BIOBRIEF
Odontogenic Keratocyst Management


THE SITUATION
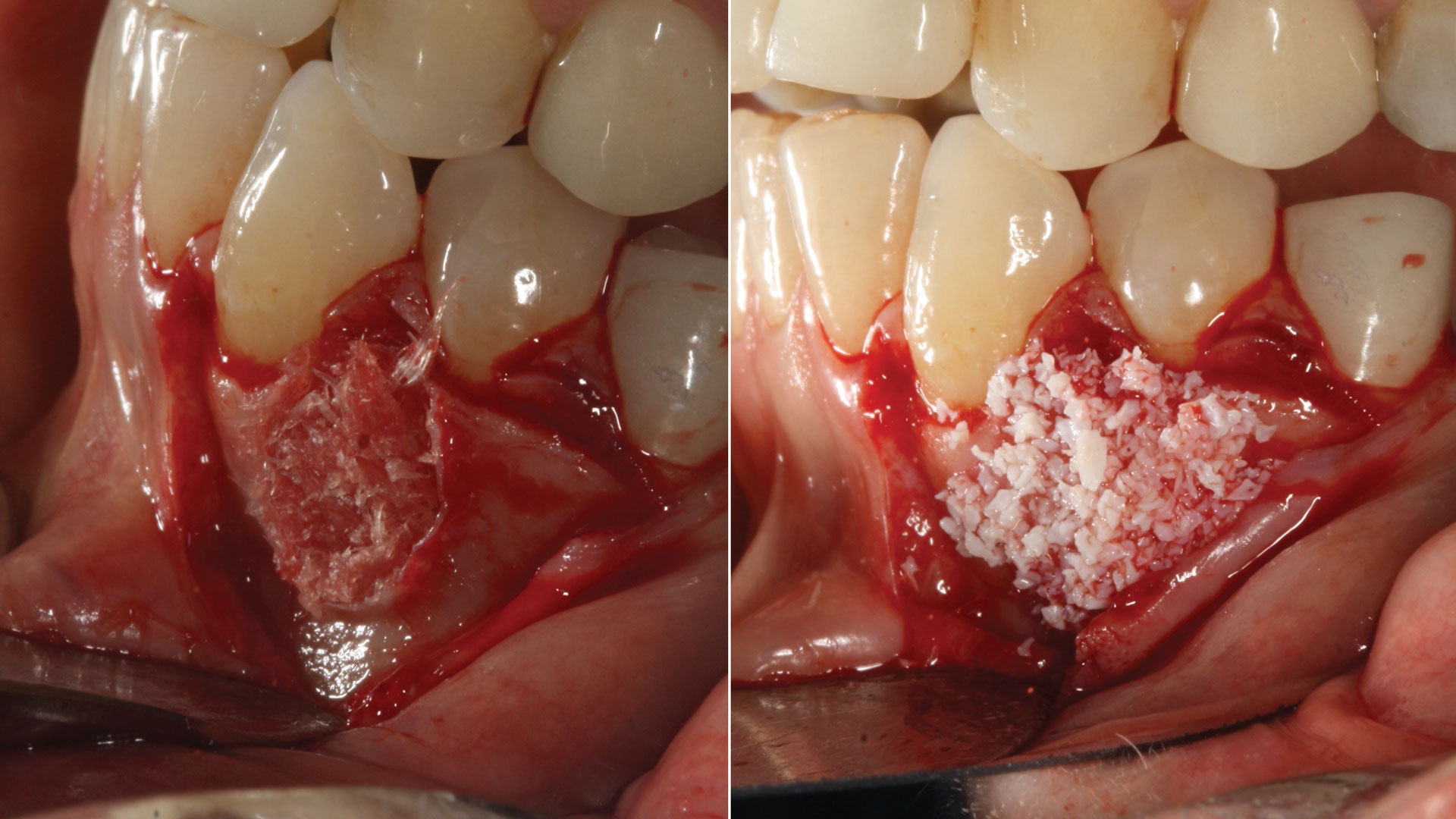
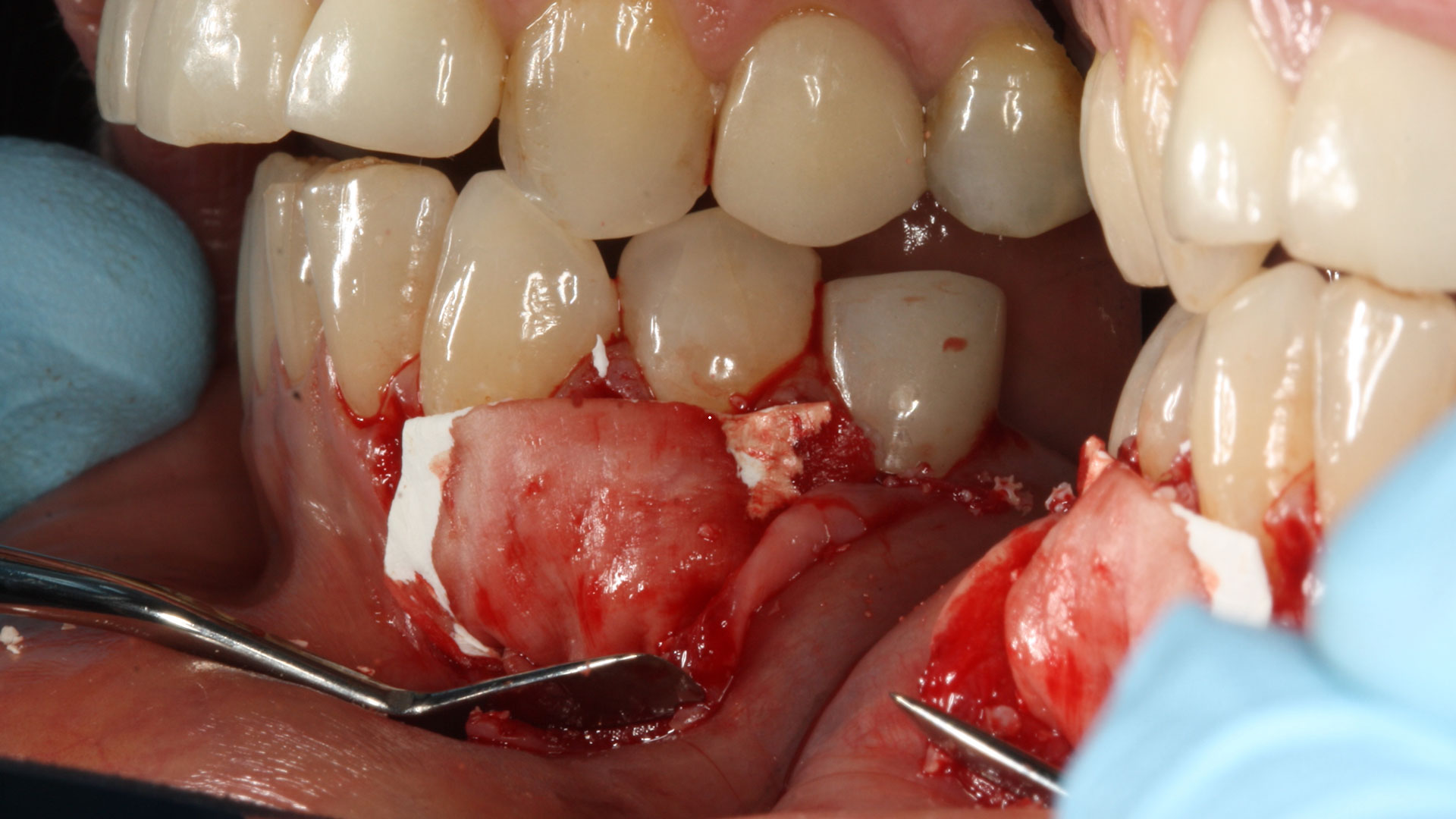
A 60-year-old-heathy Caucasian female presented with the chief complaint: “I noticed a bump on my lower left teeth since last year.” An examination revealed a stable periodontium except for enlarged gingival tissue between #21-22 measuring 10x8x5mm, well-defined borders, depressible, non-painful, and vital teeth without displacement. The treatment plan included flap surgery, excisional biopsy, GTR #21-22 (Diff Dx: Lateral periodontal cyst (LPC), Odontogenic Keratocyst (OKC), Benign Fibro-Osseous lesion (BFOL).
Guided Tissue Regeneration (GTR) using Geistlich Bio-Oss® and vallos®f was performed and covered with a resorbable collagen membrane (Geistlich Bio-Gide®).
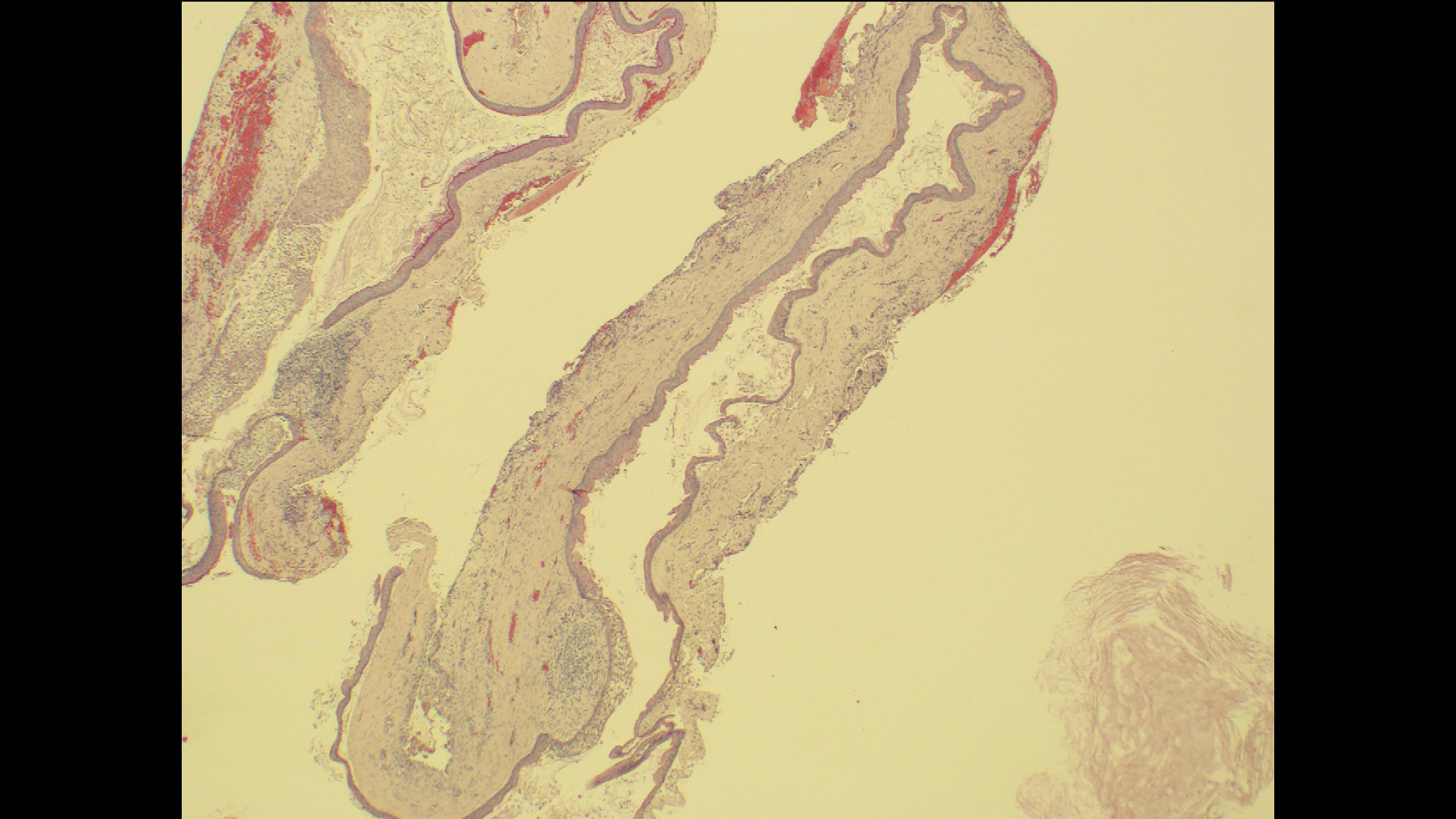
Primary closure was completed using non-resorbable sutures. Follow-up at 2, 4 weeks, 3, 6 months showed stable periodontium without re-occurrence. The pathology report indicated OKC and the area is monitored annually.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
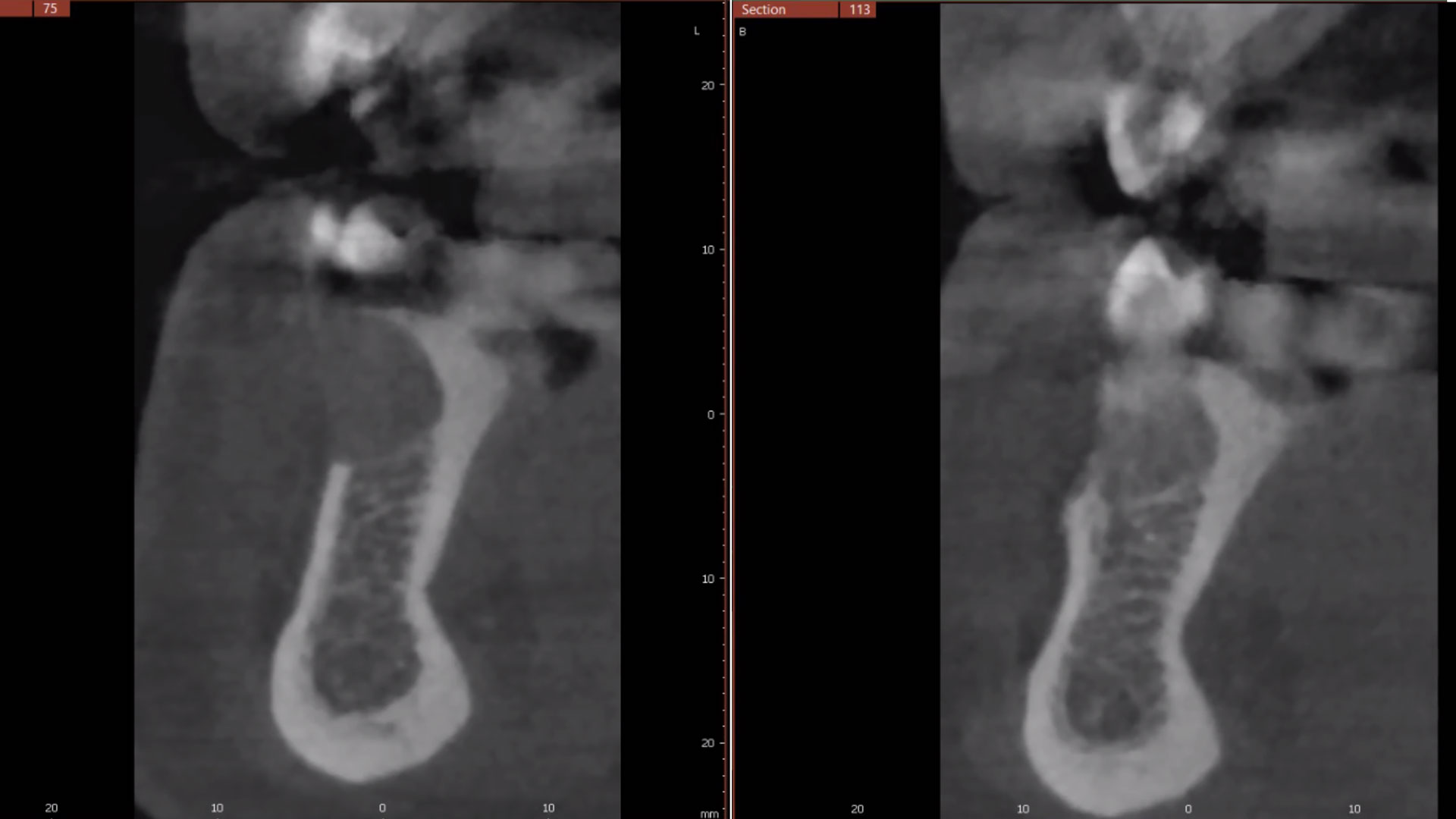
The treatment goal was to excise the lesion around #21-22 and stabilize the periodontium. Sulcular incisions #20-22 with vertical incision #22 MF were performed. Upon full thickness flap reflection, the lesion was removed (excisional biopsy). The defect extended #21M-#22D with complete facial bone loss. It was a wide 1-2 bony wall defect measuring 10x8x5mm. GTR procedure using Geistlich Bio-Oss® and vallos®f and Geistlich Bio-Gide® for the collagen membrane were employed. Primary closure was obtained using 6-0 prolene suture.
“Excisional biopsy and guided tissue regeneration is indicated to treat the pathology (#21-22 area) and stabilize the periodontium.”
— Dr. Bassam Kinaia
THE OUTCOME
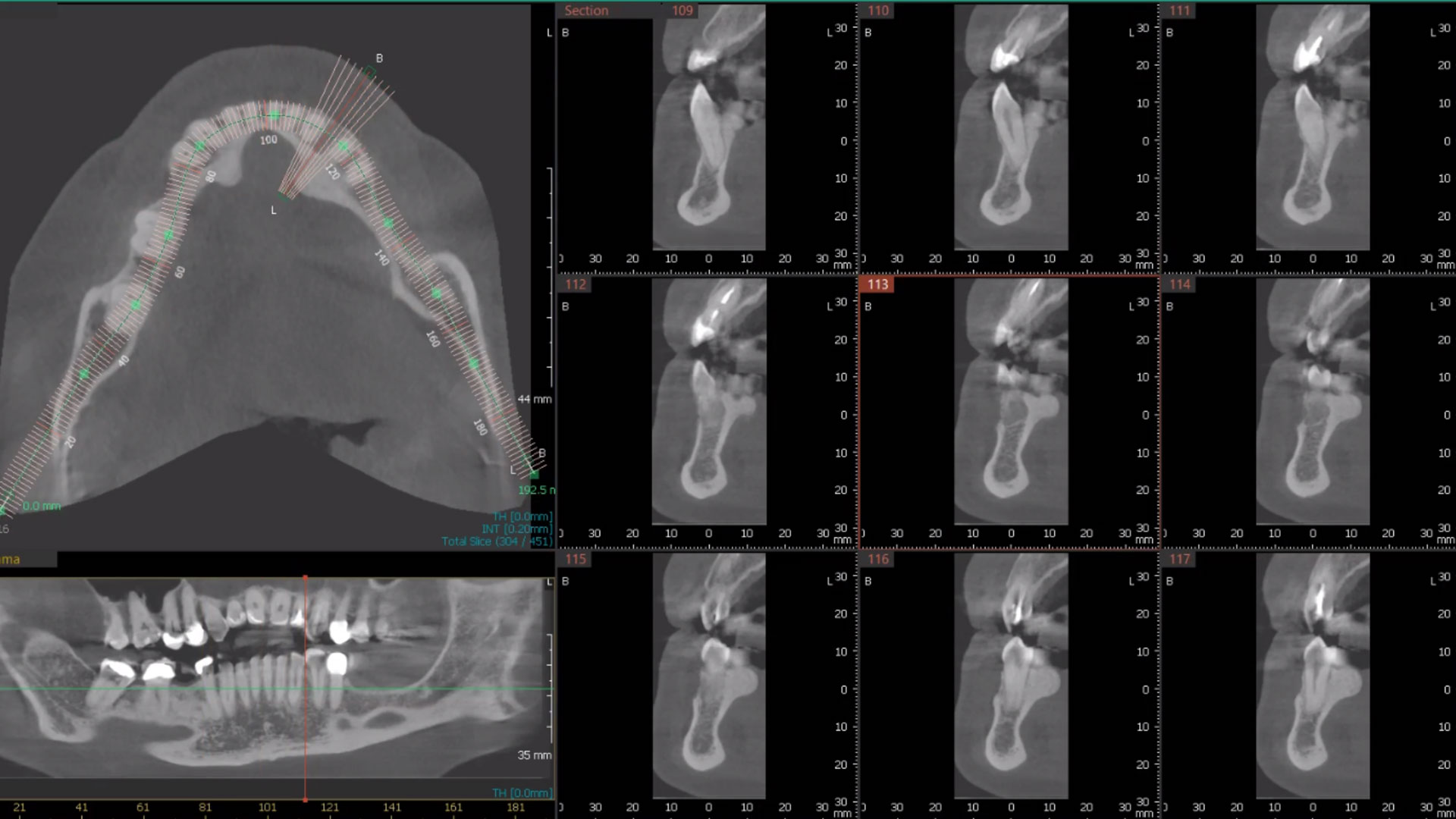
Complete excision of pathology and biopsy followed by GTR using vallos®f internally for maximum osteogenic/osteoinductive potential and Geistlich BioOss® externally for space maintenance showed excellent radiographic bone fill and stable periodontium.


Bassam Kinaia, DDS, MS, DICOI
Dr. Kinaia is the Associate Director of the Graduate Periodontology Program at the University of Detroit Mercy (UDM). He is also the former Director of the Periodontology Program at UDM in Michigan and Boston University Institute for Dental Research and Education in Dubai. He is a Diplomate of the American Academy of Periodontology (AAP) and International Congress of Oral Implantology (ICOI). He received a certificate of Excellence from the AAP in recognition of teaching-research fellowship.