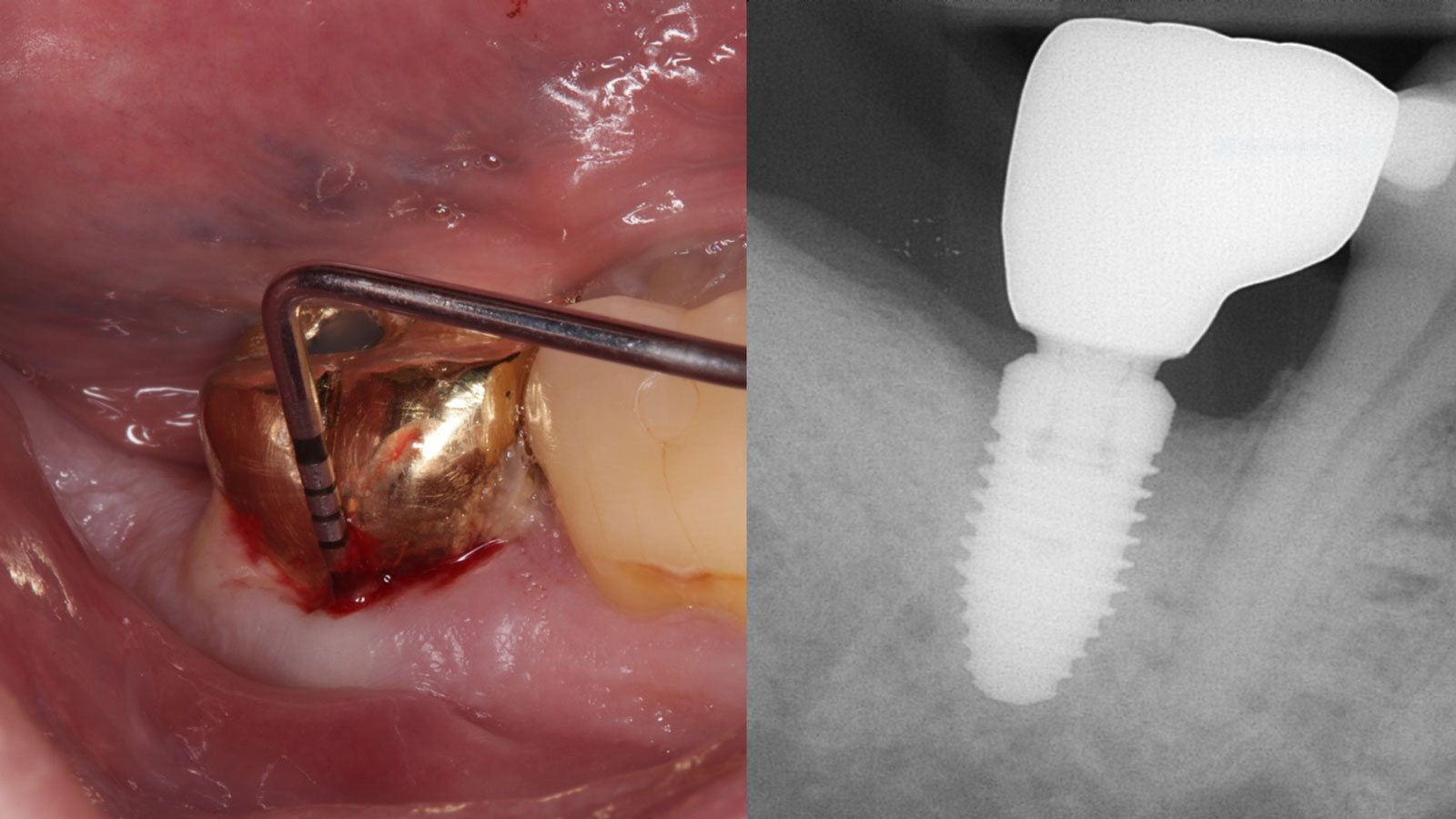
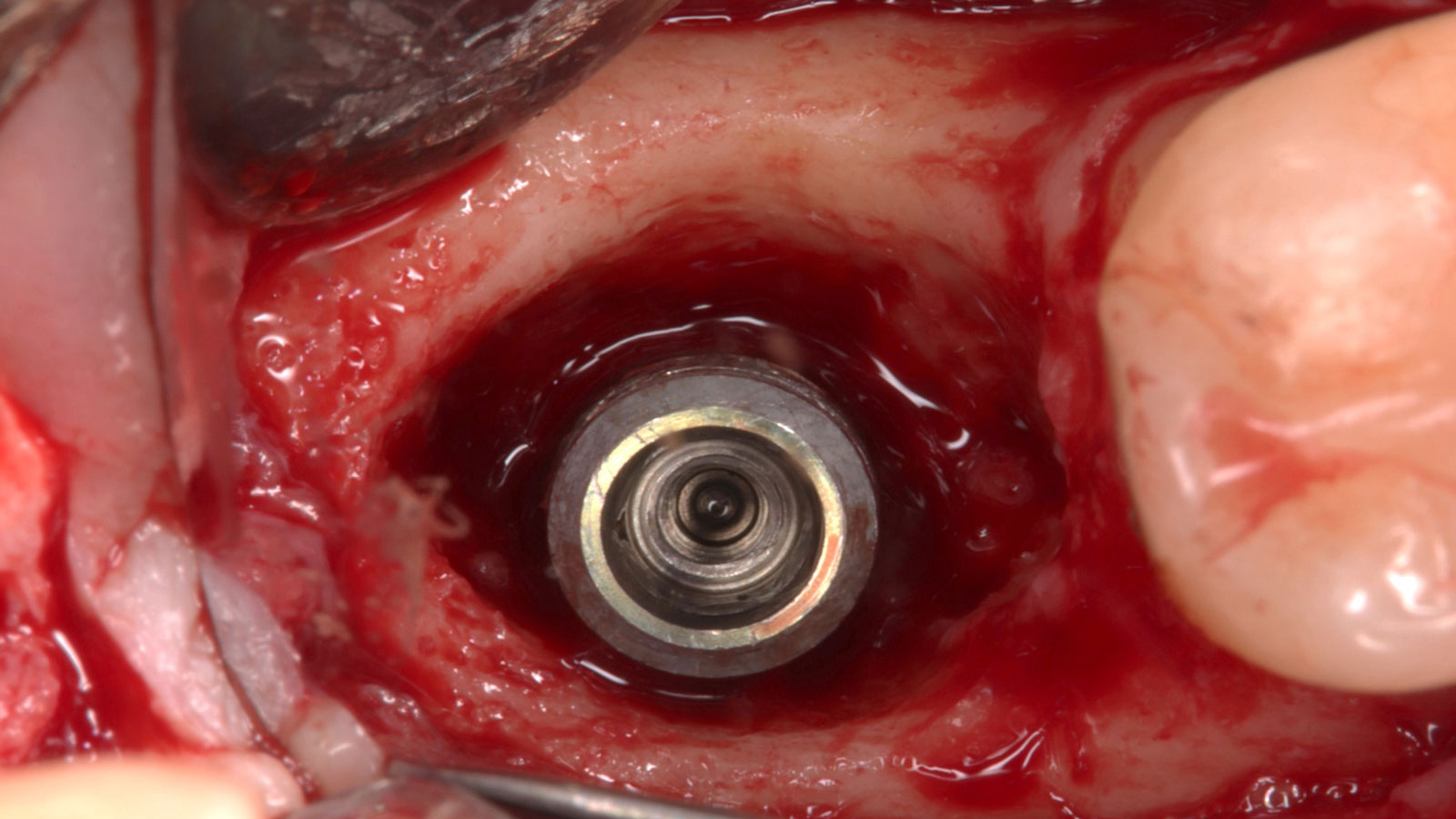
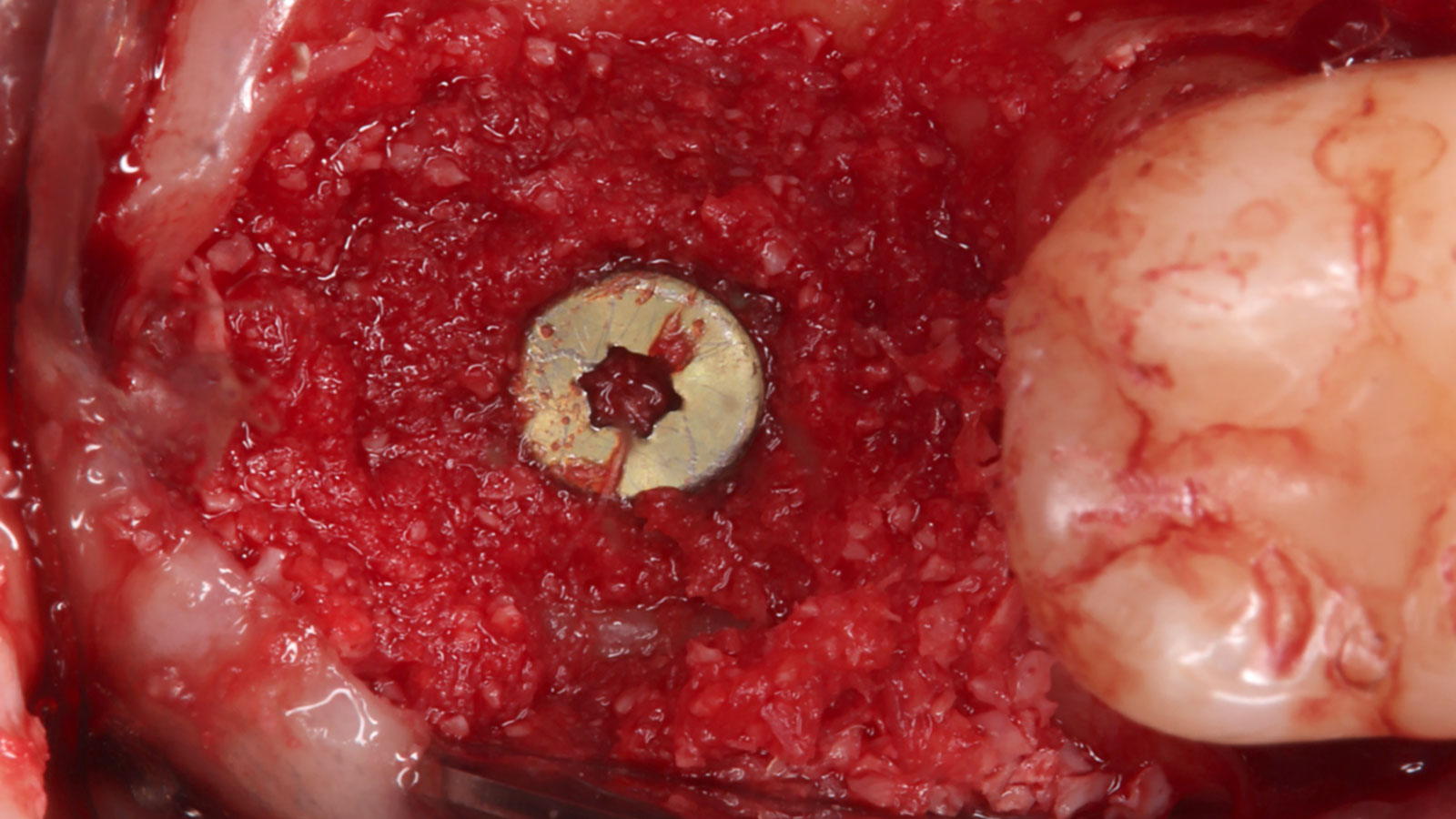
THE APPROACH
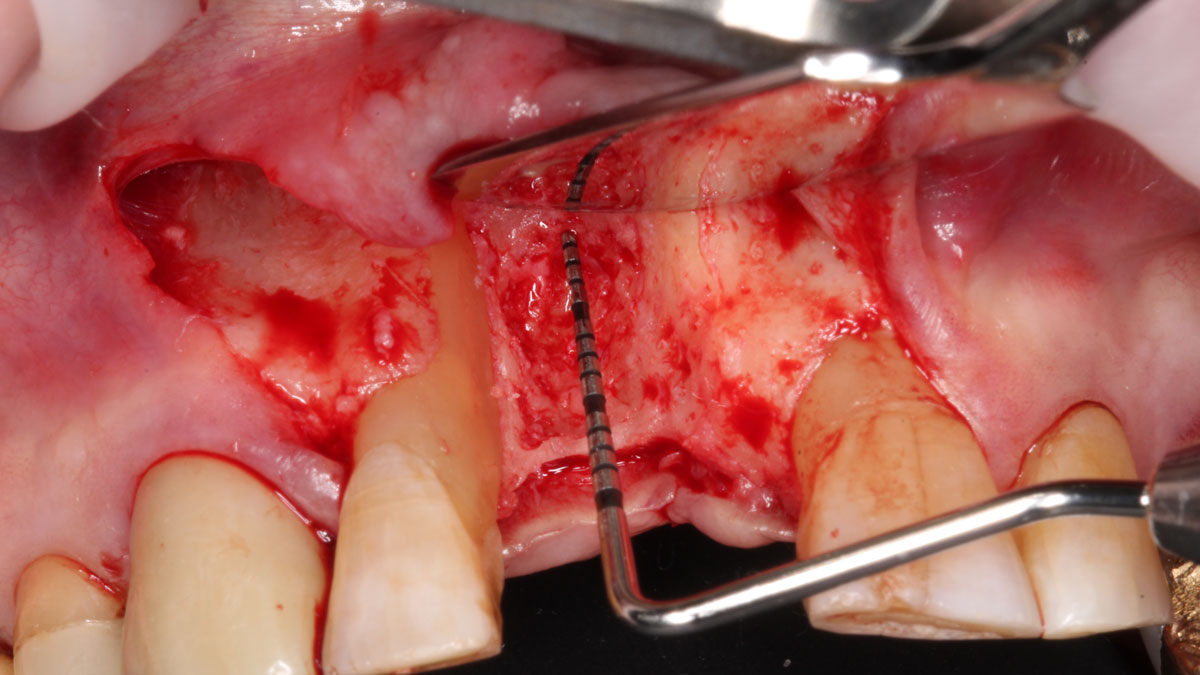
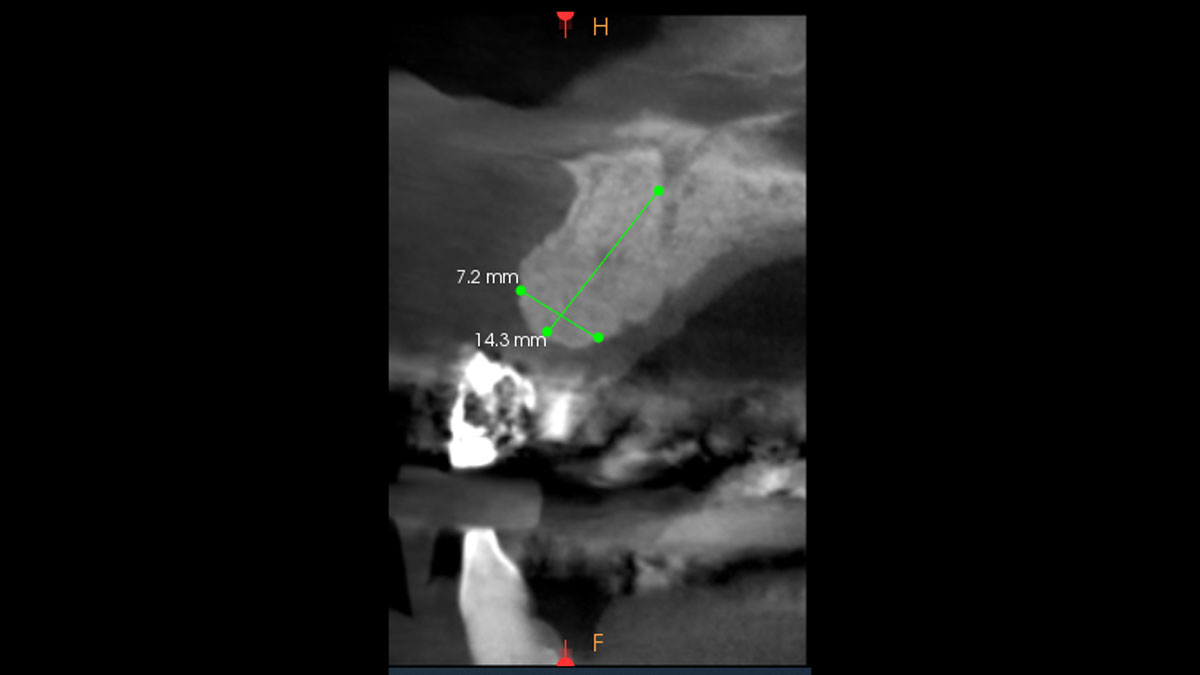
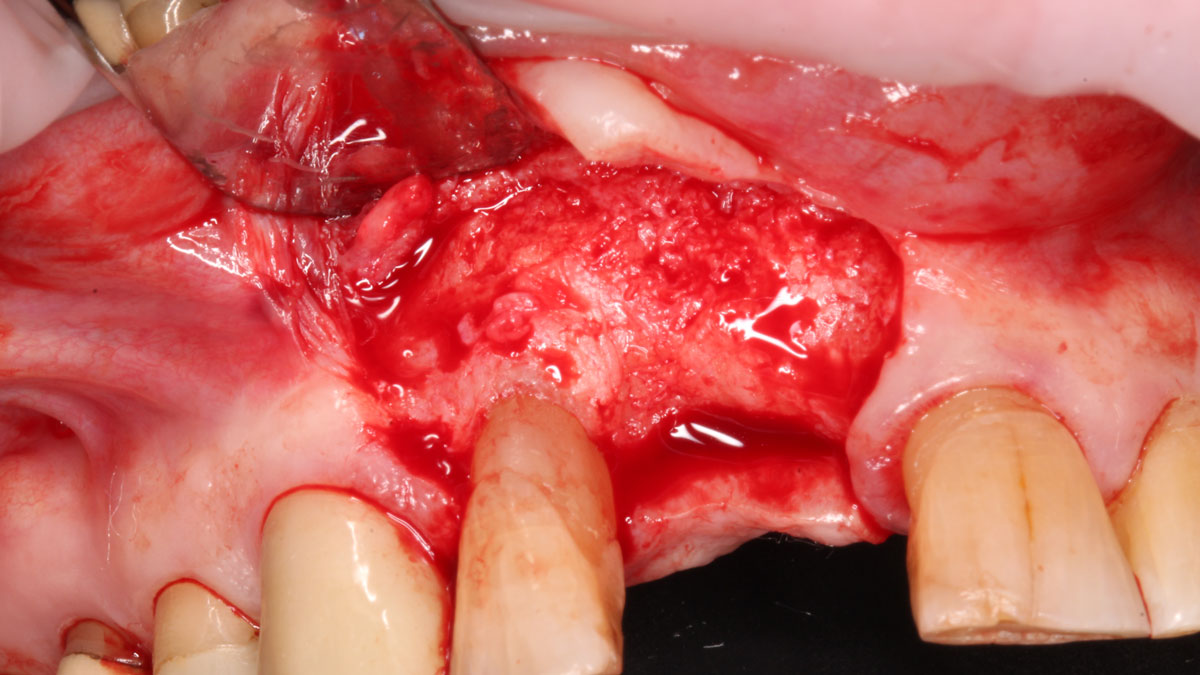
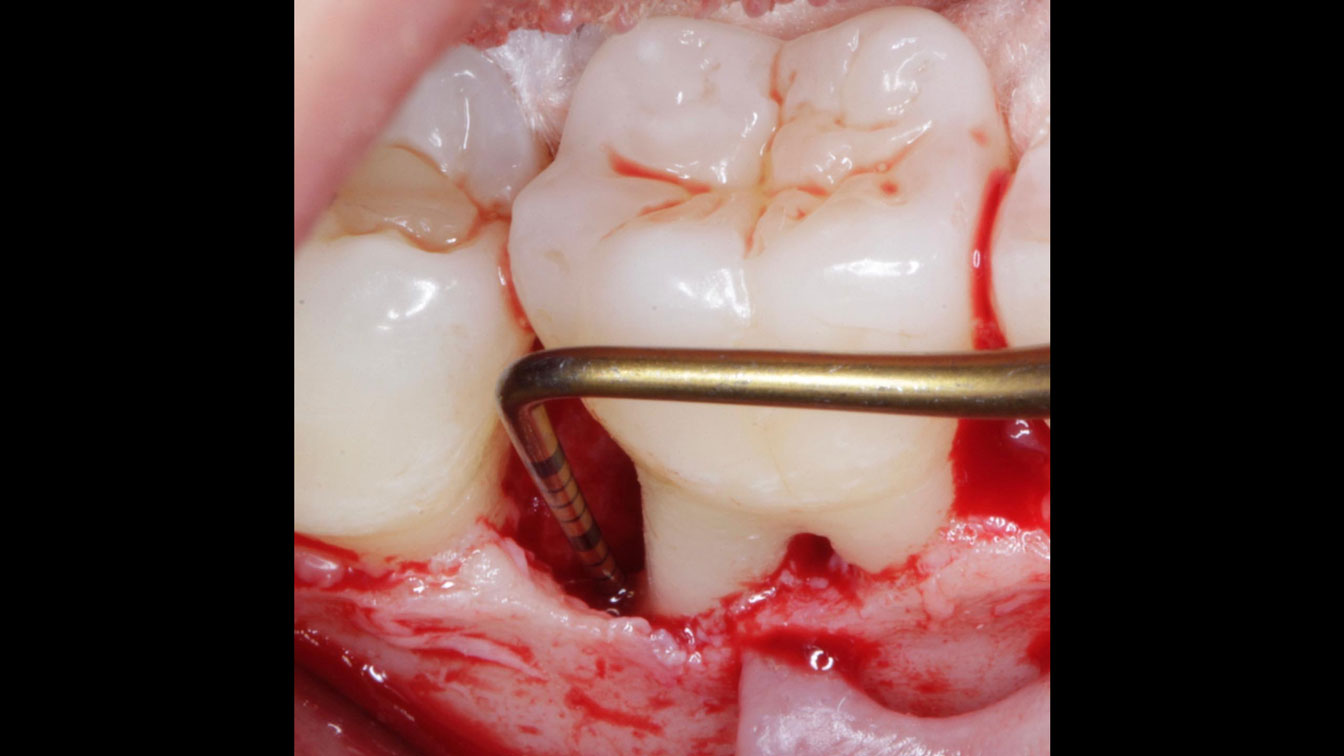
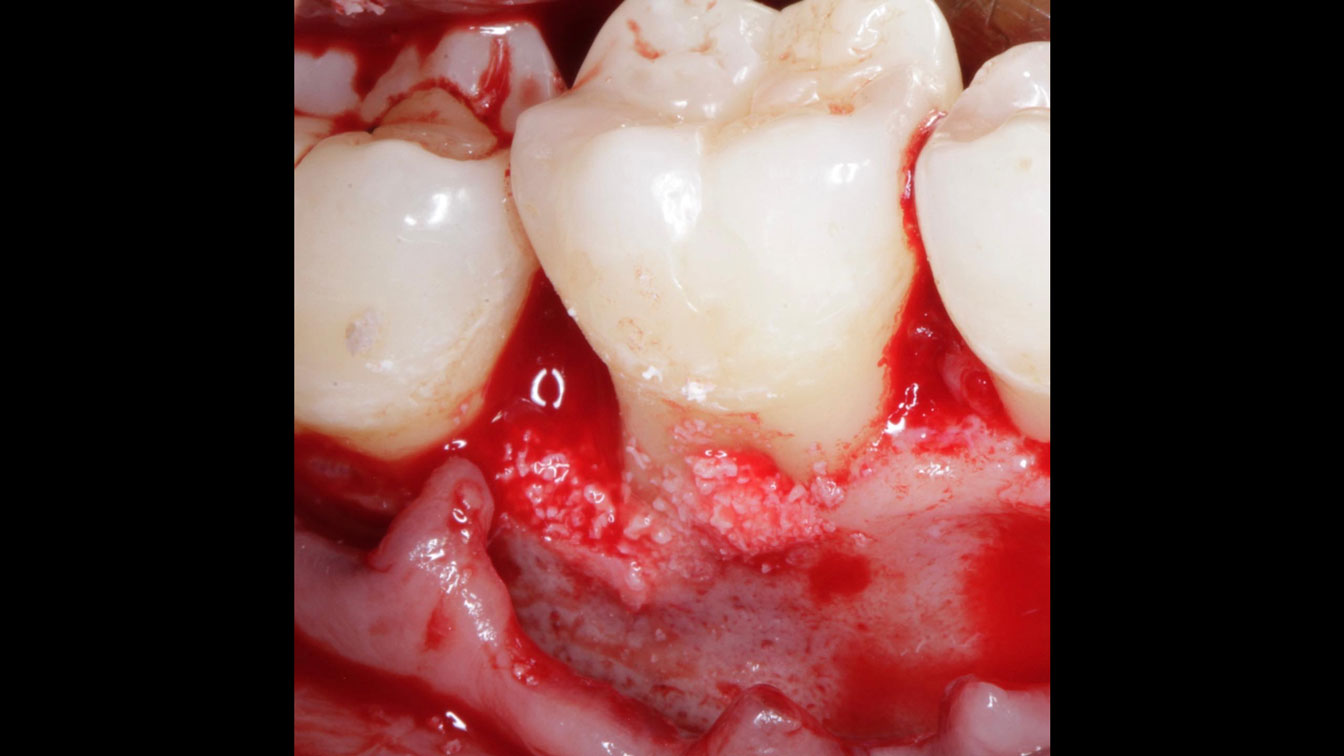
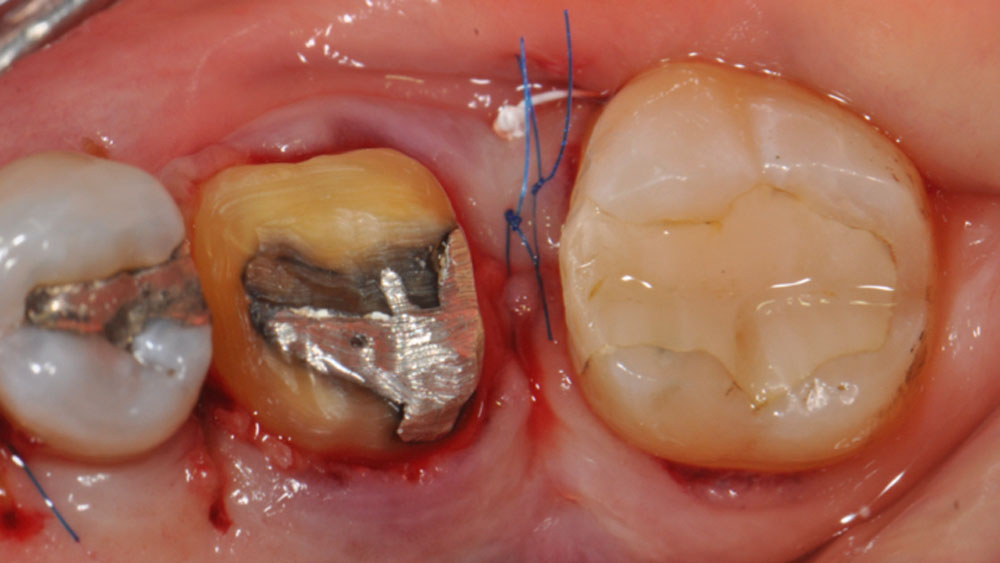
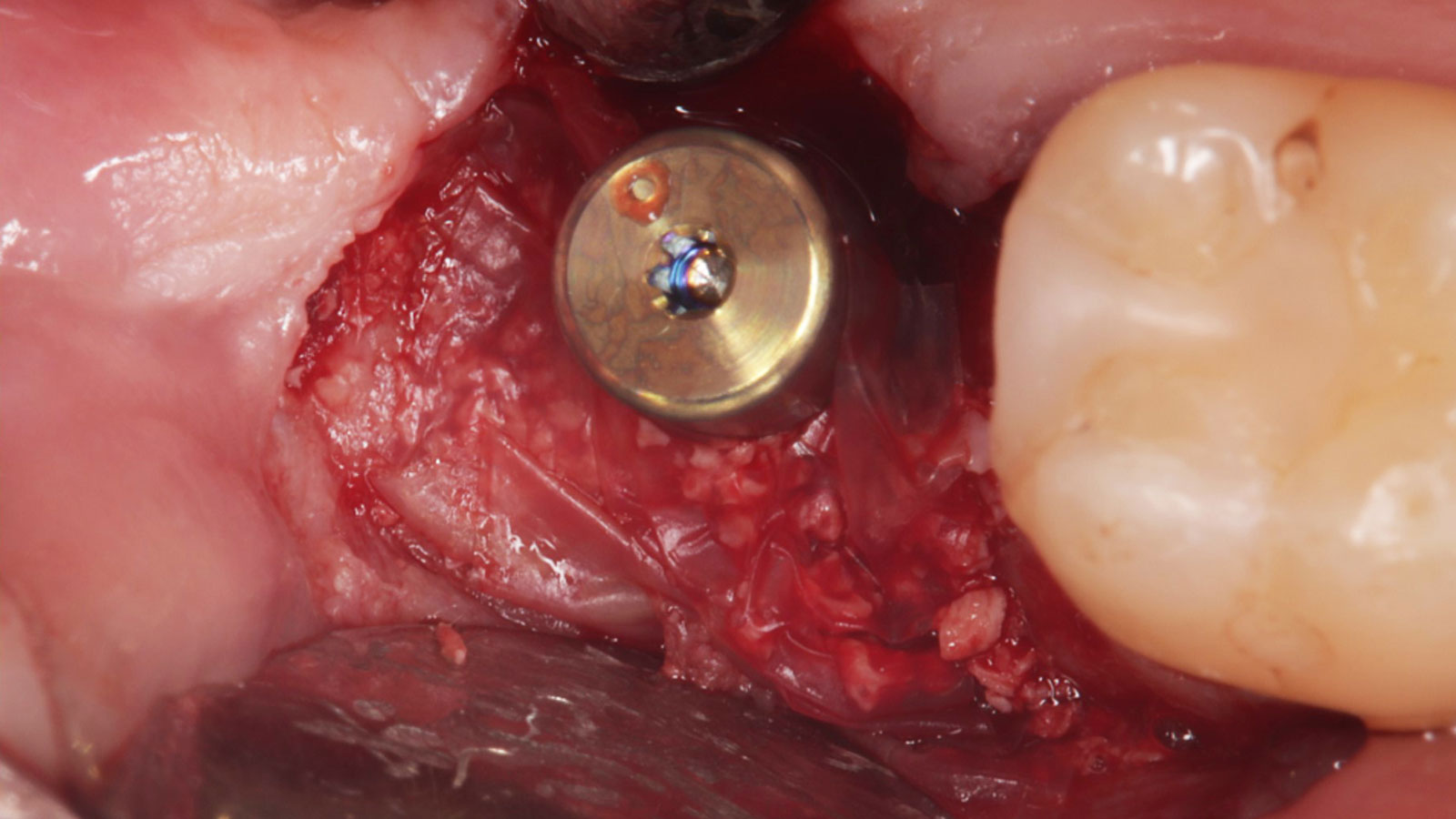
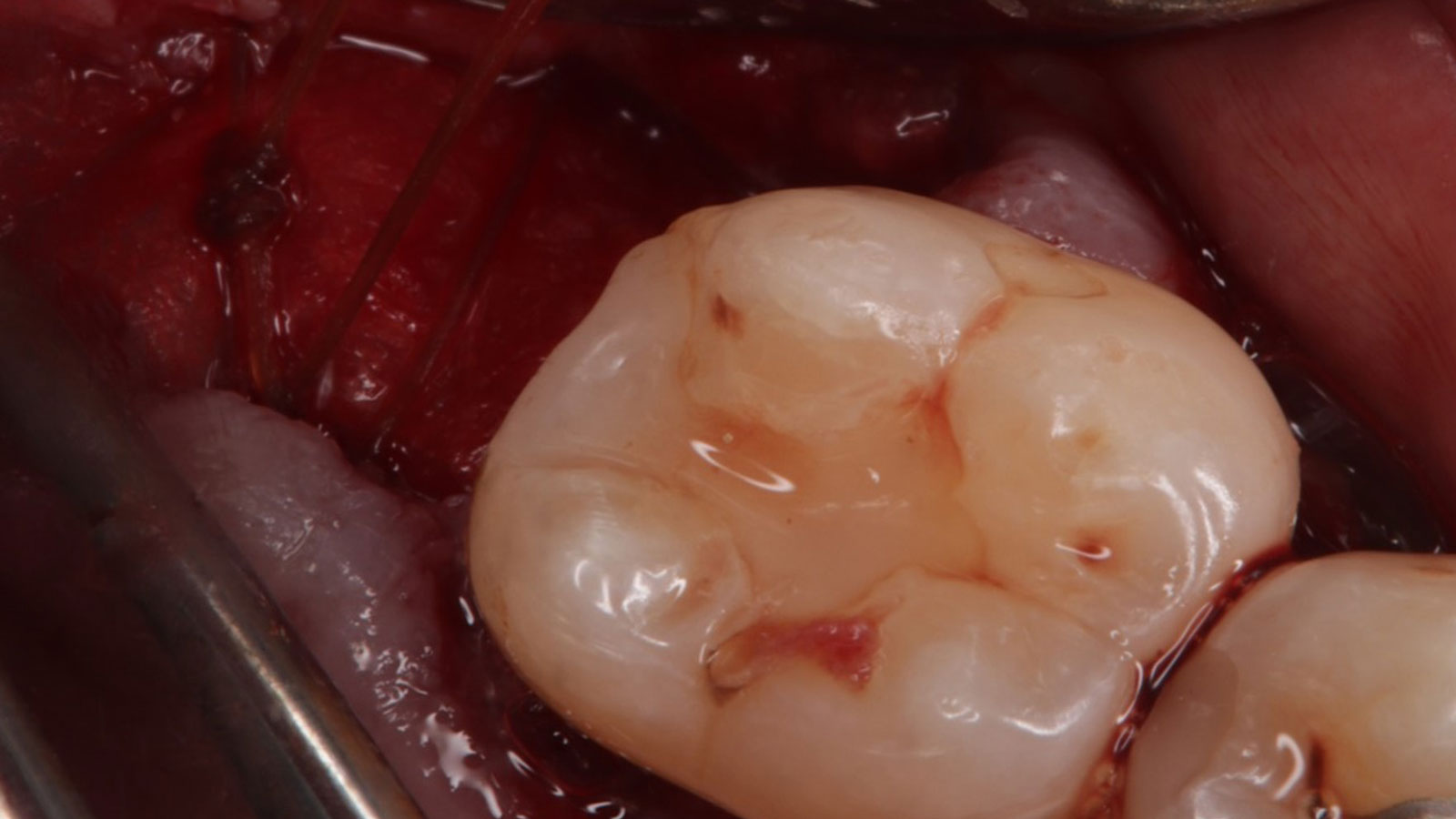
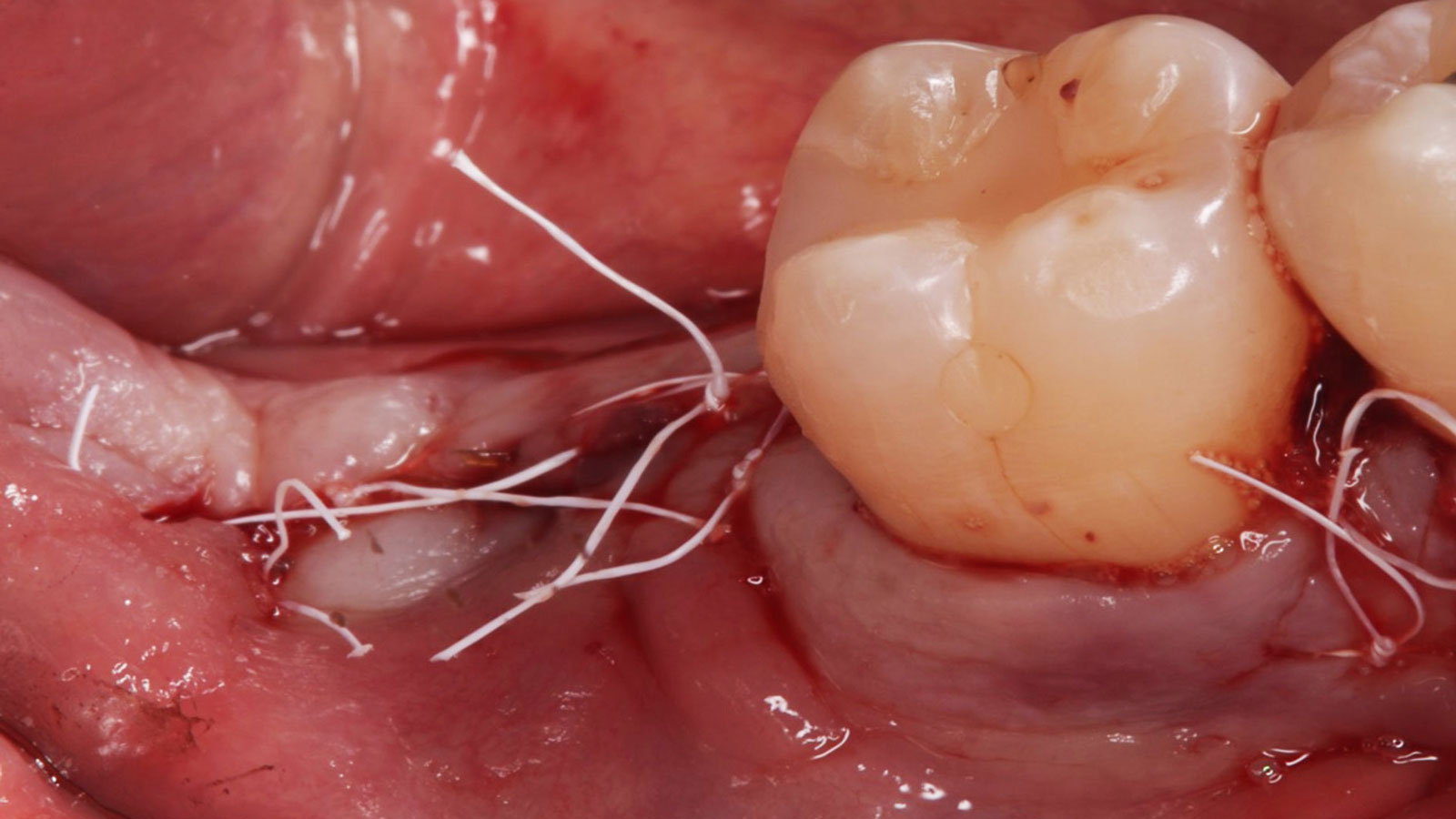
Considering the patient’s age, condition, and good compliance, a regenerative approach was chosen to preserve all teeth. Due to the extent and severity of the defect, a bone graft, biologics, and a membrane were utilized. The goal was to restore lost attachment and stabilize the teeth through splinted therapy.
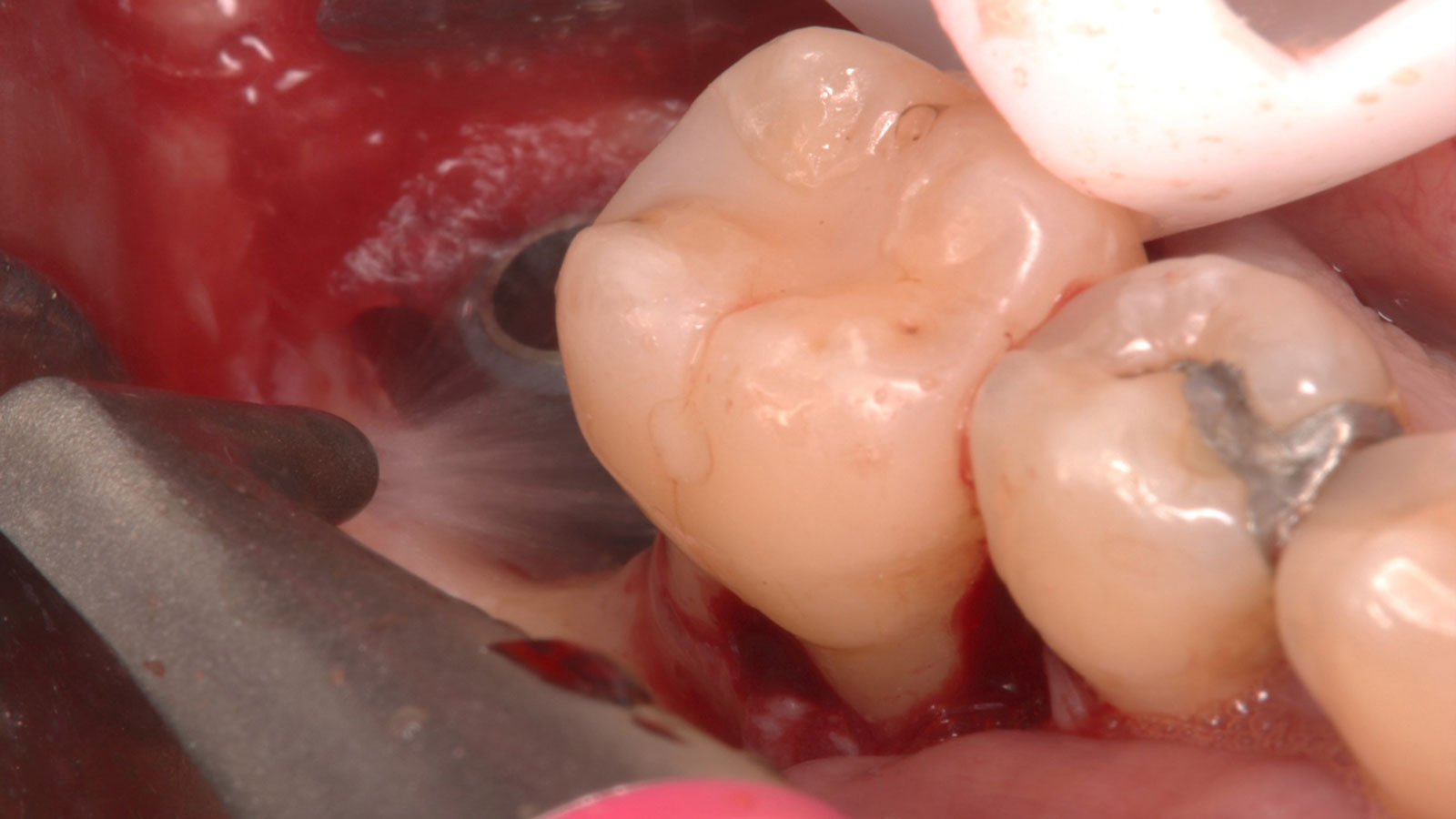
THE OUTCOME
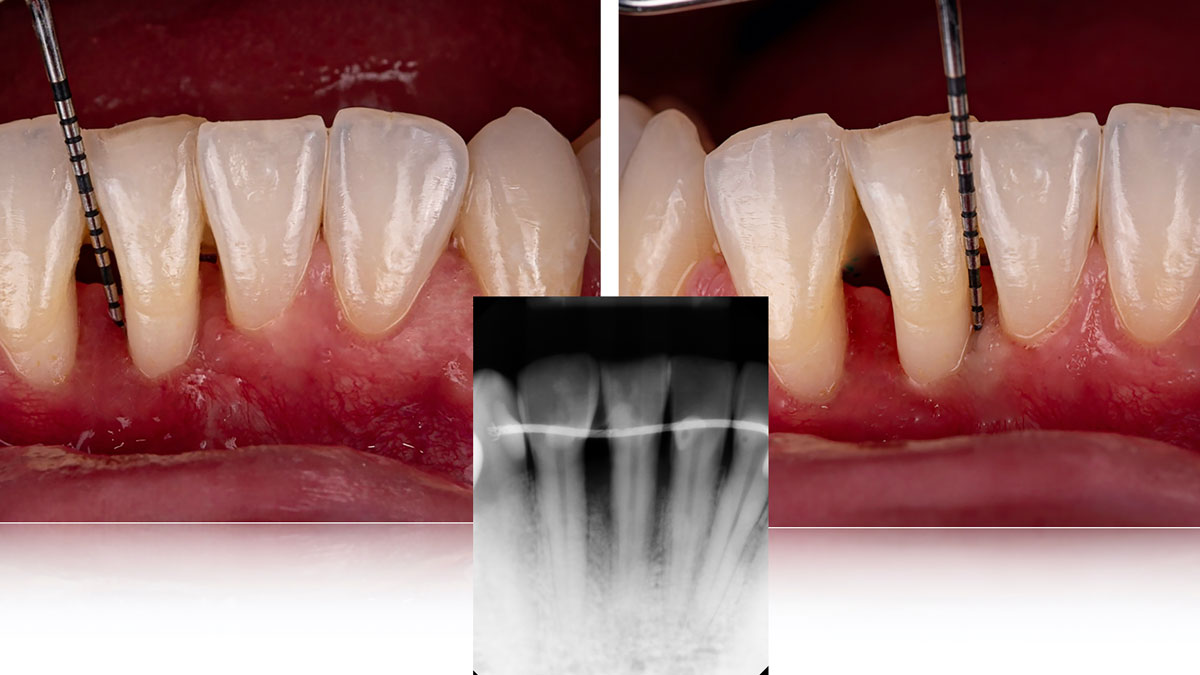
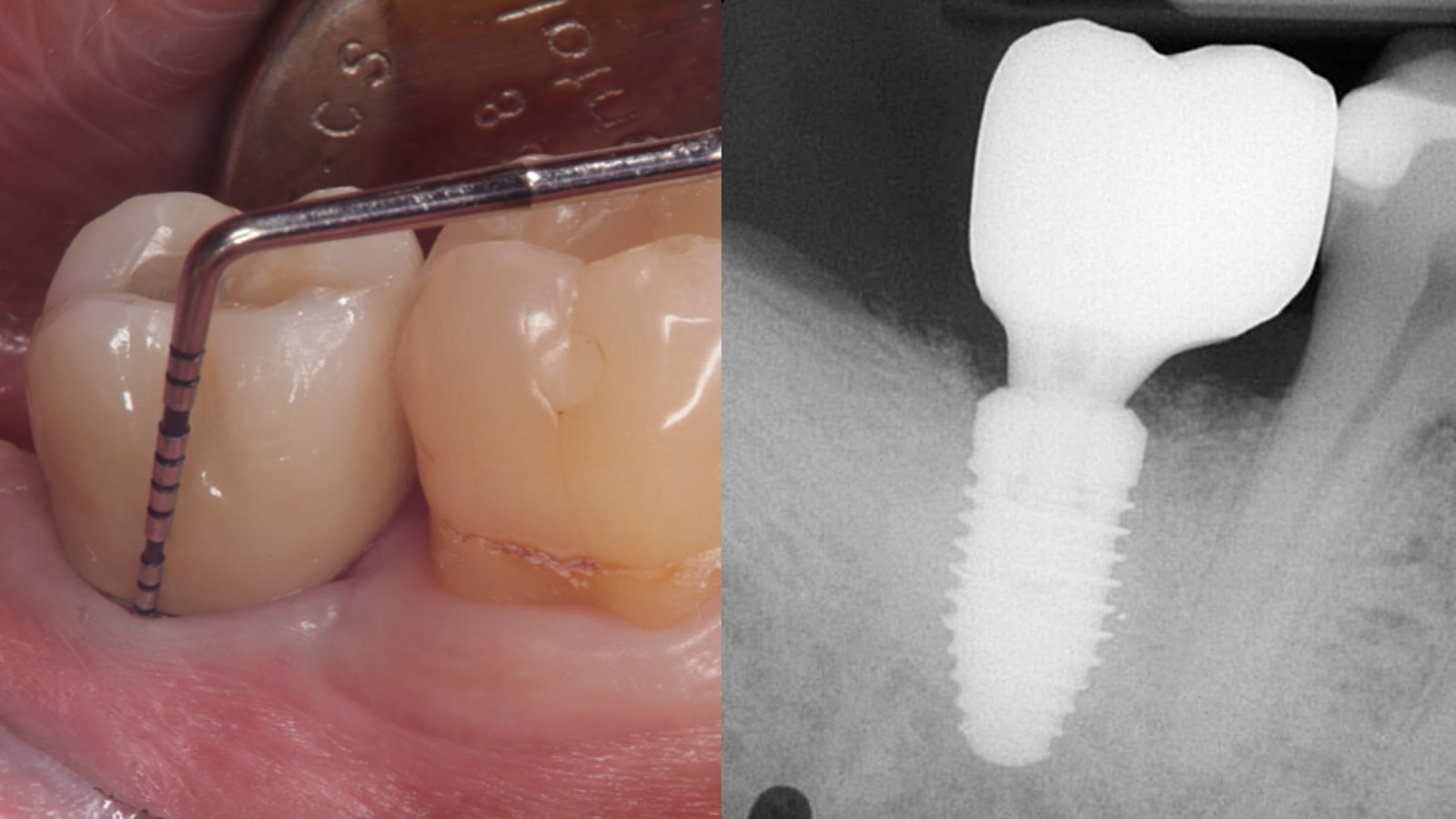
At the 7-month follow-up, probing depths decreased from 7 mm (MB, DB) to 3 mm, with radiographic bone fill indicating a 90% success. Attachment gain of 3 mm was achieved, improving from 7 mm to 4 mm. The patient reported satisfactory outcomes, and splinting effectively maintained tooth stability with no mobility.