BIOBRIEF
Bone Grafting and Immediate Implant Placement in the Maxillary First Molar Region


THE SITUATION
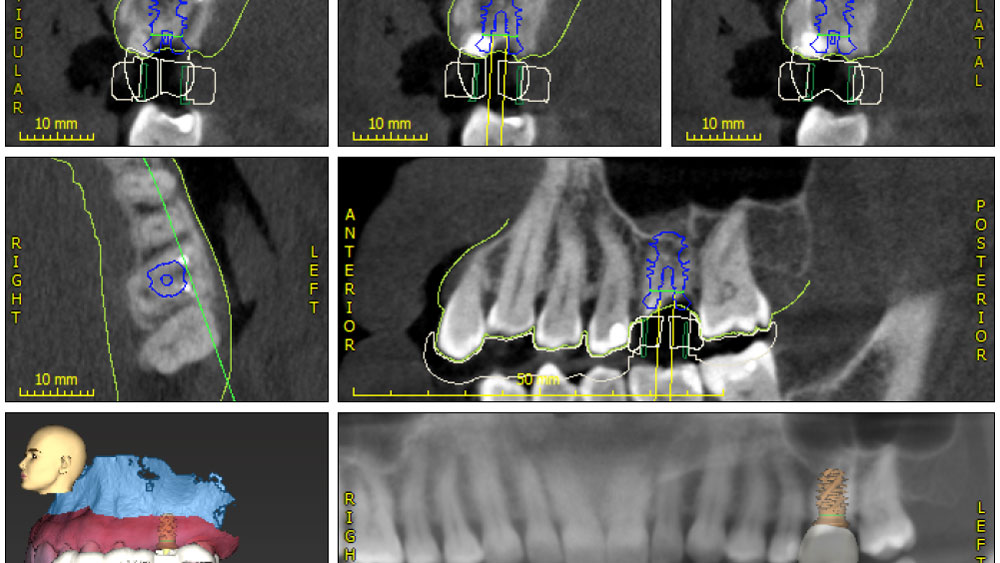
Patient presented with unrestorable left maxillary first molar. After data collection with Cone Beam Computed Tomography (CBCT) and intra-oral scanning, and clinical examination, the situation was considered favorable for minimally traumatic extraction and immediate implant placement.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system | Light smoker | Impaired immune system |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
Additional Risk Factors: Roots were divergent, and intra-radicular bone (septal bone) was excellent, with more than 5 mm of remaining apical bone to achieve optimal primary stability.
THE APPROACH
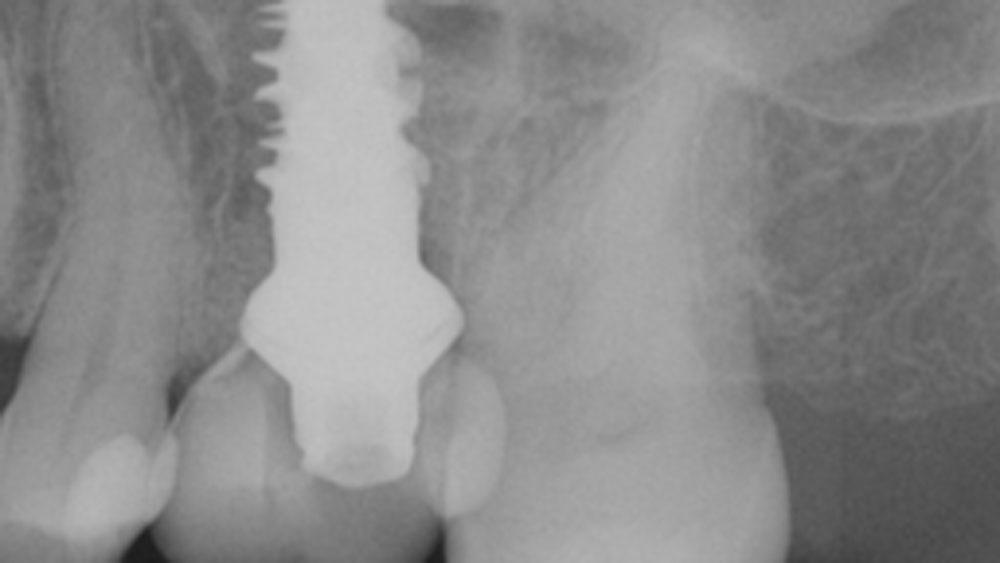
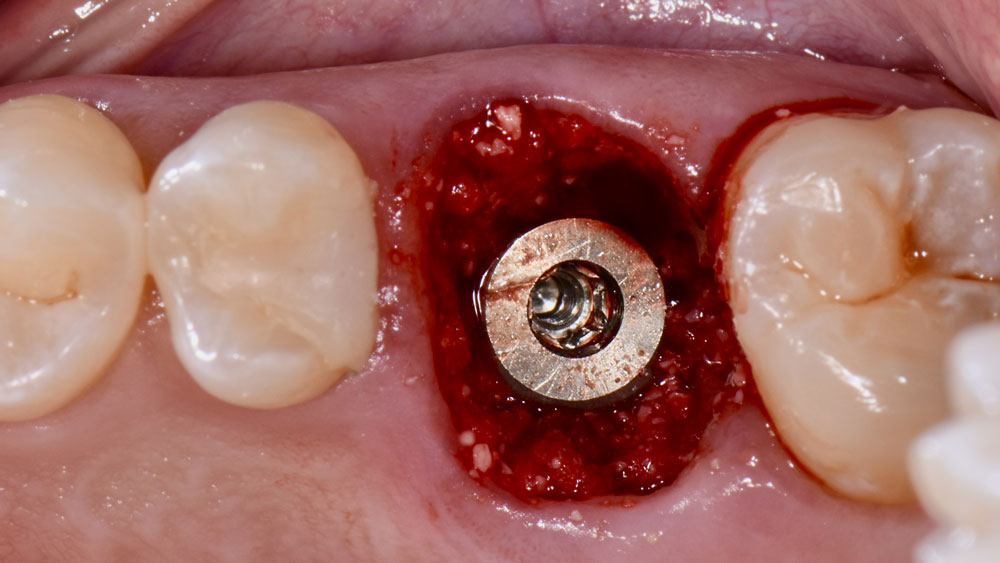
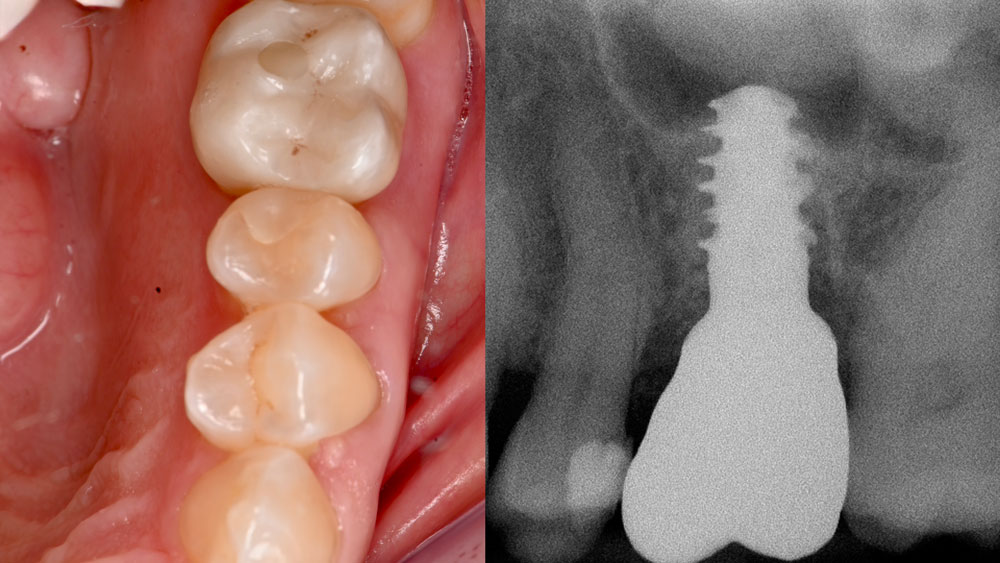
A fully guided approach was utilized, with an immediate provisional Computer-Aided Design (CAD) and Computer Aided Manufacturing (CAM) crown. Alveolar socket gaps were grafted with Geistlich Bio-Oss Collagen®, after implant placement. The provisional crown was used also as a socket seal, optimizing healing. After 3 months, a final ceramic crown was delivered. A one-year and a three-year follow-up show excellent clinical contour of the alveolar bone, and integration of the implant.
“Immediate implant placement and loading in molars is a feasible technique, with excellent long-term outcomes, if case selection is adequate, treatment planning is optimized by digital technology, and proper surgical and restorative techniques are applied.”
— Waldemar D. Polido, DDS, MS, PhD
THE OUTCOME
This case shows a three-year follow-up of an immediate implant placement, using Geistlich Bio-Oss Collagen® as a graft material on the gap. Careful tissue management, minimally traumatic extraction, and proper planning, including guided implant surgery can optimize treatment outcomes.

Waldemar D. Polido, DDS, MMS, PhD
Dr. Polido is an Oral and Maxillofacial Surgeon with MS and PhD degrees from the PUCRS School of Dentistry in Porto Alegre, RS, Brazil. He completed his residency in Oral and Maxillofacial Surgery at The University of Texas, Southwestern Medical Center in Dallas, Texas. Currently, Dr. Polido is a Clinical Professor of Oral and Maxillofacial Surgery at the Indiana University School of Dentistry. He is also the Co-Director of the Center for Implant, Esthetic, and Innovative Dentistry at Indiana University School of Dentistry in Indianapolis.

Wel-Shao Lin, DDS, FACP, PhD, MBA
Dr. Lin is a tenured Professor and Chair of Prosthodontics at Indiana University School of Dentistry. He earned his DDS from Chung-Shan and Surgical Implant Fellowship at the University of Rochester (2010). He holds a PhD in Educational Leadership (2020) and an MBA in Healthcare Administration (2022) and is currently pursuing a Master’s Intelligence. Dr. Lin specializes in dental implants, digital dentistry, and AI applications, with over 120 peer-reviewed publications. A Diplomate of the American Board of Prosthodontics and Fellow of ITI and ACP, he also serves as an associate editor for the Journal of Prosthodontics and maintains a clinical practice at Indiana University.