BIOBRIEF
Lateral Ridge Augmentation in the Posterior Mandible

THE SITUATION
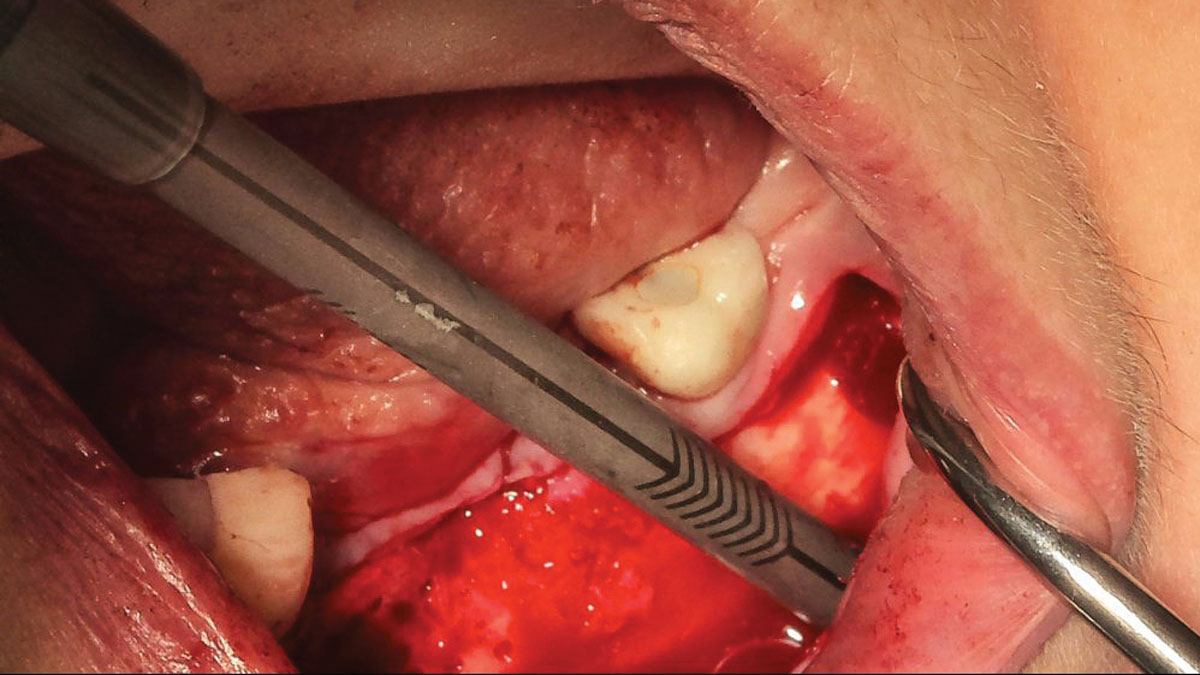
A 70-year-old female in good health presented with a fracture of tooth #19 which is the distal abutment for a four-unit bridge tooth #19-22, with pontics in the #20 and #21 positions. With the loss of the bridge, the patient desired a fixed prosthetic replacement. A bridge from tooth #22 to an implant placed at the #18 position was not deemed mechanically sound. She opted for implant placement at positions #19, #20 and #21 following lateral ridge augmentation with autogenous bone and Geistlich Bio-Oss® contained with a Geistlich Bio-Gide® membrane.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Compromised | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
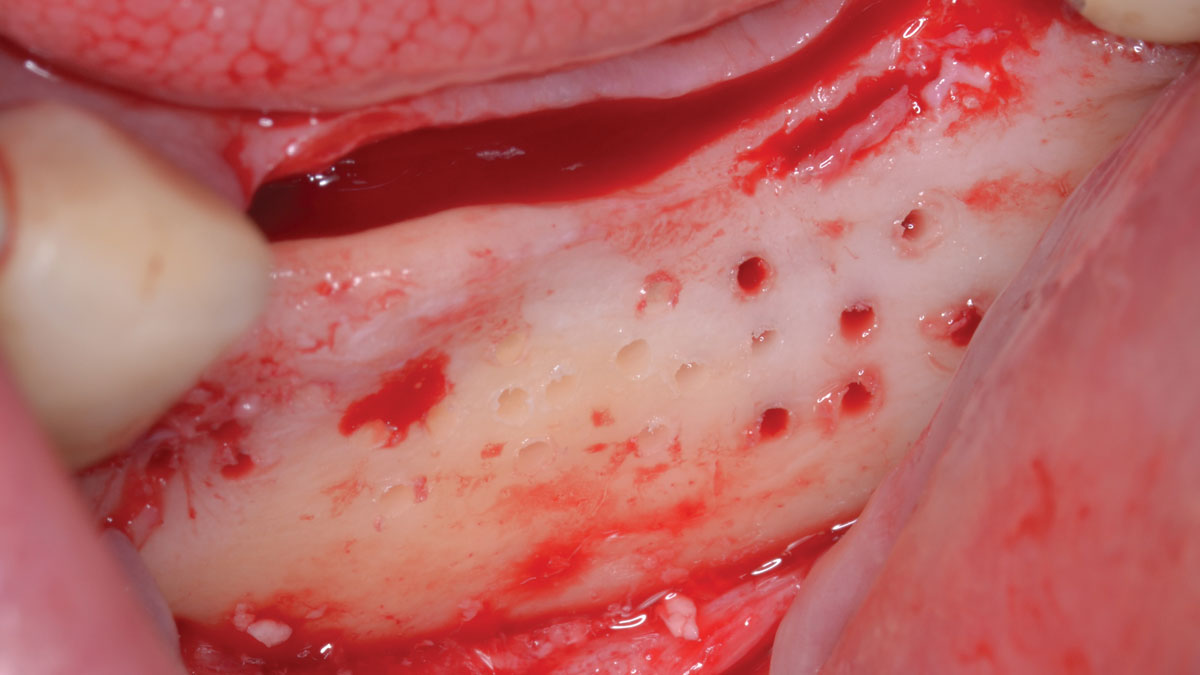
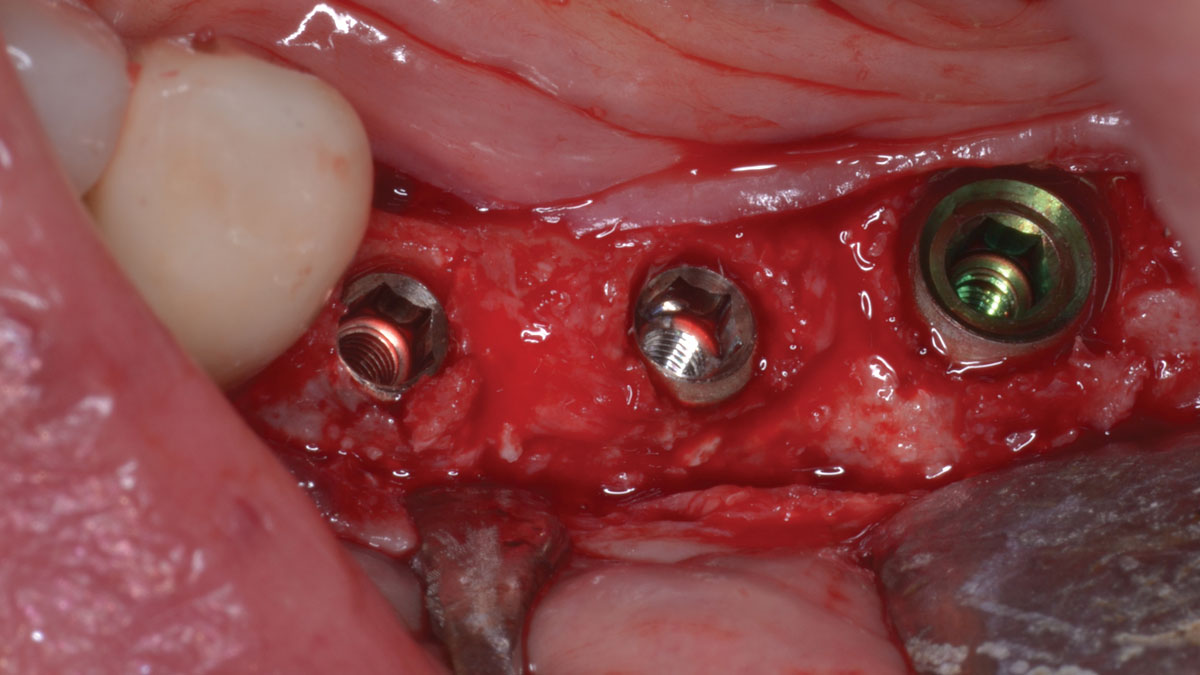
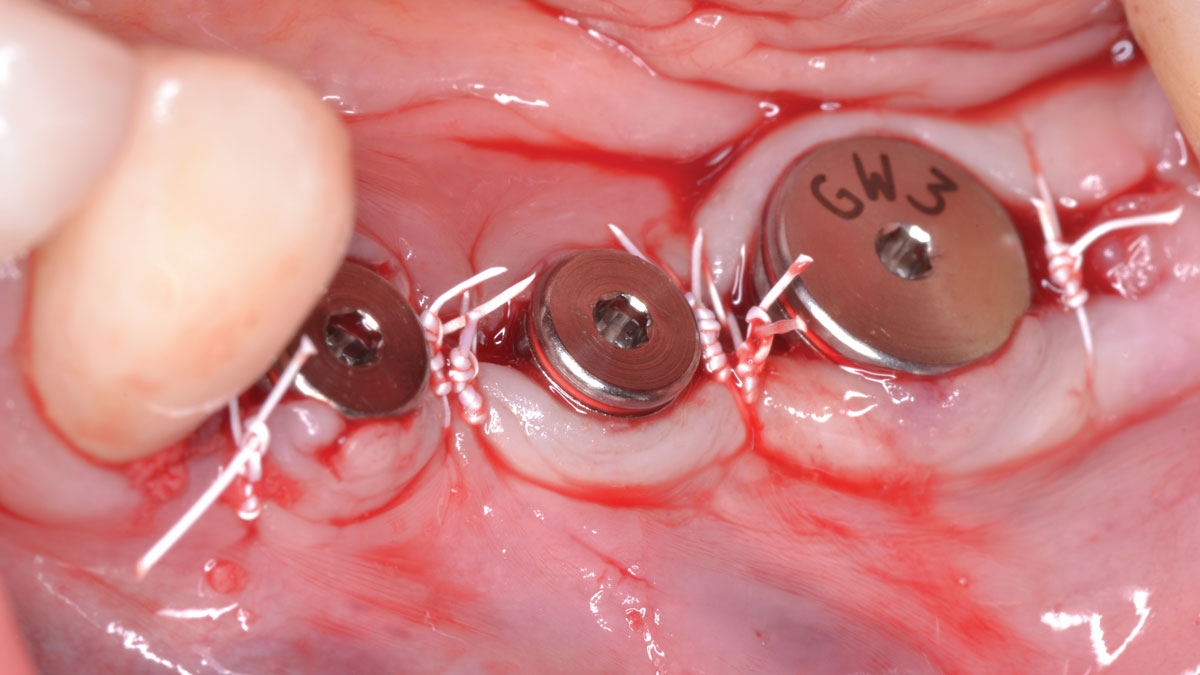
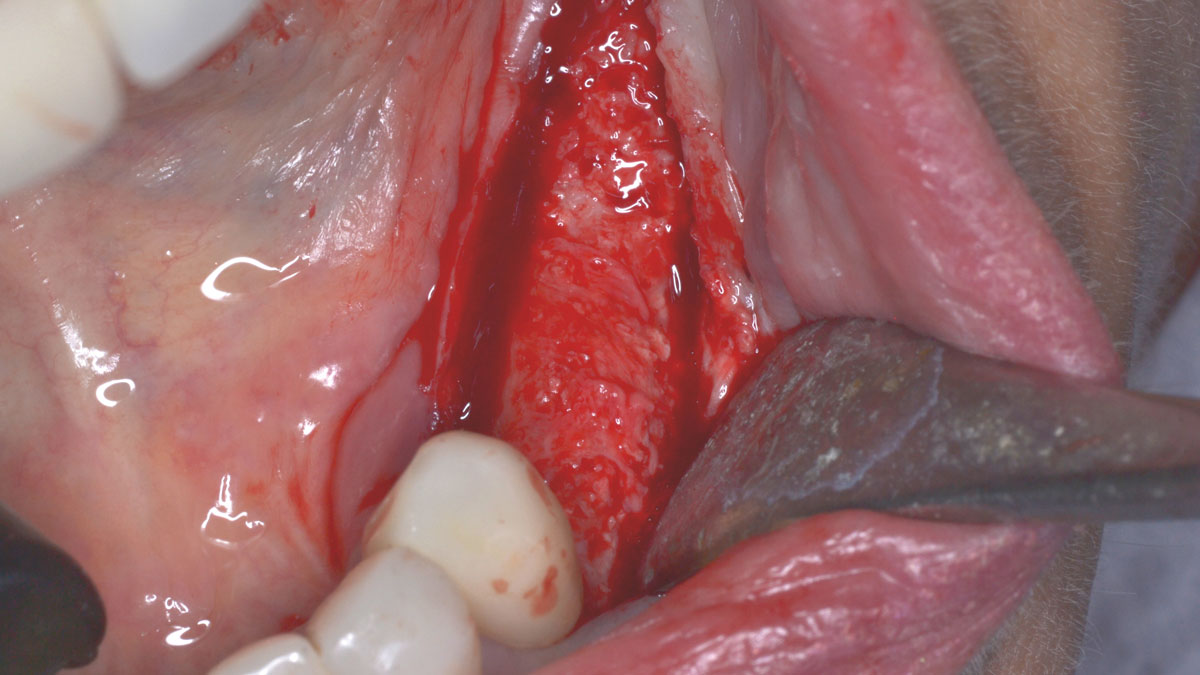
A subperiosteal flap with a mid-ridge incision was performed with anterior and posterior releasing incisions which were placed the distance of one tooth mesial and one tooth distal from the graft site. The posterior releasing incision allowed for exposure of the ramus for harvesting of the autologous bone. The grafted site was allowed to heal for a period of 8 months at which time the implants were placed. Abutment connection occurred 4 months following implant placement.
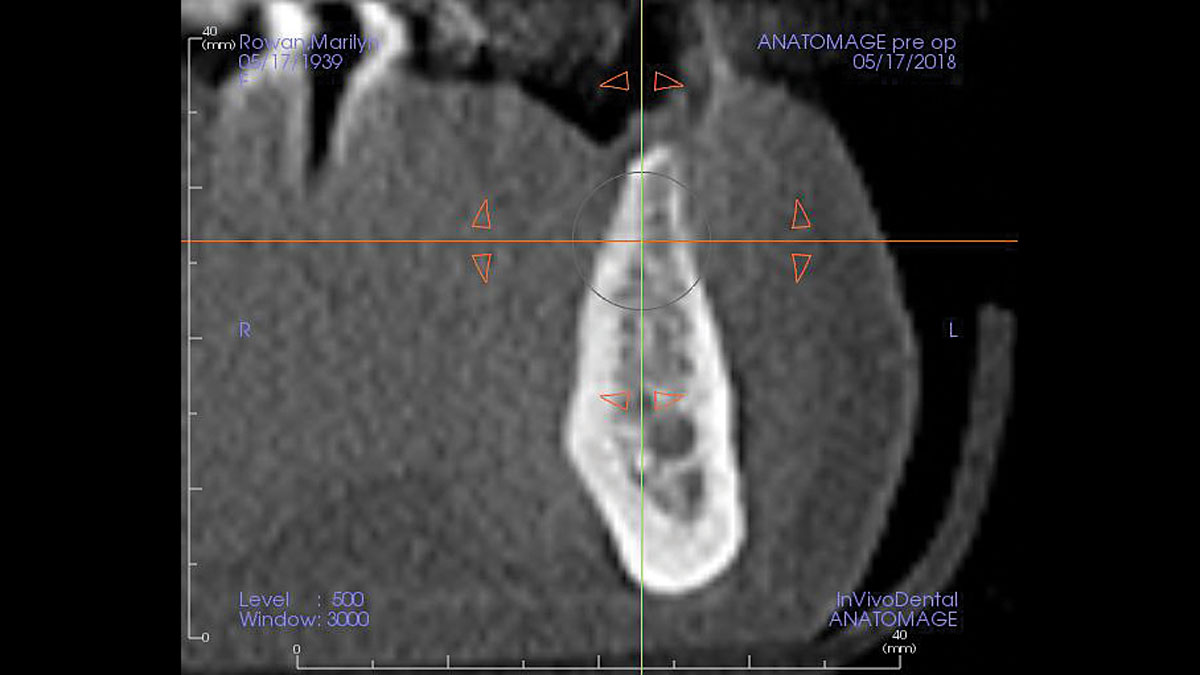
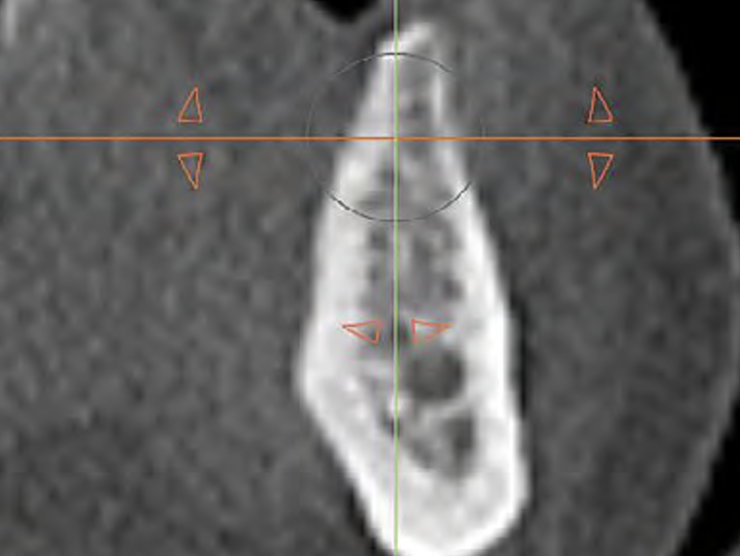
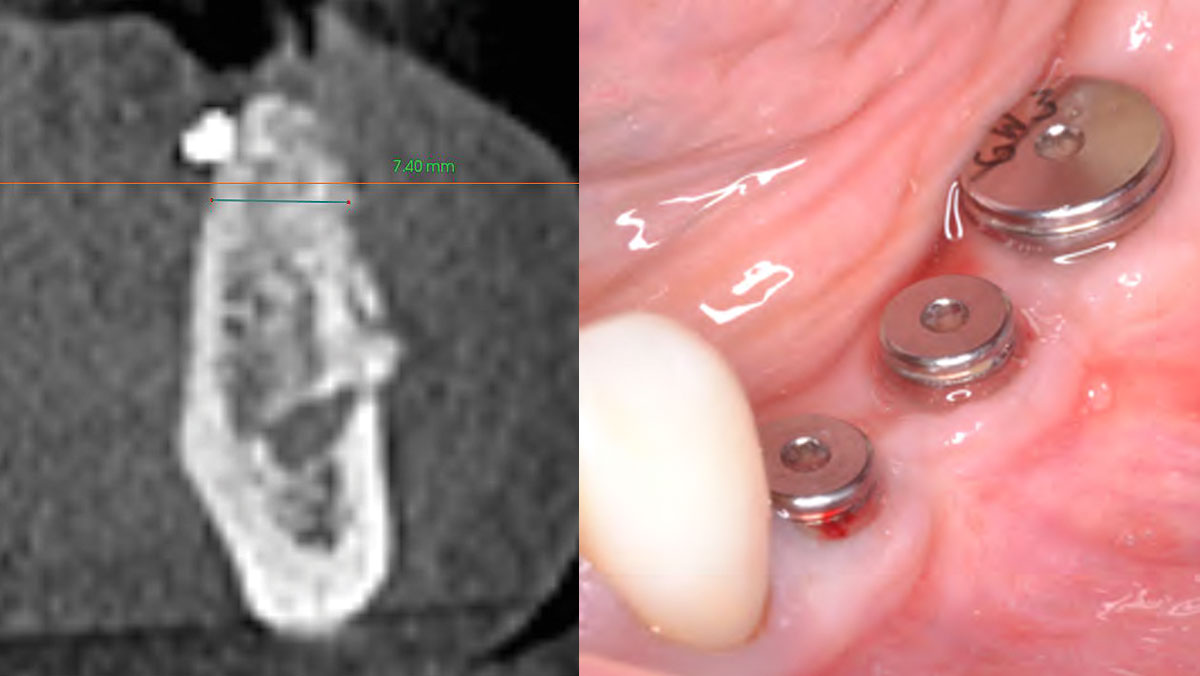
“A bone graft was required to augment the ridge, a CBCT scan was performed prior to surgery to determine bone volume and the amount of bone required to graft.”
THE OUTCOME
Following 8 months of healing, the augmented site showed sufficient bone width that was assessed with a CT scan. After examination, it was determined that the bone width was adequate for implant placement in the desired position to allow an esthetically pleasing and functional outcome for the patient.

Dr. John M. Sisto
Dr. John M. Sisto received his Doctorate in Dental Surgery degree from Loyola University and completed his residency and certification in Oral and Maxilofacial Surgery at the Cook County Hospital in Chicago. Dr. Sisto was the Director of Residency Education at Cook County Hospital from 1985 to 2010 and started the residency program in oral and maxillofacial surgery in 1990. He held teaching positions at both Northwestern and University of Illinois Dental schools as a clinical assistant professor, and also at Northwestern Medical School. He was the Division Chief of Oral and Maxillofacial Surgery at Cook County Hospital and Chairman of Dentistry at Resurrection Medical Center. Dr. Sisto has published papers on dental implant surgery, trauma surgery, orthognathic surgery and maxillofacial infections. He has lectured both locally and nationally at various educational forums.