BIOBRIEF
Enhance Periodontal Phenotype with Geistlich Mucograft® for Soft Tissue Augmentation


THE SITUATION
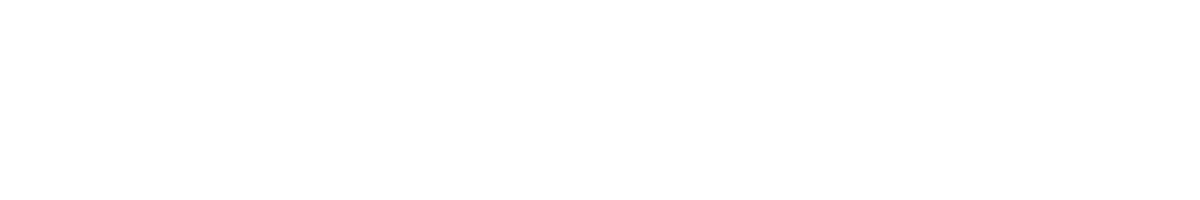
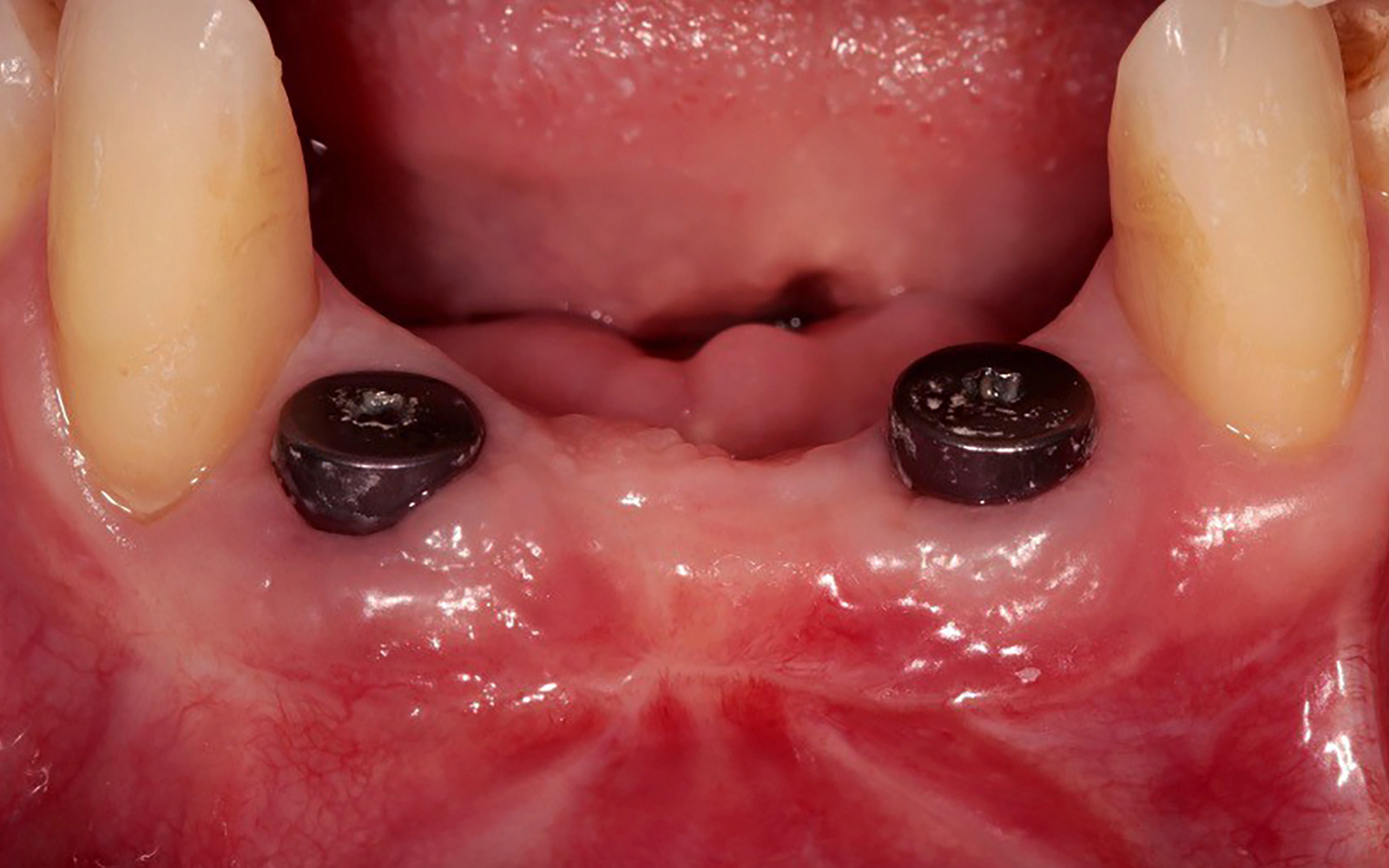
A healthy, non-smoking, 37- year-old female presented for second stage surgery at implant sites #23 and #26. Limited keratinized tissue width and gingival thickness can be appreciated in the edentulous ridge, and the patient can be classified as having a thin periodontal phenotype. Additionally, the patient states she experiences sensitivity, and the tissue feels “tender” when brushing. The patient hopes to address her needs in a minimally invasive manner.
THE RISK PROFILE
| Low Risk | Medium Risk | High Risk | |
|---|---|---|---|
| Patient’s health | Intact immune system Non-smoker | Light smoker | Impaired immune system Heavy smoker |
| Patient’s esthetic requirements | Low | Medium | High |
| Height of smile line | Low | Medium | High |
| Gingival biotype | Thick – “low scalloped” | Medium – “medium scalloped” | Thin – “high scalloped” |
| Shape of dental crowns | Rectangular | Triangular | |
| Infection at implant sight | None | Chronic | Acute |
| Bone height at adjacent tooth site | ≤ 5 mm from contact point | 5.5 – 6.5 mm from contact point | ≥ 7 mm from contact point |
| Restorative status of adjacent tooth | Intact | Restored | |
| Width of tooth gap | 1 tooth (≥ 7 mm) | 1 tooth (≤ 7 mm) | 2 teeth or more |
| Soft-tissue anatomy | Intact | Compromised | |
| Bone anatomy of the alveolar ridge | No defect | Horizontal defect | Vertical defect |
THE APPROACH
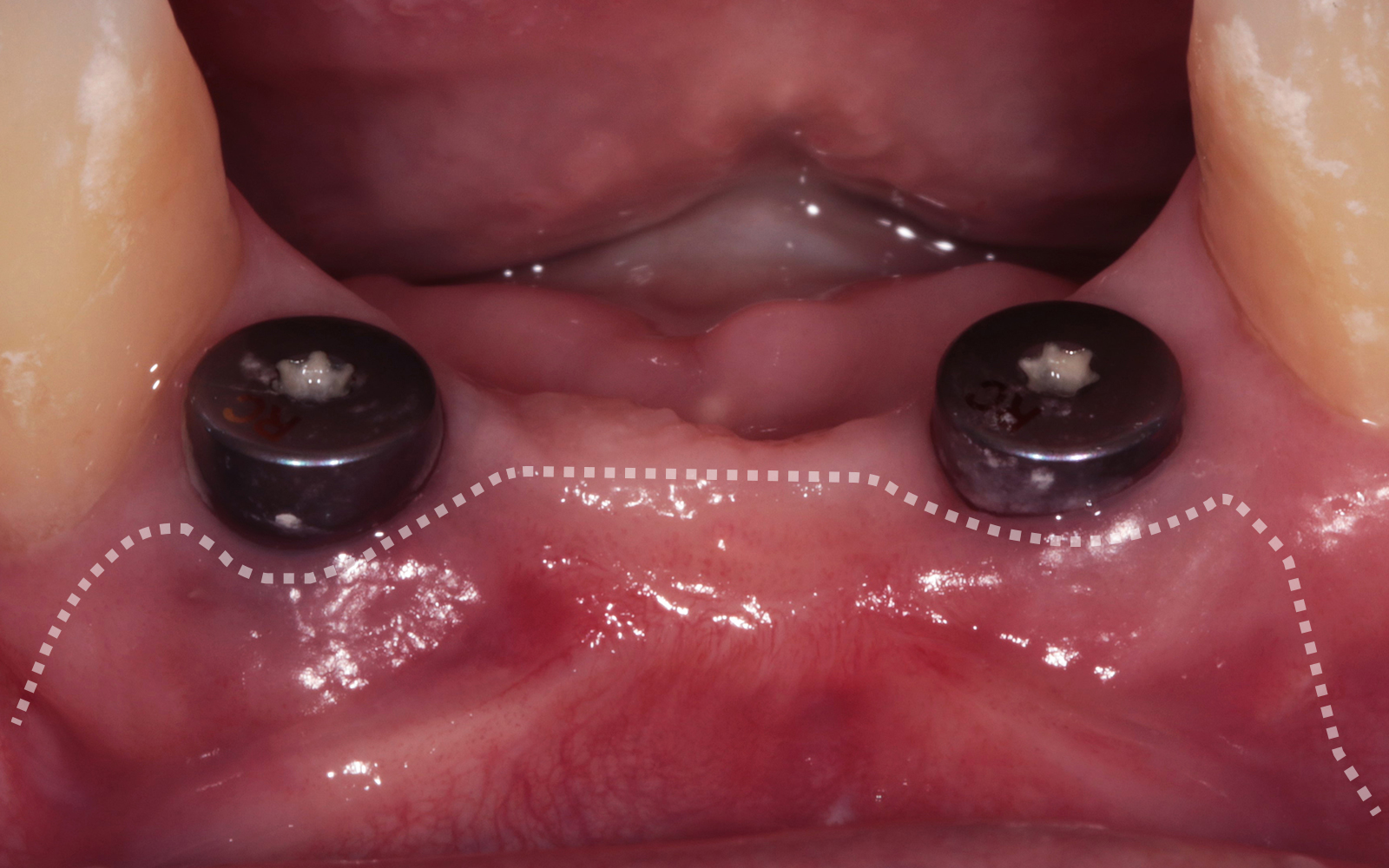
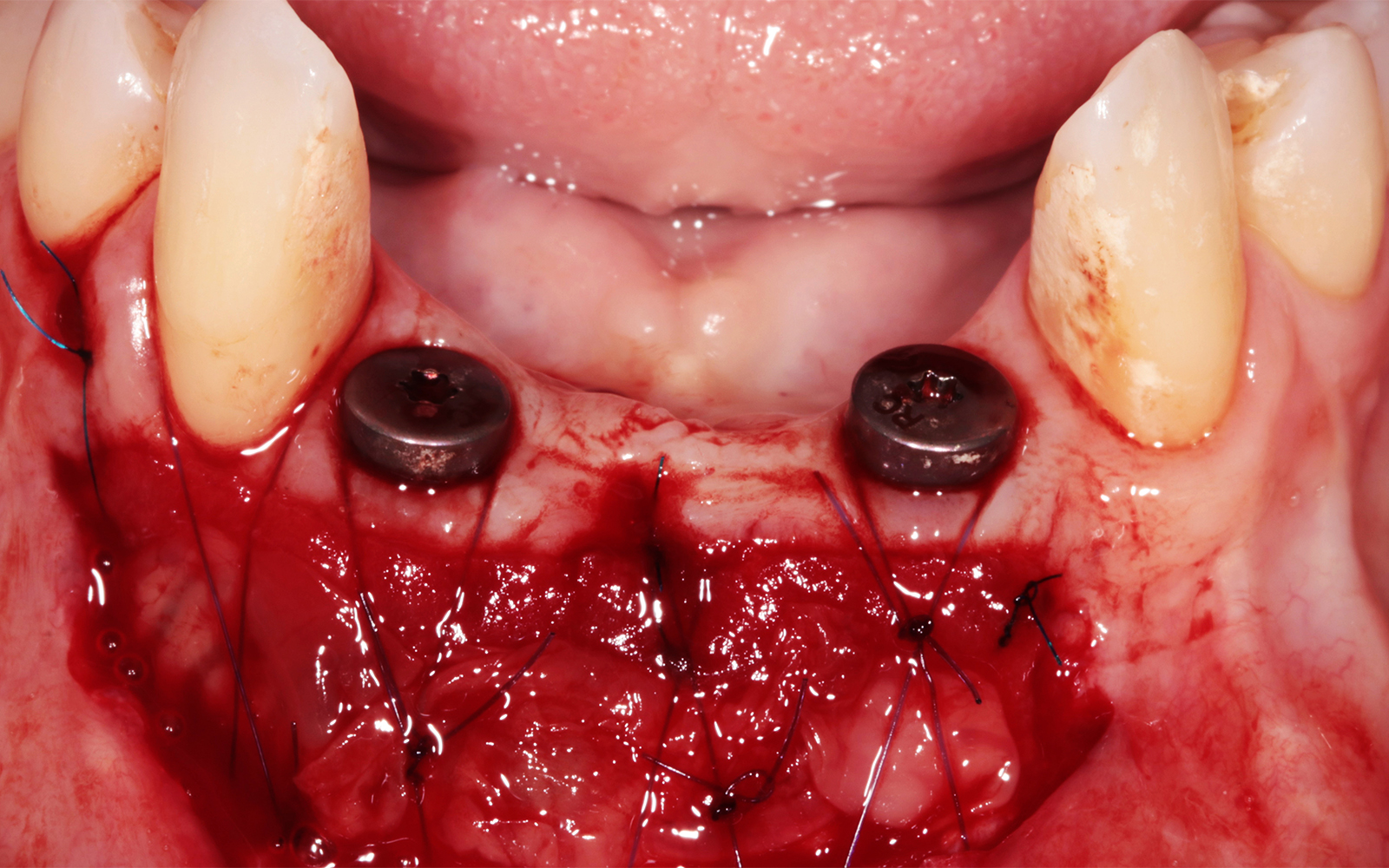
The aim of treatment was to enhance the existing periodontal phenotype from that of one which is thin, with limited keratinized tissue, to one that is thick and maintains an adequate band of attached keratinized tissue. Geistlich Mucograft® was used in conjunction with a PRF membrane, in order to provide optimal wound healing, due to its chemotactic and angiogenic properties.
A viable option that allows for reduced patient morbidity, adequate functional necessity, and ideal esthetics.
THE OUTCOME
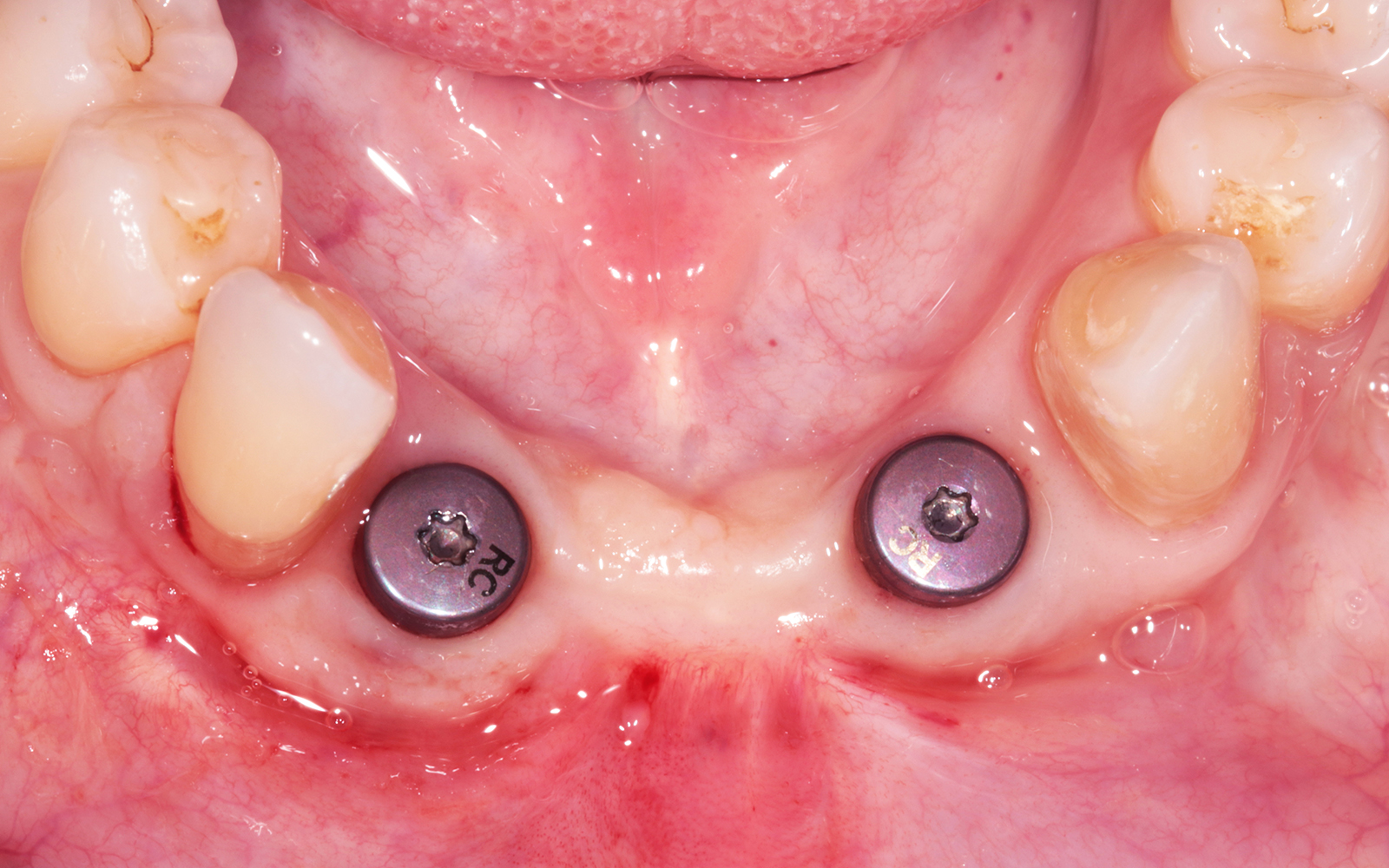
Dual application of platelet-rich fibrin (PRF) and a xenogenic collagen matrix, Geistlich Mucograft®, led to successful augmentation of the edentulous ridge. At one-year, the tissues appear healthy, and an increased keratinized tissue width and gingival thickness can be appreciated. By using this soft tissue alternative, the patient was able to avoid post-operative morbidity from a second surgical site, and the chief complaint was addressed.


Allison Rascon, D.D.S., M.S.
Dr. Allison Rascon was born and raised in Miami, Florida. She received her Bachelor of Science in Biomedical and Health Sciences from the University of Central Florida. She received her DDS from New York University, where she graduated with honors in Periodontics and was inducted into the Omicron Kappa Upsilon National Dental Honor Society in 2020. She then went on to receive a Certificate in Periodontics and Master of Science in Oral Biology from the University of Pennsylvania. Currently, she is board-eligible by the American Academy of Periodontology. She is an active member of the AAP, AO, OF, and ADA. Aside from her active participation in organized dentistry, she is also passionate about her research in periodontal and peri-implant regeneration. Dr. Rascon was a recipient of the George J. Coslet Memorial Scholarship in 2021 and 2022. During her residency, she was awarded the Best Oral Clinical Presentation Award at the Academy of Osseointegration Annual Meeting in 2022 and was the recipient of the Northeastern Society of Periodontists Tannenbaum/ Schoor Resident School Competition Award for 2023. Currently, Dr. Rascon works in private practice in Manhattan, NY.