BIOBRIEF
Selecting Biomaterials for Combined Complex Defects


THE SITUATION
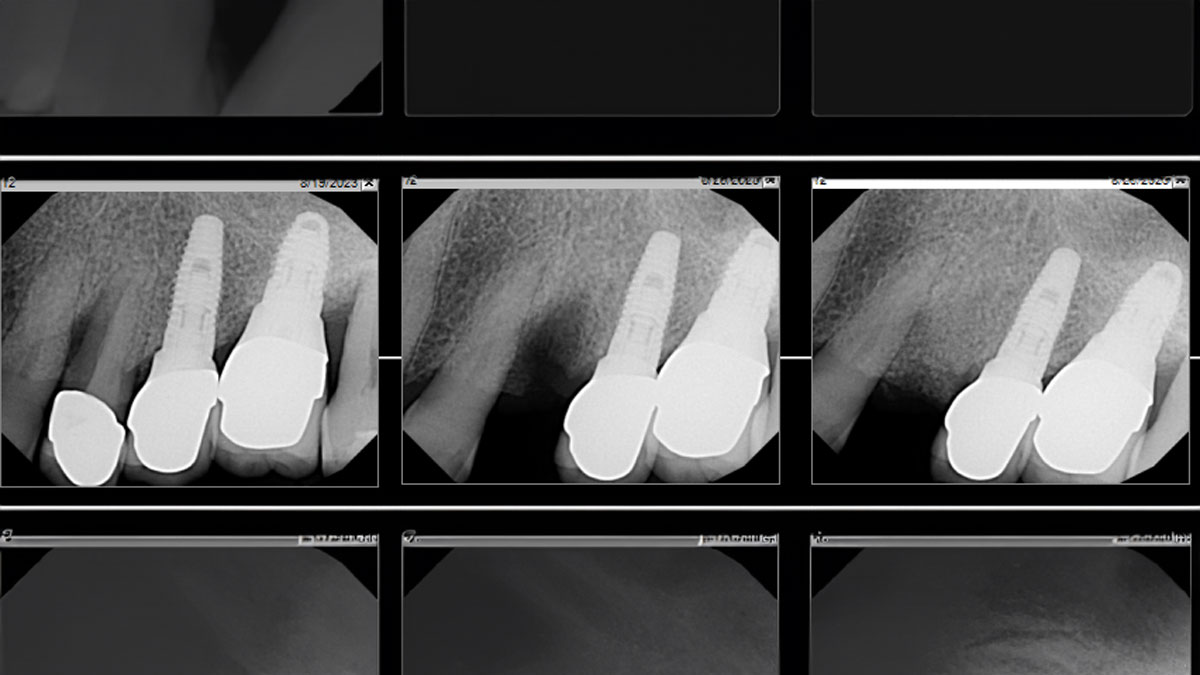
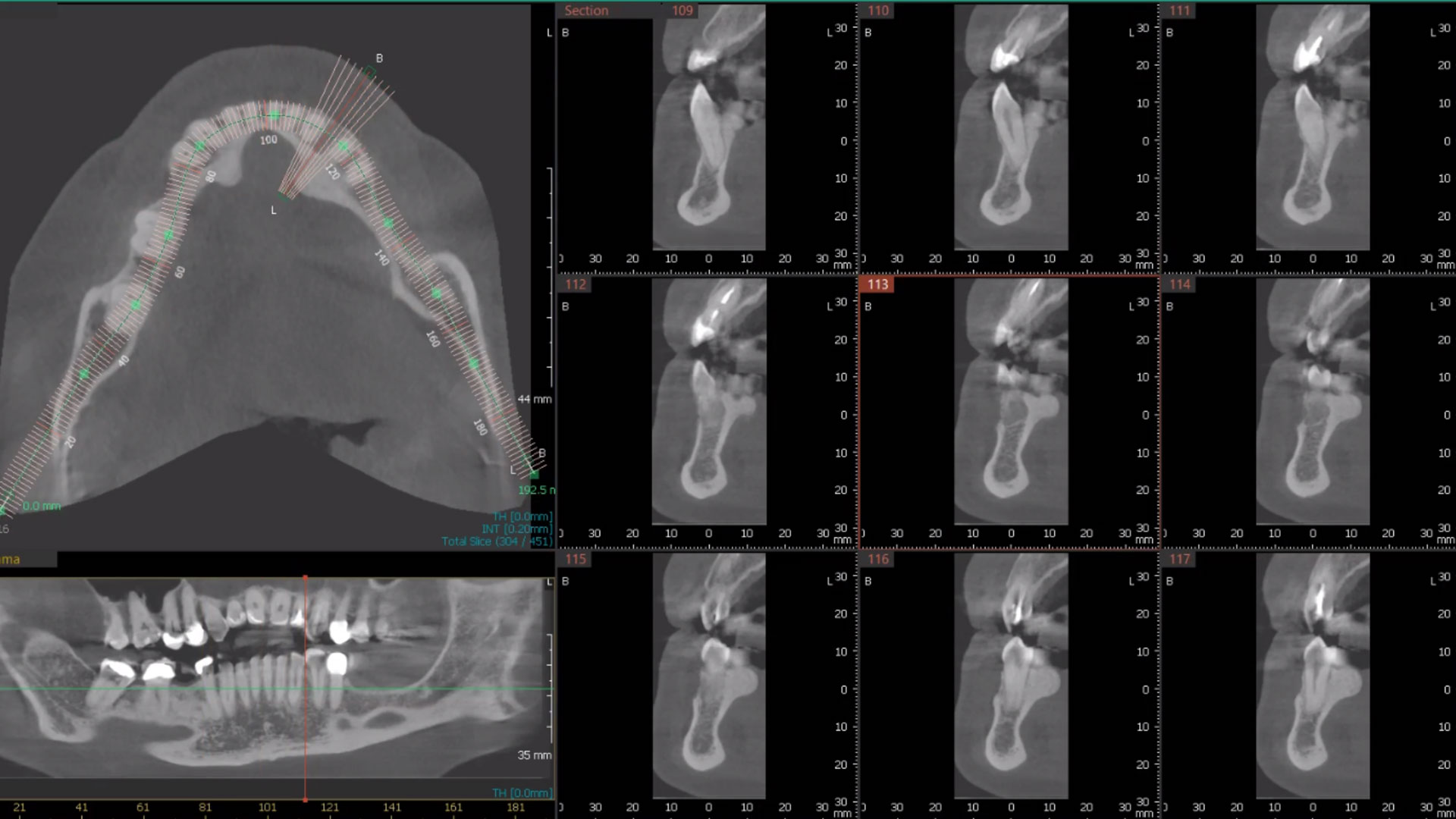
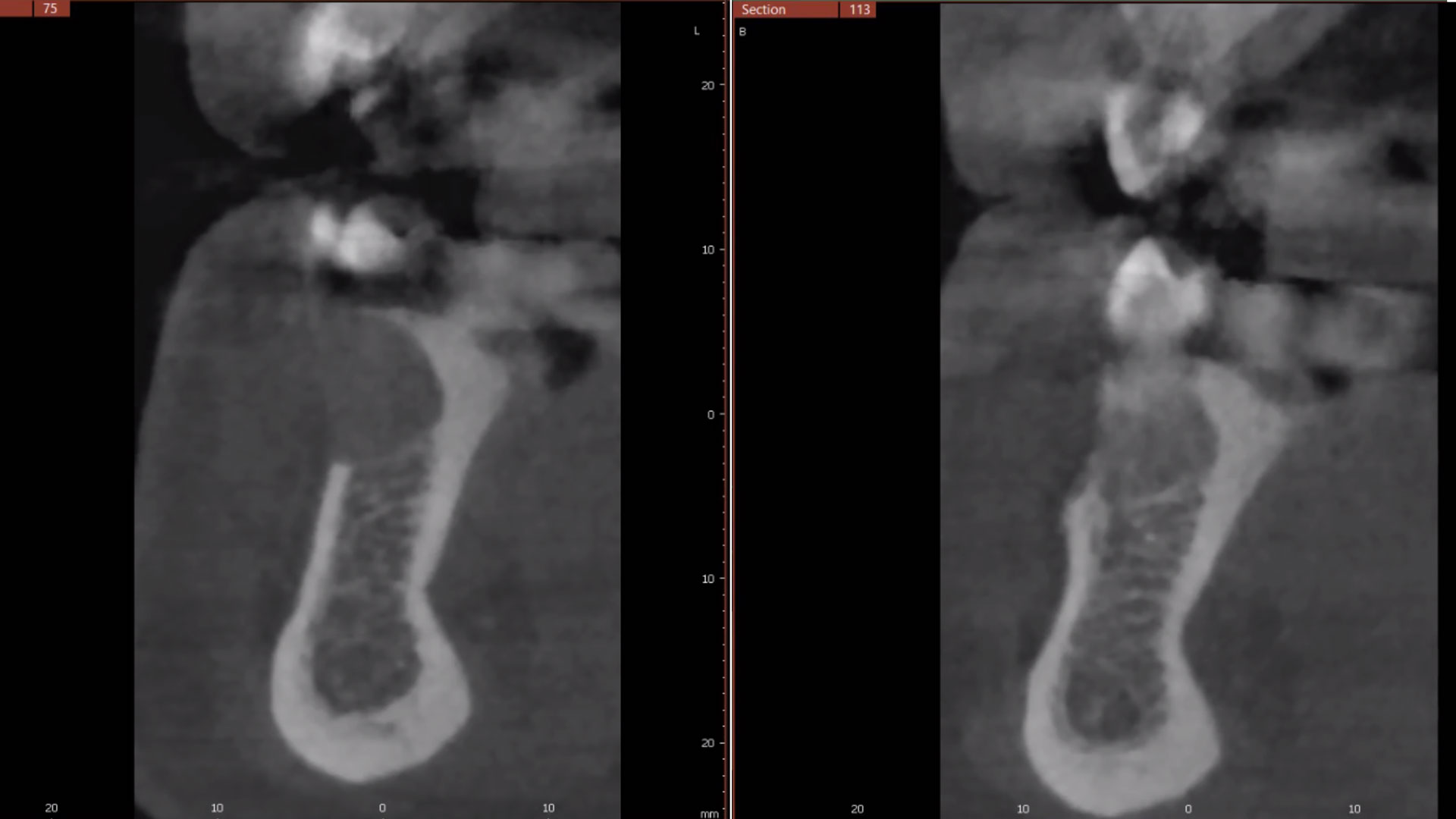
The patient called the office complaining of sensitivity and swelling in the maxillary left quadrant. He was seen and prescribed an antibiotic. Tooth #12 was deemed hopeless, and the peri-apical and radicular lesion presented on the radiograph extended significantly on the mesial aspect, impacting the interproximal bone level for tooth #11. Patient presents with implant supported restorations distal to the affected area and was concerned about the infection spreading to that area as well. The area was treated successfully, and the patient was pleased with the outcome, allowing him to preserve the tooth, on the mesial aspect of the lesion and the implant distally.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system/Non-smoker | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
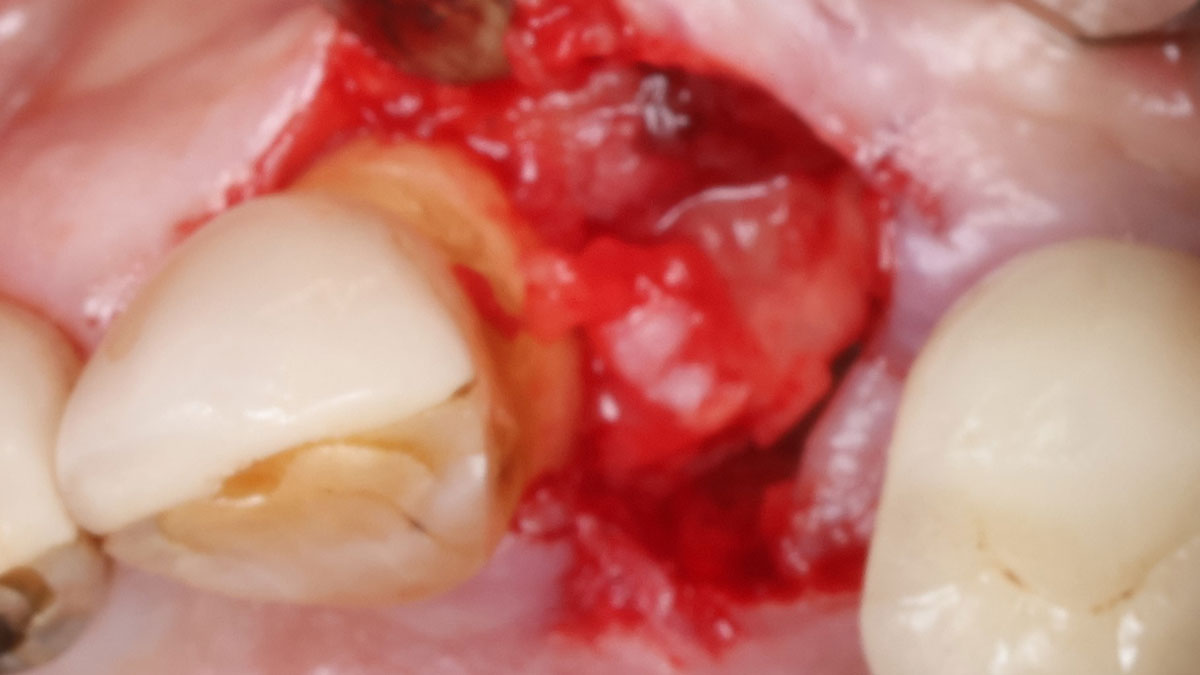
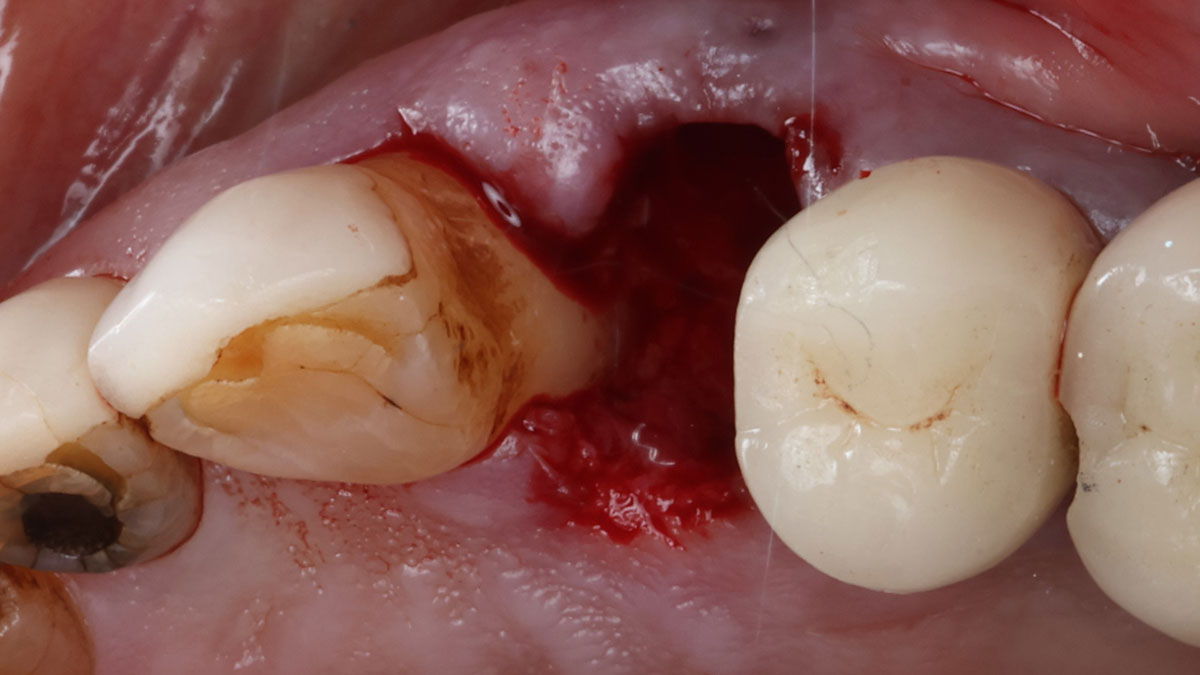
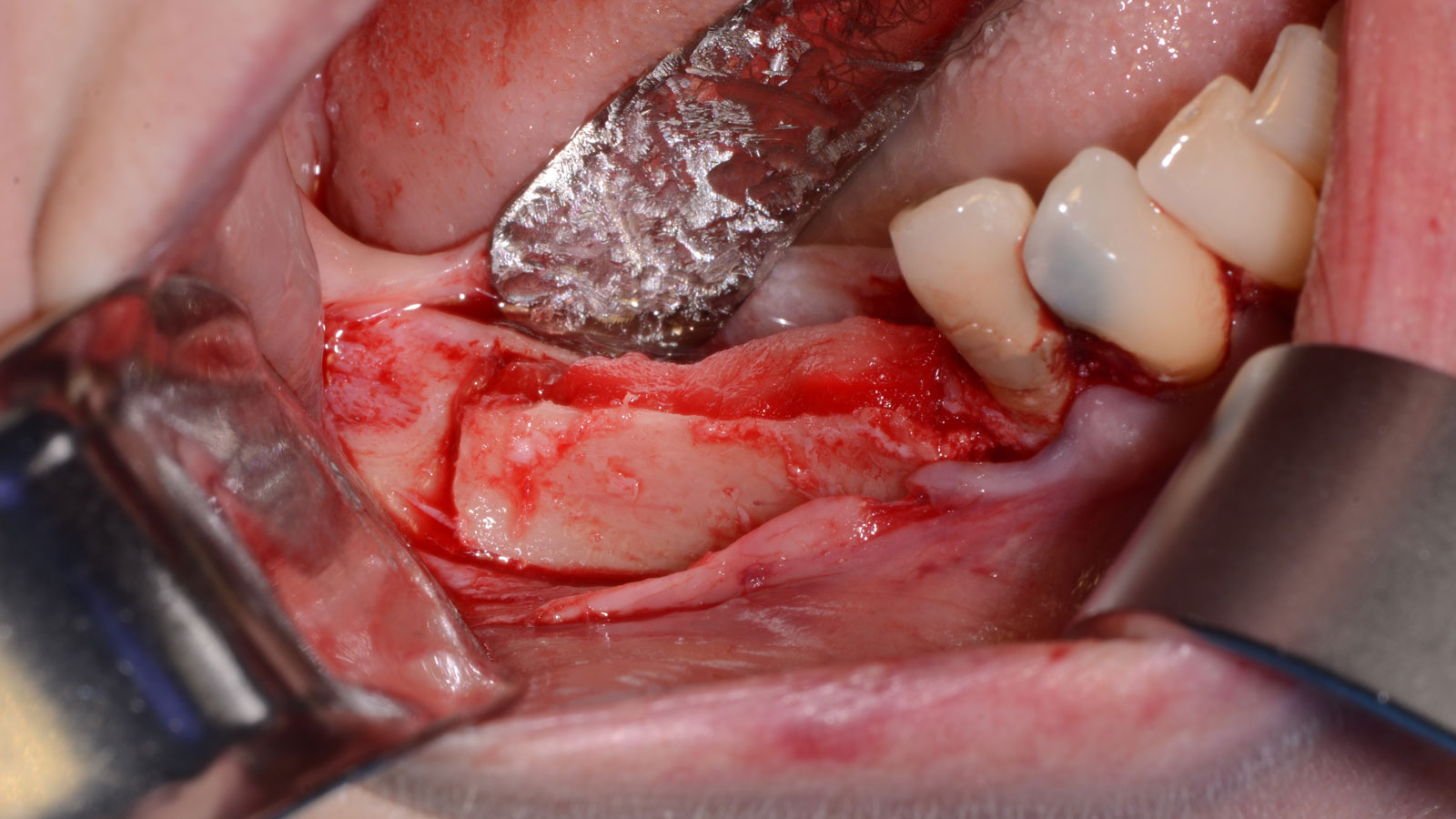
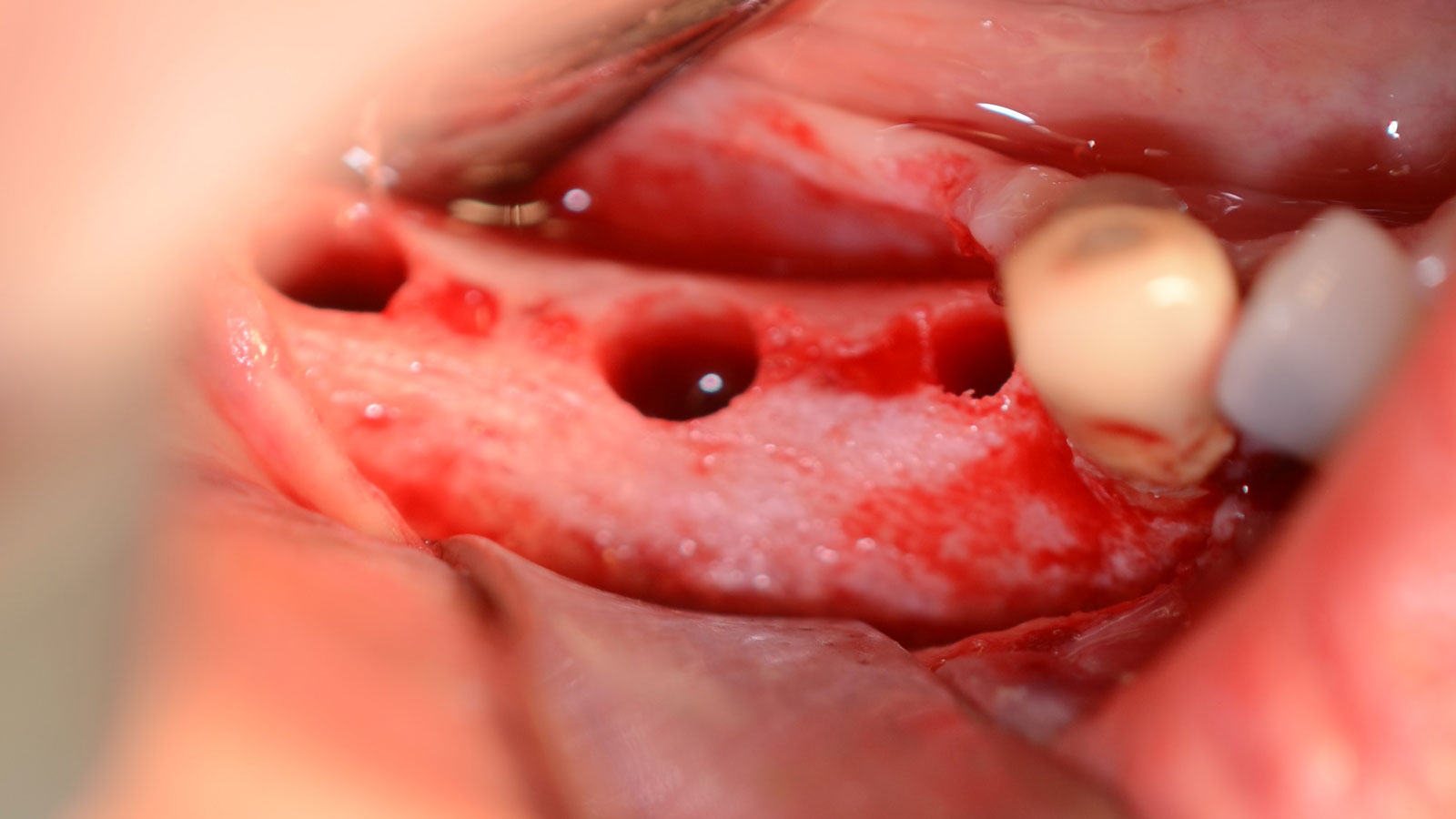
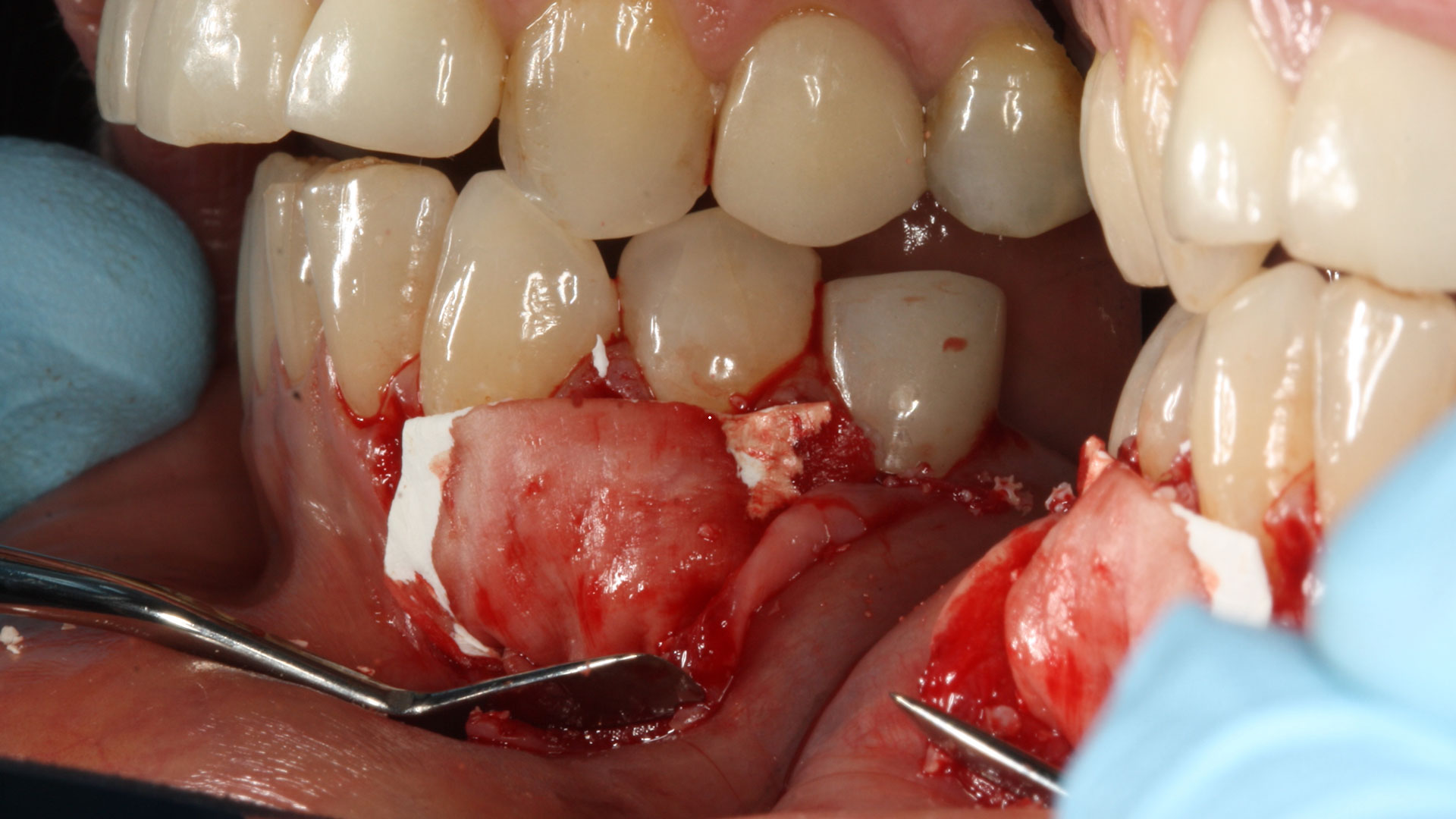
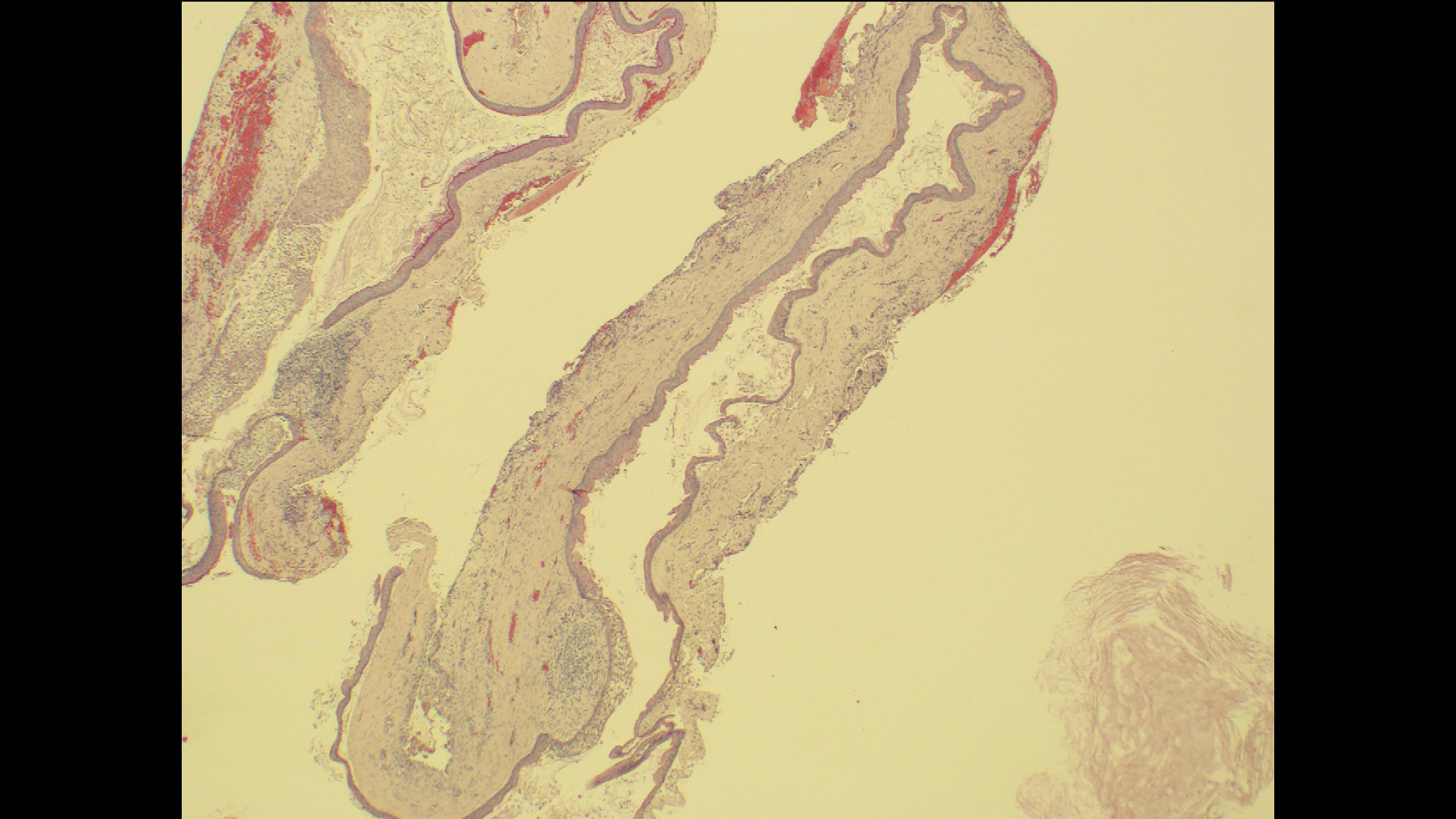
The goals of the procedure were to eliminate infection, the source of pain, and reduce periodontal problems to the adjacent tooth and implant. Full thickness flap was reflected, #12 was removed and the socket was debrided and irrigated. A peri-radicular lesion was removed and submitted for histopathological exam.
“A localized infection can easily spread and impact adjacent teeth and implants. It is critical for clinicians to intervene as soon as possible to prevent further complications. Patient education and motivation is key to successfully treat these types of clinical situations encountered in a daily practice.”
— Dr. Irina Dragan
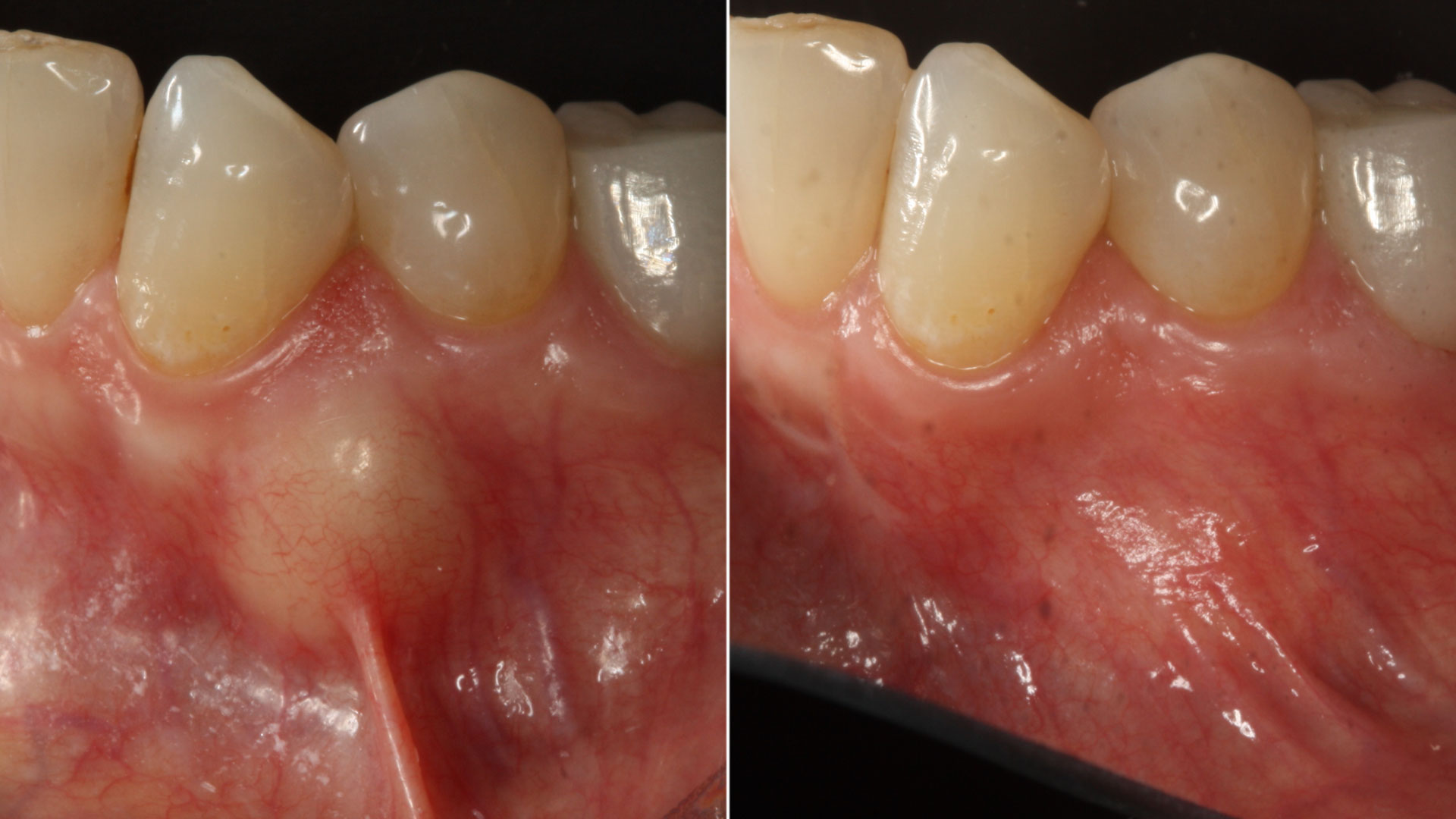
THE OUTCOME
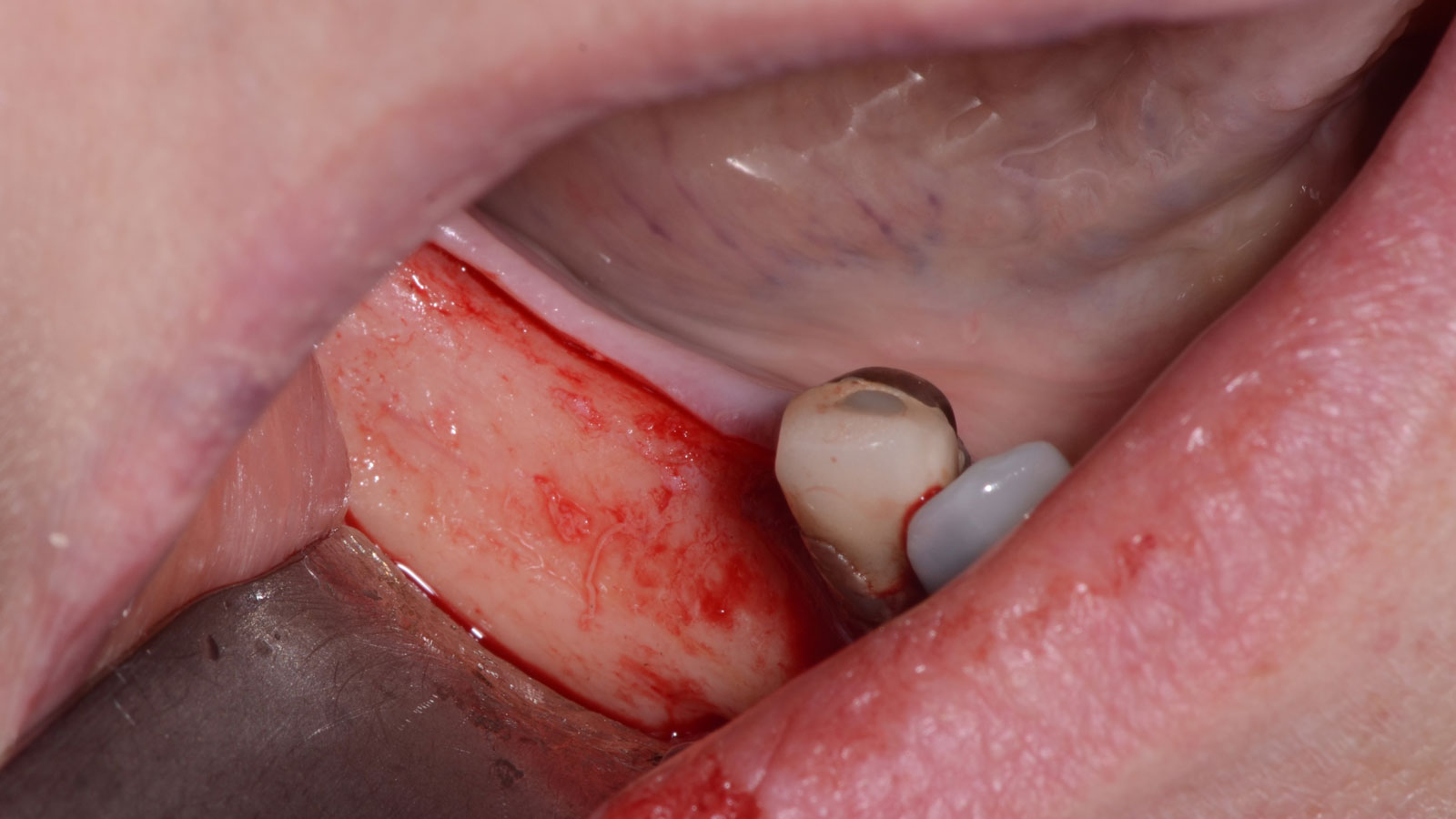
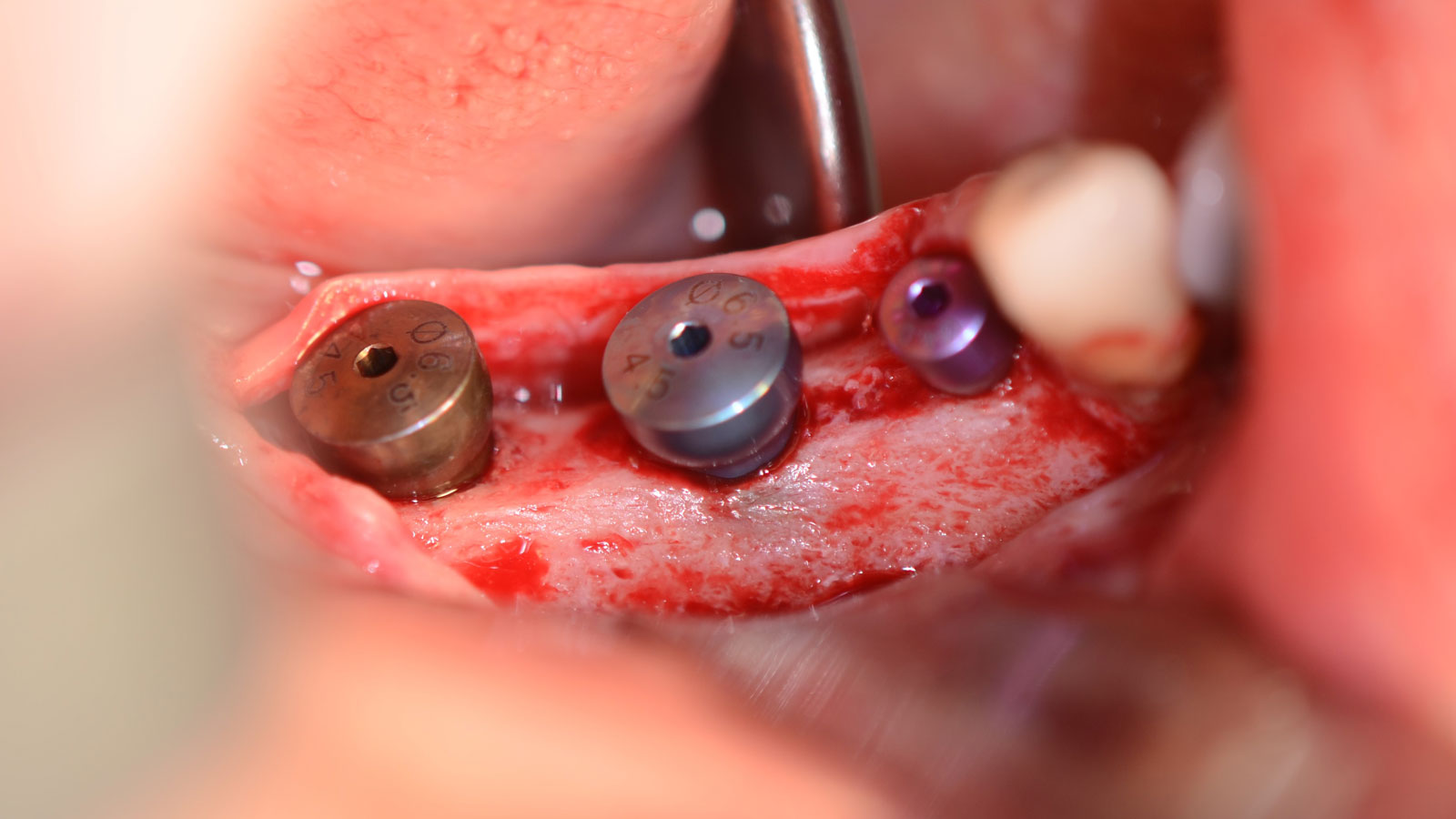
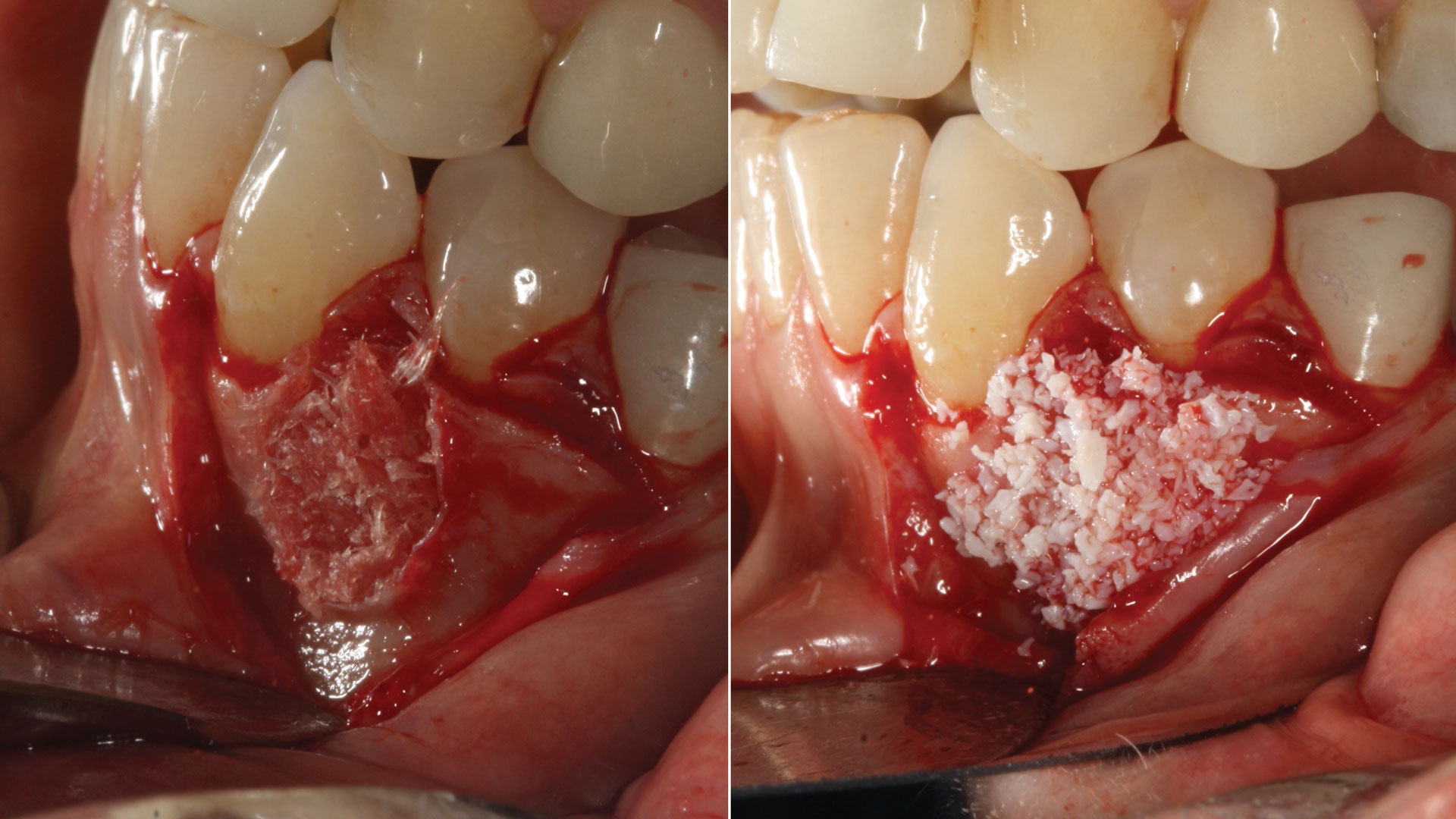
The combined defect: #11 distal guided tissue regeneration and #12 alveolar ridge preservation for #12. This area was treated with vallos®, Geistlich Bio-Oss Collagen®, and Geistlich Bio-Gide®. The xenograft was placed in the apical portion of the socket and the allograft towards the coronal surface.


Irina F. Dragan, DDS, DMD, MS, eMBA
Periodontology and Implant Dentistry
Dr. Irina Dragan is board certified and an examiner for the American Board of Periodontology and Implant Dentistry. She is part-time faculty in postgraduate periodontics at Harvard School of Dental Medicine and an adjunct associate professor of periodontology at Tufts University School of Dental Medicine. She is a periodontist and clinical researcher at The Perio Studio, a practice limited to periodontology and implant dentistry in Boston, MA.