CLINICAL CASE
THE APPROACH
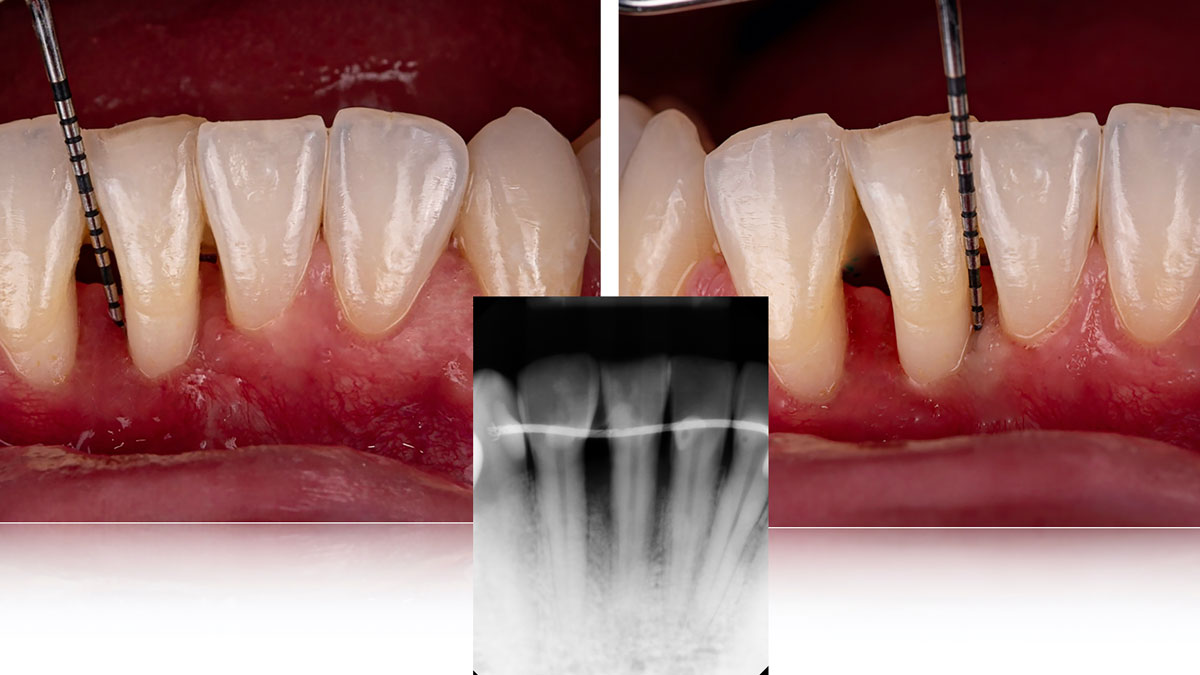
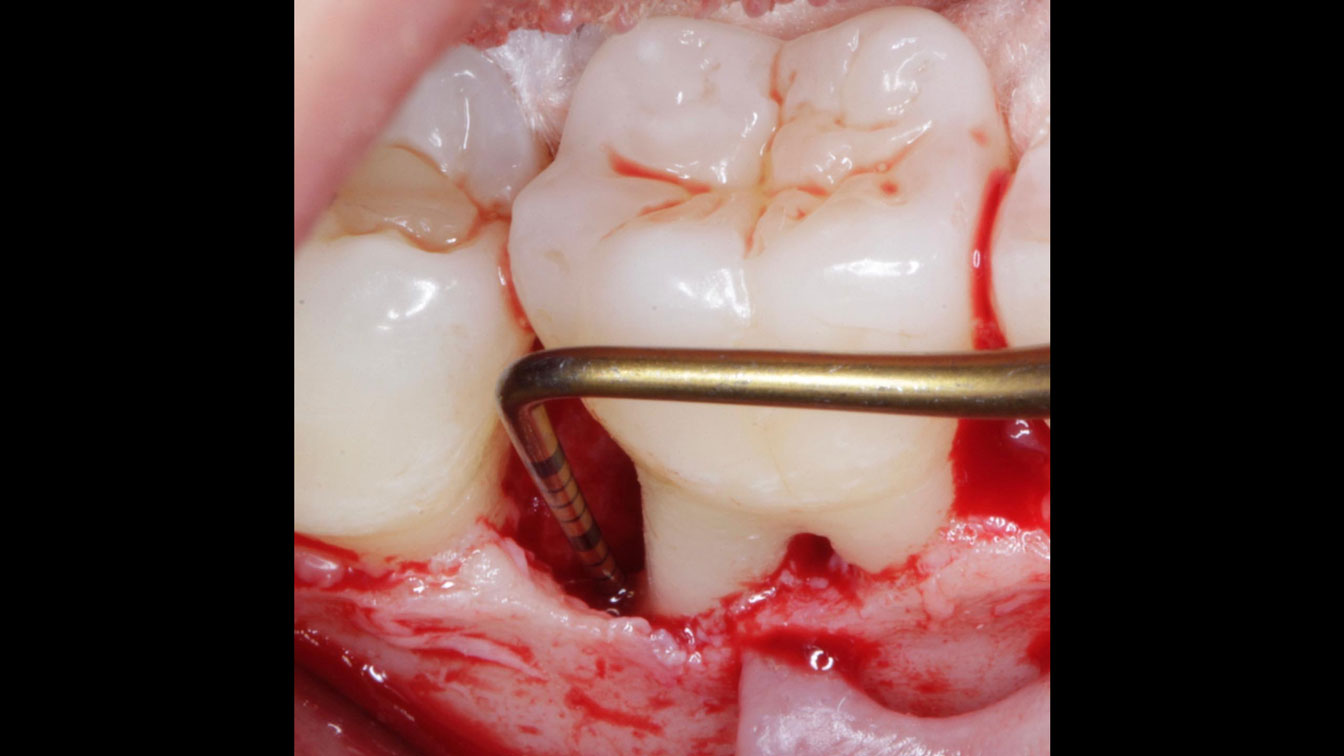
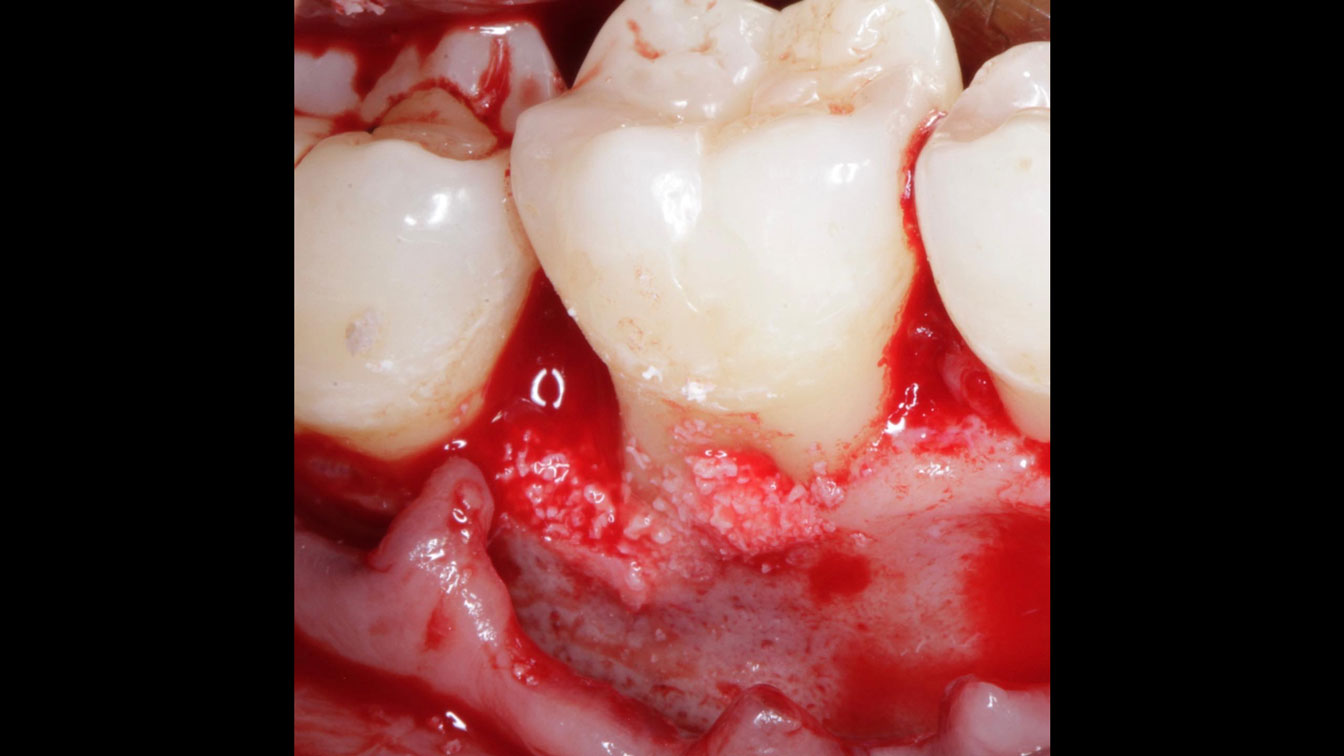
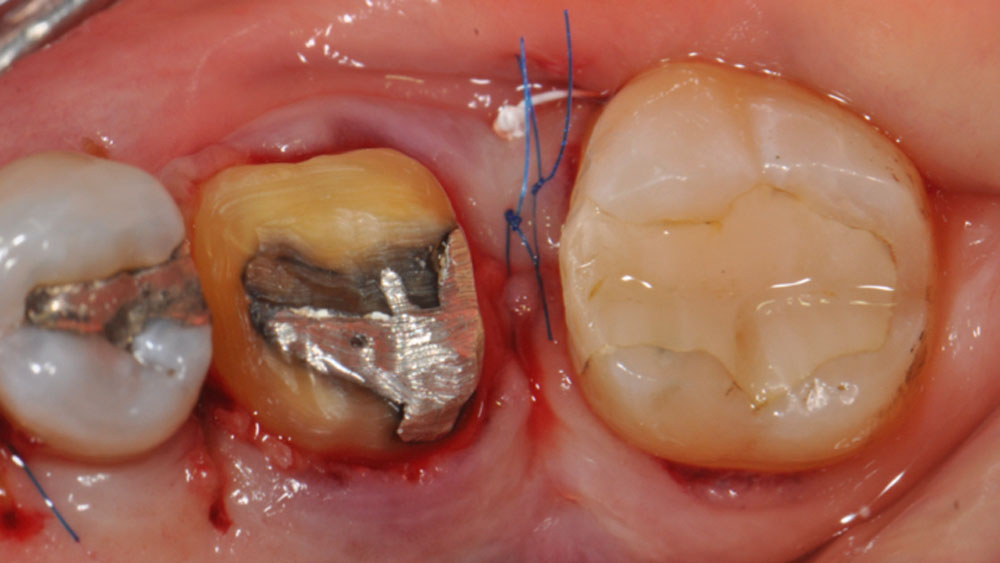
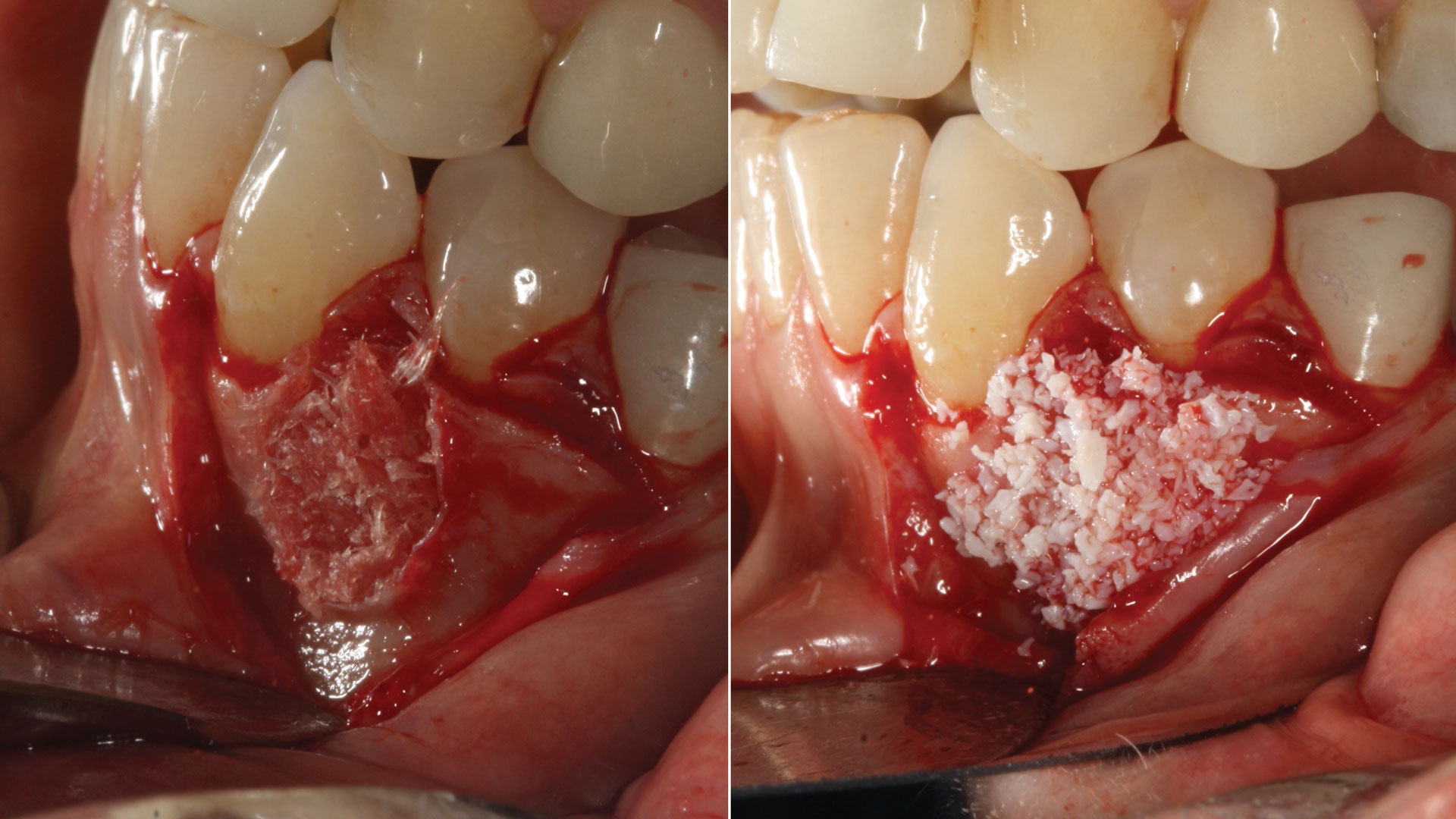
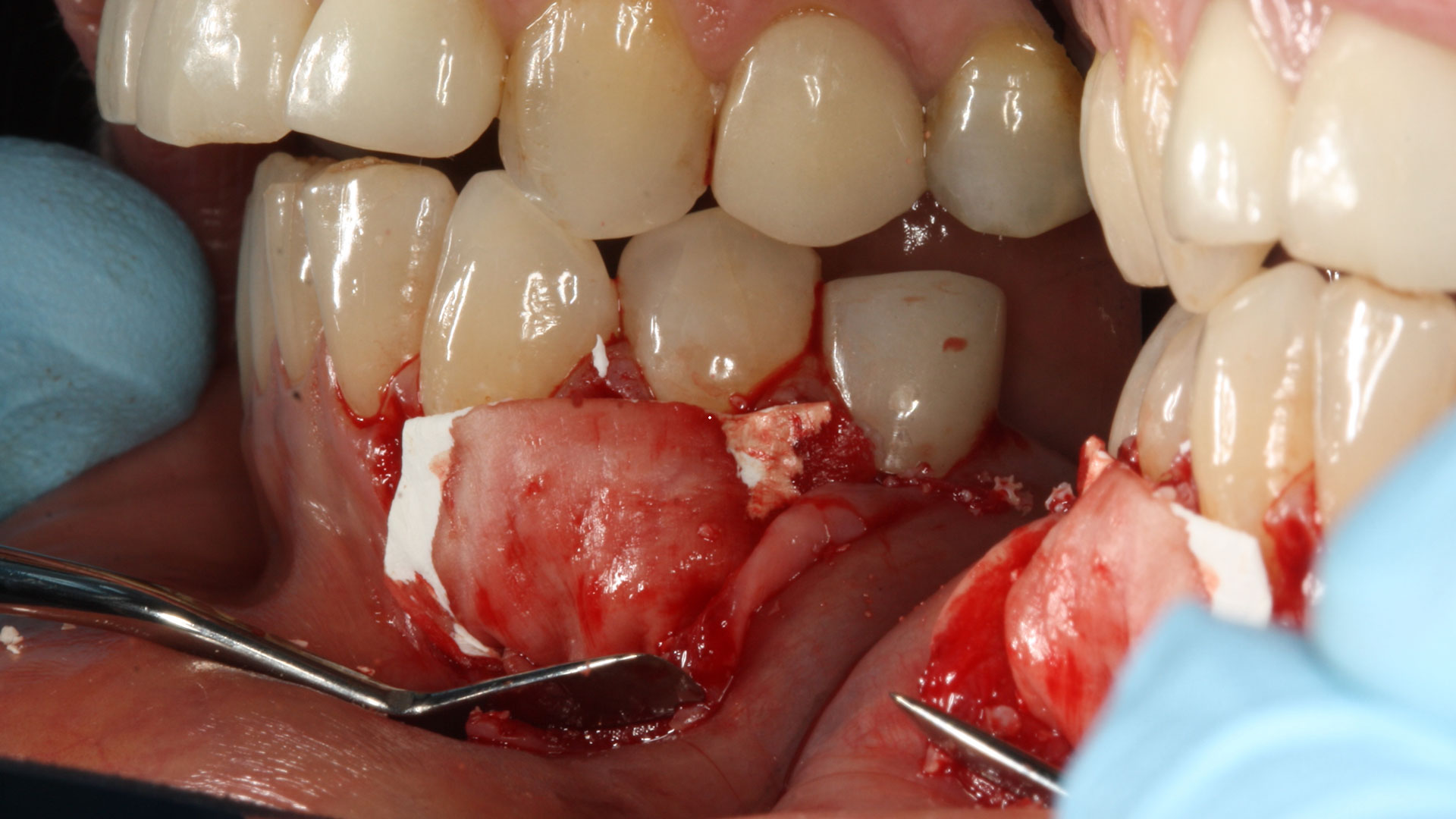
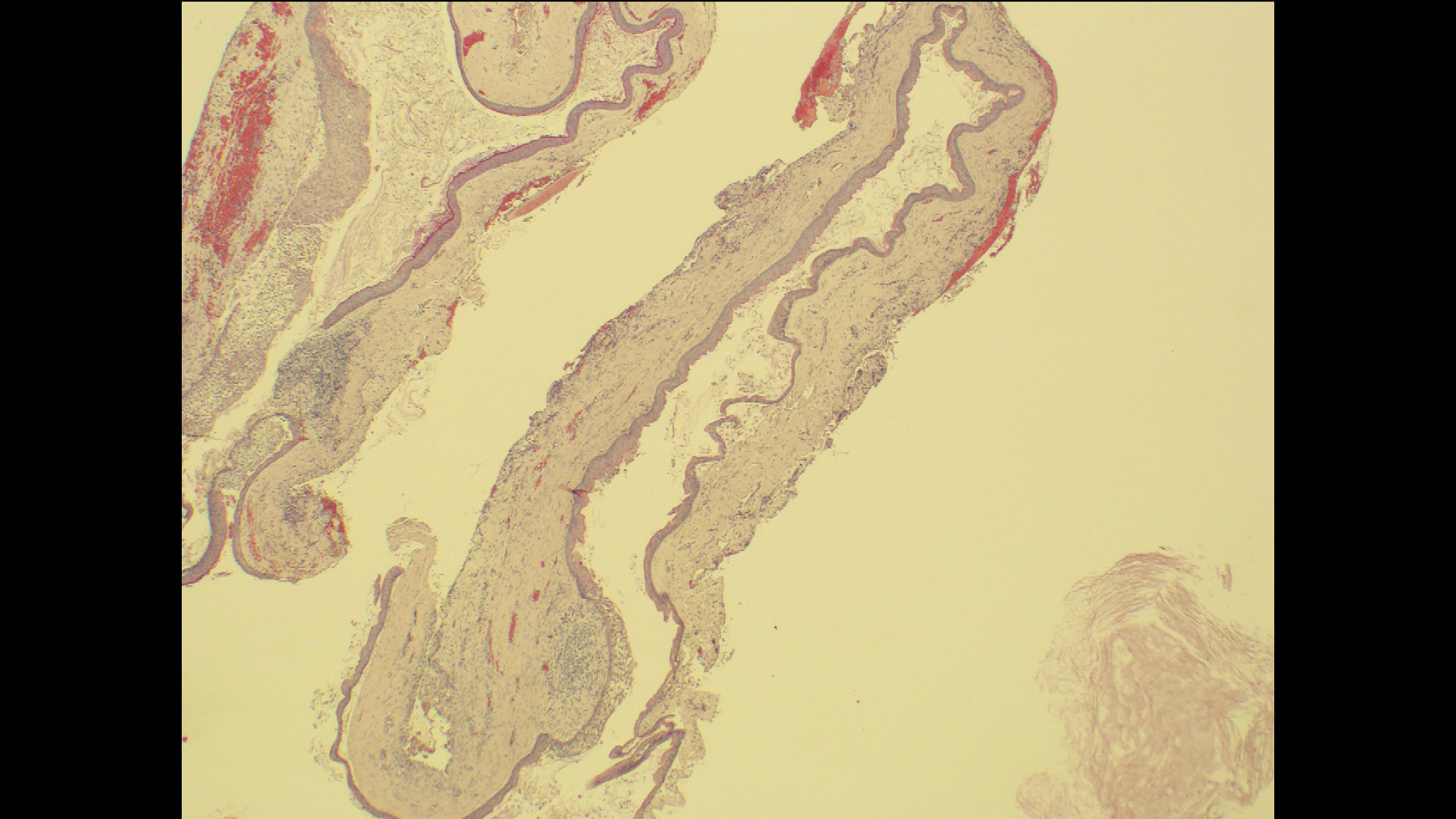
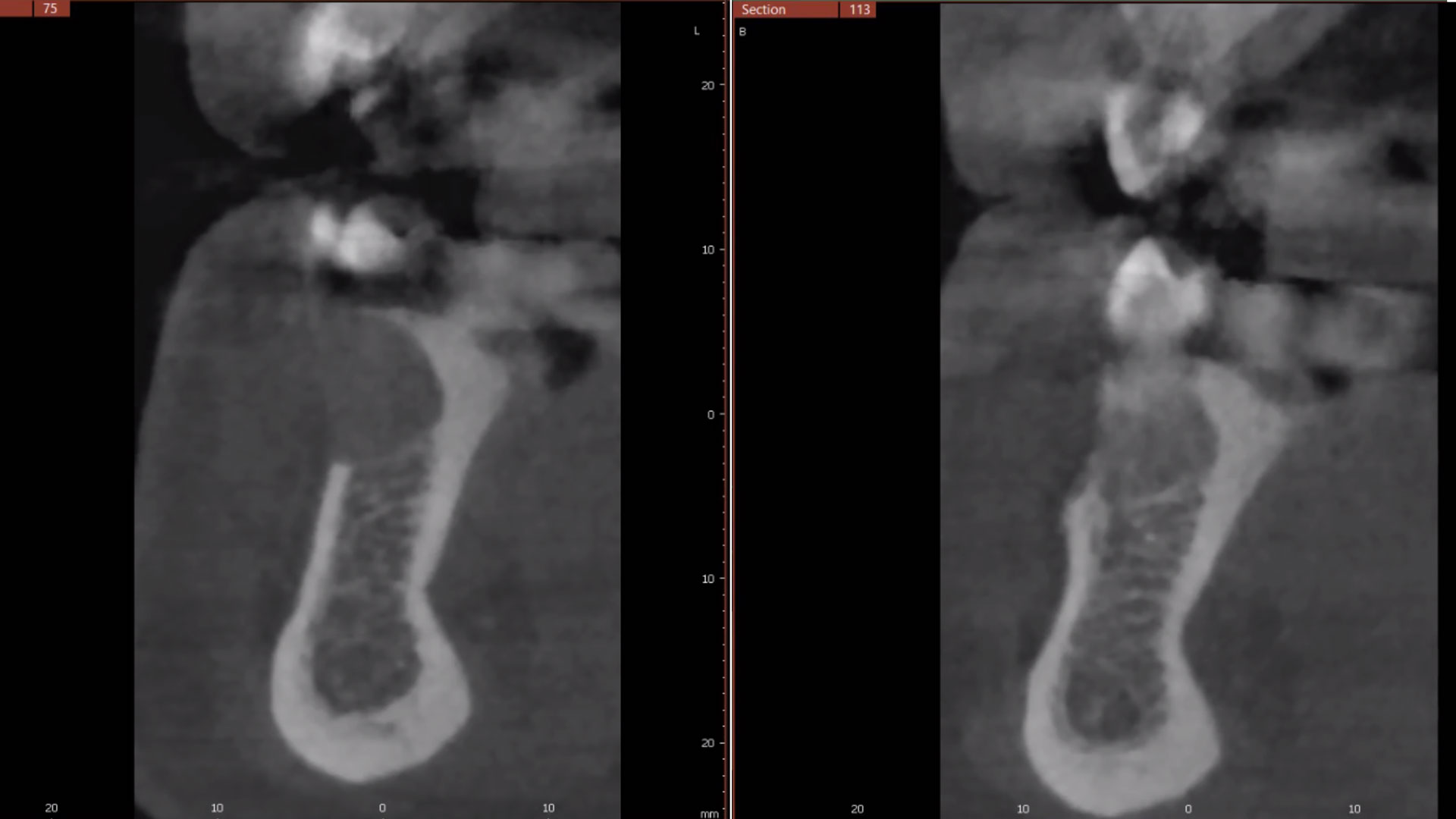
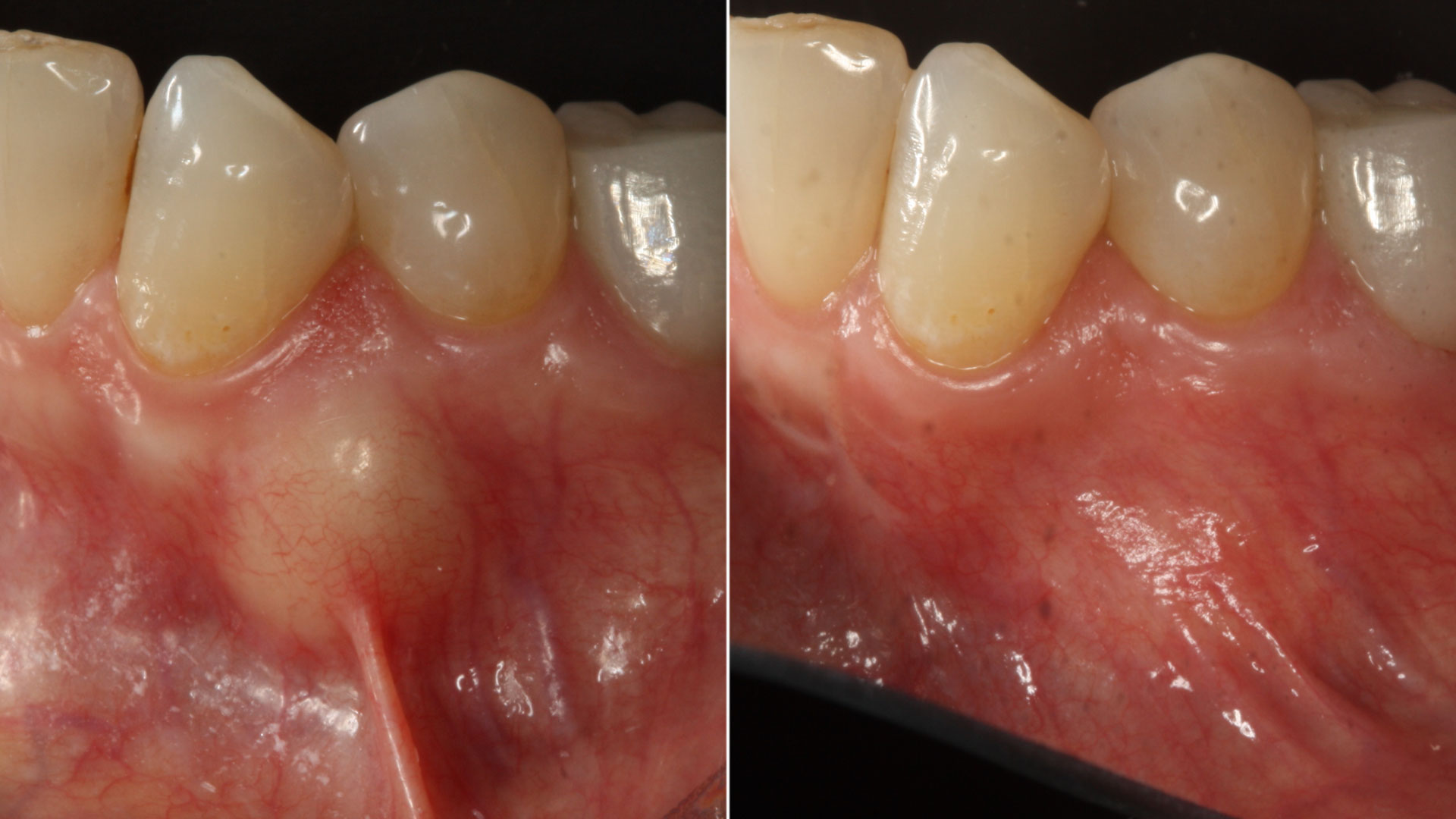
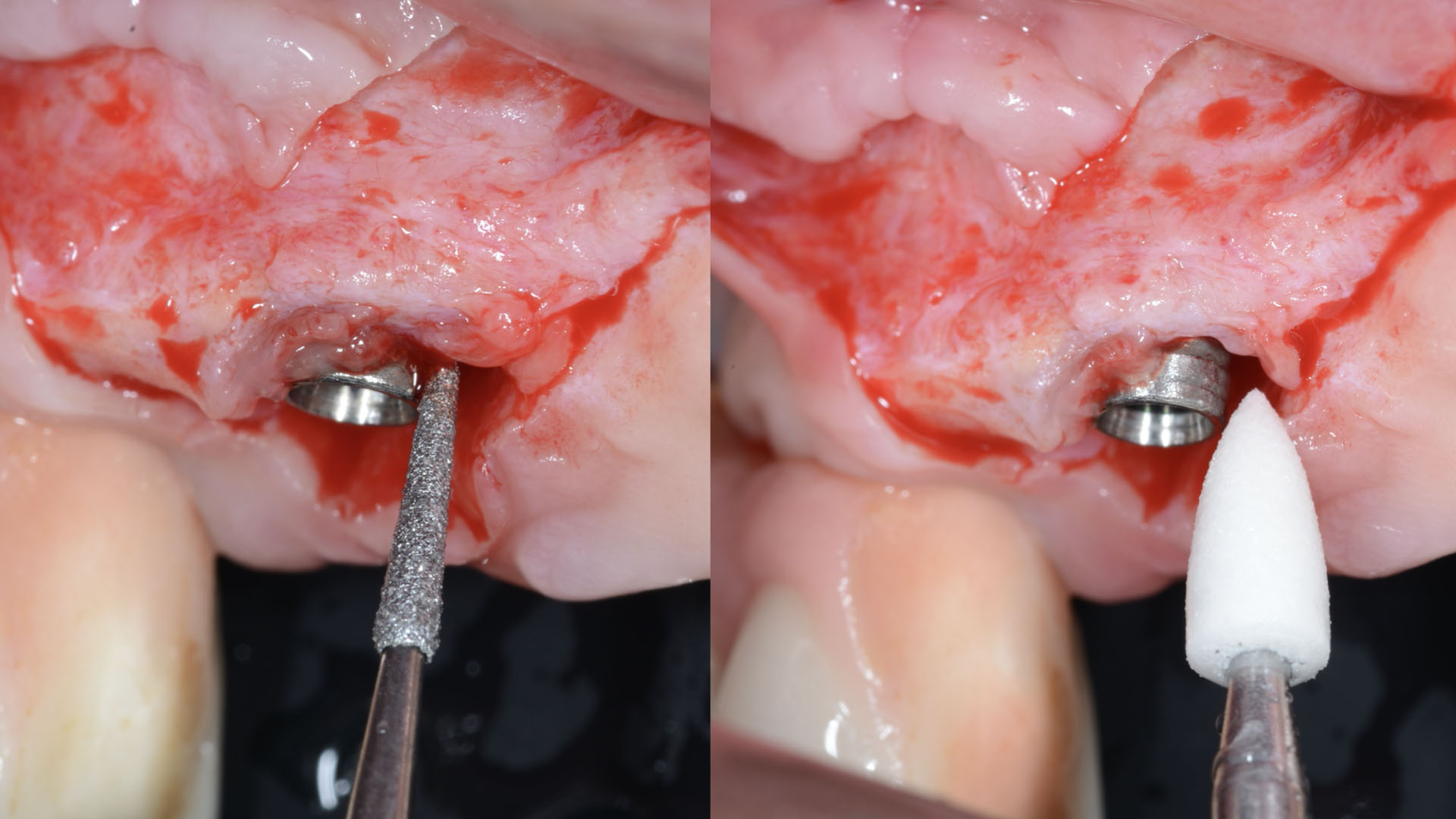
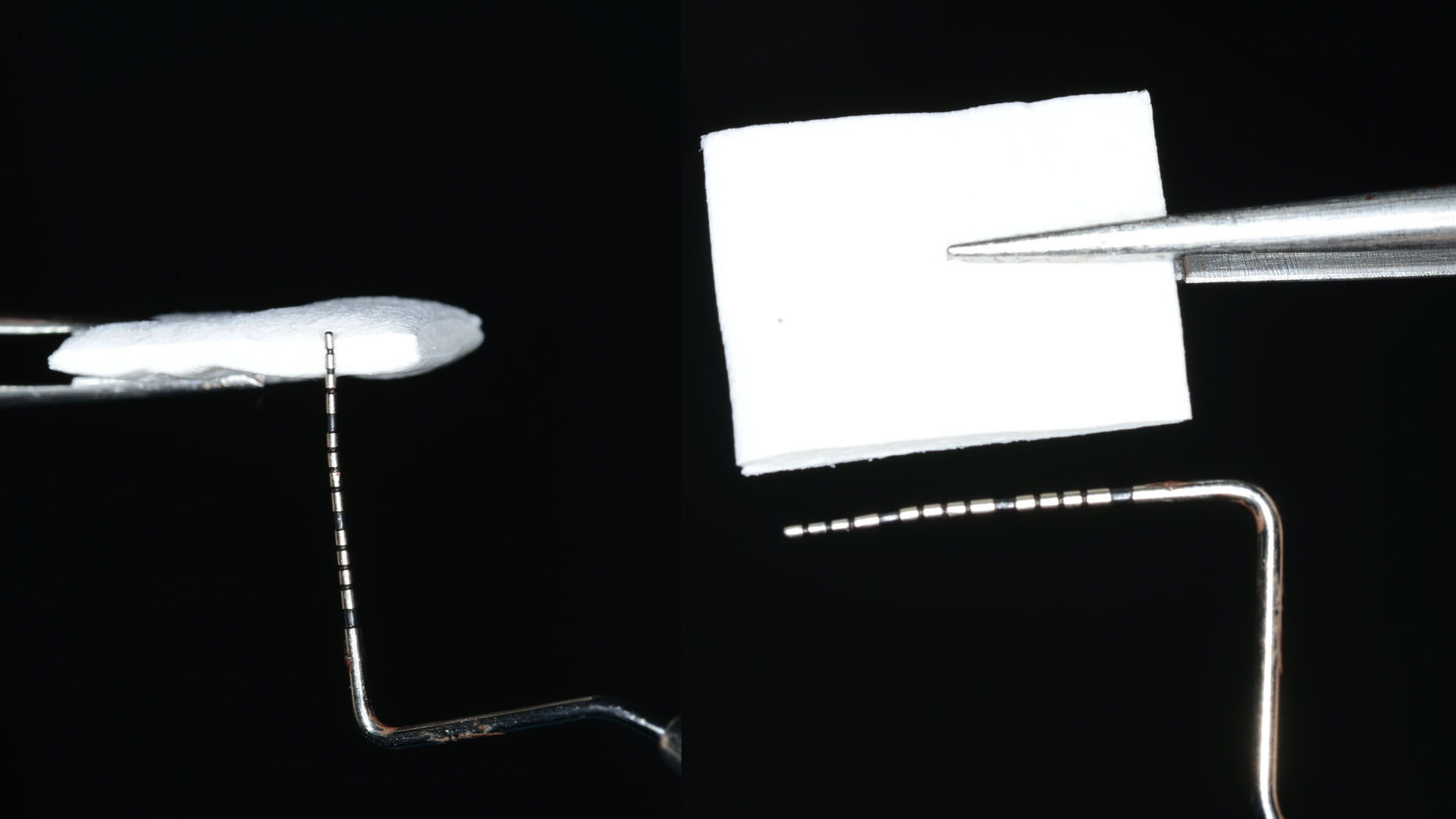
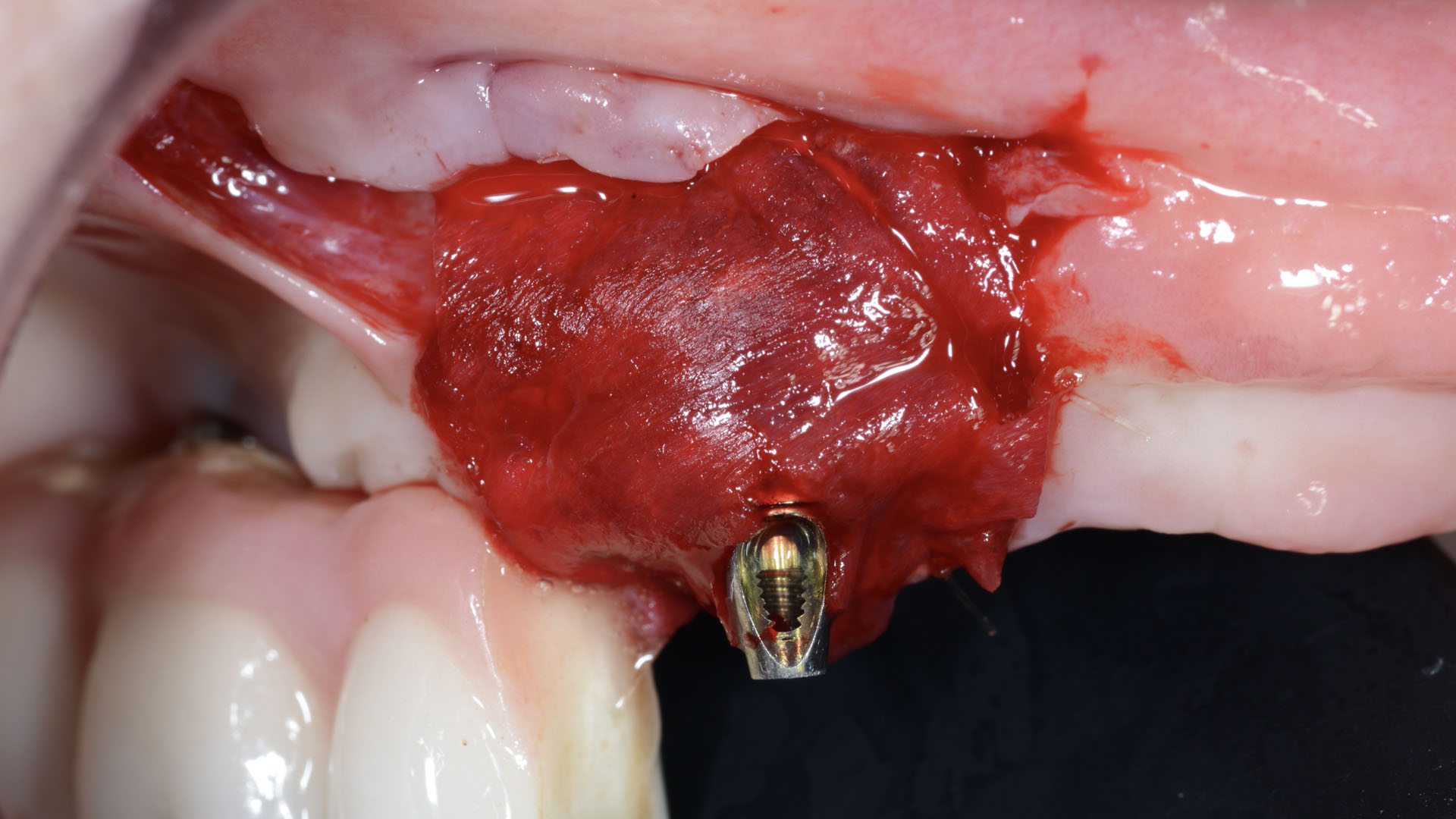
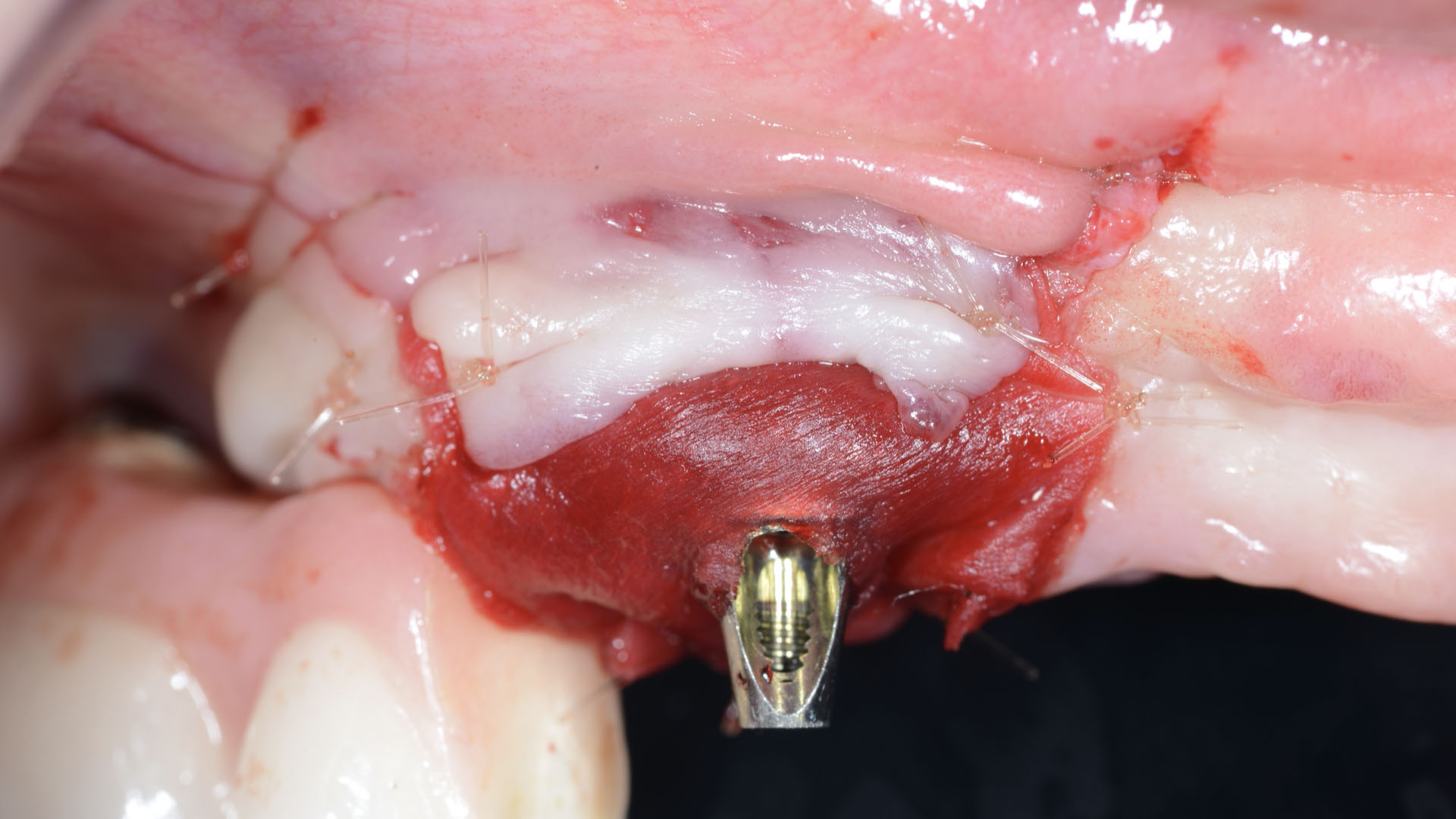
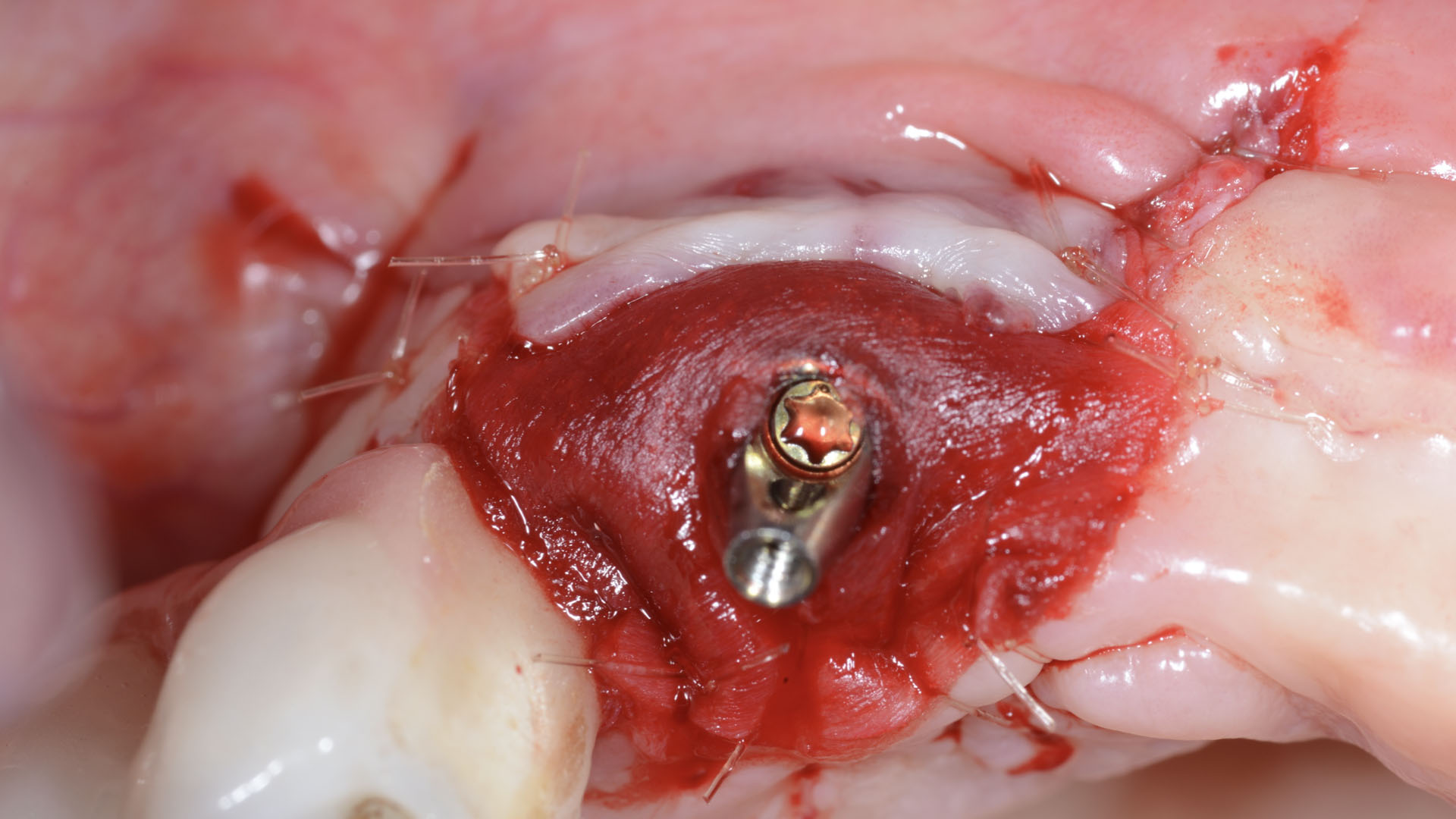
Considering the patient’s age, condition, and good compliance, a regenerative approach was chosen to preserve all teeth. Due to the extent and severity of the defect, a bone graft, biologics, and a membrane were utilized. The goal was to restore lost attachment and stabilize the teeth through splinted therapy.
THE OUTCOME
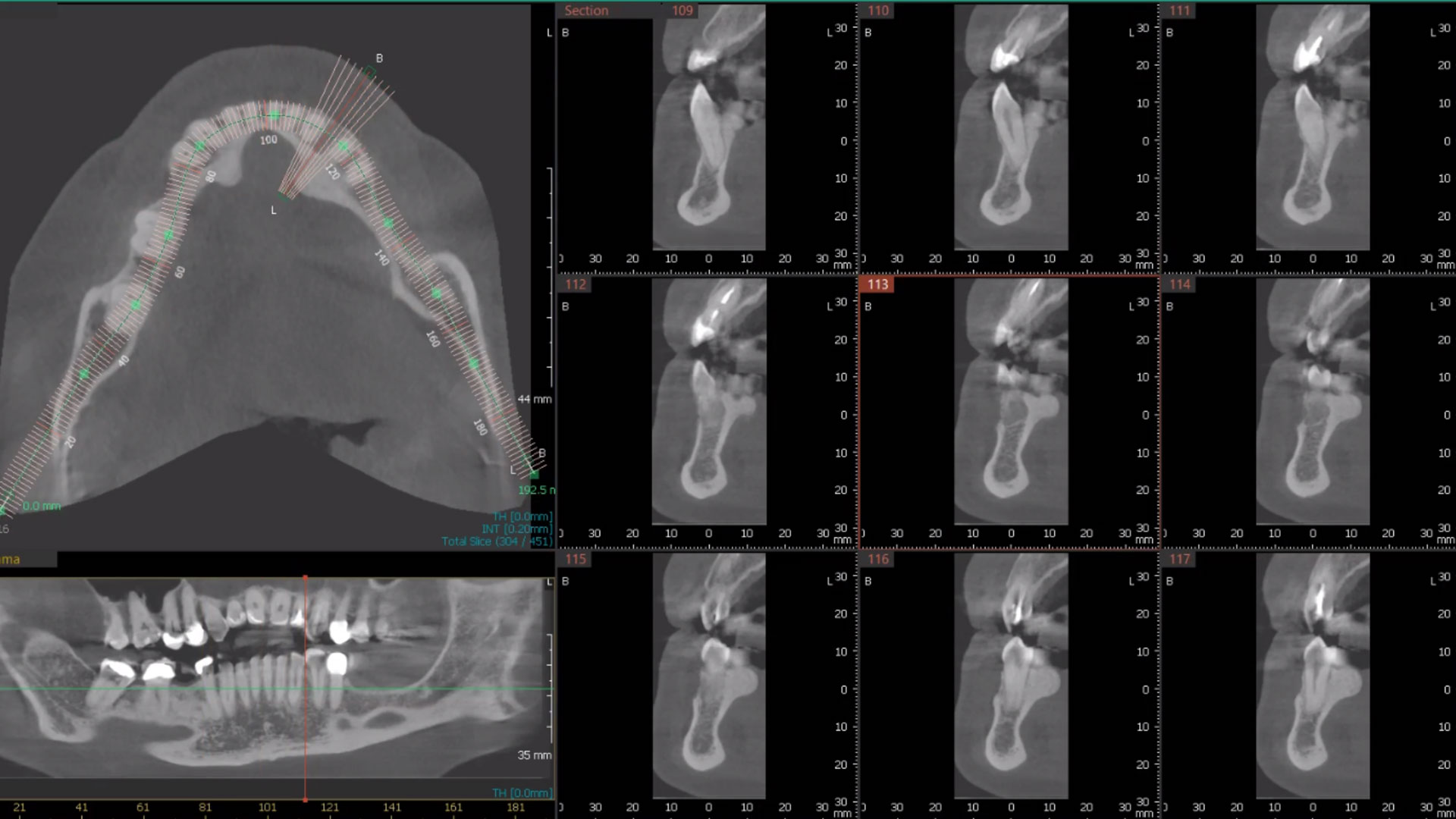
At the 7-month follow-up, probing depths decreased from 7 mm (MB, DB) to 3 mm, with radiographic bone fill indicating a 90% success. Attachment gain of 3 mm was achieved, improving from 7 mm to 4 mm. The patient reported satisfactory outcomes, and splinting effectively maintained tooth stability with no mobility.
Disclaimer: These results are not guaranteed; individual outcomes may vary depending on patient circumstances. This information is for informational purposes only and may not reflect Geistlich’s official position, opinion, or recommendation. Treatment decisions are made at the physician’s discretion, based on the unique needs of each patient.