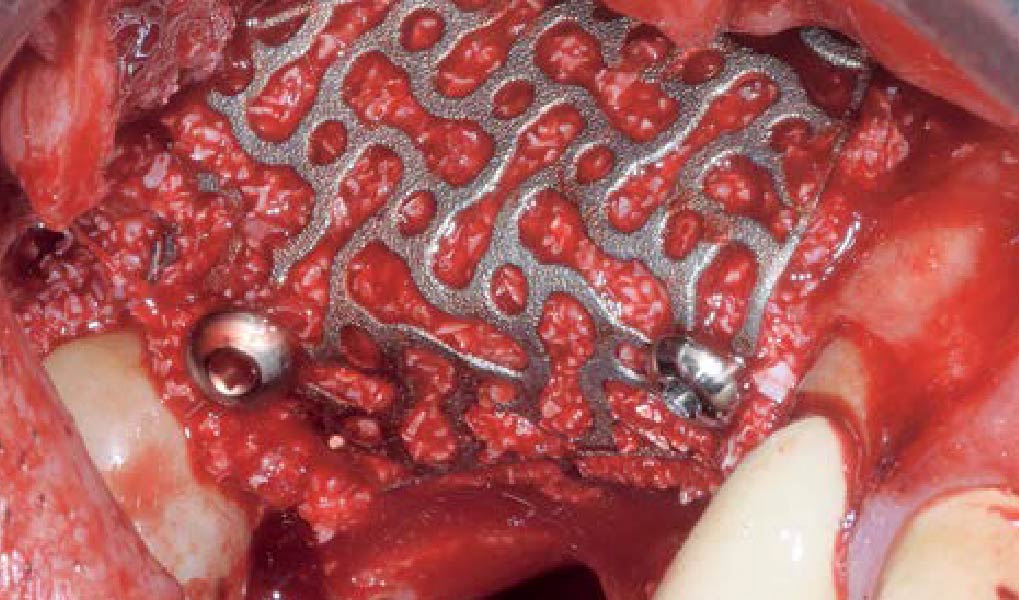
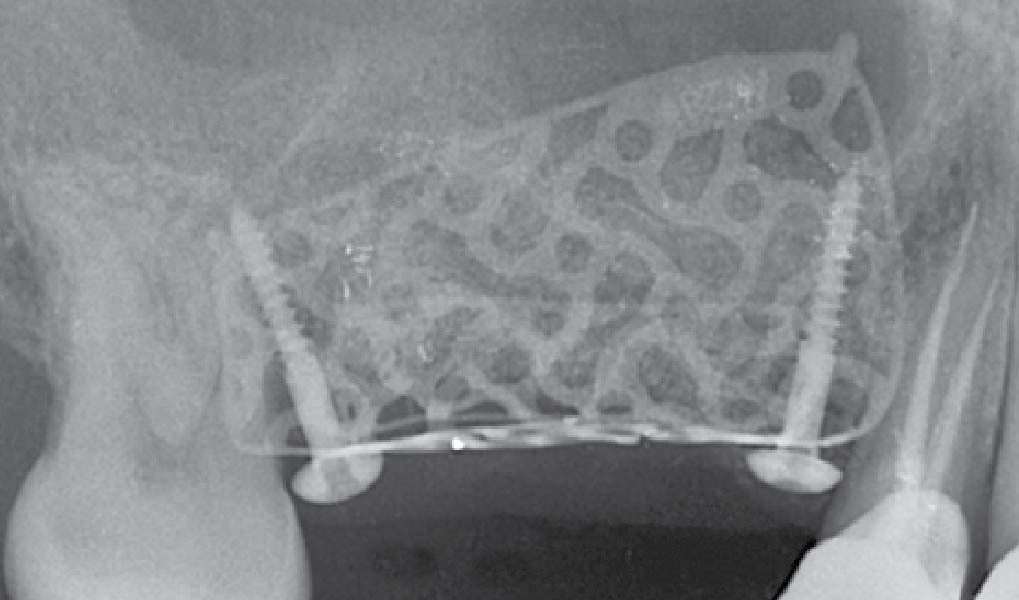
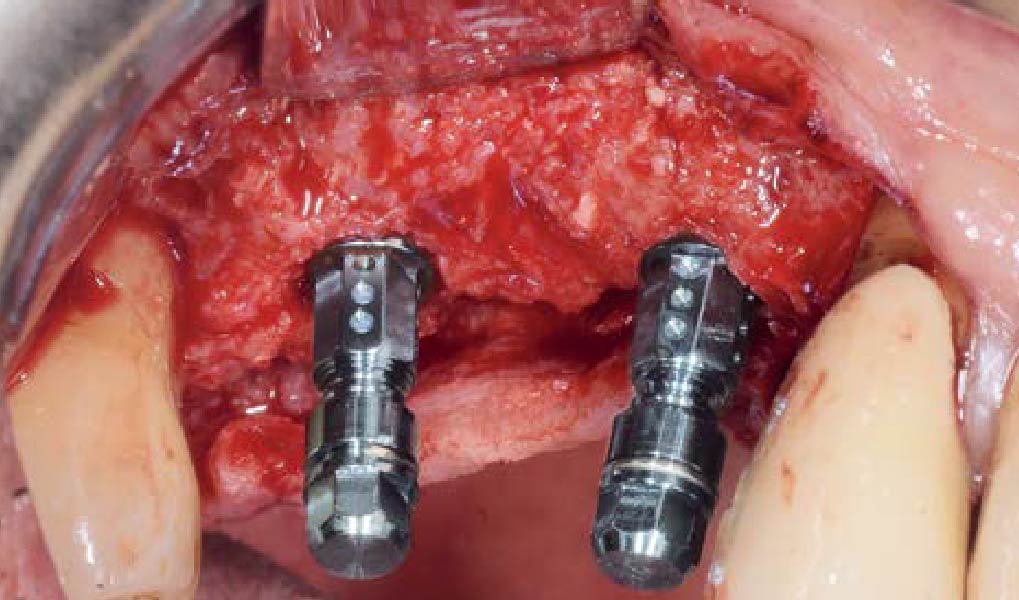
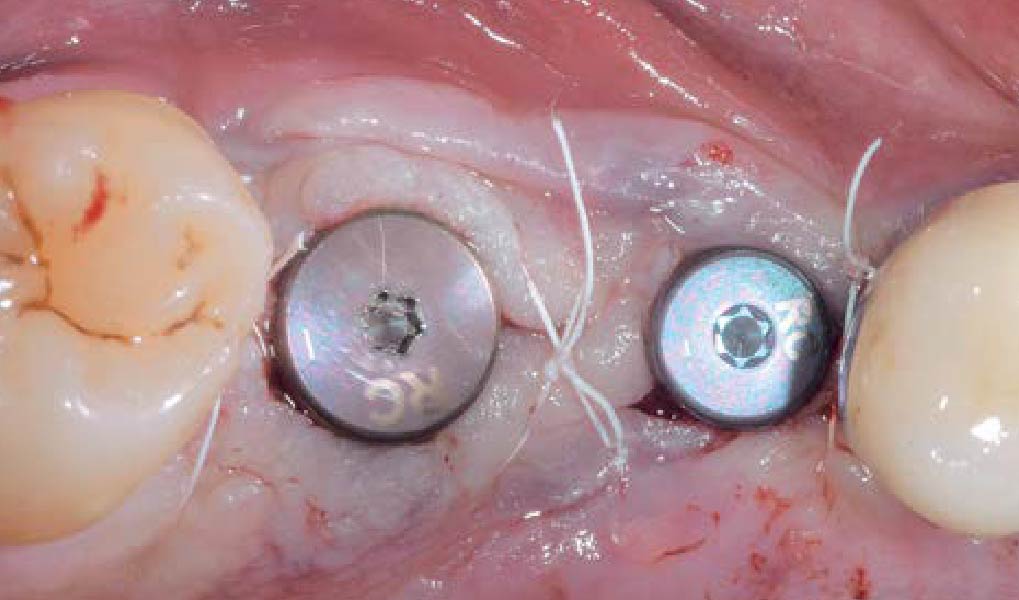
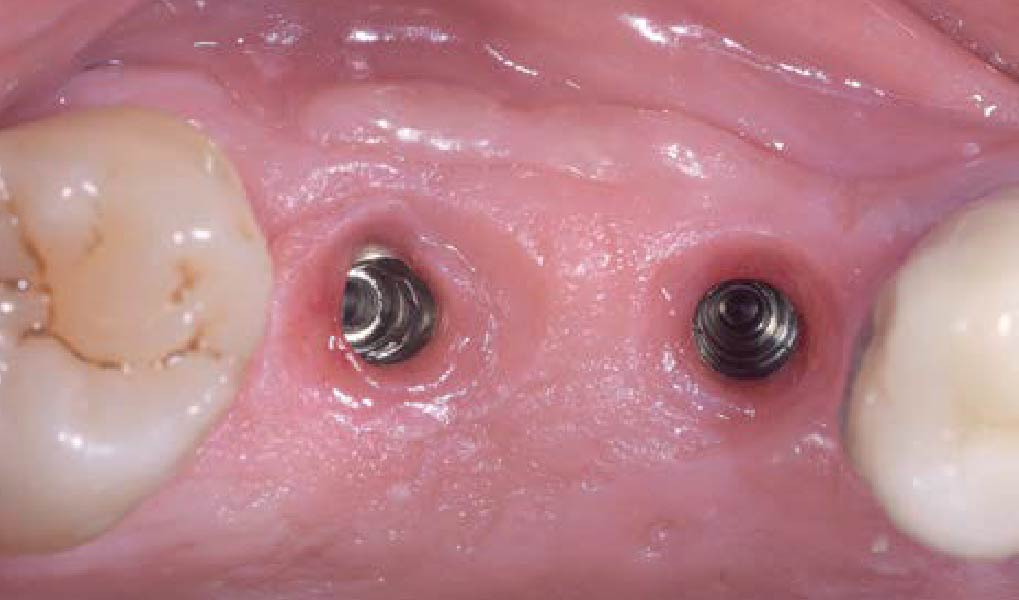
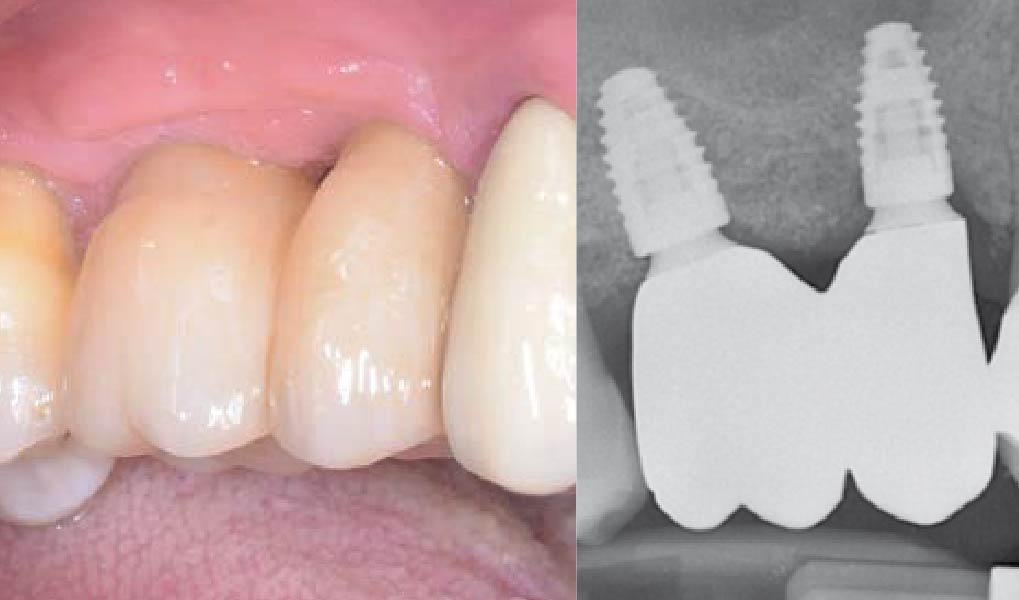
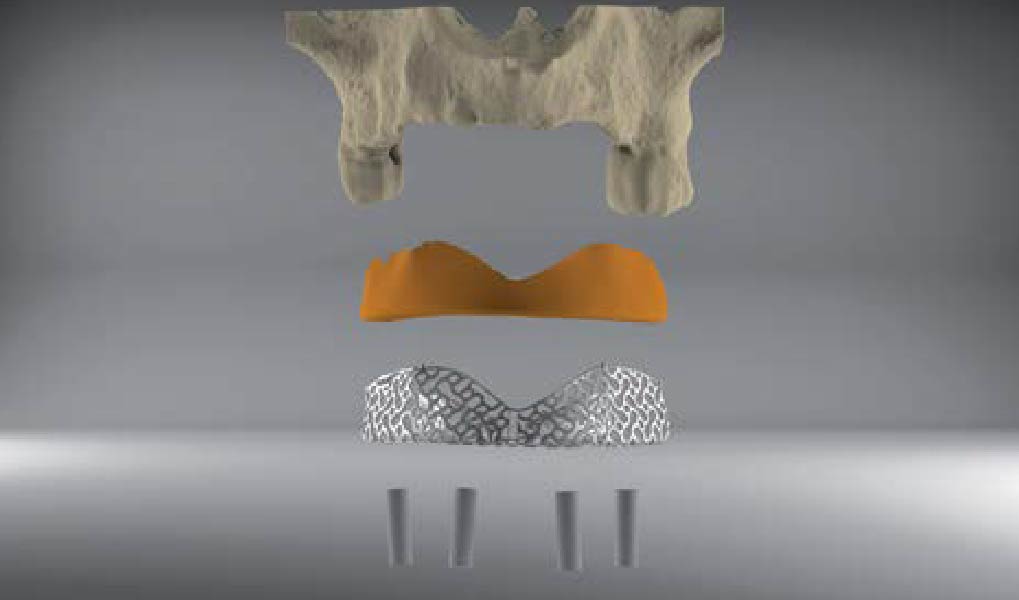
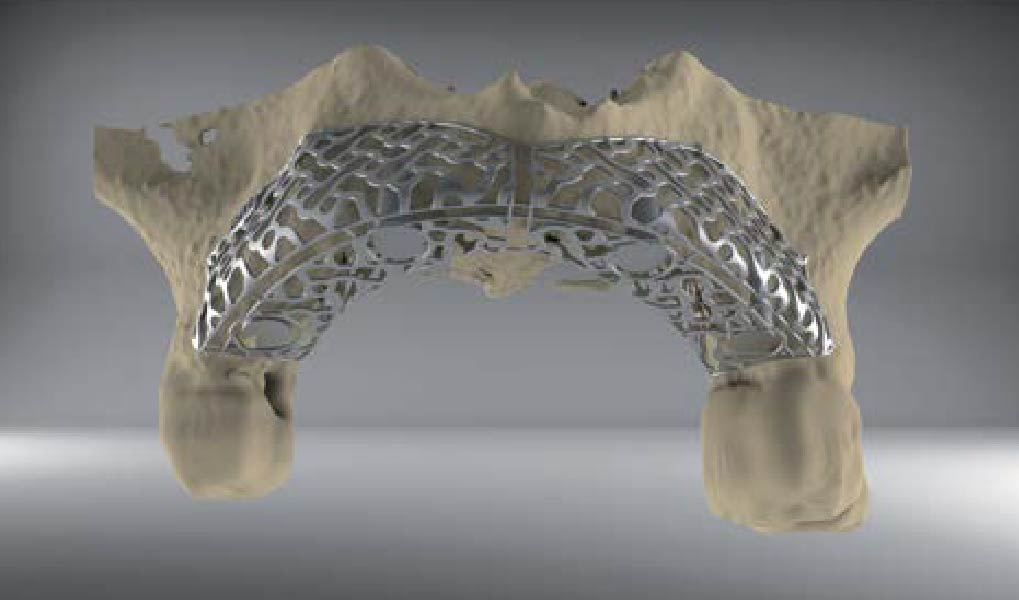
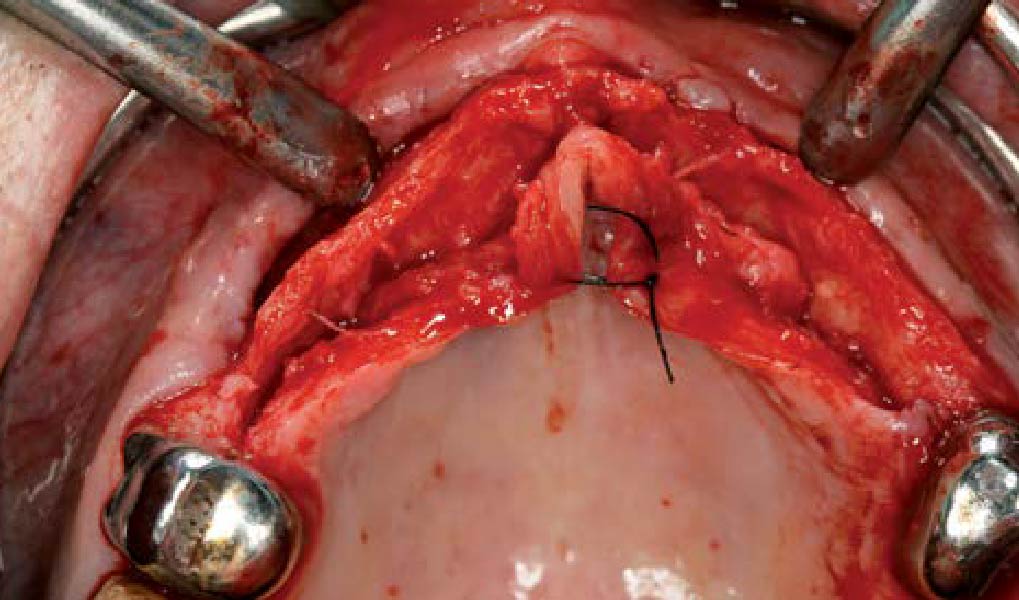
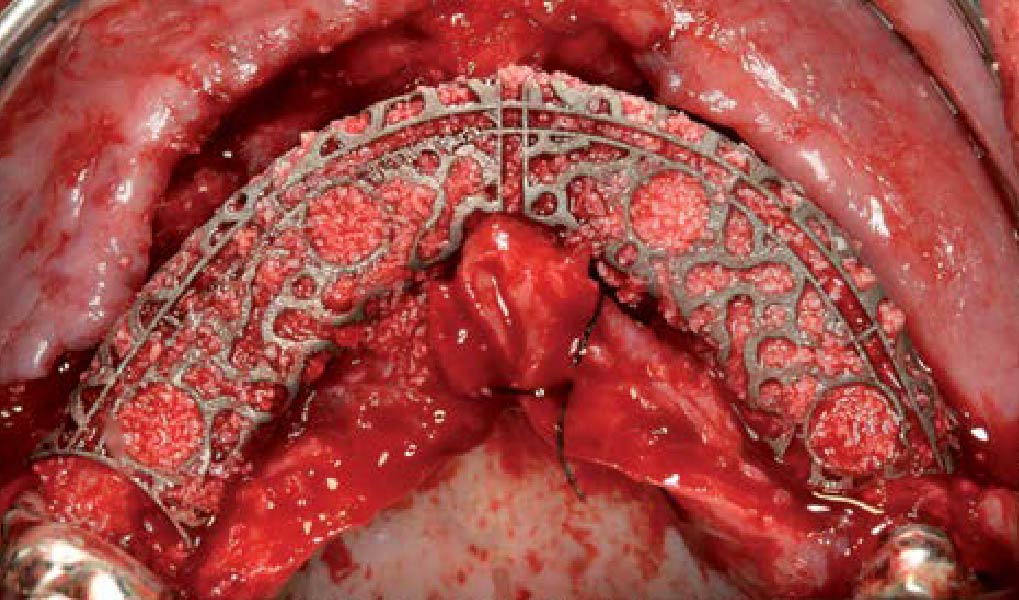
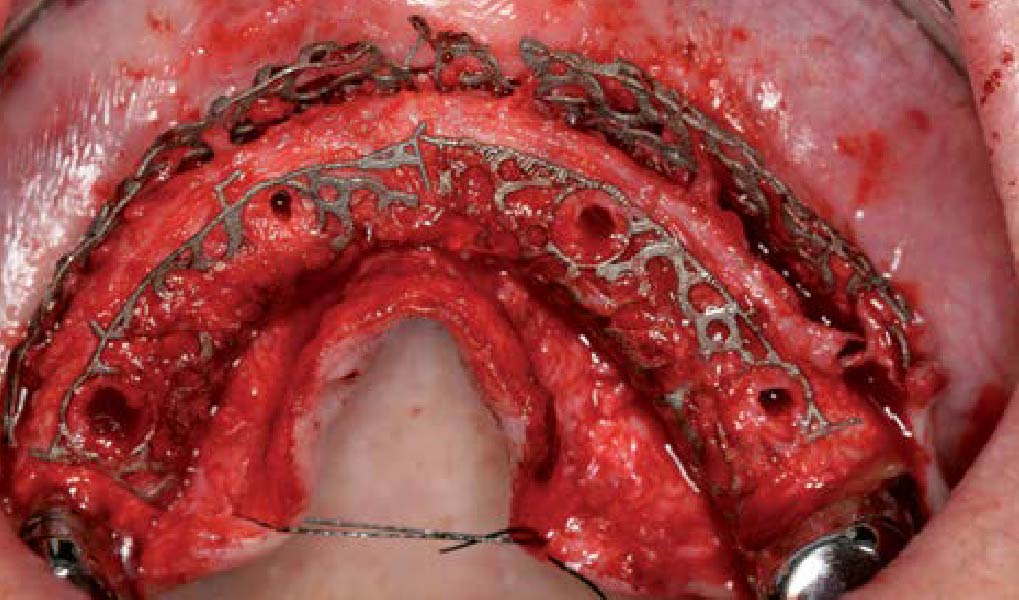
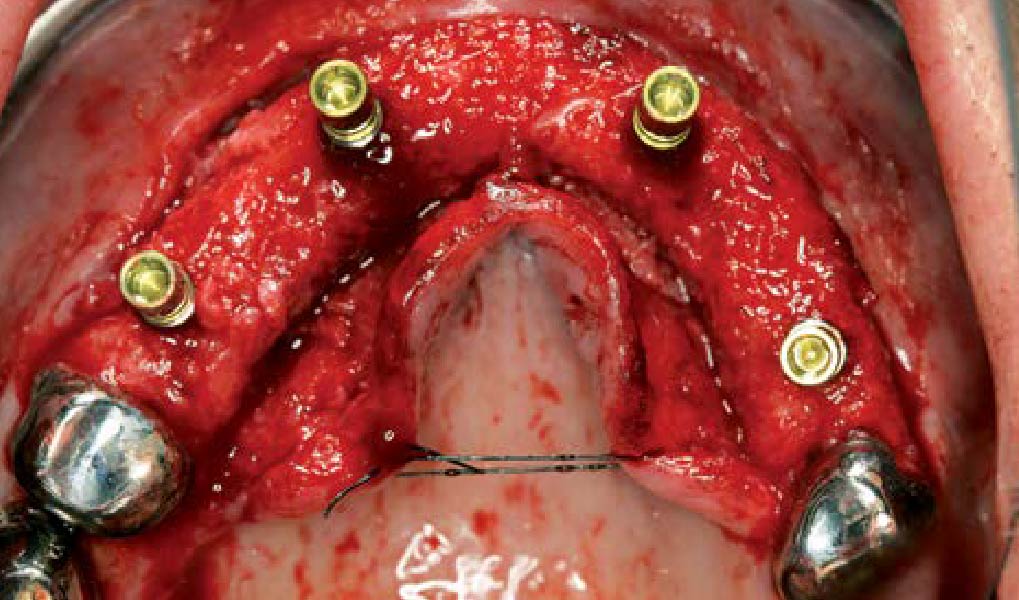
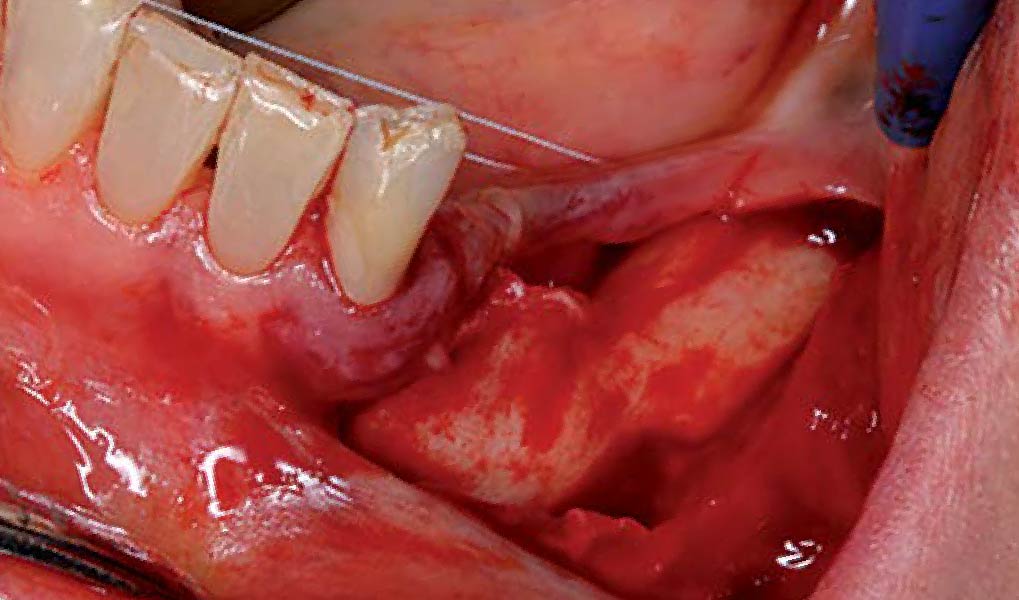
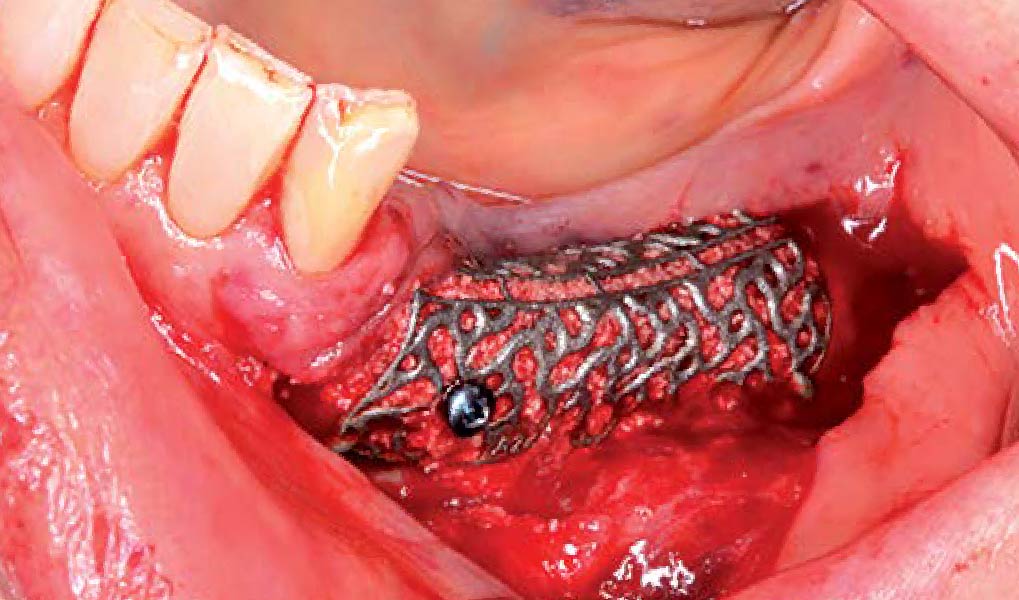
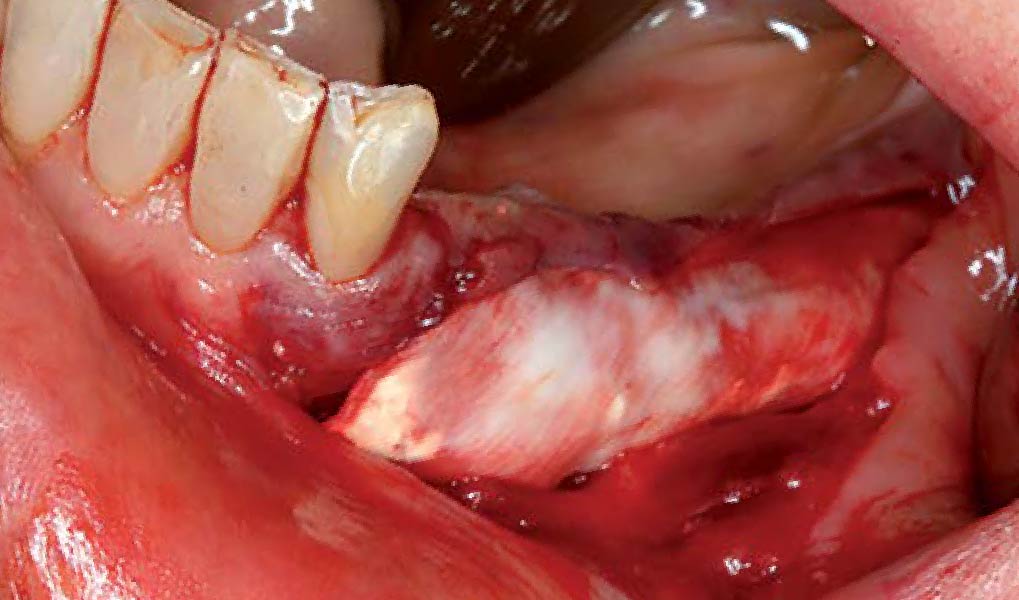
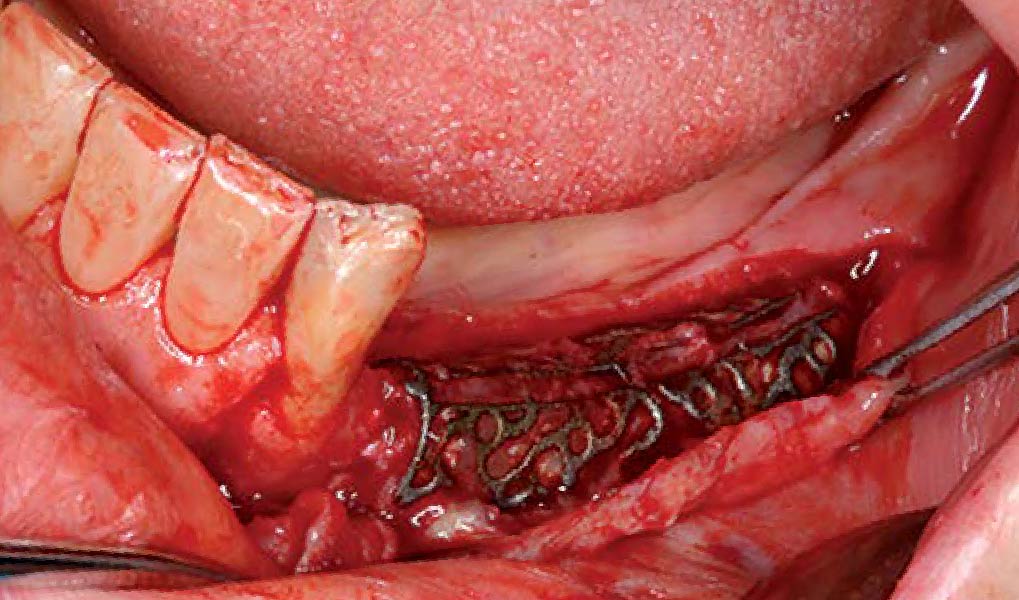
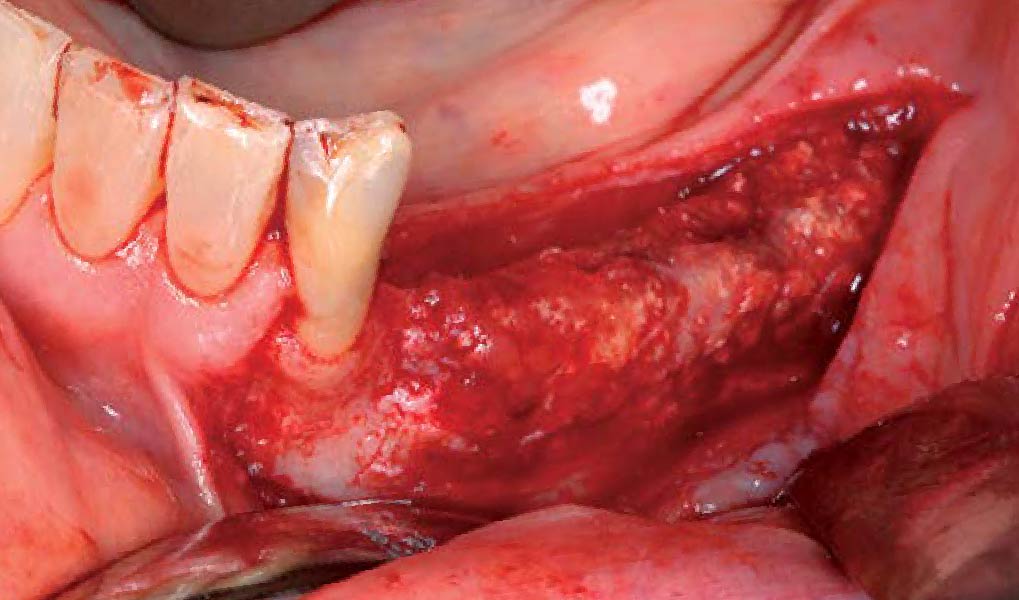
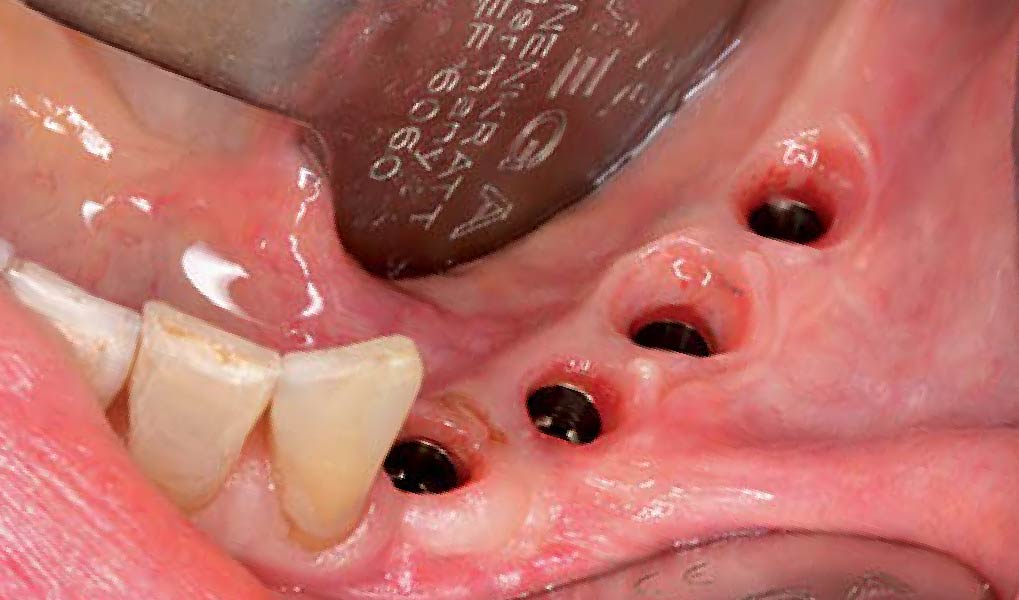
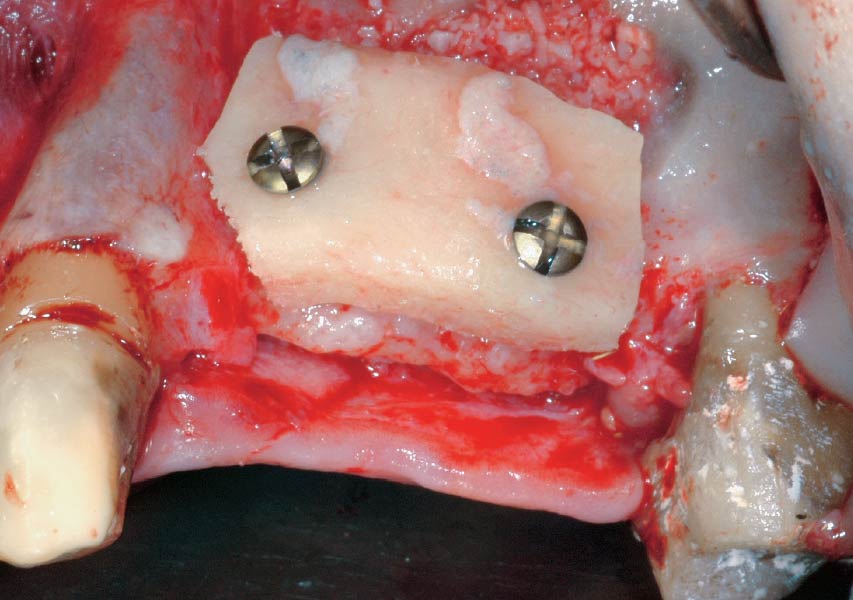
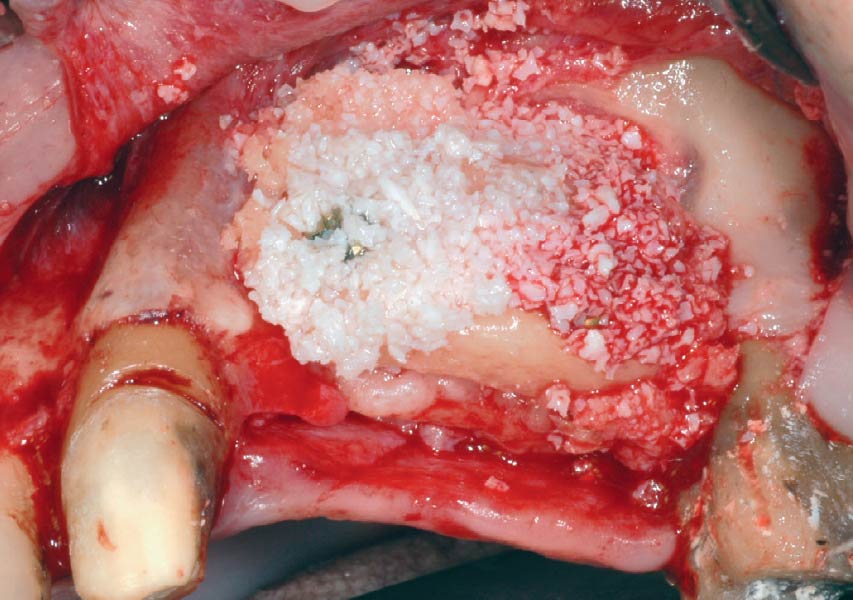
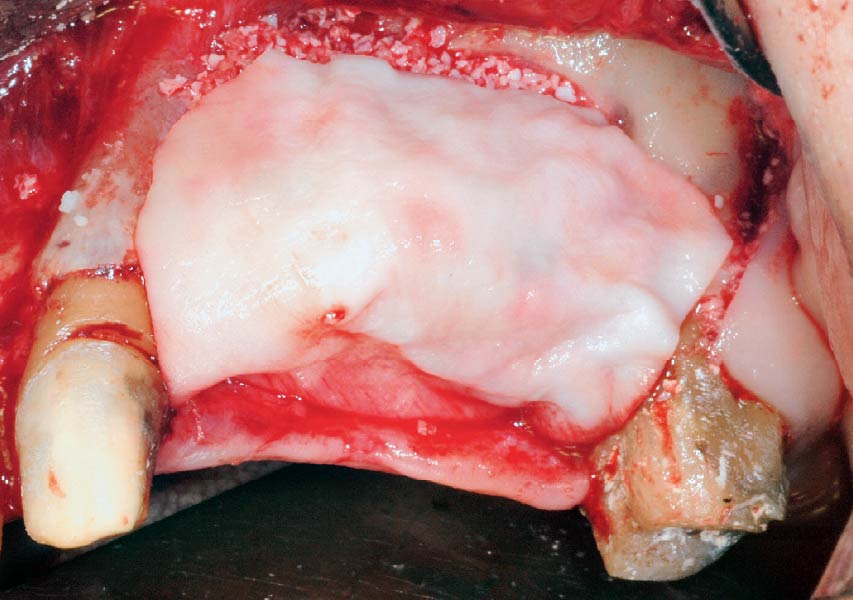
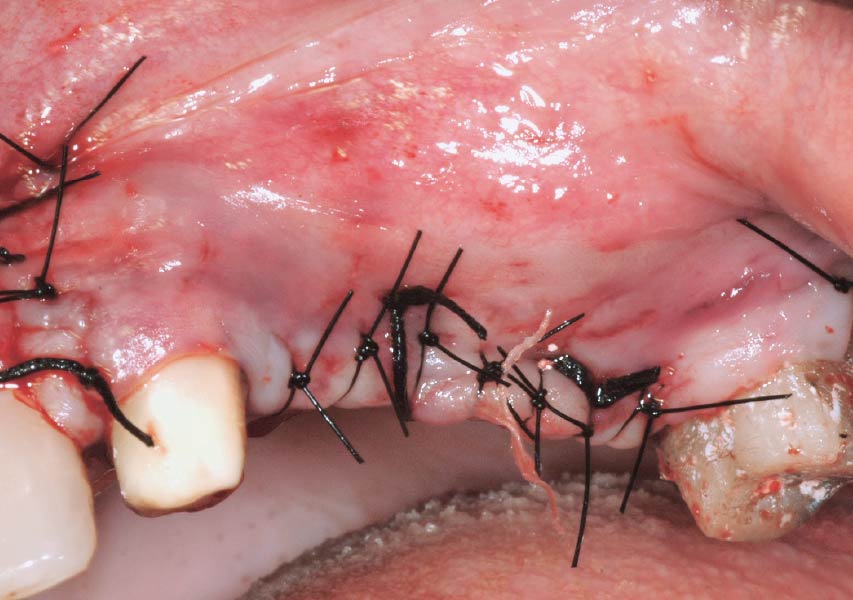
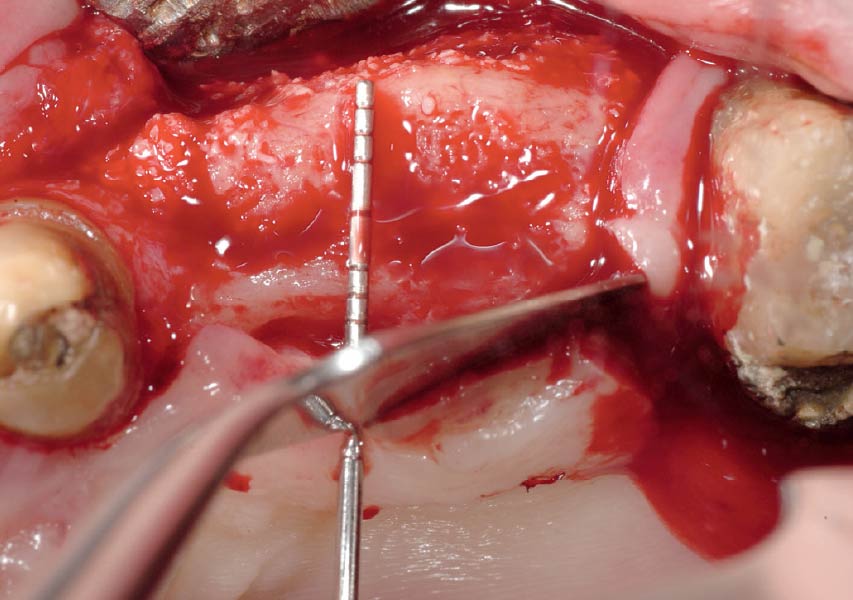
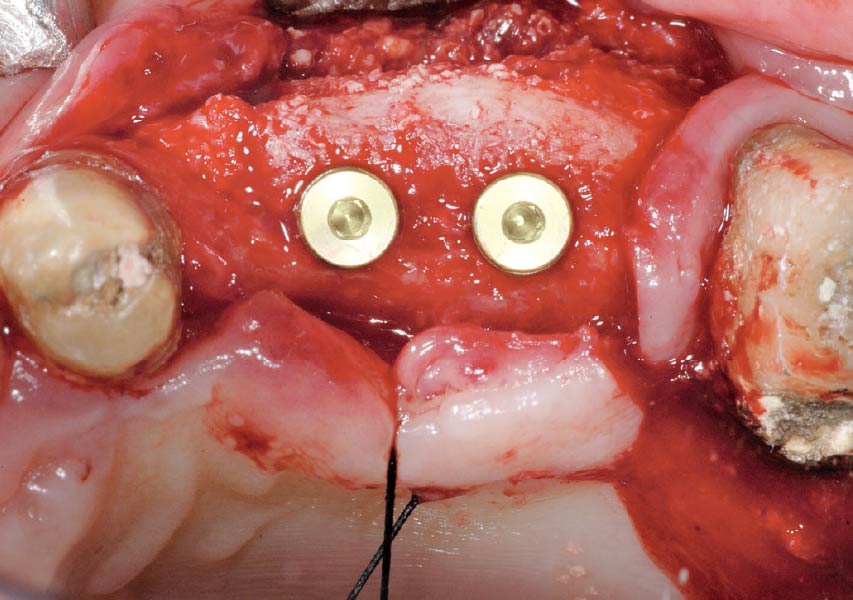
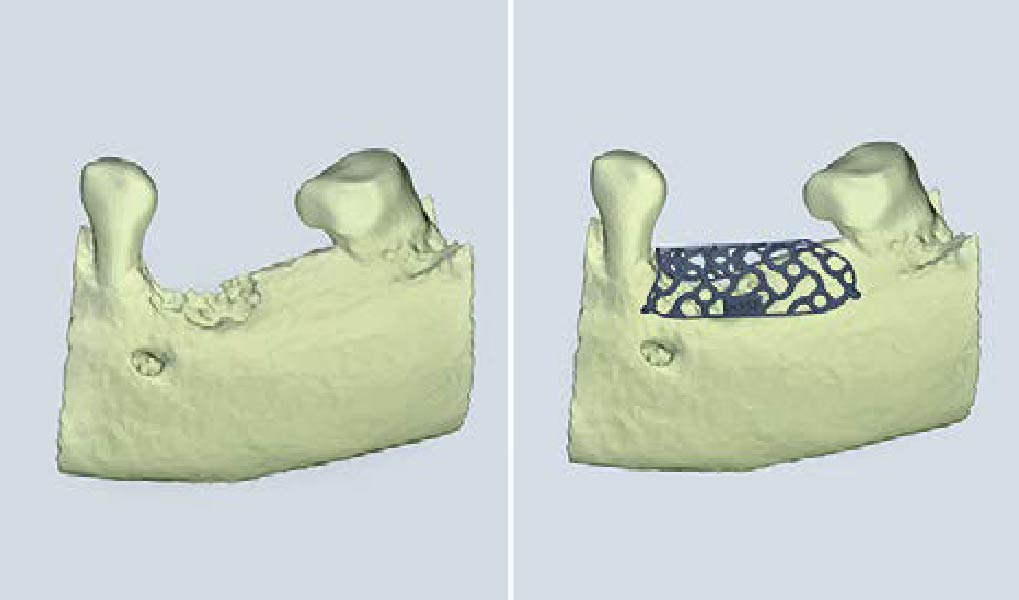
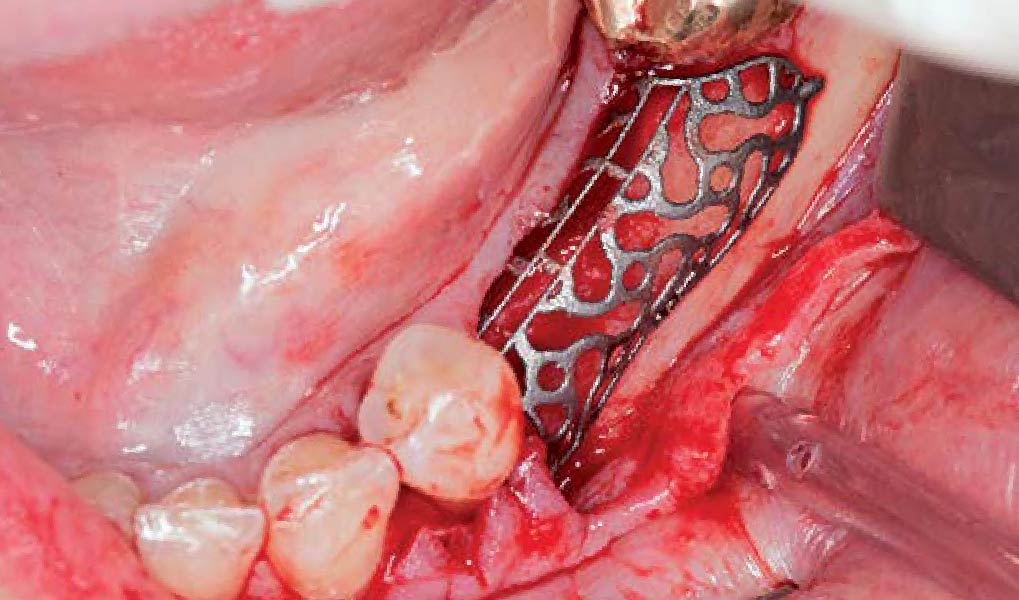
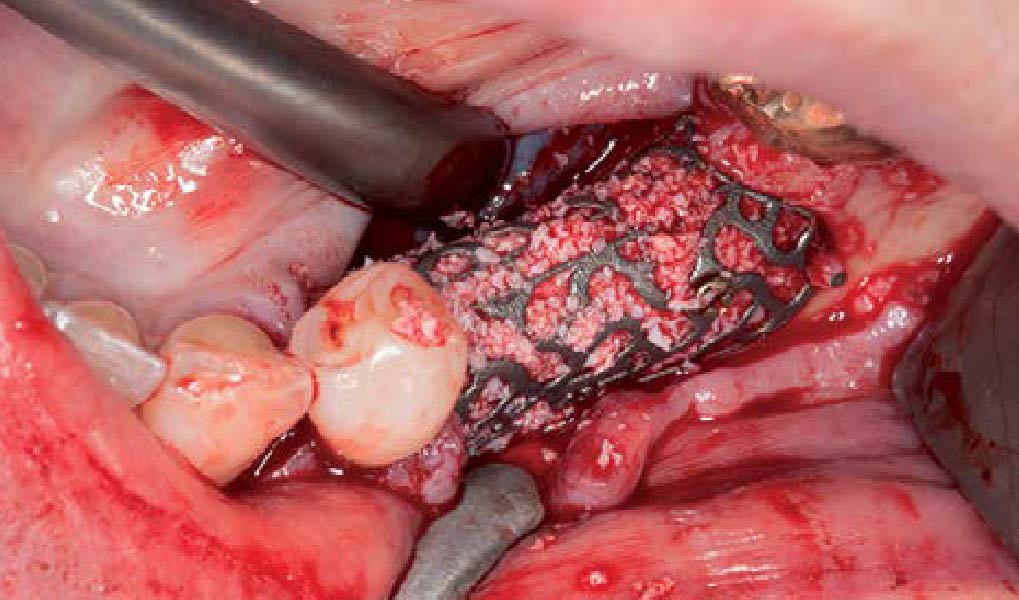
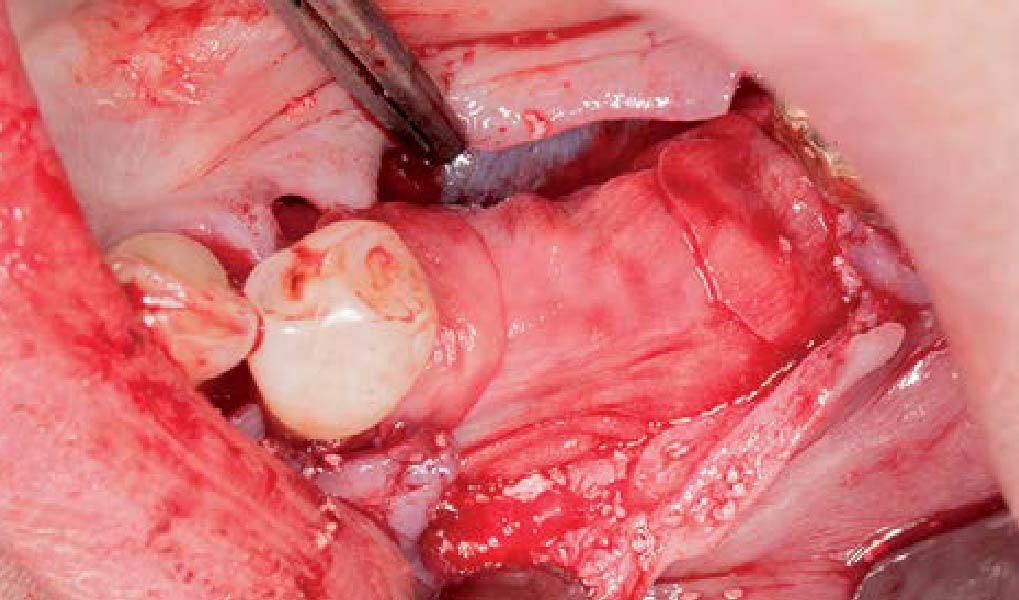
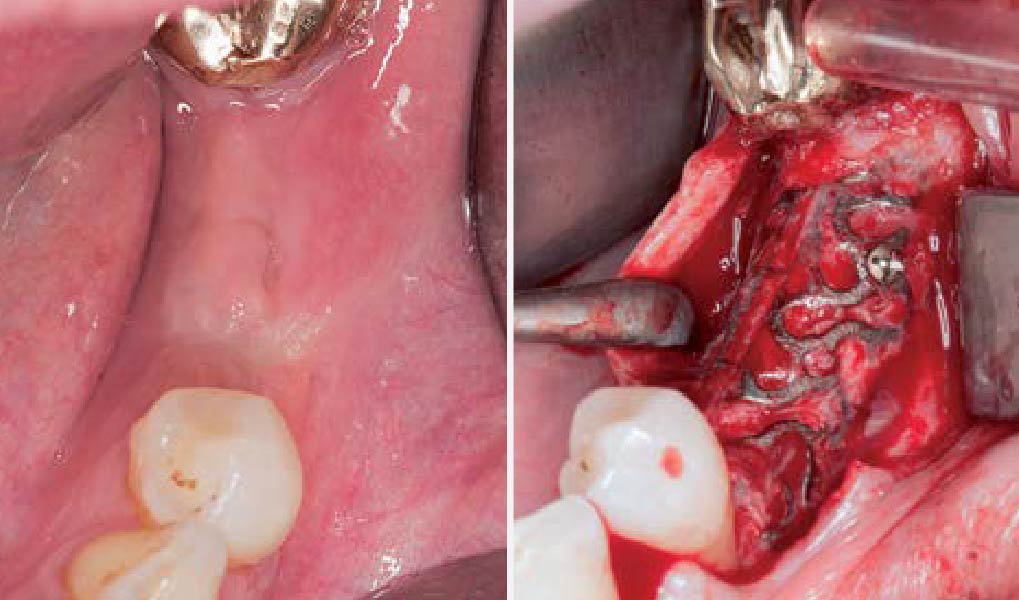
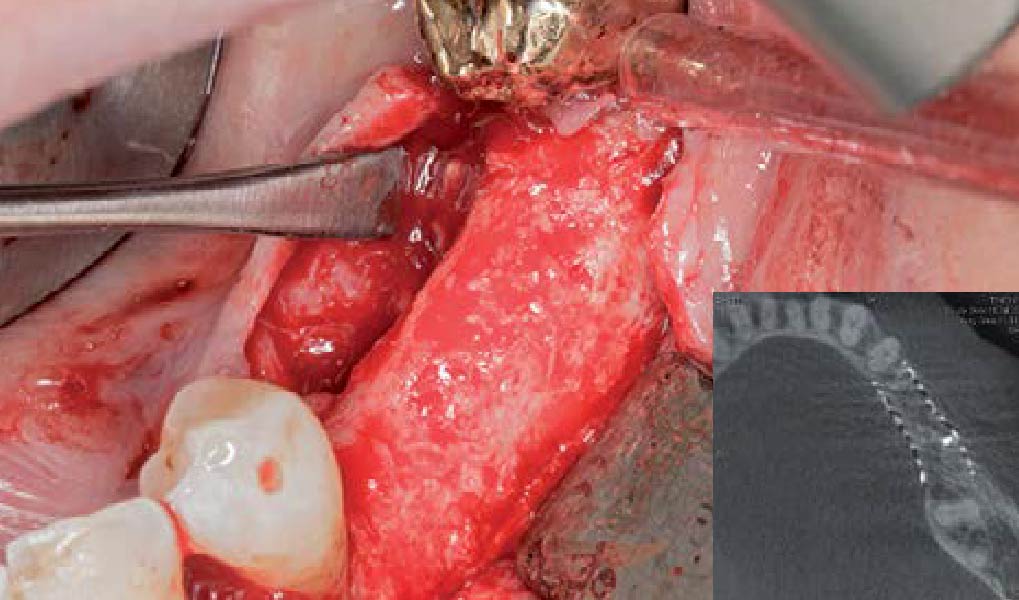
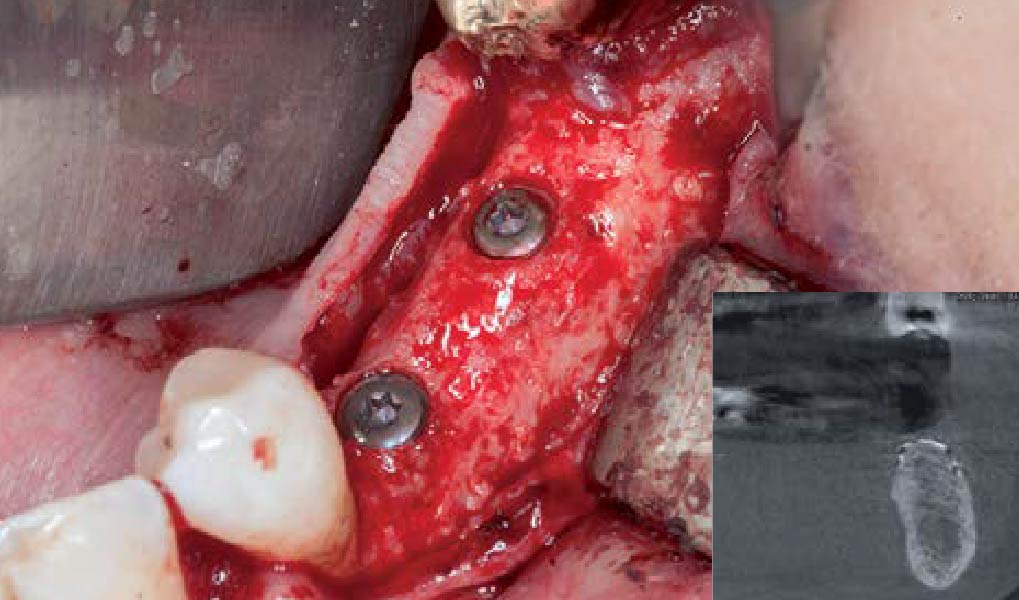
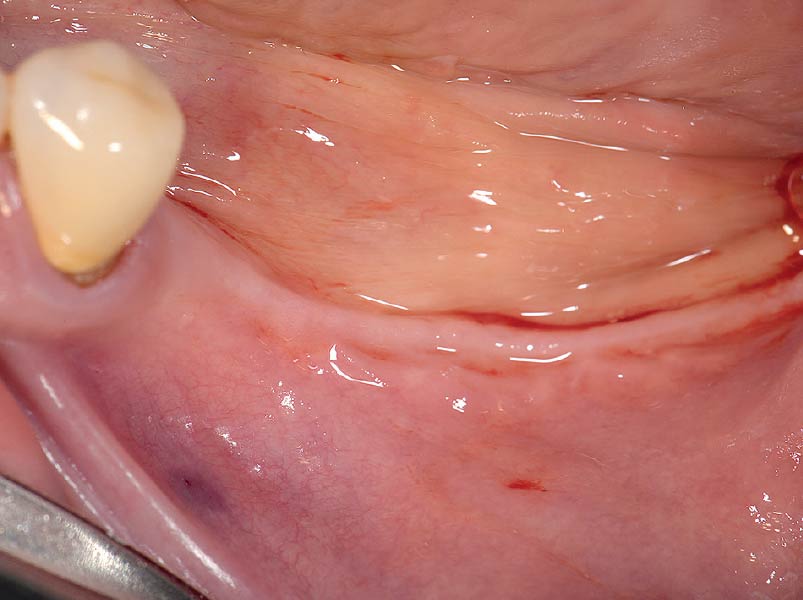
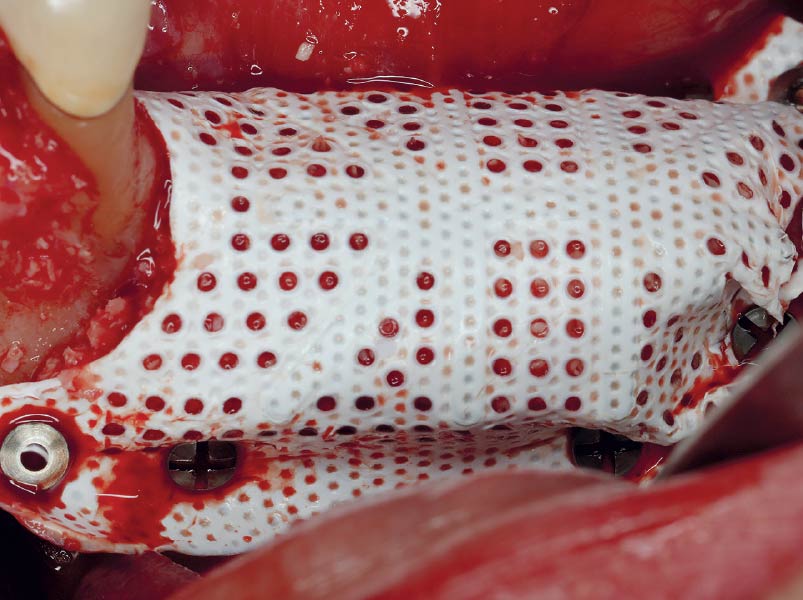
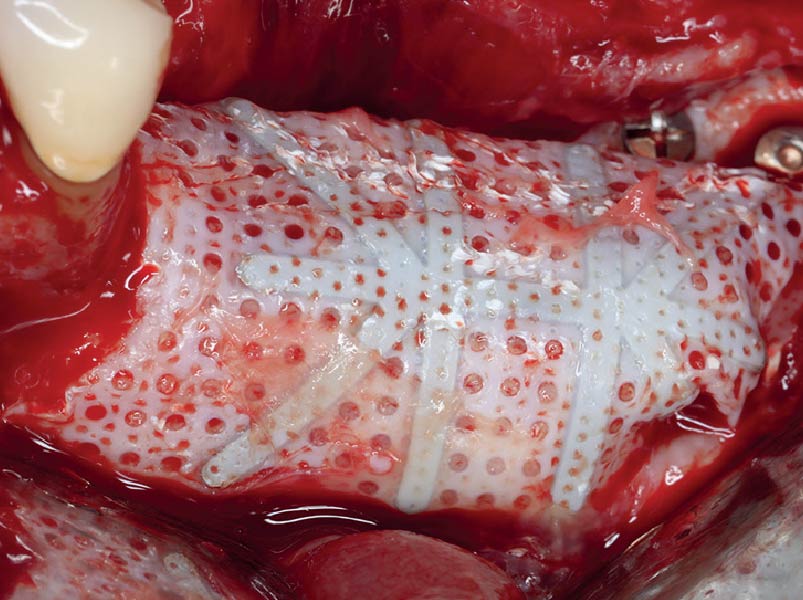
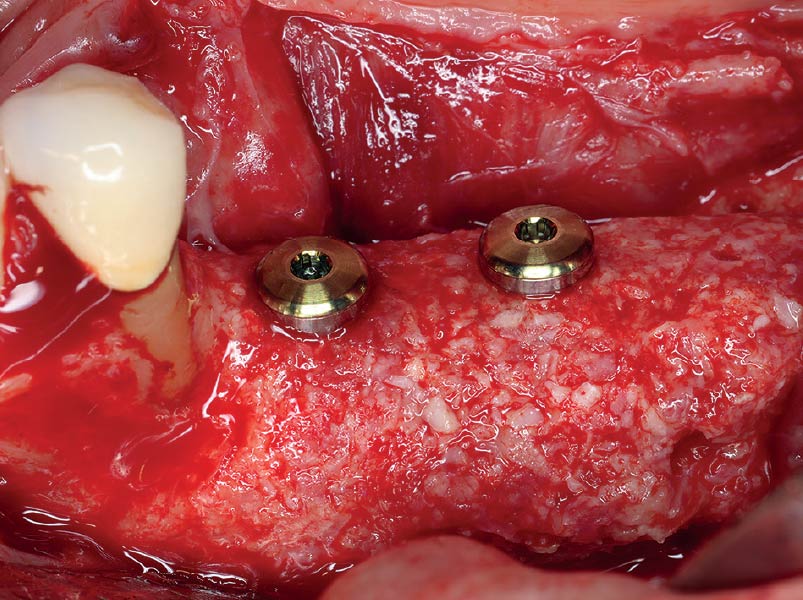
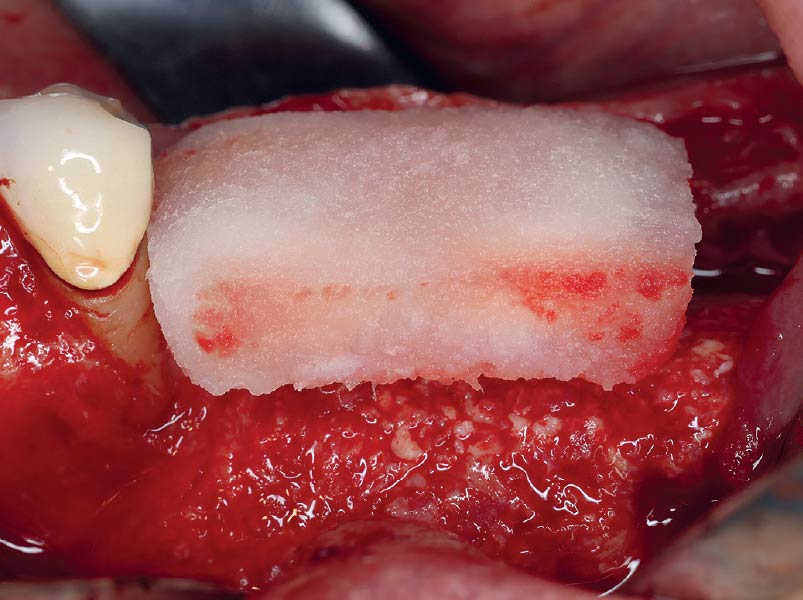
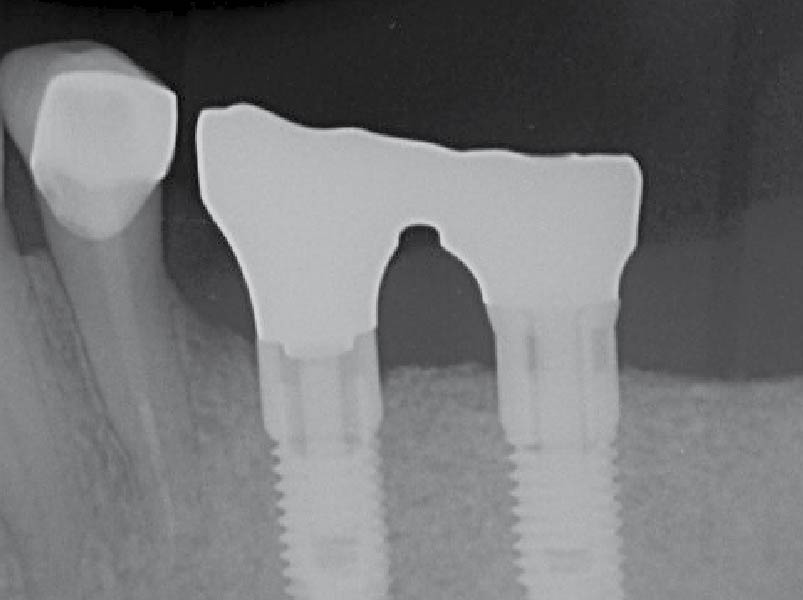
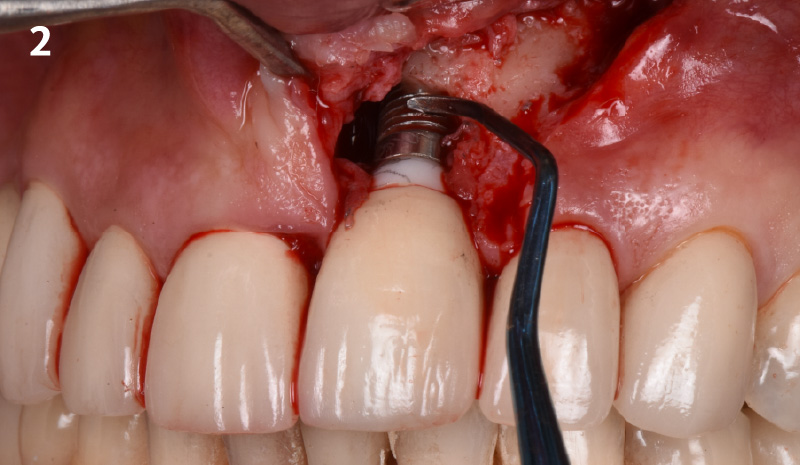
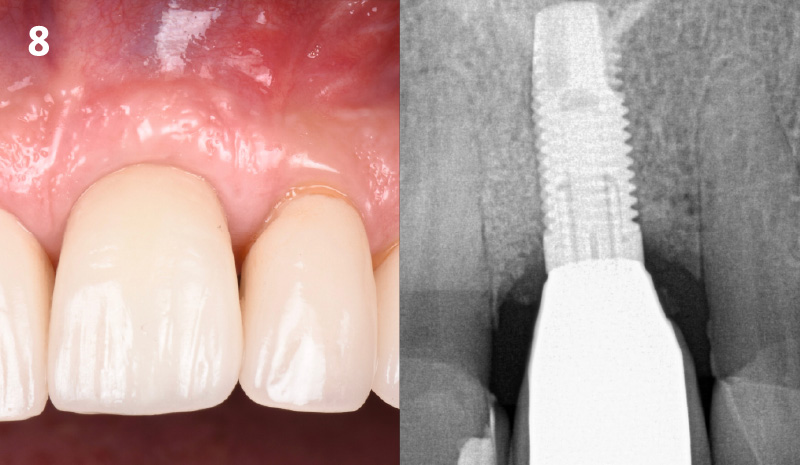
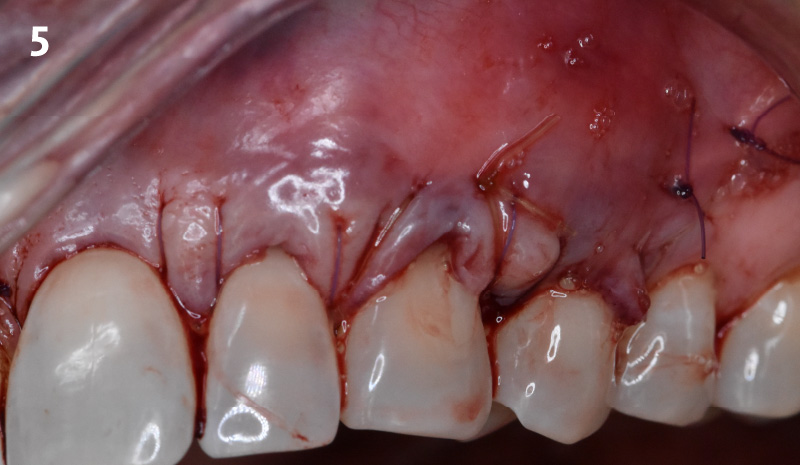
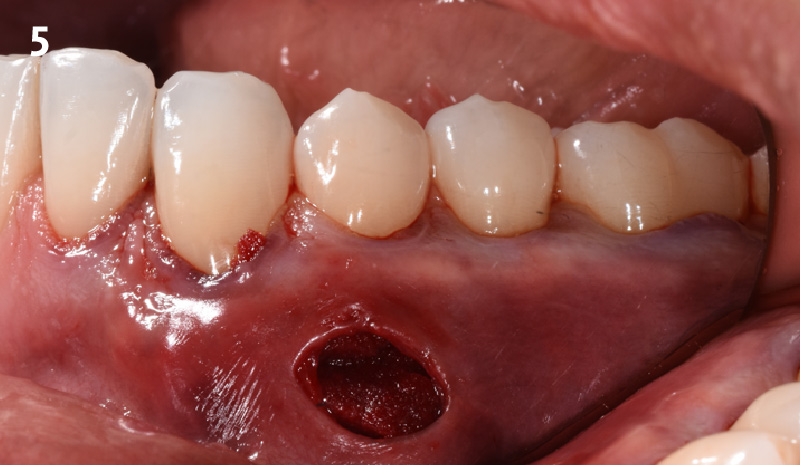
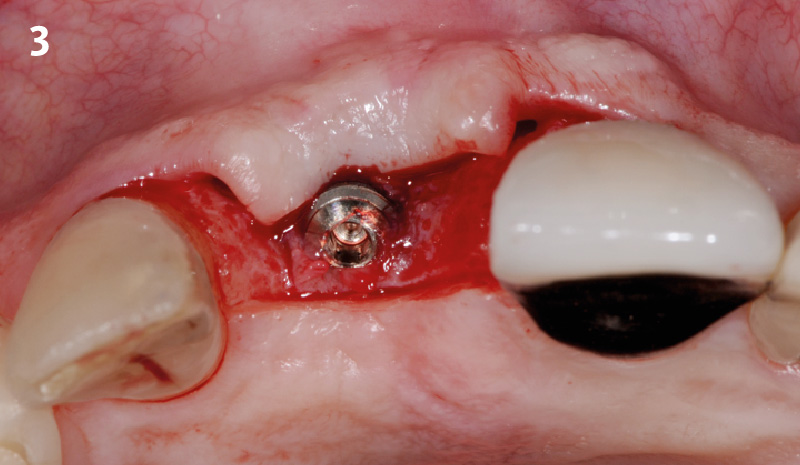
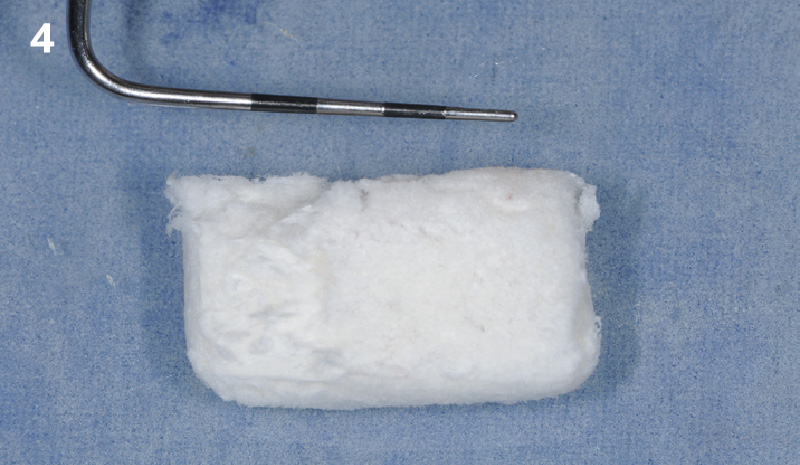
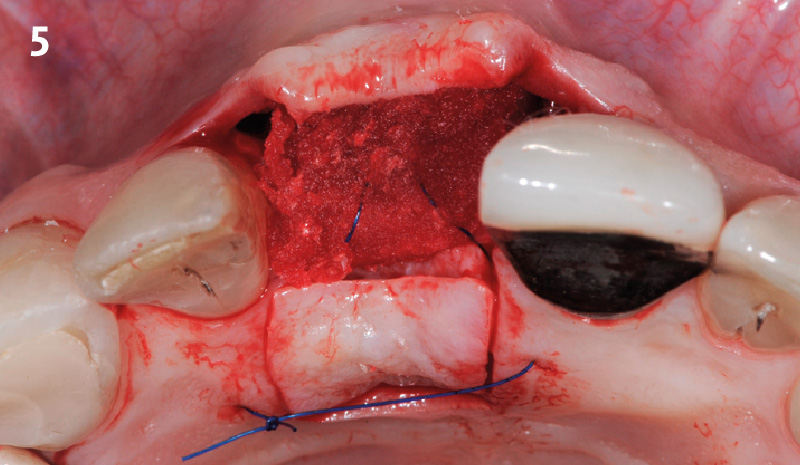
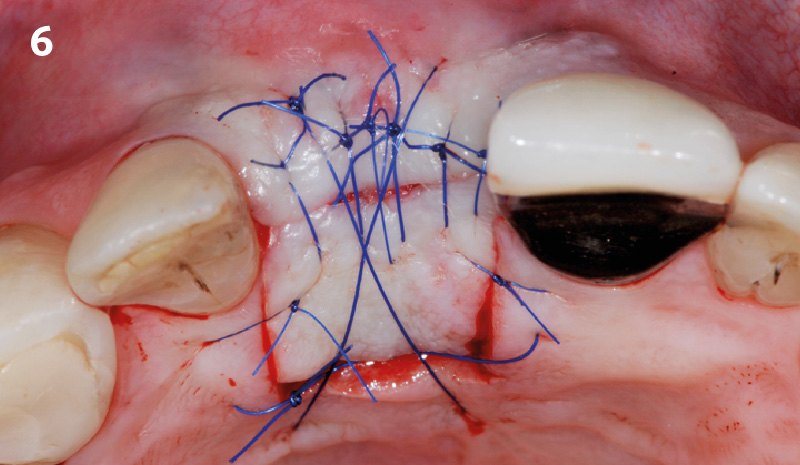
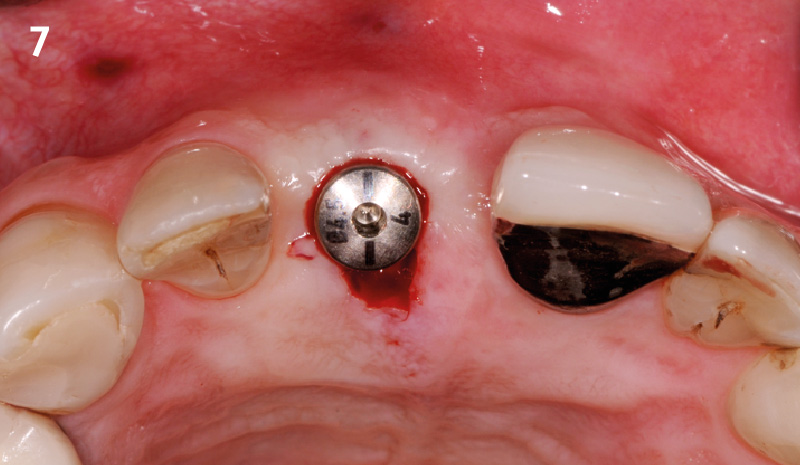
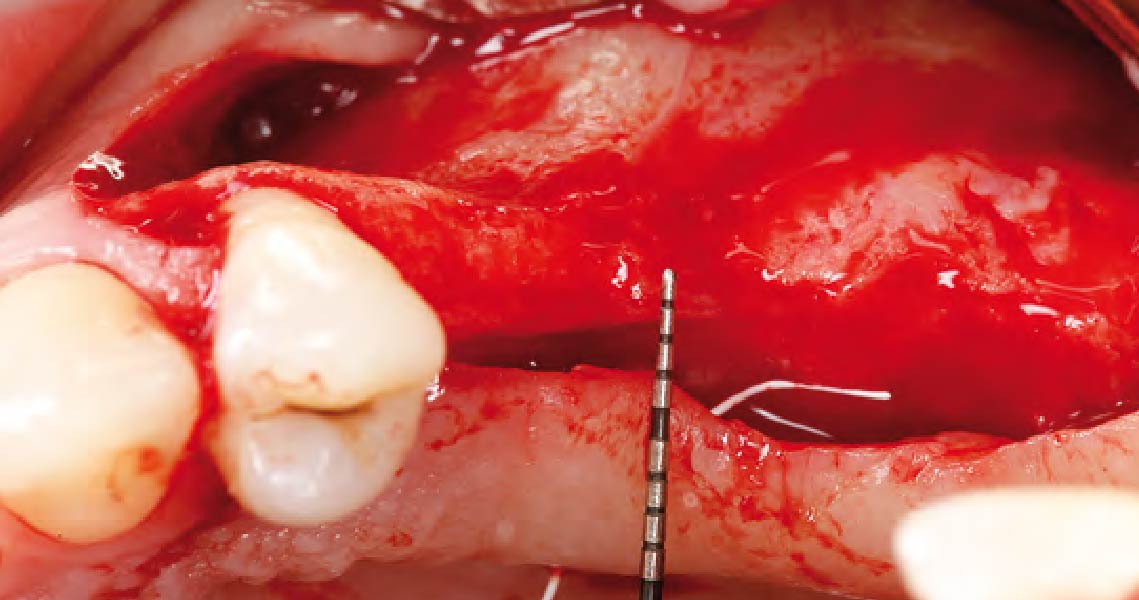
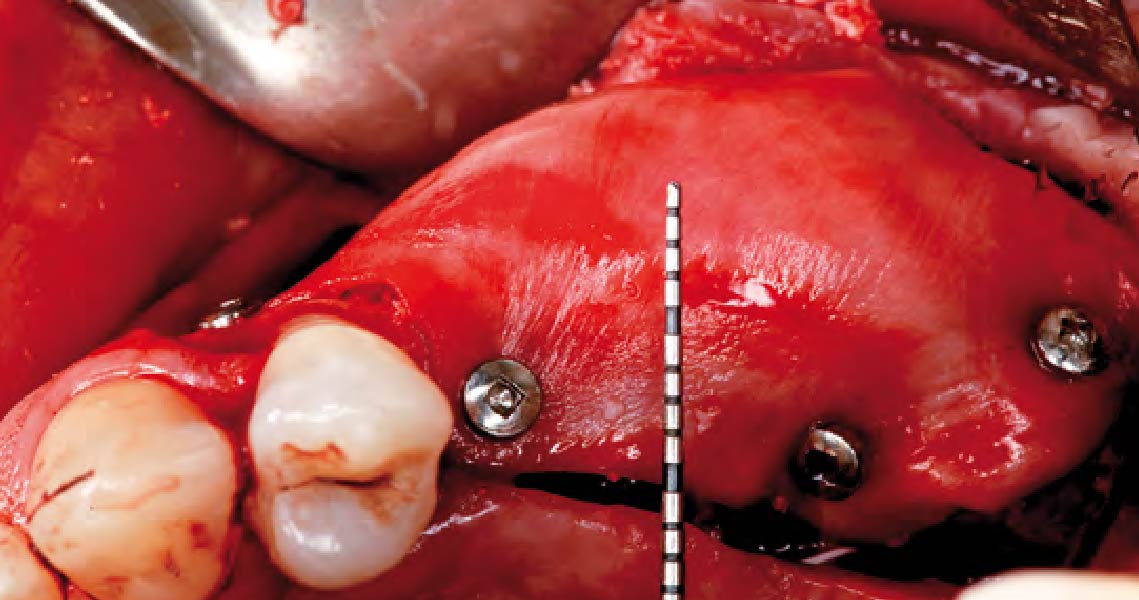
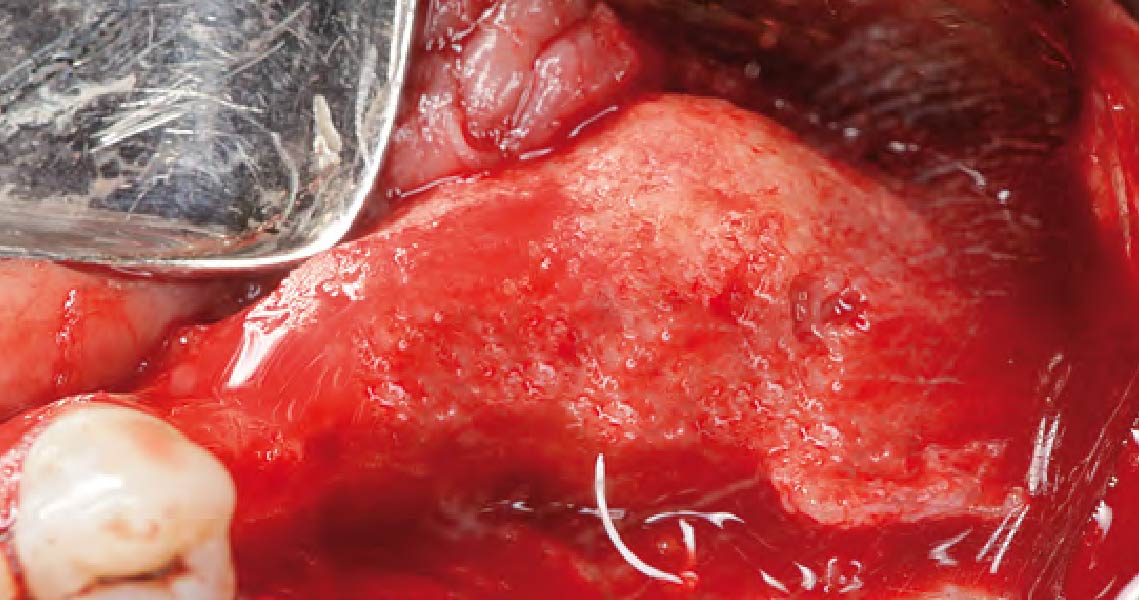
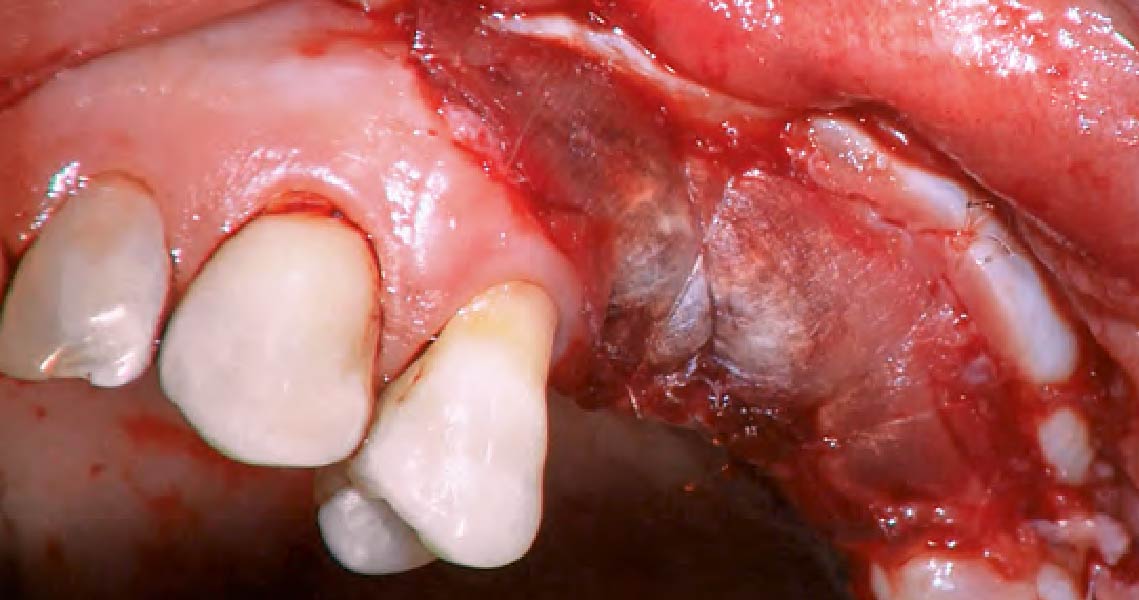
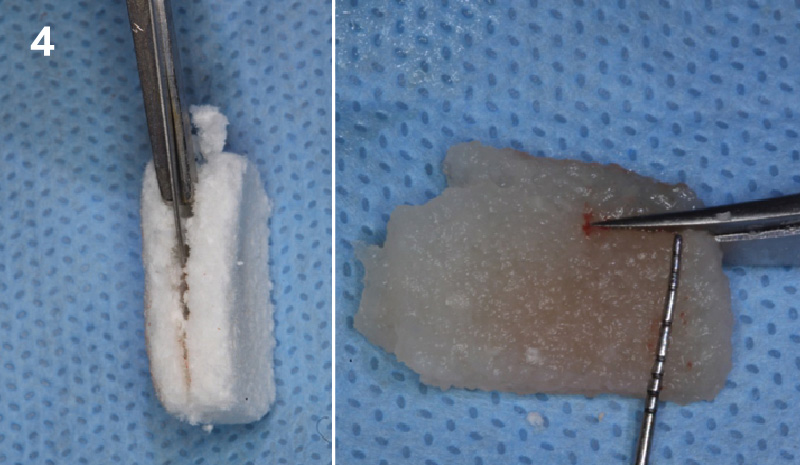
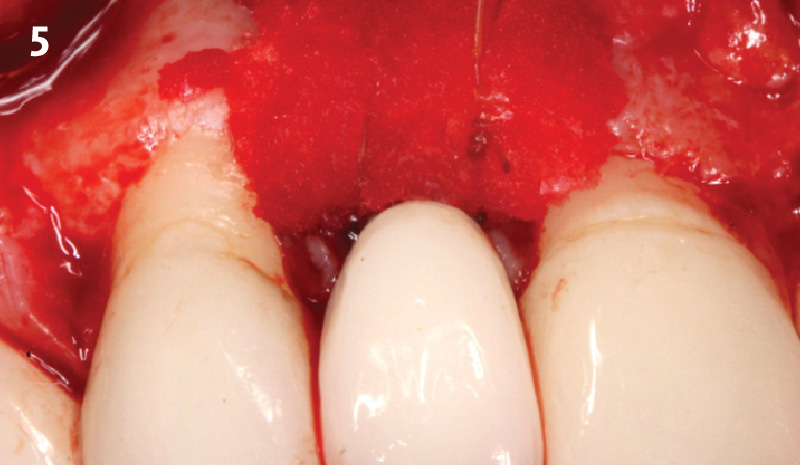
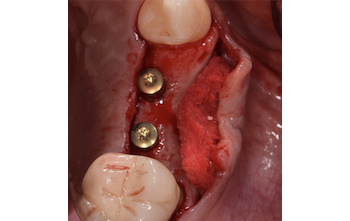
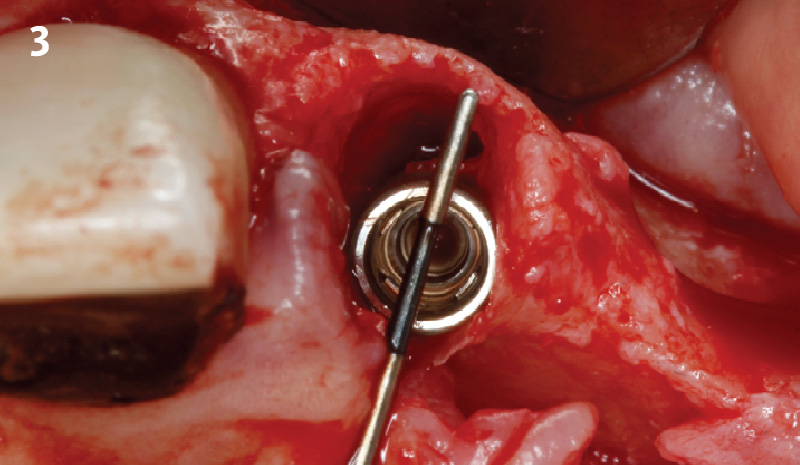
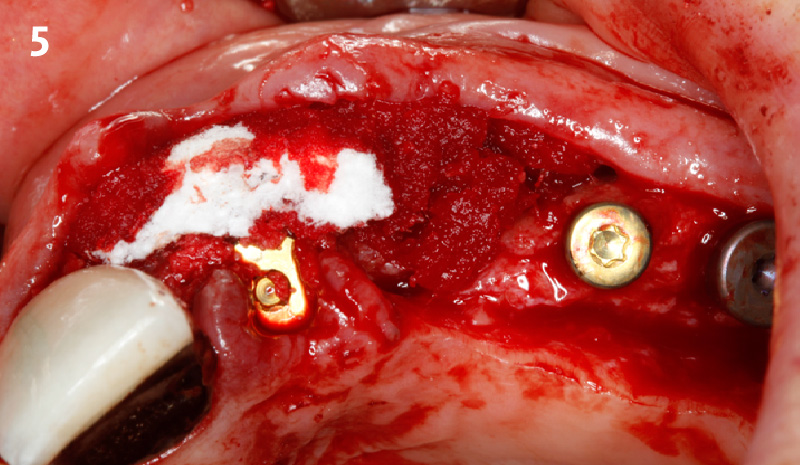
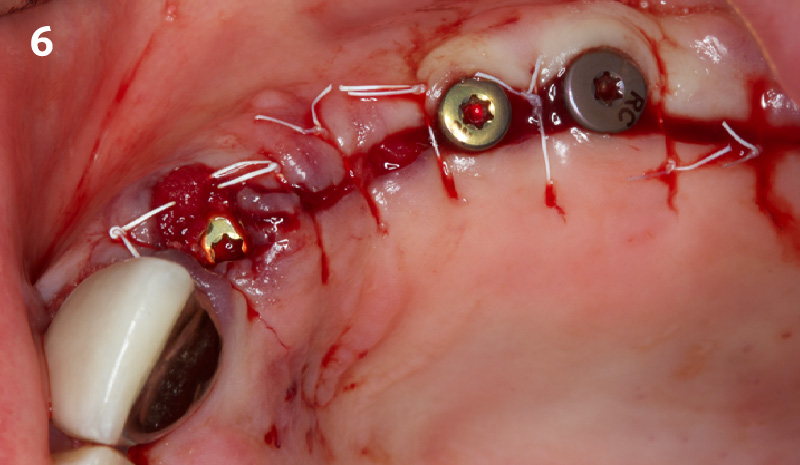
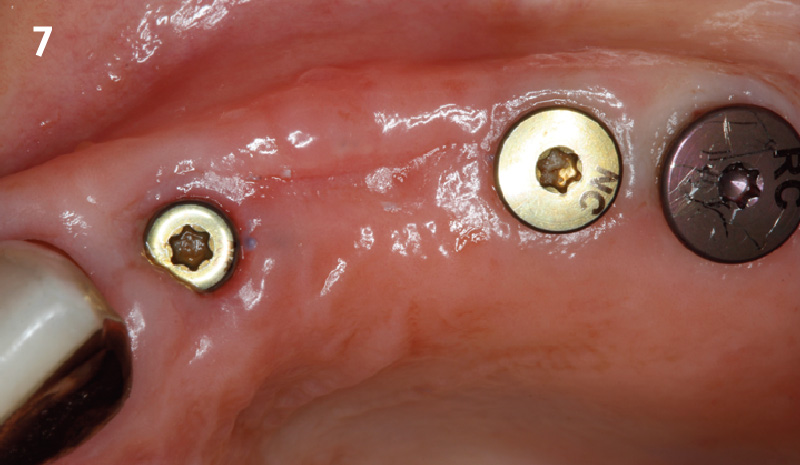
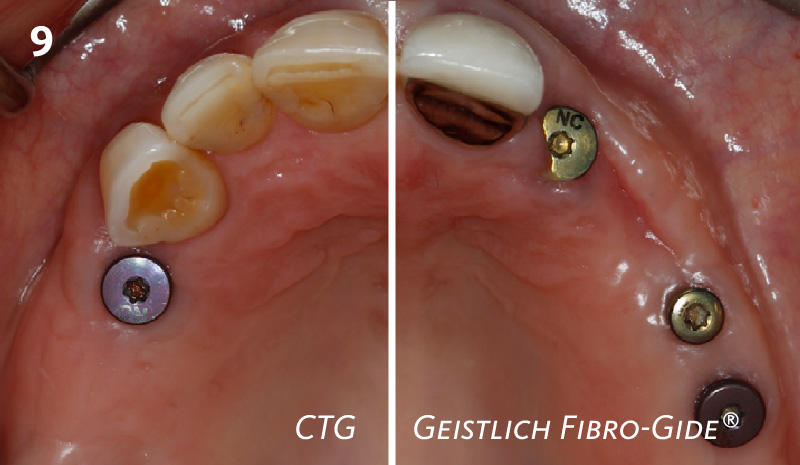
To carefully extract tooth #8 and to replace it with an early-stage implant placed with simultaneous guided bone regeneration through the use of Geistlich Bio-Oss Collagen® trimmed in an “L-Shape” under the protection of a Geistlich Bio-Gide® membrane. To augment the peri-implant soft-tissue with the use of a connective tissue graft during implant healing time, increasing the overall volume of site #8. To provisionalize the implant for the development of a proper emergence profile. To deliver a definitive reconstruction which is functional and esthetic for the patient.
“A fractured anterior tooth needs to be replaced with an implant-supported reconstruction.”
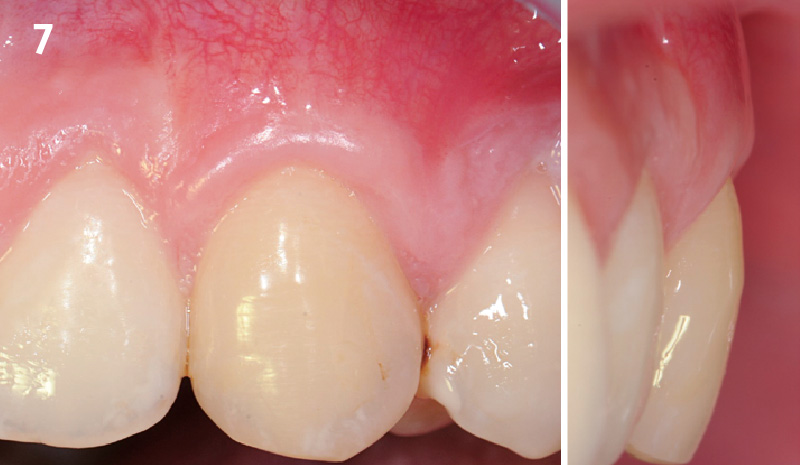
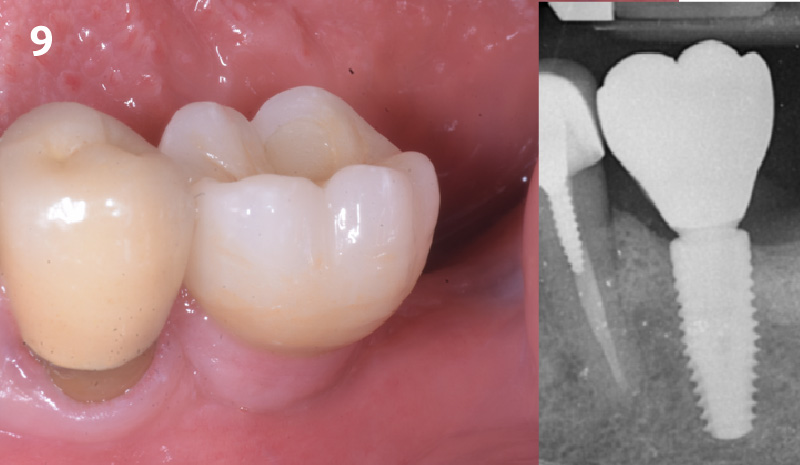
THE OUTCOME
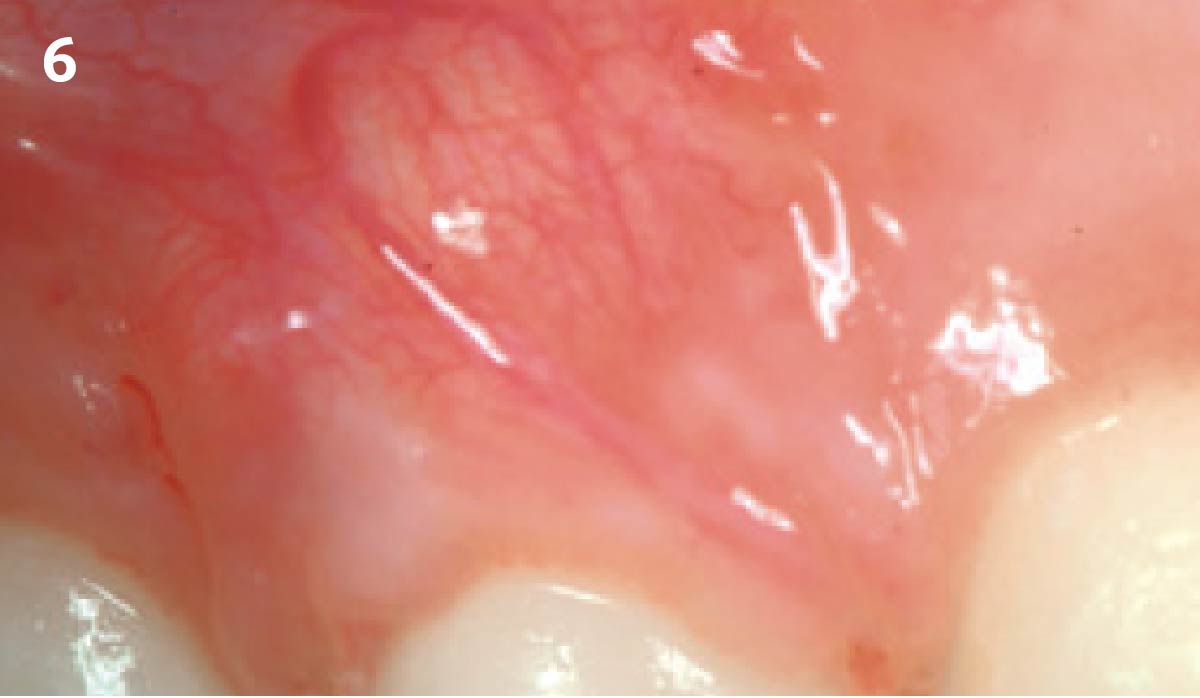
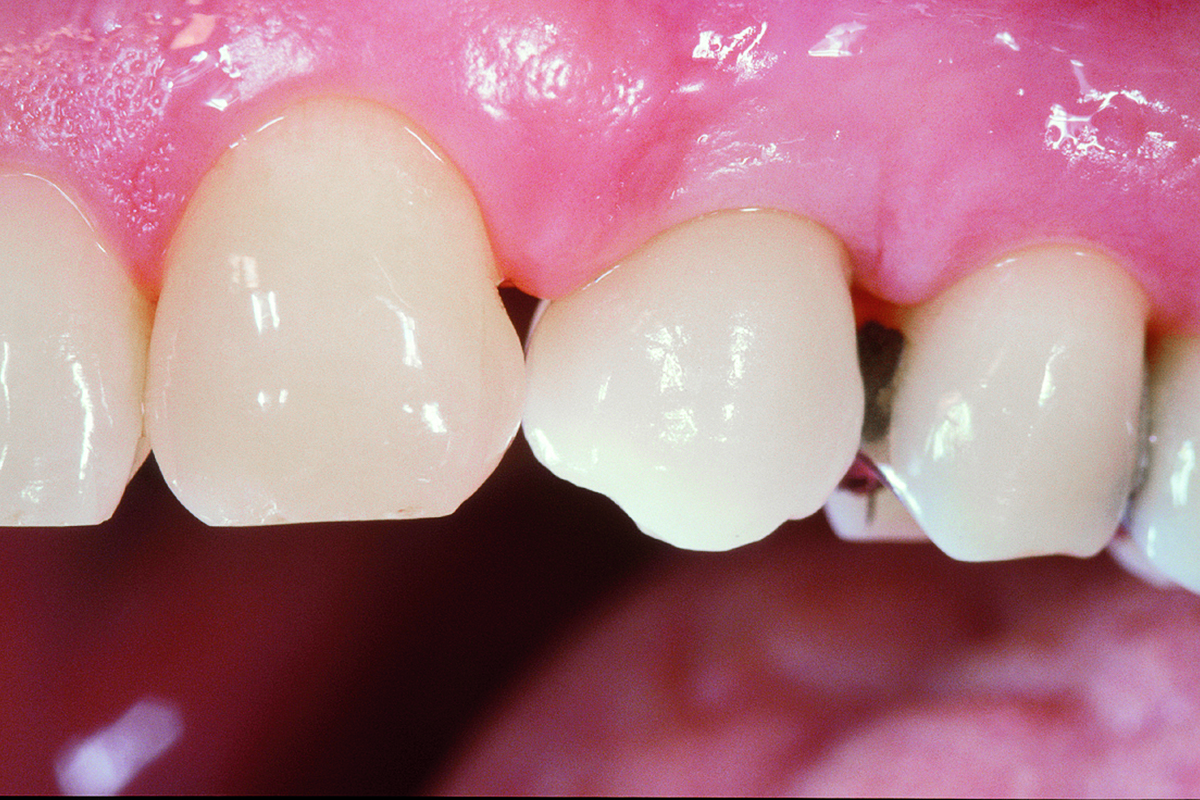
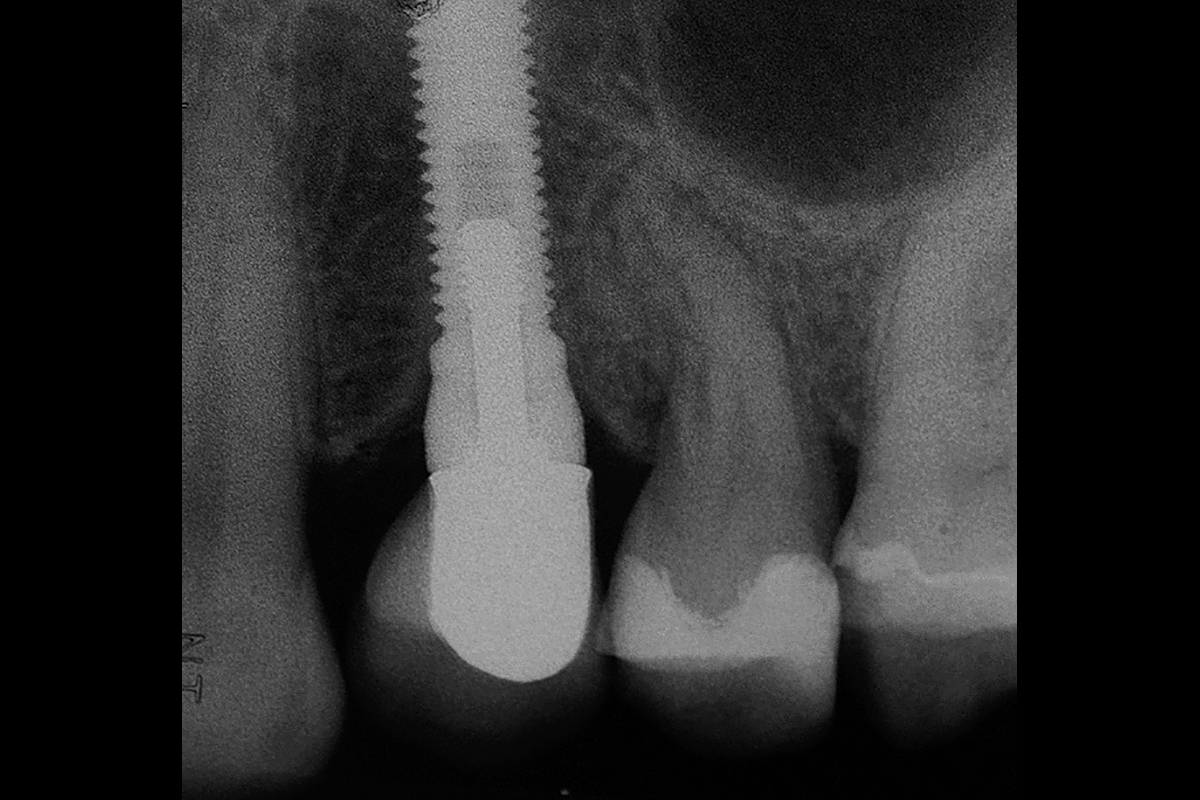
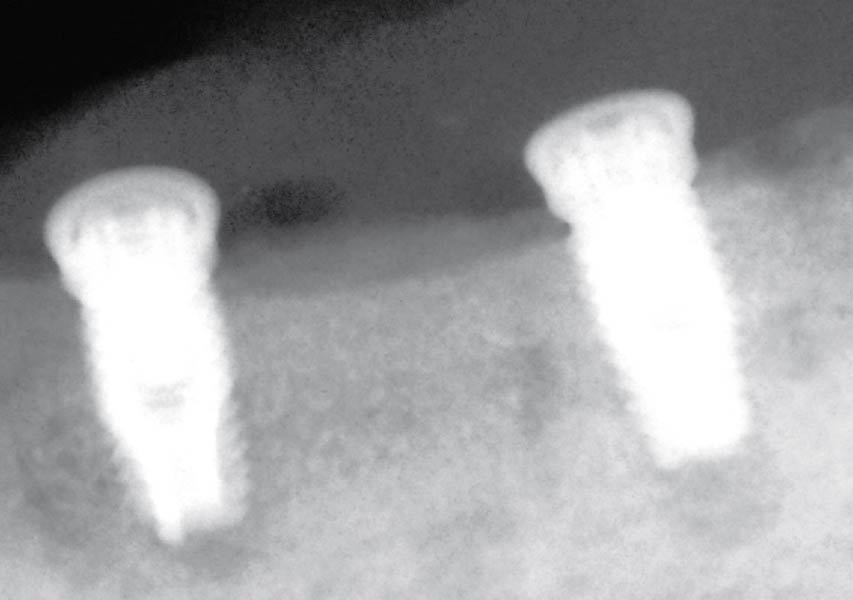
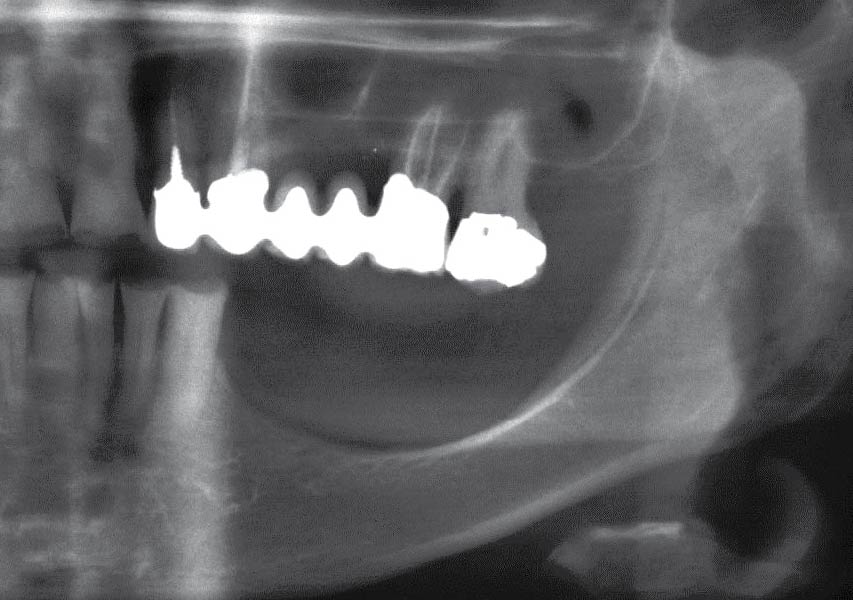
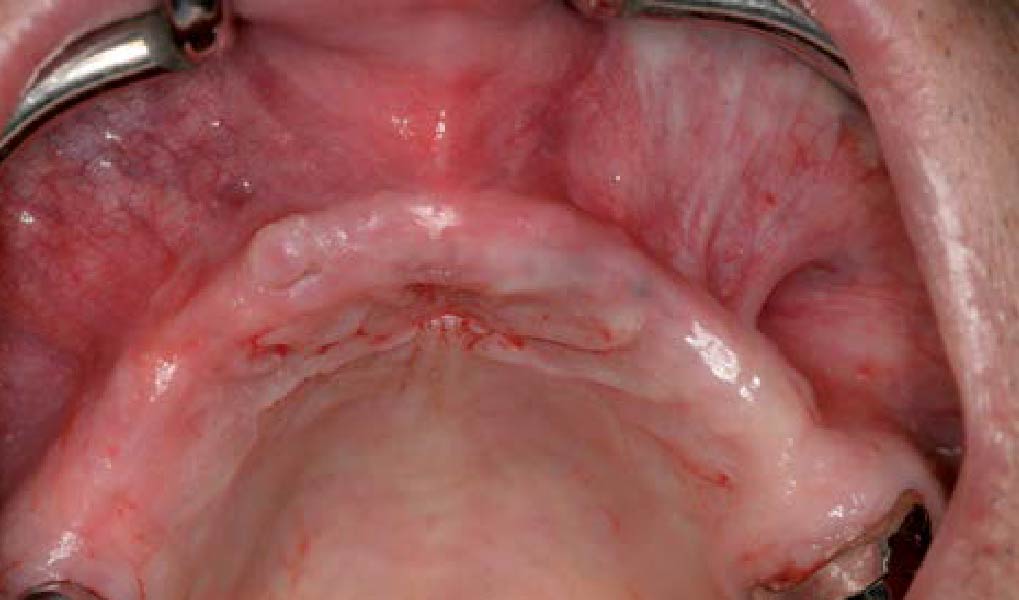
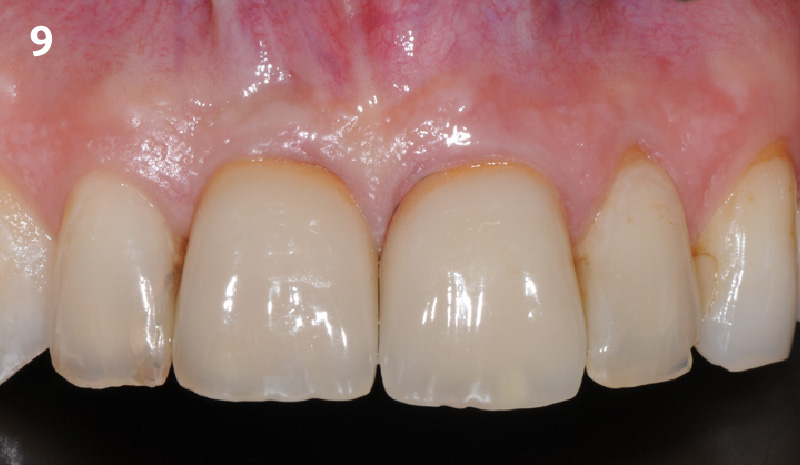
The implant and its prosthetic reconstruction were successful because they provided the patient with a fixed solution with adequate function and esthetics. The implant shows stable marginal bone levels due to the proper implant placement together with the guided bone regeneration procedure. The peri-implant soft-tissue is healthy and stable with sufficient volume created by the soft-tissue augmentation. The definitive reconstruction meets the patient’s esthetic demands and is functional in occlusion.


Prof. Dr. Ronald E. Jung
Prof. Dr. Jung is currently Head of the Division of Implantology, Clinic for Fixed and Removable Prosthodontics and Dental Material Science, Center of Dental Medicine at the University of Zürich. In 2006 he worked as Visiting Associate Professor at the Department of Periodontics at the University of Texas Heath Science center at San Antonio, USA (Chairman: Prof. D. Cochran). In 2008 he finalized his “Habilitation” (venia legendi) in dental medicine and was appointed associate professor at the University of Zürich. In 2011 he received his PhD degree from the University of Amsterdam, ACTA dental school, The Netherlands. He is an accomplished and internationally renowned lecturer and researcher, best known for his work in the field of hard- and soft-tissue management and his research on new technologies in implant dentistry.